Abstract
Objective:
The objective of this study was to evaluate the effect of skipping breakfast on body composition and cardiometabolic risk factors.
Methods:
This study conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) evaluating breakfast skipping compared with breakfast consumption. Inclusion criteria included age ≥ 18, intervention duration ≥ 4 weeks, ≥ 7 participants per group, and ≥ 1 body composition measure. Random-effects meta-analyses of the effect of breakfast skipping on body composition and cardiometabolic risk factors were performed.
Results:
Seven RCTs (n = 425 participants) with an average duration of 8.6 weeks were included. Compared with breakfast consumption, breakfast skipping significantly reduced body weight (weighted mean difference [WMD] = −0.54 kg [95% CI: −1.05 to −0.03], P = 0.04, I2 = 21.4%). Percent body fat was reported in 5 studies and was not significantly different between breakfast skippers and consumers. Three studies reported on low-density lipoprotein cholesterol (LDL), which was increased in breakfast skippers as compared with breakfast consumers (WMD = 9.24 mg/dL [95% CI: 2.18 to 16.30], P = 0.01). Breakfast skipping did not lead to significant differences in blood pressure, total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, C-reactive protein, insulin, fasting glucose, leptin, homeostatic model assessment of insulin resistance, or ghrelin.
Conclusions:
Breakfast skipping may have a modest impact on weight loss and may increase LDL in the short term. Further studies are needed to provide additional insight into the effects of breakfast skipping.
Introduction
Obesity affects nearly 40% of US adults and contributes to the development of cardiovascular disease, stroke, type 2 diabetes, and multiple cancers (1,2). Annually, the United States spends $147 billion dollars on obesity, which has nearly doubled since 1998 (3). An additional $200 billion dollars is spent annually on heart disease (4). Much research has been conducted exploring the effects of specific foods and dietary patterns on these conditions, but the effects of specific mealtimes, such as for breakfast, remain unknown.
Breakfast has anecdotally been considered the most important meal of the day, although the basis for this is unclear (5). Multiple observational studies in the United States, a 2010 systematic review, and a meta-analysis in Asian and Pacific regions have shown inverse associations between breakfast consumption and weight gain (6–10). Recently, a potentially causal link between genetically determined breakfast skipping and higher BMI through a Mendelian randomization analysis was observed (11). However, despite the fairly consistent association of breakfast consumption with decreased body weight, randomized controlled trials (RCTs) have shown equivocal results (12–14). A recent meta-analysis published in 2019 evaluating breakfast consumption, body weight, and energy intake found that those participants who skipped breakfast reduced their body weight by 0.44 kg compared with breakfast consumers (15). However, their analysis did not evaluate other body composition parameters aside from body weight, had no minimal study duration restriction, and did not evaluate other cardiometabolic risk factors.
Prospective studies suggest that adults who skip breakfast have increased risks of cardiovascular disease and cardiovascular mortality compared with adults who consume breakfast (16–18). Studies have shown higher fasting insulin, total cholesterol (TC), and low-density lipoprotein cholesterol (LDL) in children and adults who skip breakfast (8,19). RCTs have subsequently demonstrated that breakfast skipping increases TC, LDL, and high-density lipoprotein cholesterol (HDL) (12–13,20). However, most of the studies have small sample sizes, and no meta-analysis of RCTs has been conducted to assess the relationship between breakfast skipping and cardiometabolic risk factors.
The aim of this study was to conduct a systematic review and meta-analysis of RCTs evaluating the effect of skipping breakfast on body composition and cardiometabolic risk factors over a period of at least 4 weeks. We hypothesized that breakfast skipping would result in weight gain and would worsen cardiometabolic risk factors.
Methods
Search strategy
We conducted a systematic review and meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, and we registered the meta-analysis in the PROSPERO database (identifier CRD42018110858) (21,22). We searched for articles indexed in PubMed, Cochrane, the Cumulative Index to Nursing and Allied Health Literature, and Embase published from inception until October 10, 2018. Combinations of the keywords breakfast*, morning meal*, and random* were used as search terms. The actual searches for each database are included in Supporting Information Figure S1. Reference lists for the full text articles retrieved were also screened for additional articles that might be relevant. We restricted the search to RCTs in humans, but no language limitations were placed.
Inclusion criteria
We included RCTs that evaluated breakfast skipping compared with breakfast consumption. RCTs in adults (age ≥ 18) that lasted at least 4 weeks or randomized crossover trials with each arm lasting at least 4 weeks were eligible. No criteria on minimum required study length for weight change exist. Four weeks was chosen as a minimum criterion because multiple studies have shown that more weight loss at 1 month is associated with greater longer-term weight loss (23,24). A minimum of 7 participants per study arm was required, to be consistent with a 2017 American Heart Association review on meal timing and cardiovascular disease (25). Studies had to have at least one breakfast-consumption arm and one skipping-breakfast arm. Breakfast was allowed to be defined by study authors, as no agreed on definition exists (26). Lastly, at least one body composition parameter (including body weight) had to be reported before and after the intervention.
Exclusion criteria
Trials that used dietary supplements, medications, or different exercise interventions among groups were excluded. If the study population had any underlying disease or genetic condition that impacted body weight (i.e., human immunodeficiency virus, cancer, or previous bariatric surgery), these studies were excluded as well. However, cardiometabolic conditions such as diabetes, heart disease, and obesity were permissible.
Data extraction and quality assessment
Search results were downloaded to EndNote (Clarivate Analytics, Philadelphia, PA) and, after being deduplicated, were uploaded to Covidence (Veritas Health Innovation Ltd, Melbourne, Australia). Two reviewers, JPB and MIC, independently screened all titles and abstracts. Disagreements were resolved via discussion with a third author (MG-F). Full texts of any article that appeared to meet the inclusion criteria were obtained.
We extracted information on study characteristics (citation, study name, authors, publication year, funding sources, study design, study intervention, and control breakfast characteristics, including time of consumption, study duration and intervention length, and methods for assessment of compliance), study inclusion and exclusion criteria, and participant characteristics (number of participants, mean age and SD, sex, and habitual breakfast consumption status). We extracted the baseline, follow-up, and changes in mean ± SD/SE/95% CI for body composition parameters (e.g., body weight, fat mass, fat-free mass, BMI, percent body fat) and cardiometabolic parameters (e.g., systolic and diastolic blood pressure, TC, HDL, LDL, triglycerides, C-reactive protein [CRP], insulin, fasting glucose, homeostatic model assessment of insulin resistance [HOMA-IR], leptin, and ghrelin). SDs were derived from SEs, or 95% CIs when necessary, assuming a normal distribution of the parameters.
In trials that had more than one breakfast-consumption arm, groups were combined to compare all breakfast skippers with all breakfast consumers in individual studies. This was done to investigate the impact of skipping breakfast, as compared with consuming something for breakfast, and to avoid giving higher weight to studies with multiple intervention arms. Corresponding authors of the included studies were contacted for additional information when the published manuscript was unclear regarding research protocol, data, or analysis. Study quality was assessed independently by JPB and MIC using the NIH Study Quality Assessment Tool for RCTs.
Statistical analysis: data synthesis and meta-analysis
Our primary outcome of interest was the difference in preintervention to postintervention changes in body composition parameters (body weight [kilograms], fat mass [kilograms], lean mass [kilograms], BMI [kilograms per meter squared], percent body fat [percentages]), comparing breakfast skippers with breakfast consumers. Secondary outcomes included the cardiometabolic parameters described earlier. We converted TC, LDL, HDL, triglycerides, and fasting glucose to milligrams per deciliter (conversion factor for cholesterol: millimoles per liter multiplied by 38.67; triglycerides conversion: millimoles per liter multiplied by 88.57; fasting glucose conversion: millimoles per liter multiplied by 18.02). Insulin was converted to microinternational units per milliliter (conversion factor: picomoles per liter multiplied by 0.14).
We extracted preintervention and postintervention means, SDs, and changes in mean/SDs when available. If changes were not reported, we calculated the mean difference within each group, and used a correlation value of 0.8 to calculate the SD of the mean change using SD(diff [difference]) = sqrt (square root) (SD22 + SD12 − [2*0.8*sqrt (SD12)*sqrt(SD22)]). A correlation coefficient of 0.8 was chosen, as it was the average correlation coefficient found using available correlation calculation coefficients (n = 3) from other studies included in this meta-analysis that had sufficient data. When combining 2 breakfast-consuming groups, SDs were calculated using SD(combined) = sqrt([(n1 − 1)*SD12 + (n2 − 1)*SD22] / (n1 + n2 − 2)]).
Random-effects meta-analyses using weighted mean differences (WMDs) were performed to pool the effect estimates from each study. Heterogeneity was estimated between studies using the Cochran Q test and I2 statistics. We considered I2 > 30% as moderate heterogeneity and considered statistically significant heterogeneity as P < 0.10. Secondary analyses were conducted using fixed-effect models and individual breakfast arms rather than using a combination of all breakfast interventions within a single study.
We also performed stratified analyses using random-effects models. WMDs were calculated for stratified analyses of trials in groups with normal weight (BMI = 18.5 to 24.9), groups with overweight/obesity (BMI ≥ 25), and groups that habitually skipped breakfast. A secondary analysis of trials lasting ≥ 8 weeks was also run.
Funnel plots were generated, and Egger and Begg tests were used with a significance level of P < 0.05. Data were analyzed using Stata (StataCorp., College Station, Texas), with a 2-sided P value of 0.05 considered statistically significant.
Results
Literature search
Two reviewers screened 7,389 studies (Supporting Information Figure S2). Full texts were obtained for 23 articles that met the inclusion criteria. However, 16 of these articles were excluded because they had interventions lasting less than 4 weeks (n = 5), did not have breakfast consumption and breakfast skipping arms (n = 4), were not RCTs (n = 3), were the same study (abstract or poster with a different name, n = 2), were missing the outcome of interest (n = 1), or did not have the appropriate data available (n = 1). Seven articles were ultimately included in the data analysis. Study characteristics of the included RCTs are summarized in Table 1.
TABLE 1.
Study characteristics of RCTs on breakfast skipping and body composition
| Authors, y, Country | Population | No. of Participants (% female), Intervention | Age (mean y ± SD) | BMI (mean ± SD) | No. of habitual breakfast consumers (%) | Breakfast skipping | Breakfast consumption | Adherence assessed by (% compliance) | Outcomes measured | Duration | Funding |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Betts et al., 2014 (12), United Kingdom | Lean Adults (based on DXA fat mass indexes ≥ 7.5 kg/m2 for men and ≥ 11 kg/m2 for women). | 33 (64), breakfast vs. no breakfast. | 36 ± 11 | 22.4 ± 2.2 | 26 (79) | Extended overnight fast until 1200 h daily (other than water). | Energy intake ≥ 700 kcal before 1100 h daily, with at least half consumed within 2 h of waking. Food information provided, Including amount, but no foods specified. | Self-reported by participants and verified via continuous glucose monitoring (not reported). | Body weight, BMI, % body fat, lean mass, fat mass, blood pressure, lipids, CRP, insulin, HOMA-IR, glucose, leptin, ghrelin. | 6 wk | Biotechnology and Biological Sciences Research Council |
| Chowdhury et al. (13), 2016, United Kingdom | Adults with obesity (based on DXA fat mass indexes ≥ 9 kg/m2 for men and ≥ 13 kg/m2 for women). | 23 (65), breakfast vs. no breakfast. | 44 ± 10 | 33.7 ± 4.9 | 14 (61) | Extended overnight fast until 1200 h daily (other than water). | Energy intake ≥ 700 kcal before 1100 h daily, with at least half consumed within 2 h of waking. Food information provided, Including amount but no foods specified. | Self-reported by participants and verified via continuous glucose monitoring (not reported). | Body weight, BMI, % body fat, lean mass, fat mass, blood pressure, lipids, CRP, insulin, HOMA-IR, glucose, leptin, ghrelin. | 6 wk | Biotechnology and Biological Sciences Research Council |
| Dhurandhar et al. (14), 2014, United States | Adults with overweight or obesity (BMI > 25 and < 45) | 185 (76), 3 groups: control, breakfast, no breakfast. | 41.6 ± 12.1 | 32.7 ± 5.2 | 108 (58) | No calories consumed until 1100 h (other than water or zero-calorie beverages). | Instructed to consume breakfast before 1000 h dally. Nutrition education pamphlet provided but no foods or amounts specified. | Reported by participants via food diary and monthly calls (93.6% consumers, 92.4% skippers). | Body weight, BMI. | 16 wk | NIDDK; National Heart, Lung, and Blood Institute |
| Geliebter et al. (20), 2014, United States | Adults with overweight (BMI > 25). | 36 (50%), 3 groups: no breakfast, high fiber, no fiber. | 33.9 ± 7.5 | 32.8 ± 4.7 | Not reported | Reported to center at 0830 h following overnight fast each weekday. Consumed 350 mL water of plus 200 mL of decaffeinated coffee with 12 mL of nondairy creamer and 1 g of artificial sweetener. | Reported to center at 0830 h following overnight fast each weekday. Consumed either oat porridge or frosted corn flakes plus 200 mL of decaffeinated coffee with 12 mL of nondairy creamer and 1 g of artificial sweetener. Breakfasts were provided to take home for the weekends. | Direct observation, except for weekends (not reported). | Body weight, lean mass, fat mass, blood pressure, lipids, insulin, HOMA-IR, glucose, leptin. | 4 wk | Quaker Oats Center of Excellence, PepsiCo R&D Nutrition |
| LeCheminant et al. (29), 2017, United States | Healthy adults (habitual breakfast skippers; no BMI restriction). | 49 (100), breakfast vs. no breakfast. | 23.7 ± 7.5 | 22.1 ± 3.8 | 54 (0%) | No snack or meal consumed until after 1130 h (except noncaloric beverages). | Required to eat 15% of total energy Intake within 1.5 h of awakening and had to be finished eating breakfast by 0830 h. No eating restrictions after this meal. | Reported by participants via food log (90% consumers, 98% skippers). | Body weight, BMI, % body fat, lean mass, fat mass. | 4 wk | Fulton Grant from Brigham Young University |
| Leidy et al. (28), 2015, United States | break/>Adults/adolescents with overweight/obesity (habitual breakfast skippers; BMI: 25 to 39.9). | 54 (59), | 19 ± 5.7 | 29.8 ± 4.6 | 49 (0) | Fasting until 1000 h (except for water). | Instructed to consume either normal-proteln (cereal with milk) or high-protein (egg-based dish, with pork/ham) Isocalorlc breakfasts between 0600 h and 0945 h. | Reported by participants via daily log. Breakfast meals provided to patients (98.1%). | Body weight, BMI, % body fat, lean mass, fat mass. | 12 wk | The Pork Checkoff |
| Schlundt et al. (27), 1992, United States | Women with obesity (no BMI range specified). | 45 (100), breakfast vs. no breakfast. | Not reported (18- to 55-y range). | Not reported. | 29 (59) | Instructed to eat 2 meals daily, 1,200 kcal total. Provided with bran muffins to match fiber. | Instructed to eat 3 meals per day, 1,200 kcal total. Provided with cereal for breakfast. | Reported by participants via log. Menus and cereal/bran muffins provided (97% skippers). | Body weight, % body fat. | 12 wk | None reported |
Studies are all parallel RCTs (Dhurandar, Geliebter, and Leidy studies all had 3 parallel arms).
CRP, C-reactive protein; DXA, dual-energy x-ray absorptiometry; HOMA-IR, homeostatic model assessment of insulin resistance; RCT, randomized controlled trial.
Characteristics of the RCTs
All included trials were parallel RCTs. The sample sizes ranged from 23 to 185 participants. A total of 425 participants were included in the meta-analysis. Participant range of age was 18 to 65 years old, with a mean age of 35 years old (average age not reported in Schlundt et al. (27)). All the studies were conducted in the United States and the United Kingdom. The studies lasted between 4 and 16 weeks, with an average duration of 8.6 weeks. Five of the trials were conducted in adults with overweight or obesity (13–14,20,27,28), and two of the trials were conducted in adults with normal weight (12,29). The mean baseline BMI was 30.1 (average not reported in Schlundt et al. (27)). Two of the studies were conducted in habitual breakfast skippers (28,29), with the Schlundt et al. study (27) being stratified by habitual breakfast consumer/skipper. The details of the breakfast interventions varied across trials and can be seen in Table 1. The skipping-breakfast and breakfast interventions generally involved extending the overnight fast until between 1000 hours and 1200 hours the following morning and a predefined breakfast meal routine, respectively. Breakfast meals ranged from recommendations alone, to premade foods that were provided to participants, and to direct observation in the laboratory. Adherence was assessed by using self-reported food logs (12–14,27–29), direct observation (20), and continuous glucose monitoring (12,13). Reported adherence levels ranged from 90% to 98% (Table 1). Using the NIH Quality Assessment Tool for controlled intervention studies to assess for study quality, 6 studies (12–14,20,28,29) were rated as being of “good” quality and 1 (Schlundt et al. (27)) was rated as being of “fair” quality.
Body composition meta-analysis
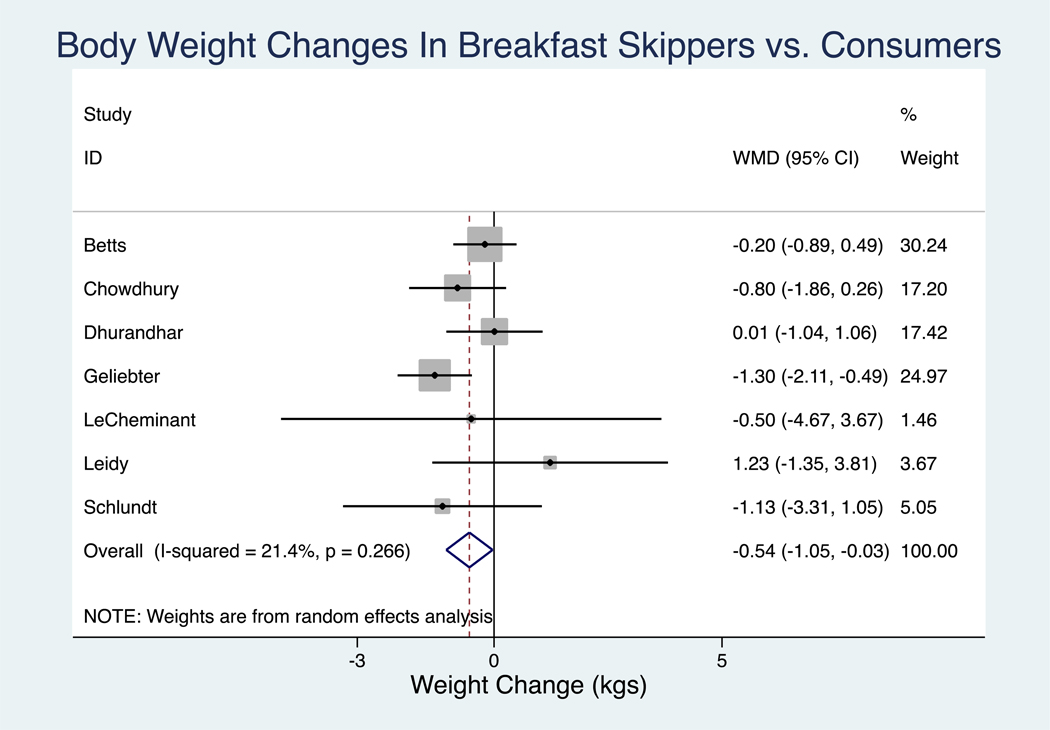
Body weight was the only outcome reported in all 7 studies. A random-effects meta-analysis of the results showed that at the end of the trials, as compared with breakfast consumers, participants who skipped breakfast had a greater reduction in body weight (WMD = −0.54 kg [95% 95% CI: −1.05 to −0.03], P = 0.04]), with low heterogeneity (I2 = 21.4%; P heterogeneity = 0.27) (Figure 1, Table 2). BMI, lean mass, fat mass, and percent body fat were reported in 5 studies. No significant differences were observed for other body composition parameters, including changes in BMI, lean mass, or fat mass (Table 2, Supporting Information Figure S3).
Figure 1.
Random-effects meta-analysis of changes in body weight (kilograms) in breakfast skippers as compared with breakfast consumers in RCTs. Closed rectangles and horizontal bars represent overall estimates (difference of means) and 95% CIs for individual studies. Diamonds represent overall estimate combining all the studies. ID, identifier; RCT, randomized controlled trial; WMD, weighted mean difference.
TABLE 2.
Primary outcome summary for random-effects meta-analysis of WMD in body composition parameters in breakfast skippers as compared with breakfast consumers
| Outcome | No. of studies (No. of participants) | WMD | Lower 95% CI | Upper 95% CI | P value | I2, % | Egger P value | Begg P value |
|---|---|---|---|---|---|---|---|---|
| Body weight (kg)a | 7 (425) | −0.54 | −1.05 | −0.03 | 0.04a | 21.4 | 0.72 | 0.88 |
| BMI | 5 (345) | −0.11 | −0.28 | 0.06 | 0.22 | 0 | 0.63 | 0.62 |
| % Body fat | 5 (204) | 0.33% | −0.40 | 1.06 | 0.37 | 46.2 | 0.37 | 0.62 |
| Lean mass (kg) | 5(188) | −0.24 | −0.84 | 0.36 | 0.44 | 0 | 0.26 | 0.14 |
| Fat mass (kg) | 5(188) | 0.27 | −0.43 | 0.97 | 0.45 | 0 | 0.76 | 0.81 |
Statistically significant at P < 0.05.
WMD, weighted mean difference.
Cardiometabolic parameter meta-analysis
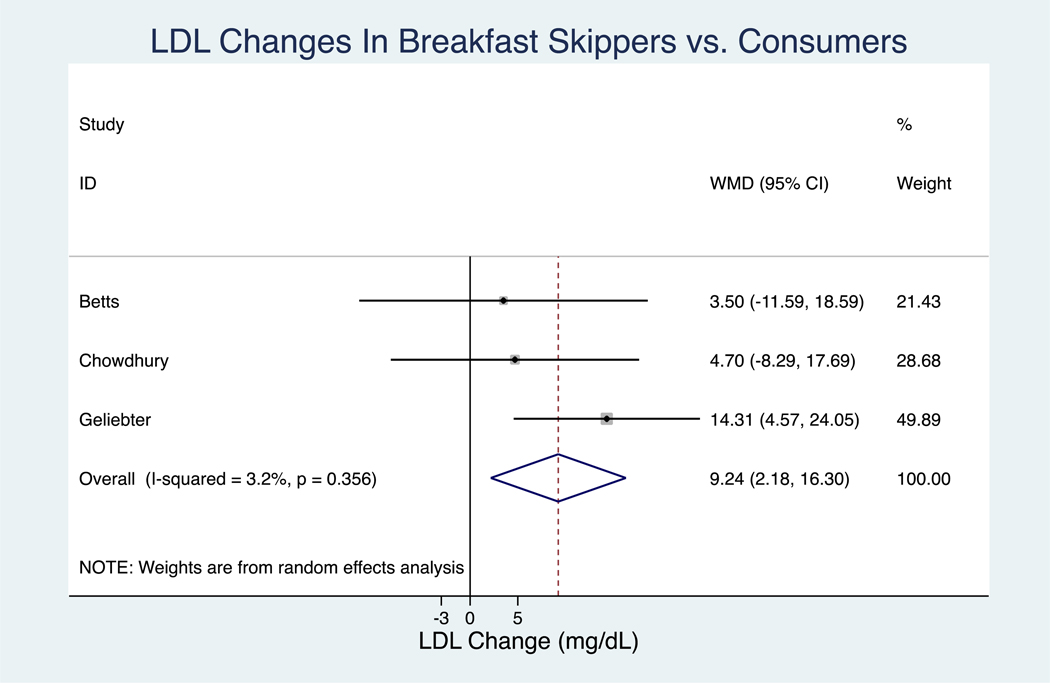
Cardiometabolic parameter variables were not consistently reported, with 2 or 3 studies (n = 56 to 92 participants) reporting each cardiometabolic variable (Table 3). LDL significantly increased by 9.24 mg/dL (95% CI: 2.18 to 16.30; P = 0.01, with an I2 = 3.2%; P heterogeneity = 0.36) in breakfast skippers, as compared with breakfast consumers (Figure 2, Table 3). No significant differences were observed for blood pressure, TC, HDL, triglycerides, CRP, insulin, fasting glucose, HOMA-IR, leptin, or ghrelin in breakfast skippers as compared with breakfast consumers (Table 3, Supporting Information Figure S4).
TABLE 3.
Secondary outcomes summary for random-effects meta-analysis of WMD in cardiometabolic parameters in breakfast skippers as compared with breakfast consumers
| Outcome | No. of studies (No. of participants) | WMD | Lower 95% CI | Upper 95% CI | P value | I2, % | Egger P value | Begg P value |
|---|---|---|---|---|---|---|---|---|
| Systolic BP (mmHg) | 2 (69) | −6.30 | −14.73 | 2.14 | 0.14 | 76.1 | — | 0.32 |
| Diastolic BP (mm Hg) | 2 (69) | −2.43 | −5.96 | 1.09 | 0.18 | 0 | — | 0.32 |
| TC (mg/dL) | 3 (92) | 11.57 | −2.91 | 26.05 | 0.12 | 73 | 0.25 | 0.60 |
| HDL (mg/dL) | 3 (92) | 0.58 | −1.37 | 2.53 | 0.77 | 0 | 0.04a | 0.12 |
| LDL (mg/dL) | 3 (92) | 9.24 | 2.18 | 16.30 | 0.01a | 3.2 | 0.16 | 0.12 |
| Triglycerides (mg/dL) | 3 (92) | −0.92 | −12.84 | 10.99 | 0.88 | 0 | 0.40 | 0.60 |
| CRP | 2 (56) | 0.04 | −0.36 | 0.45 | 0.84 | 0 | — | 0.32 |
| Insulin (uIU/mL) | 3 (92) | −0.39 | −1.41 | 0.63 | 0.46 | 0 | 0.49 | 0.60 |
| Fasting glucose (mg/dL) | 3 (92) | −1.49 | −4.37 | 1.39 | 0.31 | 0 | 0.28 | 0.60 |
| HOMA-IR | 3 (92) | −0.27 | −0.73 | 0.19 | 0.25 | 57.2 | 0.71 | 0.60 |
| Leptin (ug/L) | 3 (92) | −1.93 | −4.70 | 0.74 | 0.15 | 32.7 | 0.42 | 0.60 |
| Ghrelin (pg/mL) | 2 (56) | −12.16 | −109.80 | 85.47 | 0.81 | 39 | — | 0.32 |
statistically significant at P < 0.05.
—, insufficient number of studies to calculate Egger P value; BP, blood pressure; CRP, C-reactive protein; HDL, high-density lipoprotein cholesterol; HOMA-IR, homeostatic model assessment of insulin resistance; LDL, low-density lipoprotein cholesterol; No., number; TC, total cholesterol; WMD, weighted mean difference.
Figure 2.
Random-effects model meta-analysis for changes in (A) HDL and (B) LDL concentrations in milligrams per deciliter from RCTs comparing breakfast skipping versus breakfast consumption. Conversion factor: TC from millimoles per liter to milligrams per deciliter: 38.67. Closed rectangles and horizontal bars represent the overall estimates (difference of means) and 95% CIs for individual studies. Diamonds represent the overall estimate combining all the studies. HDL, high-density lipoprotein cholesterol; ID, identifier; LDL, low-density lipoprotein cholesterol; RCT, randomized controlled trial; TC, total cholesterol; WMD, weighted mean difference.
Publication bias
The small number of studies limits the evaluation of publication bias. For the primary analysis of body weight, neither the Egger nor Begg test results for funnel plot asymmetry were significant, with P values of 0.72 and 0.88, respectively. The funnel plot showed a fairly symmetric distribution of the studies (Supporting Information Figure S5). Egger and Begg test results are reported for all outcomes in Tables 2–3, with the respective funnel plots for statistically significant values available in Supporting Information Supporting Information Figure S5-S6. These results are provided for reference but cannot rule out publication bias.
Secondary analysis
We conducted a secondary analysis using a fixed-effect inverse-variance approach. This model revealed consistent body weight changes (−0.55 kg [95% CI: −0.96 to −0.13], P = 0.01) and increased LDL (9.30 mg/dL [95% CI: 2.38 to 16.23], P = 0.008) in breakfast skippers as compared with breakfast consumers. It also found significantly decreased systolic blood pressure (−5.12 mm Hg [95% CI: −8.98 to −1.25], P = 0.04) and increased TC (15.54 mg/dL [95% CI: 8.75 to 22.33], P < 0.001) in breakfast skippers compared with breakfast consumers. There were no other statistically significant findings using the fixed-effect approach.
Two studies had multiple breakfast consumption arms. The primary analyses evaluated the impact of breakfast skipping, so multiple breakfast groups, irrespective of meal composition, were combined into a single comparator arm. We also ran analyses that compared each breakfast consumption group individually with the breakfast skipping group in the multiple breakfast consumption arm studies (Supporting Information Table S1-S2) Statistically significant findings included body weight (−0.60 kg [95% CI: −1.12 to −0.09], P = 0.02), TC (13.11 mg/dL [95% CI: 0.93 to 25.30], P = 0.04), LDL (12.07 mg/dL [95% CI: 5.96 to 18.17], P = 0.04), and insulin (−0.89 uIU/mL [95% CI: −1.75 to −0.03], P = 0.04).
Stratified analysis
Four stratified analyses were performed using random-effects models: studies in populations with normal weight, overweight/obesity, and habitual breakfast consumption, and trials lasting ≥ 8 weeks (Supporting Information Tables S3-S5). Insufficient data were available for studies conducted in nonhabitual breakfast consumers.
There were 2 studies of adults with normal weight, which did not reveal any significant differences in body composition parameters between breakfast skippers and breakfast consumers (Supporting Information Table S3). Cardiometabolic parameters were only reported in one of the studies, so subgroup analysis of cardiometabolic parameters was not performed in the group of participants with normal weight.
Five studies were performed in participants with overweight/obesity. No body composition parameters were significantly different between groups. Only 2 of these 5 studies in populations with overweight/obesity reported cardiometabolic outcomes. Breakfast skippers, as compared with breakfast consumers, had significantly different LDL levels (10.51 mg/dL, P = 0.03; I2 = 25.7%; P heterogeneity = 0.25) and HOMA-IR (−0.56, P = 0.01; I2 = 0%; P heterogeneity = 0.65) (Supporting Information Table S4).
Two studies were conducted in participants who habitually ate breakfast, with the Schlundt et al. (27) trial also reporting stratified results for habitual breakfast consumers and skippers. Among those who habitually skipped breakfast, there were no significantly different body composition parameters between those assigned to skip breakfast as compared with those who were assigned to consume breakfast (Supporting Information Table S3). No cardiometabolic parameters were reported in studies of habitual breakfast skippers.
Three trials had a duration of at least 8 weeks. Body weight was the only body composition outcome reported by all 3 trials and was not significant in breakfast skippers as compared with breakfast consumers (−0.04 kg, P = 0.94; I2 = 0%). BMI and percent body fat were reported in 2 studies and were not significantly different between groups (Supporting Information Table S5).
Discussion
This systematic review and meta-analysis of 7 RCTs confirms prior data demonstrating that breakfast skipping results in modest weight loss and is the first, to our knowledge, to evaluate the impact of breakfast skipping on several cardiometabolic parameters. Our findings demonstrate that breakfast skipping compared with breakfast consumption over the short term (4 to 16 weeks) results in approximately 0.54 kg, or 1.19 pounds, of weight loss without significant changes in other body composition parameters. Compared with breakfast consumers, LDL increased by 9.24 mg/dL in those who skipped breakfast. The present work provides the most updated and comprehensive estimates of the effects of breakfast skipping on body composition and other cardiometabolic risk factors in adults over a minimum duration of 4 weeks.
Although systematic reviews of observational studies typically find improved weight control with breakfast consumption (9,10), our results are consistent with a recent meta-analysis of RCTs of breakfast consumption on weight loss and energy consumption by Sievert et al. (15), who found that breakfast skipping yielded an additional 0.44 kg of weight loss as compared with breakfast consumption. Interestingly, none of the other body composition parameter changes were statistically significant, including a nonsignificant decrease in lean mass and increase in percent body fat.
Recommendations for consuming breakfast for weight management are generally based on the belief that breakfast consumption could promote lasting satiating effects or decreased energy intake across the day. A 2018 review article found positive to neutral support that short-term breakfast consumption improved appetite control, satiety, and postprandial energy expenditure, particularly when it included solid foods with larger amounts of protein (≥ 30 g protein/meal) and energy (≥ 350 kcal/meal) (30).
The effects of breakfast consumption on total daily energy intake has also been explored. Although a short RCT found significantly reduced energy intake (~90 kcal/d) overall on days when participants consumed breakfast compared with when they skipped it (31), a meta-analysis of RCTs found that breakfast consumers had higher total daily energy intake (~260 kcal/d) than breakfast skippers (15). Unfortunately, satiety and energy intake could not be evaluated in our meta-analysis of longer RCTs. When evaluating leptin and ghrelin levels, no statistically significant differences were observed between breakfast skippers and consumers, despite breakfast skippers losing more weight than breakfast consumers.
While it appears that longer-term RCTs (≥ 4 weeks) of breakfast skipping did not affect leptin or ghrelin, longer-term RCTs that include the assessment of ingestive behavior and other physiological mechanisms linking breakfast patterns with weight management are needed.
Another possible explanation for the seemingly protective effect of breakfast on body weight is that breakfast consumers display other health-related behaviors. A 2019 Australian observational study found that differences in daily diet intake among cereal breakfast eaters, noncereal breakfast eaters, and breakfast skippers were attributable to different food choices both at breakfast and during the rest of the day (32). Furthermore, in a 10-year prospective study, the protective effect of breakfast consumption on the prevention of weight gain was partially explained by fiber and nutrient intake (6). This supports the hypotheses that overall dietary quality and possibly other socioeconomic or health-related behaviors, such as physical activity (33), may be responsible for the protective association seen in observational studies of breakfast consumers.
Breakfast quality could also play a key role. However, breakfast quality in the trials included in this meta-analysis varied significantly. Four studies allowed participants to choose whatever breakfast foods they wanted (12–14,29), with three of them providing a nutrition pamphlet that included healthy choices (12–14). The other 3 studies provided cereal (27), corn flakes or oatmeal (20), and milk with cereal or an egg-based option (waffle, pancake, or burrito) with a pork or ham product for breakfast (28). The heterogeneous breakfast qualities across trials limits our ability to assess the effects of breakfast quality on body weight and cardiometabolic parameters.
Our data confirm that neither skipping nor consuming breakfast alone, without the context of overall caloric restriction or improvements in diet quality, is an effective strategy for clinically significant weight loss for most individuals. Long-term RCTs would be valuable to further explore these aforementioned hypotheses. Any recommendations requiring the inclusion or exclusion of the breakfast meal for weight loss should also consider the quality of breakfast, the composition and quality of the overall diet, and other socioeconomic factors and lifestyle behaviors, such as smoking, sleep, and physical activity.
Although other studies have reviewed the impact of meal frequency on cardiometabolic parameters (25), this is the first meta-analysis, to our knowledge, to evaluate the effects of breakfast skipping in RCTs. It is important to note that cardiometabolic parameters were secondary outcomes of this analysis, and, unfortunately, these outcomes were not measured in the majority of trials that were analyzed. We found that breakfast skipping, as compared with breakfast consumption, led to significant increases in LDL (9.24 mg/dL). Although TC showed a nonsignificant increase of 11.57 mg/dL (P = 0.12) in the primary random-effects model, it was statistically significant when using a fixed effects model (15.54 mg/dL, P < 0.001) and when using individual breakfast comparator arms (13.11, P = 0.04). The increase in TC may still be clinically relevant. However, it is imperative that these findings be interpreted cautiously, as they are based on only 3 studies with 92 total participants.
Despite the small sample size, these observations are consistent with a 2005 RCT in lean women that found significant increases in TC and LDL after 2 weeks of skipping breakfast (31). Short-term fasting studies (1 to 7 days of fasting), have also demonstrated increases in TC, LDL (34), and HDL (35). However, refeeding the participants in the Horne et al. (35) study after a 1-day fast attenuated the changes in these variables. Explanations for these changes induced by fasting include increased lipid extraction from endogenous stores, decreases in liver lipoprotein uptake, or a combination of the 2 (36).
Macronutrient differences and specific food choices between breakfast groups may also be responsible for the increases in LDL observed. For example, observational studies in the United States, Spain, and the United Kingdom have consistently found higher total fat intake associated with individuals who skip breakfast (37–40). Given that not all fats are created equal, the type of fat that was substituted or the quality of the carbohydrate that was eaten or replaced could dictate whether or not a positive health impact is observed.
Unfortunately, the limited data available in this analysis preclude analyzing the role that altered dietary macronutrient composition may play with regard to the LDL seen in the breakfast skipping group. Similarly, the heterogeneity and lack of controlled breakfast-meal makeup across studies inhibited our ability to compare the quality of foods included in the breakfast meals and overall diet quality. These differences may also have contributed to the change in body weight and LDL observed between breakfast skippers and consumers.
The observed increases in LDL and trend of increased TC may help explain findings in longitudinal studies of breakfast skipping and cardiovascular disease (16–18), as LDL is a leading factor for causing atherosclerotic cardiovascular disease (41). For example, multiple prospective studies have demonstrated increased risks of cardiovascular disease in breakfast skippers, with hazard ratios or relative risks ranging from 1.14 to 1.27 (16,18). Additionally, a 2019 prospective study of 6,550 adults followed for up to 23 years, found an increased risk of cardiovascular mortality, with a hazard ratio of 1.87 for breakfast skippers compared with those consuming breakfast (17).
However, given that only 3 studies in this meta-analysis reported LDL as an outcome, this finding should be interpreted cautiously. No effects were seen in blood pressure, HDL, triglycerides, CRP, insulin, HOMA-IR, leptin, or ghrelin in the primary analysis. Further research is warranted investigating the effects of breakfast skipping on cardiovascular health, especially focusing on breakfast quality.
Strengths of this study include a robust systematic search that considered all studies published since database inception in any language. By mandating a minimum duration of 4 weeks for RCTs, we allowed time for weight loss and cardiometabolic changes to occur, and potentially begin to stabilize. Restricting our analysis to RCTs allowed for a causal interpretation of the findings and aided in controlling for other confounders invariably present in observational study designs.
This study was limited by the relatively small amount of data that was available. Only 7 studies met the criteria for a total of 425 participants. Furthermore, body weight was the only measure reported in all trials. Although other body composition parameters were reported in at least 5 trials, cardiometabolic parameters were only reported in 2 to 3 studies, depending on the parameter. This greatly limits the interpretability of many of the secondary results.
Although the 4-week-minimum-duration inclusion criterion was chosen on the basis of limited evidence, there is no consensus statement on the minimum duration required to achieve weight loss. This duration seemed sufficient to demonstrate weight changes, as the stratified analyses of trials lasting ≥ 8 weeks demonstrated a nonsignificant weight loss of 0.04 kg in breakfast skippers compared with breakfast consumers. Given that weight and cardiometabolic risk factors are important for long-term health, it is not possible to extrapolate how they may vary over longer periods of time with continued breakfast skipping/consumption. Furthermore, skipping breakfast is a complex behavior that inevitably leads to other dietary alterations that might be responsible for these results. In an attempt to be more comprehensive, we included a number of potentially relevant outcome variables and cannot rule out the possibility of a type 1 error. Lastly, there was inconsistency in the studies analyzed regarding breakfast food selection, quality, and quantity. This makes generalizations difficult and precludes giving advice on the types of breakfast food to consume or not consume.
Further research is needed to explore the impact of breakfast skipping in specific populations, including specific BMI categories, older adults, and those with underlying cardiometabolic diseases. Other possible mediating variables, including sex, fitness level, socioeconomic status, race/ethnicity, and use of medications/caffeine/alcohol, also need to be evaluated. Controlled studies of longer duration are needed to elucidate the magnitude and persistence of body composition and cardiometabolic markers changes over time. Finally, interventions should consider the impact of breakfast on overall diet composition, breakfast food quality, and alternative intermittent fasting approaches when examining the effects of breakfast consumption on body weight and cardiovascular risk factors.
Conclusion
Findings from the present systematic review and meta-analysis of RCTs of adults lasting at least 4 weeks showed that breakfast skipping led to a greater reduction in body weight as compared with breakfast consumption. Breakfast skippers had significantly increased LDL compared with breakfast consumers, although this finding should be interpreted cautiously, as less than half of the studies included in this meta-analysis reported lipid outcome measures. No other body composition or cardiometabolic parameters were significantly different between the groups. Although breakfast skipping had a modest impact on weight loss in the short term, its long-term impact on body composition and cardiometabolic health requires further study. Future interventions focusing on food quality, specific macronutrient profiles, and restricted feeding intervals may provide additional insight into more optimal eating patterns for weight control, cardiometabolic health, and public health purposes.
Supplementary Material
Study Importance.
SWhat is already known?
-
►
Prospective studies have demonstrated inverse associations between consuming breakfast and weight gain. However, randomized controlled trials (RCTs) have shown equivocal results, with a recent meta-analysis finding modest weight loss in breakfast skippers as compared with breakfast consumers.
-
►
Prospective studies suggest that skipping breakfast is associated with worse cardiometabolic health, and several RCTs have shown that skipping breakfast leads to increases in HDL, LDL, and total cholesterol.
What does this study add?
-
►
Our findings confirm that modest weight loss occurs when skipping breakfast without significant changes in other body composition parameters and that LDL is significantly increased in breakfast skippers as compared with breakfast consumers.
How might these results change the direction of research?
-
►
Further studies focusing on food and breakfast quality, specific macronutrient profiles, and restricted feeding intervals are needed to provide additional insight into more optimal eating patterns for weight control and cardiometabolic health.
-
►
The increase in LDL warrants further investigation with larger controlled trials.
Acknowledgments
The authors thank all of the study authors for their assistance and James Betts, Enhad Chowdhury, Emily Dhurandar, and Heather Leidy, as well as their co-authors. We recognize Kenneth Verboven and Dominique Hansen (Rehabilitation Research Centre, Biomedical Research Unit, Faculty of Rehabilitation Sciences, Hasselt University, Diepenbeek, Belgium) for their willingness to share their data, although none of the data or materials derived from the data was used in this analysis. We recognize the guidance provided by Heather Baer and the statistical support provided by the Harvard. T.H. Chan Biostatistics Student Consulting Center.
Funding agencies: No grants or funding was received for this manuscript. MIC is supported by the NIH National Heart, Lung, and Blood Institute (K01HL141535). MG-F is supported by American Diabetes Association grant 1-18-PMF-029.
Footnotes
Disclosure: The authors declared no conflict of interest.
Supporting information: Additional Supporting Information may be found in the online version of this article.
References
- 1.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016 NCHS Data Brief, no. 288. Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 2.Jensen MD, Ryan DH, Apovian CM, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. J Am Coll Cardiol 2014;63:2985–3023. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Blaha MJ, Chiuve SE, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Betts JA, Chowdhury EA, Gonzalez JT, Richardson JD, Tsintzas K, Thompson D. Is breakfast the most important meal of the day? Proc Nutr Soc 2016;75:464–474. [DOI] [PubMed] [Google Scholar]
- 6.van der Heijden AA, Hu FB, Rimm EB, van Dam RM. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity (Silver Spring) 2007;15:2463–2469. [DOI] [PubMed] [Google Scholar]
- 7.Wyatt HR, Grunwald GK, Mosca CL, Klem ML, Wing RR, Hill JO. Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obes Res 2002;10:78–82. [DOI] [PubMed] [Google Scholar]
- 8.Deshmukh-Taskar P, Nicklas TA, Radcliffe JD, O’Neil CE, Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr 2013;16:2073–2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mesas AE, Munoz-Pareja M, Lopez-Garcia E, Rodriguez-Artalejo F. Selected eating behaviours and excess body weight: a systematic review. Obes Rev 2012;13:106–135. [DOI] [PubMed] [Google Scholar]
- 10.Horikawa C, Kodama S, Yachi Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med 2011;53:260–267. [DOI] [PubMed] [Google Scholar]
- 11.Dashti HS, Merino J, Lane JM, et al. Genome-wide association study of breakfast skipping links clock regulation with food timing. Am J Clin Nutr 2019;110:473–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr 2014;100:539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chowdhury EA, Richardson JD, Holman GD, Tsintzas K, Thompson D, Betts JA. The causal role of breakfast in energy balance and health: a randomized controlled trial in obese adults. Am J Clin Nutr 2016;103:747–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dhurandhar EJ, Dawson J, Alcorn A, et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014;100:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sievert K, Hussain SM, Page MJ, et al. Effect of breakfast on weight and energy intake: systematic review and meta-analysis of randomised controlled trials. BMJ 2019;364:l42. doi: 10.1136/bmj.l42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cahill LE, Chiuve SE, Mekary RA, et al. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation 2013;128:337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rong S, Snetselaar LG, Xu G, et al. Association of skipping breakfast with cardiovascular and all-cause mortality. J Am Coll Cardiol 2019;73:2025–2032. [DOI] [PubMed] [Google Scholar]
- 18.Kubota Y, Iso H, Sawada N, Tsugane S; JPHC Study Group. Association of breakfast intake with incident stroke and coronary heart disease: the Japan public health center-based study. Stroke 2016;47:477–481. [DOI] [PubMed] [Google Scholar]
- 19.Smith KJ, Gall SL, McNaughton SA, Blizzard L, Dwyer T, Venn AJ. Skipping breakfast: longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr 2010;92:1316–1325. [DOI] [PubMed] [Google Scholar]
- 20.Geliebter A, Astbury NM, Aviram-Friedman R, Yahav E, Hashim S. Skipping breakfast leads to weight loss but also elevated cholesterol compared with consuming daily breakfasts of oat porridge or frosted cornflakes in overweight individuals: a randomised controlled trial. J Nutr Sci 2014;3:e56. doi: 10.1017/jns.2014.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bonnet J, Cardel M, Cellini J, Guasch-Ferré M, Hu FB. The impact of breakfast skipping on body composition and cardiometabolic risk factors: a systematic review and meta-analysis. PROSPERO identifier: CRD42018110858. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42018110858. Published October 18, 2018. [Google Scholar]
- 23.Wadden TA, Foster GD, Wang J, et al. Clinical correlates of short- and long-term weight loss. Am J Clin Nutr 1992;56(1 suppl):271S–274S. [DOI] [PubMed] [Google Scholar]
- 24.Nackers LM, Ross KM, Perri MG. The association between rate of initial weight loss and long-term success in obesity treatment: does slow and steady win the race? Int J Behav Med 2010;17:161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.St-Onge MP, Ard J, Baskin ML, et al. ; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; Stroke Council. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 2017;135:e96–e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Neil CE, Byrd-Bredbenner C, Hayes D, Jana L, Klinger SE, Stephenson-Martin S. The role of breakfast in health: definition and criteria for a quality breakfast. J Acad Nutr Diet 2014;114(12 suppl):S8–S26. [DOI] [PubMed] [Google Scholar]
- 27.Schlundt DG, Hill JO, Sbrocco T, Pope-Cordle J, Sharp T. The role of breakfast in the treatment of obesity: a randomized clinical trial. Am J Clin Nutr 1992;55: 645–651. [DOI] [PubMed] [Google Scholar]
- 28.Leidy HJ, Hoertel HA, Douglas SM, Higgins KA, Shafer RS. A high-protein breakfast prevents body fat gain, through reductions in daily intake and hunger, in “breakfast skipping” adolescents. Obesity (Silver Spring) 2015;23:1761–1764. [DOI] [PubMed] [Google Scholar]
- 29.LeCheminant GM, LeCheminant JD, Tucker LA, Bailey BW. A randomized controlled trial to study the effects of breakfast on energy intake, physical activity, and body fat in women who are nonhabitual breakfast eaters. Appetite 2017;112:44–51. [DOI] [PubMed] [Google Scholar]
- 30.Gwin JA, Leidy HJ. A review of the evidence surrounding the effects of breakfast consumption on mechanisms of weight management. Adv Nutr 2018;9:717–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farshchi HR, Taylor MA, Macdonald IA. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr 2005;81:388–396. [DOI] [PubMed] [Google Scholar]
- 32.Fayet-Moore F, McConnell A, Cassettari T, Petocz P. Breakfast choice is associated with nutrient, food group and discretionary intakes in Australian adults at both breakfast and the rest of the day. Nutrients 2019;11:E175. doi: 10.3390/nu11010175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clayton DJ, James LJ. The effect of breakfast on appetite regulation, energy balance and exercise performance. Proc Nutr Soc 2016;75:319–327. [DOI] [PubMed] [Google Scholar]
- 34.Sävendahl L, Underwood LE. Fasting increases serum total cholesterol, LDL cholesterol and apolipoprotein B in healthy, nonobese humans. J Nutr 1999;129: 2005–2008. [DOI] [PubMed] [Google Scholar]
- 35.Horne BD, Muhlestein JB, Lappé DL, et al. Randomized cross-over trial of short-term water-only fasting: metabolic and cardiovascular consequences. Nutr Metab Cardiovasc Dis 2013;23:1050–1057. [DOI] [PubMed] [Google Scholar]
- 36.Horne BD, Muhlestein JB, Anderson JL. Letter by Horne et al. regarding article, “Prognostic Value of Fasting Versus Nonfasting Low-Density Lipoprotein Cholesterol Levels on Long-Term Mortality: Insight From the National Health and Nutrition Survey III (NHANES-III)”. Circulation 2015;131:e472. doi: 10.1161/CIRCULATIONAHA.114.012891 [DOI] [PubMed] [Google Scholar]
- 37.O’Neil CE, Nicklas TA, Fulgoni VL III. Nutrient intake, diet quality, and weight/adiposity parameters in breakfast patterns compared with no breakfast in adults: National Health and Nutrition Examination Survey 2001–2008. J Acad Nutr Diet 2014;114(12 suppl):S27–S43. [DOI] [PubMed] [Google Scholar]
- 38.Drewnowski A, Rehm CD, Vieux F. Breakfast in the United States: food and nutrient intakes in relation to diet quality in national health and examination survey 2011–2014. A Study from the International Breakfast Research Initiative. Nutrients 2018;10:1200. doi: 10.3390/nu10091200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ruiz E, Avila JM, Valero T, Rodriguez P, Varela-Moreiras G. Breakfast consumption in Spain: patterns, nutrient intake and quality. Findings from the ANIBES study, a study from the International Breakfast Research Initiative. Nutrients 2018;10:1324. doi: 10.3390/nu10091324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gaal S, Kerr MA, Ward M, McNulty H, Livingstone MBE. Breakfast consumption in the UK: patterns, nutrient intake and diet quality. A study from the International Breakfast Research Initiative Group. Nutrients 2018;10:999. doi: 10.3390/nu100;80:999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Euro Heart J 2017;38:2459–2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.