Abstract
Asthma is a chronic disease with clinical variations throughout its course. Periods of symptom aggravation can occur with the need to escalate therapy. Nevertheless, further investigation should be considered when atypical manifestations appear or when worsening of symptoms occurs. Proximal tracheal/bronchial obstruction can mimic symptoms observed in patients with asthma. Primary benign tracheal tumors are rare, but can constitute the cause for such symptoms. We present a case report of a patient with asthma and a tracheal lesion.
Keywords: Tracheal Harmartoma, Asthma, Bronchoscopy
1. Introduction
Primary tracheal tumors are usually malignant. Benign tumors account for only 10% of cases [1,2]. While hamartomas are the most frequent subtype of lung tumors, their location in the trachea is rare. Patients may have symptoms of dyspnea, cough and hemoptysis [3] that may be confused with other pathologies, such as chronic obstructive airway diseases [2], therefore the diagnosis can be delayed in patients with previously diagnosed asthma. Careful examination of flow-volume curves can alert for the presence of a partial central obstruction and must not be overlooked [4].
2. Case report
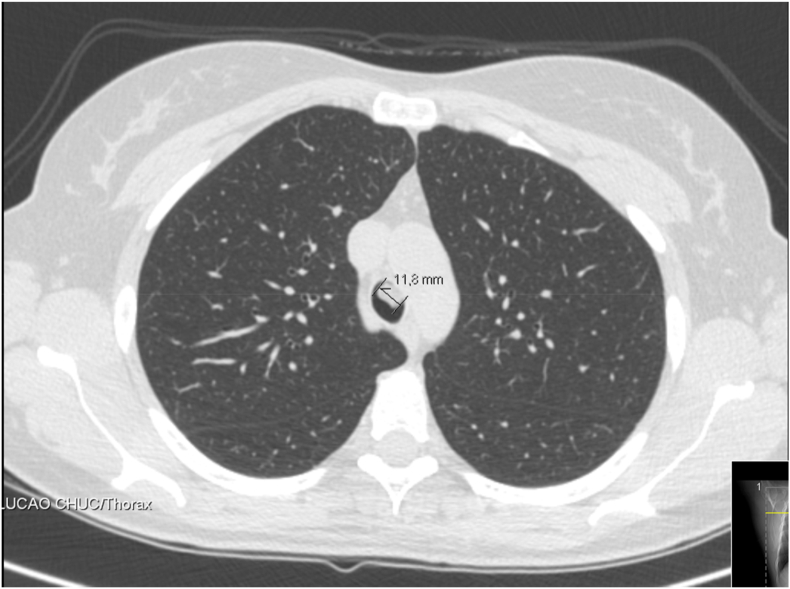
A 34-year-old female patient, with a history of non-allergic asthma, former smoker of approximately 5 pack-years, was followed at the Pulmonology clinic. She also had history of Wolff-Parkinson-White syndrome and rhinitis. Treatment prescribed was inhaled budesonide/formoterol, bilastine, and nasal fluticasone. In the last year the patient showed worsening symptoms of cough and dyspnea, that continued even after therapeutic adjustment to high dose inhaled corticosteroid. Also, three acute exacerbations occurred in this period. To study this clinical aggravation, thoracic-CT was performed, which revealed a oval hypodense formation in the left anterolateral wall of the trachea, with 12 mm (Fig. 1). Flexible bronchoscopy showed a polypoid lesion between the middle and the lower third of the trachea with implantation in the anterior wall and partial obstruction (<50%) of the lumen (Fig. 2).
Fig. 1.
Thoracic–CT image of tracheal lesion.
Fig. 2.
Bronchoscopic image of the tracheal lesion.
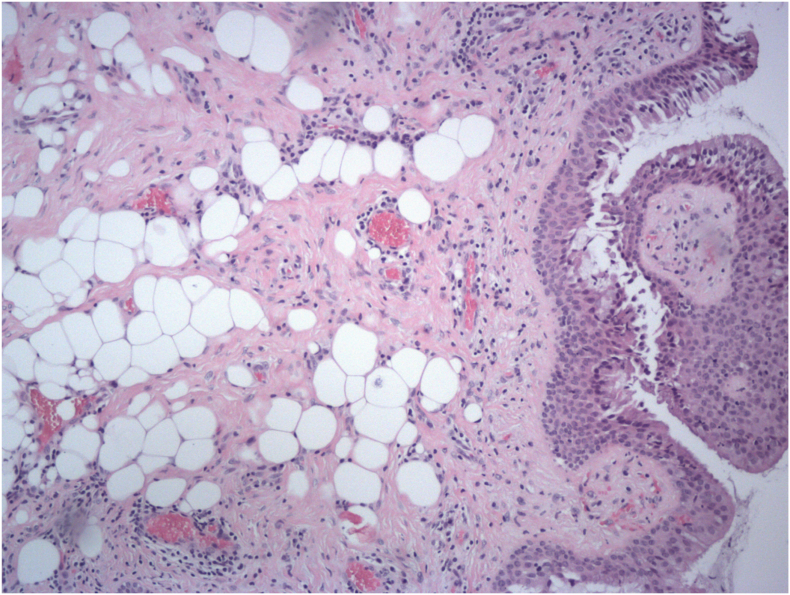
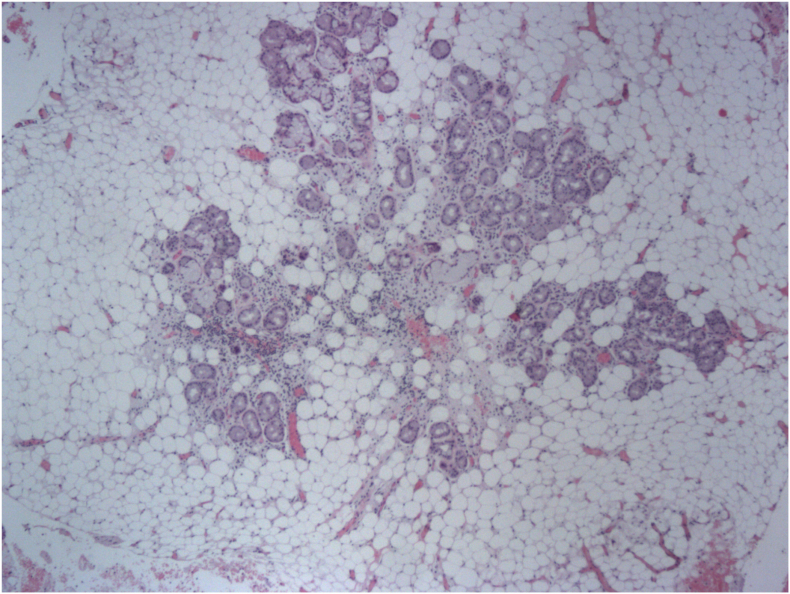
Tissue biopsied from the lesion had pathological findings consistent with a tracheal lipoma. Considering it was a benign tumor a rigid bronchoscopy was performed to resect it. Histology of the resected tissue showed changes compatible with the diagnosis of tracheal hamartoma - respiratory epithelium with underlying basal cell hyperplasia, proliferation of mature adipocytes involving mucinous glands with areas of mature and immature cartilage and areas of mononuclear inflammatory infiltrate (Fig. 3, Fig. 4).
Fig. 3.
Adipose tissue on the lamina propria of the tracheal mucosa.
Fig. 4.
Sero-mucinous glands dissociated by adipose tissue.
After excision, the patient reported significant clinical improvement, without complications of the reported procedures. Flexible bronchoscopy was performed to review remaining abnormalities. Two millimetric tumors were observed, at the site of implantation of the resected hamartoma, that were excised.
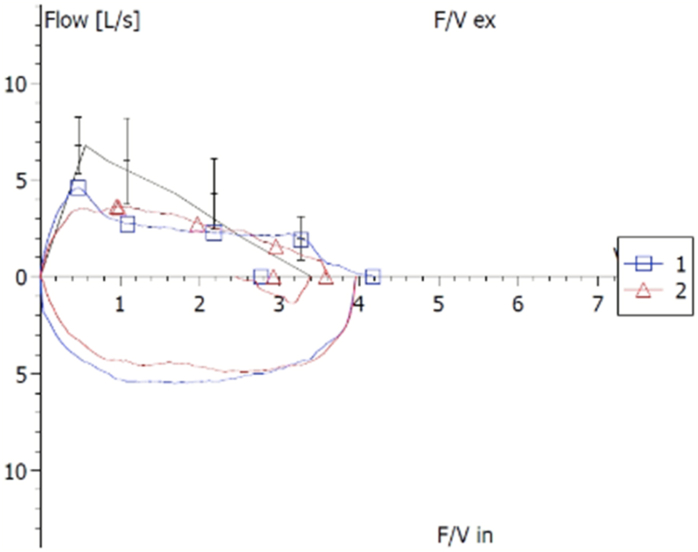
Posteriorly, when reviewing the clinical data of the patient, we noticed that the flow volume-curve was flattened (Fig. 5), but in the technical report it was referred that the patient had insufficient collaboration and so these alterations were interpreted then as the result of lack of cooperation during the functional respiratory testing. The patient maintained follow-up at the pulmonology clinic.
Fig. 5.
Flow volume curve in functional respiratory test.
3. Conclusions
A hamartoma is defined as a benign tumor with a configuration of cells presumably derived from primitive connective tissue such as cartilage, fat, bone, and smooth muscle cells [1]. The most frequent symptoms associated with primary tracheal tumors are cough, hemoptysis and dyspnea [3]. In this case, at first, the clinical worsening of the patient was interpreted only has an aggravation of asthma symptoms and treated accordingly. This shows that there should be a high degree of suspicion when a disease that previously had a relatively stable evolution worsens. Complementary diagnostic exams, especially imaging, are essential to exclude other unforeseen aggravating factors. Also, careful examination and interpretation of flow-volume curves is fundamental and must not be neglected [4].
Declaration of competing interest
None of the authors of this paper has a financial or personal relationship with other people or organizations that could inappropriately influence or bias the content of the paper.
It is to specifically state that “No Competing interests are at stake and there is No Conflict of Interest” with other people or organizations that could inappropriately influence or bias the content of the paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101127.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Hon C. Endotracheal hamartoma case report: two contrasting clinical presentations of a rare entity. Int. J. Surg. Case Rep. 2017;38:98–101. doi: 10.1016/j.ijscr.2017.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahn Primary tracheal tumors: review of 37 cases. J. Thorac. Oncol. 2009 May;4(5):635–638. doi: 10.1097/JTO.0b013e31819d18f9. [DOI] [PubMed] [Google Scholar]
- 3.Gaissert Uncommon primary tracheal tumors. Ann. Thorac. Surg. 2006 Jul;82(1):268–272. doi: 10.1016/j.athoracsur.2006.01.065. [DOI] [PubMed] [Google Scholar]
- 4.Panjwani A, Lodha J. Pulmonary function test in upper airway obstruction: a simple yet effective diagnostic test. Egypt. J. Intern. Med. 31:243–246.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.