To the Editor: Information on the natural history of asymptomatic infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remains scarce.1-3 The outbreak of coronavirus disease 2019 (Covid-19) on the cruise ship Diamond Princess led to 712 persons being infected with SARS-CoV-2 among the 3711 passengers and crew members, and 410 (58%) of these infected persons were asymptomatic at the time of testing (see the Supplementary Appendix, available with the full text of this letter at NEJM.org).4,5 Here, we report the natural history of asymptomatic SARS-CoV-2 infection in part of this cohort.
A total of 96 persons infected with SARS-CoV-2 who were asymptomatic at the time of testing, along with their 32 cabinmates who tested negative on the ship, were transferred from the Diamond Princess to a hospital in central Japan between February 19 and February 26 for continued observation. Clinical signs and symptoms of Covid-19 subsequently developed in 11 of these 96 persons, a median of 4 days (interquartile range, 3 to 5; range, 3 to 7) after the first positive polymerase-chain-reaction (PCR) test, which meant that they had been presymptomatic rather than asymptomatic. The risk of being presymptomatic increased with increasing age (odds ratio for being presymptomatic with each 1-year increase in age, 1.08; 95% confidence interval [CI], 1.01 to 1.16). Eight of 32 cabinmates with a negative PCR test on the ship had a positive PCR test within 72 hours after arrival in the hospital but remained asymptomatic. In total, data on 90 persons with asymptomatic SARS-CoV-2 infection, defined as persons who were asymptomatic at the time of the positive PCR test and remained so until the resolution of infection (as determined by two consecutive negative PCR tests), were available for analysis (Fig. S1 in the Supplementary Appendix).
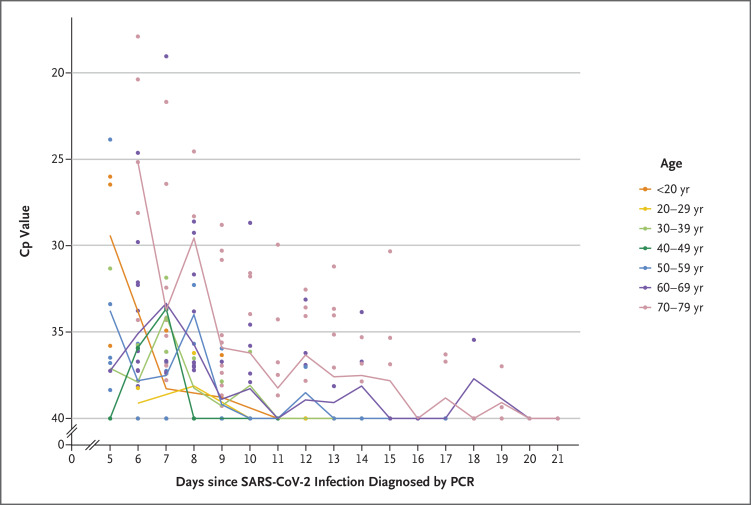
The group of persons with asymptomatic SARS-CoV-2 infection consisted of 58 passengers and 32 crew members, with median age of 59.5 years (interquartile range, 36 to 68; range, 9 to 77). A total of 24 of these persons (27%) had coexisting medical conditions, including hypertension (in 20%) and diabetes (9%). The first PCR test at the hospital was performed a mean of 6 days after the initial positive PCR test on the ship. The median number of days between the first positive PCR test (either on the ship or at the hospital) and the first of the two serial negative PCR tests was 9 days (interquartile range, 6 to 11; range, 3 to 21), and the cumulative percentages of persons with resolution of infection 8 and 15 days after the first positive PCR test were 48% and 90%, respectively. The risk of delayed resolution of infection increased with increasing age (mean delay in resolution for an increase in age from 36 to 68 years, 4.41 days; 95% CI, 2.28 to 6.53) (Figure 1).
Figure 1. Crossing-Point Values in RT-PCR Testing of Asymptomatic Persons with SARS-CoV-2 Infection.
Included in the analysis are persons who had at least one positive polymerase-chain-reaction (PCR) test for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the hospital. With fluorescence-based real-time reverse-transcriptase PCR (RT-PCR), the number of cycles at which the fluorescence signal from amplification exceeds the background fluorescence level is determined as the crossing point (Cp), threshold cycle, or other measures by different instrument manufacturers. A lower value correlates with a higher copy number of the target nucleotide sequence.
In this cohort, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection. The time to the resolution of infection increased with increasing age.
Supplementary Appendix
Disclosure Forms
This letter was published on June 12, 2020, at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med 2020;382:2081-2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020;323:1406-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility — King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Field briefing: Diamond Princess COVID-19 cases, 20 Feb update. Tokyo: National Institute of Infectious Diseases, February 21, 2020 (https://www.niid.go.jp/niid/en/2019-ncov-e/9417-covid-dp-fe-02.html).
- 5.Ministry of Health, Labour and Welfare. Official report on the cruise ship Diamond Princess. March 5, 2020. (https://www.mhlw.go.jp/stf/newpage_09997.html).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.