Abstract
Background:
Despite the growing interest in the development of emergency care systems and emergency medicine (EM) as a specialty globally, there still exists a significant gap between the need for and the provision of emergency care by specialty trained providers. Many efforts to date to expand the practice of EM have focused on programs developed through partnerships between higher- and lower-resource settings.
Objective:
To systematically review the literature to evaluate the composition of EM training programs in low- and middle-income countries (LMICs) developed through partnerships.
Methods:
An electronic search was conducted using four databases for manuscripts on EM training programs – defined as structured education and/or training in the methods, procedures, and techniques of acute or emergency care – developed through partnerships. The search produced 7702 results. Using a priori inclusion and exclusion criteria, 94 manuscripts were included. After scoring these manuscripts, a more in-depth examination of 26 of the high-scoring manuscripts was conducted.
Findings:
Fifteen highlight programs with a focus on specific EM content (i.e. ultrasound) and 11 cover EM programs with broader scopes. All outline programs with diverse curricula and varied educational and evaluative methods spanning from short courses to full residency programs, and they target learners from medical students and nurses to mid-level providers and physicians. Challenges of EM program development through partnerships include local adaptation of international materials; addressing the local culture(s) of learning, assessment, and practice; evaluation of impact; sustainability; and funding.
Conclusions:
Overall, this review describes a diverse group of programs that have been or are currently being implemented through partnerships. Additionally, it highlights several areas for program development, including addressing other topic areas within EM beyond trauma and ultrasound and evaluating outcomes beyond the level of the learner. These steps to develop effective programs will further the advancement of EM as a specialty and enhance the development of effective emergency care systems globally.
Introduction
The World Health Assembly Resolutions 60.22, 68.15, and 72.16 all highlight the significant gap between the need for and the provision of emergency care that currently exists globally [1,2,3]. Low-income countries carry more than three times the burden of disease for emergency conditions in terms of disability-adjusted life years (DALYs) than do high-income countries, while emergency usage rates in low-income countries are 3% of those of high-income countries [4]. As more and more countries experience population and economic growth, globalization, rapid urbanization, and progression through the demographic transition, the demand for strong systems to address both the care and prevention of trauma, communicable diseases, and non-communicable diseases will only continue to grow.
Emergency care systems – which broadly include the provision of both acute and emergency care and services – are comprised of at least five major components: individual and community capacity, preparedness, and resilience; delivery of appropriate out-of-hospital care by laypersons; a means of access to formal services by the public; transport and/or delivery of appropriate pre-hospital care by trained professionals; and clinical care and referral networks [5,6]. The specialty of emergency medicine (EM) – a unique discipline with a well-defined and universal set of technical and cognitive skills – has developed over the last 50 years to lead the provision of clinical care by training not only physicians, but also other healthcare personnel at all levels. Additionally, the specialty of EM also serves as a guide for the overall development of emergency care systems through a focus on core concepts and strategies aimed at reducing morbidity and mortality of emergent conditions and to provide secondary disease prevention [5,6,7,8,9,10].
Although still a relatively young specialty, EM has been expanding rapidly across the globe, and more than 50 national EM organizations are now members of the International Federation for Emergency Medicine (IFEM) [11]. Although some concepts, such as burden of disease and resource availability, are unique to each local context, the specialty of EM provides a unique opportunity where partnerships can develop to share universal content as well as established resources in education and training relevant to high-resource settings, low-resource settings, or both. To date, the development of EM in many countries has occurred in part because of educational partnerships between nations or regions where one partner has more experience with EM as a specialty. Such partnerships can occur regardless of each country’s income level, but frequently involve partnerships between a high-income country and a low- or middle-income country (LMIC) [12,13,14,15].
Though programs developed from such educational partnerships are increasingly common, there is little to describe their features. One review describes some of the features of training programs in LMICs, but it does not specifically focus on programs resulting from partnerships [16]. Additionally, there is some guidance in the literature as to how to approach the creation of these training programs as well as the overall development of EM, but this information is now outdated and there is little information specific to training and education [17] In this systematic review, we aim to address this gap by highlighting the scope, content, and features of EM programs developed in LMICs through partnerships.
Methods
An electronic search using PubMed, Web of Science, CINAHL, and EMBASE was conducted for all available publications to the date of the search (30 August 2018) without restriction on the scope of the EM content, the training level of the learners (i.e. medical student, nurse, mid-level, physician), or the length of the program (defined here as short duration – up to one month, medium duration – between one month and one year, and long duration – more than one year). The search strings may be found in Supplement 1. We have defined an EM training program as “structured education and/or training in the methods, procedures, and techniques of acute or emergency care”. Inclusion criteria determined a priori were EM training programs developed in the hospital or clinical setting in an LMIC – as defined by the World Bank at the time of the search – and supported by at least one higher-resource international partnership [18]. In-hospital programs were targeted as, in our experience, partners often seek out institutions given the often more familiar workforce and resources as well as the perception that training is likely to have the highest impact in this setting. Manuscripts focusing only on pre-hospital or non-clinical providers were excluded. Manuscripts with a predominant focus on other specialties (i.e. obstetrics/neonatal care and emergency surgery) were excluded. Only manuscripts in English were considered. Systematic reviews and abstracts/posters were excluded. Two reviewers screened each abstract with conflicts resolved after a third review to determine the included manuscripts.
The included manuscripts were then scored by the reviewers in order to select and more closely examine a high-quality subset. Each manuscript was scored by two reviewers and manuscripts with scores differing by more than three points (n = 13) or that differed between reviewers across the threshold for inclusion (n = 19) were reviewed and scored a third time. Scoring (0–2 points for each category) focused on seven areas: manuscript design, overall quality, overall clarity, ethical considerations, significance, description and/or study of program attributes and/or learner or clinical outcomes, and type of providers (Supplement 2). The methods used for this scoring were adapted from methods established in other reviews in the field of global EM [19]. The reviewers’ scores were then averaged for a final score on each manuscript. On review of the average scores, the upper quartile was found to be designated by a score of 12 and above. Manuscripts were then labeled as ‘low-scoring’ (below 12) or ‘high-scoring’ (12 or above).
Abstracts were screened using Covidence (Melbourne, Australia). Statistical analyses (Krippendorf’s alpha for nominal and for interval data for two or more reviewers) were done using Microsoft Excel and Stata/IC v15.1 (StataCorp; College Station, Texas USA). The study was registered and approved by PROSPERO (Registration: CRD42018100194).
Results
The search produced 7702 results. A total of 2433 duplicates were removed prior to screening, leaving 5269 studies to be screened by two reviewers. From this, 105 manuscripts met inclusion criteria for scoring. Of these, four were found to be in high income countries, six could not be obtained, and one was found to be a duplicate, leaving 94 manuscripts in the final analysis (Figure 1). Programs in 42 countries are represented in these manuscripts (Figure 2).
Figure 1.
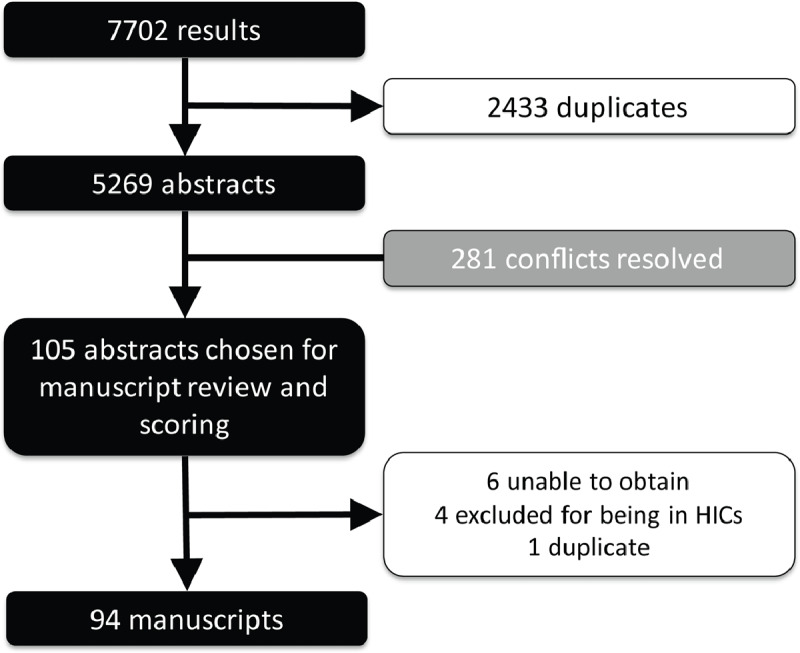
PRISM chart.
Figure 2.
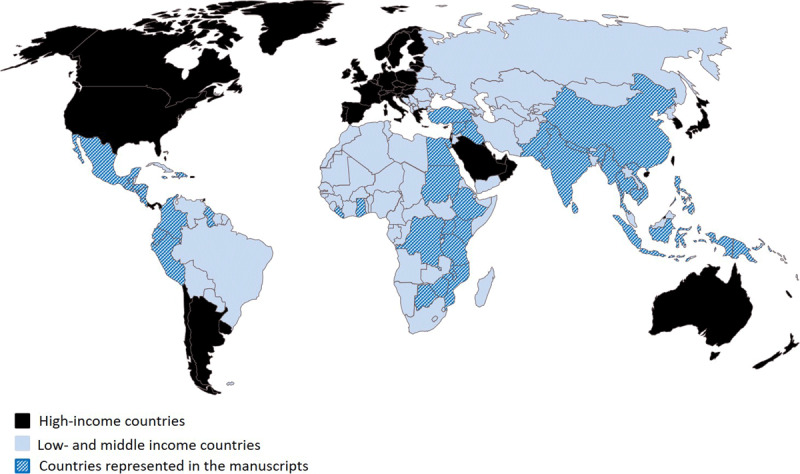
Low- and middle-income countries with programs highlighted in the 94 abstracts.
Of these manuscripts, 30 focus on EM programs with a broad scope, 18 focus on trauma training, 17 on pediatric training, and 16 on ultrasound training. Most programs focus on physician-learners; however, 17 programs train physicians and nurses together, and 15 train multidisciplinary teams (physicians and/or nurses along with other clinical and non-clinical professionals and/or staff). Additionally, eight programs focus solely on nurses and six on medical students. Finally, more than half of the programs are of short duration. Only three are of medium duration, and 15 are of long duration (Table 1).
Table 1.
Summary of the 94 included manuscripts.
| Characteristics | Number of Manuscripts |
|---|---|
| Content | |
| Broad EM | 30 |
| Trauma | 18 |
| Pediatrics | 17 |
| Ultrasound | 16 |
| Procedures | 5 |
| Pediatric Trauma | 2 |
| Disaster | 2 |
| Toxicology | 1 |
| Neurology | 1 |
| CPR | 1 |
| Maternal and Child Health | 1 |
| Learners | |
| Physicians | 33 |
| Physicians and Nurses | 17 |
| Multidisciplinary* | 15 |
| Nurses | 8 |
| Medical Students | 6 |
| Health Workers | 4 |
| Physician Assistants/Nurse Practitioners | 1 |
| Unspecified | 10 |
| Program Duration | |
| Short (up to 1 month) | 51 |
| Medium (>1 month to 1 year) | 3 |
| Long (>1 year) | 15 |
| Unspecified | 25 |
* Physicians and/or nurses along with other clinical and non-clinical professions and/or staff.
The manuscripts were then scored in order to highlight a high-quality subset. When assessing the inter-rater reliability of the raw scores among the reviewers, the reviewers’ scores agreed +/–2 points 74.7% of the time (Krippendorff’s alpha 0.732). When assessing the inter-rater reliability to distinguish “low-scoring” from “high-scoring” manuscripts, the reviewers agreed 80.0% of the time (Krippendorff’s alpha 0.526). A total 26 manuscripts received an average score of 12 and above.
Overview of High-Scoring Manuscripts
Fifteen of the high-scoring manuscripts focus on seven specific content areas (ultrasound, trauma, pediatrics, pediatric trauma, neurological emergencies, toxicological emergencies). They span the years 2012–2018, are published in twelve journals, and highlight work in thirteen countries (Table 2) [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34]. Eleven of the manuscripts discuss general EM programs. These span the years 1999–2018, are published in 10 different journals, and highlight work in nine countries (Table 3) [35,36,37,38,39,40,41,42,43,44,45]. The components of the eleven manuscripts on broadly focused EM training programs are further highlighted here. Post hoc review of the other 83 included manuscripts demonstrated that results and the conclusions drawn from the 11 high-scoring manuscripts were representative of the larger group.
Table 2.
Overview high-scoring manuscripts on content-specific EM programs.
| First Author | Journal | Year Published | Low-resource Setting | Higher-resource Partner | Learners | General Overview (short: up to 1 month; medium: >1 month to 1 year; long: >1 year) |
|---|---|---|---|---|---|---|
| Becker | Trop Med Int Health | 2017 | Ghana | USA | Physicians | Ultrasound, unspecified duration |
| Cioè-Peña | Trauma | 2017 | El Salvador | USA | Physicians and Nurses | Trauma, short duration |
| Crouse | Pediatr Emerg Care | 2016 | Guatemala | USA | Physicians, Nurses, Medical Students, Others | Pediatrics, short duration |
| Denny | World J Emerg Med | 2018 | Tanzania | USA | Physicians, Students, Others | Ultrasound, short duration |
| Henwood | Trop Med Int Health | 2016 | Rwanda | USA, Canada | Physicians | Ultrasound, short duration |
| Kapoor | Emerg Med J | 2016 | Guatemala | USA | Physicians and Nurses | Pediatric Trauma, short duration |
| Kesinger | Injury | 2014 | Colombia | USA | Physicians | Trauma, unspecified duration |
| Merchant | World J Surg | 2015 | Mozambique | USA | Hospital Personnel, Others | Trauma, short duration |
| McCredie | Int Health | 2018 | Nepal | Canada, UK, USA | Physicians | Neurological Emergencies, short duration |
| Meaney | Resuscitation | 2012 | Botswana | USA | All Healthcare Providers | CPR, short duration |
| Reynolds | AfJEM | 2016 | Tanzania, Mexico | USA | Physicians | Ultrasound, short duration |
| Senarathna | PLoS One | 2013 | Sri Lanka | Australia | Hospital Staff | Toxicological Emergencies, short duration |
| Stolz | Trop Med Int Health | 2015 | Uganda | USA | Nurses | Ultrasound, long duration |
| Tafoya | J Emerg Med | 2017 | Ghana | USA | Physicians | Ultrasound, short duration |
| Wanjiku | AfJEM | 2017 | Kenya | USA | Medical Students | Trauma, short duration |
Table 3.
Overview high-scoring manuscripts on broad EM programs.
| First Author | Journal | Year Published | Low-resource Setting | Higher-resource Partner | Learners | General Overview (short: up to 1 month; medium: >1 month to 1 year; long: >1 year) |
|---|---|---|---|---|---|---|
| Aggarwal | J Emerg Trauma Shock | 2014 | India | USA | Physicians | Comprehensive long residency program |
| Hammerstedt | Ann Emerg Med | 2014 | Uganda | USA | Nurses | Comprehensive long course; development of new provider level |
| Keyes | Ann Emerg Med | 1999 | Costa Rica | USA | Physicians | Comprehensive long residency program |
| Lim | Afr J Health Professions Educ | 2017 | Tanzania | USA, South Africa | Physicians | Comprehensive long residency program |
| Meshkat | BMC Med Educ | 2018 | Ethiopia | Canada | Physicians | Comprehensive long residency program |
| Mahadevan | AEM Educ Train | 2018 | Uganda | USA | Medical Students | Online vs classroom-based training; short course |
| Niyogi | AfJEM | 2015 | Ghana | USA | Physician Assistants | Task-shifting; short course |
| Pean | Ann Global Health | 2015 | Haiti | USA | Medical Students | Bilateral exchange; short course |
| Reynolds | J Public Health Policy | 2012 | Tanzania | USA, Canada, South Africa | Physicians and Nurses | Comprehensive training at multiple levels up to residency program level (medium and long) |
| Rouhani | Int J Emerg Med | 2018 | Haiti | USA | Physicians | Bridging the gap to residency programs; comprehensive medium-duration course |
| Stanley | Confl Health | 2015 | Thailand/Myanmar | UK | Nurses (and medics) | Primary care setting/front line providers; short course |
Broadly-focused EM Training Programs: Program Components
Participants include nurses (two programs), medical students (two programs), physician assistants (one program), physicians (five programs), and nurses and physicians together (one program). All of the manuscripts describe all or a subset of the following components: goals/objectives, program certification/recognition, curriculum outline/content, methods of assessment, funding, logistics, educational resources, outcomes, and challenges (Table 4).
Table 4.
Program components from the selected manuscripts on broad EM programs.
| First Author | Goals and Objectives | Certification/Recognition | Curriculum Outline/Content | Methods of Assessment | Funding | Logistics | Educational Resources | Outcomes | Challenges |
|---|---|---|---|---|---|---|---|---|---|
| Aggarwal | To provide guidelines for EM curricula in India – residency and medical student | Formal residency training | Core topics and required procedures for residents outlined; off-service rotations (minimum two weeks); medical student rotation (one month); no specific academic activities for medical students; required Casualty (two weeks) or EM (four weeks) posting during internship; no specific academic activities for interns; academic activities are department-wide | Thesis requirement; end-of-rotation assessment; log book; final examination with theory and practical components with short-answer questions, short cases, procedural skills (simulated), and OSCEs | Not discussed | Three-year training program; institutional requirements for ED resources and capacity and EM instructors defined | Calls for re-organization/re-structuring of existing resources; lists commonly used books and journals; reports essential list for departmental library | Clear requirements for institutions for the practice of and training in EM | Ongoing conflict and confusion with other specialty degrees such as trauma and surgery and critical care |
| Hammerstedt | To deliver emergency care through non-physician providers (Emergency Care Practitioners, or ECPs) in rural, low-resource settings | Emergency Care Practitioner certification | Graduated clinical and educational responsibilities; research and quality improvement requirements; weekly conferences comprised of didactic lectures, simulation, and procedural skill laboratories First year (Junior ECP) – 40 hours per week in beside learning; three hours of conference per week Second year (Senior ECP) – lead the junior-level conferences; present morbidity and mortality lectures; bimonthly CME classes on topics such as teaching | Intermittent quizzes and final written and oral examinations; procedure and patient follow-up logs; regular feedback with program director; oral case-based remediation test if needed; regular evaluation by visiting emergency physicians | Non-profit organization (Global Emergency Care) | Two-year program, train-the-trainer model | Core competencies from Uganda’s Medical Education for Equitable Services to All Ugandans and the US’s Accreditation Council for Graduate Medical Education Outcome Project; content developed by global emergency care physicians, the hospital medical superintendent, and faculty from Mbarara University and the Ministry of Health | Emergency care practitioners trained; plans to monitor patient outcomes and to expand to other sites | Tracking outcomes; expansion to other sites; funding; continued international faculty support |
| Keyes | To develop EM as a specialty in Costa Rica | Certificate for the Faculty Preparation Course; formal residency training | Faculty Preparation Course: review of core EM topics and instruction in teaching techniques – two hours on case review and journal club and four hours of lectures as well as clinical rotations (200 hours) and workshops; two-thirds of lectures in flipped classroom format Residency: overlap with the Faculty Preparation Course as well as a preceptor program and weekly grand rounds | Written and oral examinations monthly | Project HOPE, People-to-people Health Foundation and USAID | Faculty Preparation Course on-site by international faculty (one year) followed by the residency program (three years) supported by the first faculty for at least five years; learners included foreign physicians | ACLS, ATLS, PALS; US residency materials adapted to the local setting | 14 graduates from the residency as of 1999 | Attrition; payment for/status of physicians after graduation |
| Lim | To determine the acceptability of small-group learning in EM training | Formal residency training | Initially a lecture-based format in 2010 and redesigned to include small-group learning (40% of the curriculum) in 2014 including case-based seminars, procedure labs, and resuscitation simulations | Described elsewhere – written, oral and practical examinations; quantitative and qualitative survey | Described elsewhere – Abbott Fund Tanzania along with a departmental business plan for financial sustainability | Small groups done weekly (seminars) or 1–2 times per month (procedure labs, simulations) with an instructor-learner ratio of 4-6:1 | Described elsewhere – African Federation for Emergency Medicine; International Federation for Emergency Medicine | Small groups more effective at improving clinical practice and preferred for enjoyment of learning and peer- and instructor-relationship building; preferred by learners with more experience | Novel type of learning; some sessions remain too “lecture-like”; relationship building may be difficult across learner levels |
| Meshkat | To develop and deliver comprehensive EM residency training; specific objectives outlined in the manuscript | Formal residency training | Clinical, Clinical Epidemiology, and EM Administration streams; didactics (separated into blocks), beside teaching, simulation, procedural sessions, and journal club; three half days a week for three months of the year; off-service rotations; formal faculty-resident mentorship program; monthly video conferencing | Session and rotation evaluations; written and practical examinations | University-based funding; Grand Challenges Canada; International Development Research Centre; hospital-based funding | Three-year program with annually repeating junior lecture series and bi-annually repeating senior series; three one-month teaching trips by visiting faculty/senior residents; briefings for visiting faculty; curriculum co-director oversight | Core content based on facility assessment, learner needs assessment, and evaluation of disease burden; free and open-access EM-specific materials listed; University of Toronto postgraduate medical education documents used to develop evaluation methods | The program is in its seventh year as of 2018 with 34 graduates, 20 working in EDs throughout Ethiopia, and 25 modules published online | Development of content by outside experts leads to discordance with local practice and resources; the program was time and resource-intensive in first three years; gaps in visiting faculty led to low morale; internet connection with teleconferencing occasionally poor |
| Mahadevan | To determine differences in knowledge acquisition between online and classroom-based teaching on EM concepts | None | 20 modules; 10–15-minute videos or in-person teaching; case-based | Multiple choice and free-response questions | University-based grant | The online course was offered during 10 weeks of the academic year and the classroom-based course was completed over one week during the school break | Novel course developed by Stanford physicians; clips from the show ER | Both groups improved their scores on the post-test with no significant difference overall between the two groups | High numbers of late enrollees and attrition, especially in online course; the online group post-test was delayed by three months |
| Niyogi | To increase knowledge and to allow for task-shifting in the delivery of emergency care by teaching physician assistants (PAs) to identify and stabilize patients with acute conditions; focus on ABCs | In-service training in the Ghana Health Service | Didactic lectures, problem- and case-based small group sessions, skill stations, simulations, laminated algorithms, and a tabletop mass casualty incident exercise; initial training of trainers and supervision of initial trainings by international faculty | Written testing; observation of learners; case review; simulations | Not described | Nine-day trainer training with a refresher six months later; five-day in-service trainings led by trainers in groups of 2–3 | ABCCC approach from the Integrated Management of Adolescent and Adult Illnesses and the Integrated Management of Childhood Illnesses; Ghana Standard Treatment Guidelines | All post-test scores improved from pre-test scores; the trainer refresher pre-test scores fell nearly to initial pre-test levels, but regional pre-test refresher scores stayed relatively high; 22 initial senior trainers, 39 enrolled in initial regional courses | Decay in knowledge over time; minimal differences in knowledge between trainers and trainees; resource limitations at non-training sites; scope of practice limitations for PAs; lack of familiarity with leading/facilitating case-based methodologies and simulation; refresher courses delayed too long; inability for trainees to leave clinical requirements for the training |
| Pean | To increase knowledge and confidence in emergency response skills using a near-peer model | BLS certification | BLS (three days); EM Module – lectures and skills sessions (two days) | Written examination and observed practical skills examination; fund of knowledge tests and self-efficacy surveys; one-year follow up survey | Self-funded and/or sponsored by private donations as well as Doctor’s Hospital at Renaissance in Edinburg, Texas, and the Icahn School of Medicine at Mount Sinai in New York, New York | One week annually for two years; student to instructor ratio 3:1; follow up survey given during the second year; lectures in the morning followed by skills sessions in the afternoon | BLS resources supplied by the Regional Emergency Medical Services Council of New York City; STRAKER Translations for translating written material; EM Module from the introductory course at Icahn School of Medicine at Mount Sinai | Improvements in fund of knowledge and self-efficacy test scores | Unexpected scheduling changes; language barrier; difficulty with maintaining continuity and connection among cohorts; high levels of non-completion and absenteeism; difficulties in communicating expectations; limited access to electricity |
| Reynolds | To provide multiple levels of training to provide emergency care | Formal residency training – Master of Medicine track | International faculty with transition to local faculty; competency-based; half of the time is spent on rotations in other specialties | Written multiple choice questions and essay exam; oral case-based exam; observed clinical exam (OSCE) with case presentation; professional performance audits | Abbott Fund Tanzania along with a departmental business plan for financial sustainability | 10-module nursing curriculum; 1-year registrar program; 3-year residency program | African Federation for Emergency Medicine; International Federation for Emergency Medicine | 90% of nurses have completed the program; residency graduates since 2013; credentialed registrars | Differences in scope of practice in low-resource settings – curricula and off-service rotations must be modified accordingly; culture of practice slow to change |
| Rouhani | To address a gap in human resources and knowledge in EM until more physicians are able to complete formal residency programs | Formal certificate with the Ministry of Health and National Medical School | Didactic lectures, simulation, journal club, morbidity and mortality conference, skill sessions clinical supervision, and development and delivery of one lecture; learners comprised of physicians from multiple hospitals; international and national faculty | Attendance of 75%, 180 supervised clinical hours, written pre- and post-test, completed case and procedure log | Course free of charge; participants retained full salary; non-local participants provided food and housing; subsidized in-country expenses for visiting faculty | 6-month course; 96-hour didactic program conducted every other week; eight visiting faculty volunteering 3–4 weeks | Use of established residency resources; ACLS and PALS resources | 11/14 graduates still working in Emergency Departments one year later; average improvement of 15 points between pre- and post-test scores | Frequent turn-over of clinical supervisors; resource limitations at non-training sites; views of staff/culture of institution; lack of curriculum flexibility; varied baseline knowledge; language barrier |
| Stanley | To improve competence in assessment and management of emergent conditions | None | Scenario-based drills/training with whiteboard and reference cards; focus on ABCDE | Observed scenarios (OSCE) and feedback form; pre-assessment; 1–2-week post-assessment and 8-week assessment | Not described | Three sites; four days at each site (pre-assessment, training, post-assessment, 8-week assessment) with two identical sessions daily | Previously used local training tools and instructor experience | Assessment scores and self-reported confidence scores all improved after the intervention | Attendance low |
Goals and Objectives
Each of the eleven programs conducted formal needs assessments and/or had focus group discussions to identify learning gaps and to determine the content, style, and/or duration of each program, fulfilling the first two steps Kern et al.’s six-step model for curriculum development [46]. These efforts drew upon the strengths and experiences of the instructors while considering the knowledge level of the learners and using familiar teaching styles and/or providing orientation to new instructional methods. One manuscript highlights a pilot study prior to full implementation of a program [35]. Three studies highlight instructor (both international and local) development and orientation prior to commencement of the program [38,41,42].
Certification/Recognition
More than half of the manuscripts discuss alignment with local or national governing bodies, such as the Ministry of Health (MoH) regarding formal recognition, licensing, and/or certification of their respective programs.
Curriculum Outline/Components
The curricula highlighted in these manuscripts span short, foundational programs to medium-length programs with abbreviated, comprehensive EM curricula to full-length residency programs (of at least three years). All offer mixed learning methods ranging from traditional didactic lectures and small group discussions (i.e. journal clubs and case-based sessions) to hands-on practical sessions and workshops, such as simulation and procedural training. Curricula are often organized into blocks or modules by topics or organ systems. Longer programs allocate one to three half-days every one or two weeks for learning sessions in addition to daily bedside clinical teaching. Volunteer patients, mannequins, laminated algorithms, white boards, and other simulation materials as well as video/online materials, handbooks, and textbooks are highlighted as curriculum tools. Many programs incorporate pediatrics as well. All residency programs list the requirement of off-service rotations, such as surgery, anesthesia, and critical care. Only one manuscript offers extensive online access to their curriculum map and resources [41]. One of the short programs emphasizes the need for refresher courses, particularly when limited curricula are offered and/or baseline knowledge is varied or limited [39]. One manuscript specifically evaluates the acceptability of a novel-to-context learning modality (small group sessions) within the overall program [45].
Methods of Assessment
All programs have a written component of assessment. These examinations consist of multiple-choice questions, short-answer, and/or essay questions. Many manuscripts highlight programs that also have practical examinations – skills stations, oral and/or case-based examinations as well as objective structured clinical examinations (OSCEs). Longer programs also often track attendance and require case and/or procedure logs with minimum required numbers. Minimum passing requirements for examinations and attendance, when specified, range from 70–80%. There are often end-of rotation evaluations and performance audits, especially for residency programs with off-service rotations. There is usually ongoing informal feedback and mentorship. One program mentions requiring a thesis [44].
Funding
Three of the 11 manuscripts do not discuss how their programs are supported, while the others note a combination of private donors, non-profit organizations, healthcare organizations, and funding from universities in higher-resource settings. Manuscripts that mention their funding sources note a mix of self-funding or subsidized funding for international faculty. Among the larger funding sources listed are the Abbott Fund, USAID, Grand Challenges, and Project HOPE. Salary for learners in residency programs and fees for learners for non-residency programs are less clear – at least one program notes that there are no fees for their learners, and those who had to travel for the program received room and board [36].
Logistics
All of the programs involve international visiting faculty for ongoing full or supervisory support either in person and/or via teleconferencing, messaging, or other methods of remote engagement. Visiting faculty contributions are described as ranging from one week up to multiple years onsite and/or remotely. Longer programs tend to have curricula that repeat one or more times over the course of the program. Train-the-trainer techniques are used in two of the programs [39,43]. Two programs mention their learner-to-instructor ratio for hands-on sessions (a range of 3–6:1) [38,45]. One program is structured to have two identical sessions daily in order to accommodate the learners, who must provide continuous coverage in the clinical setting [35].
Educational Resources
Content for the curricula is drawn from a variety of sources – usually initially from EM content belonging to the high-resource partner. Specific materials and organizations listed among the programs for reference include basic life support (BLS), advanced cardiac life support (ACLS), advanced trauma life support (ATLS), pediatric advanced life support (PALS), textbooks (specifically Tintinalli, Rosen, and Goldfrank, among others), World Health Organization (WHO) resources (such as Integrated Management of Adolescent and Adult Illness and Integrated Management of Childhood Illnesses), Canadian Association of Emergency Physicians (CAEP), American College of Emergency Physicians (ACEP), IFEM, Society for Academic Emergency Medicine (SAEM), African Federation for Emergency Medicine (AFEM), European Society for Emergency Medicine (EuSEM), World Association for Disaster and Emergency Medicine (WADEM), Australasian Society for Emergency Medicine (ASEM), Consortium of Universities for Global Health (CUGH), Johns Hopkins Global Health, international EM journals (i.e. International Journal of Emergency Medicine), and American and Canadian graduate medical education (GME) resources.
Outcomes
Knowledge acquisition, clinical performance, and/or learner confidence/self-assessment are among the outcomes listed for almost all of the programs. All programs conduct immediate assessments; however, many of the programs also assess knowledge retention at a variety of time points: eight weeks, three months, six months, and one year. Additionally, some programs highlight the number of graduates as well as the number of individuals still practicing in EM. None of the program outcomes extend beyond the learner, although future studies of clinical outcomes are mentioned in one manuscript [43].
Challenges
Challenges common to many of the programs include establishing the status and culture of practice of EM in low-resource, novel settings. Additionally, the manuscripts describe how differences in scope, practice, and content between the high-resource and low-resource settings as well as among program sites within low-resource settings require translation and adaptation of any shared educational resources and techniques. Overall resource limitations for learning as well as practice materials are frequently noted. Language barriers (for both instruction and materials) as well as issues with remote connection and use of local and remote technologies are also highlighted. Additionally, lack of continuity and connection between learners and the rotating visiting faculty – who may be present in person for as little as one week – leads to reduced engagement and morale. Decay in knowledge, especially after short programs, is also a concern, with re-assessment between 2–3 months highlighted as potentially an ideal time for re-assessment or refresher training. Difficulties with both learner (e.g. attendance given the requirement of ongoing continuous clinical duties still required during many of the programs) and curriculum flexibility leads to attrition for many programs. There are also ongoing concerns regarding sustainable funding highlighted in several of the manuscripts – for the program, for visiting faculty, as well as for learners/graduates.
Discussion
These manuscripts describe many types of EM programs being implemented via partnerships worldwide to train in-hospital personnel critical for the overall development of emergency care systems – from short, focused courses on topics such as ultrasound training or trauma training to full residency programs. The most established programs are those that are of at least one year in duration and those with formal integration into the healthcare and/or medical education system of the country (e.g. supported by the MoH). These programs can then offer official certification and/or credentialing to ensure that graduates will have both potential positions and financial security as well as a career path as EM develops and the culture of practice changes.
All of the programs involve on-site and/or remote international faculty for varying lengths of time; however, programs in which at least a core subset of faculty are involved in face-to-face teaching through the duration of the program foster stronger partnerships and allow for continuity of evaluation as well as continuous improvement and adaptation of the program. Given the differences in resources and culture of practice, all visiting faculty need at least prior experience in education/training and low-resource environments and/or a comprehensive orientation to the site prior to providing instruction. One manuscript describes the challenges of conflicting expectations between instructors and learners due to the limited preparation and experience by the visiting faculty [38].
Furthermore, the use of international faculty is rarely sustainable, especially when support for these faculty is not available. Programs that involve a train-the-trainer component as well as faculty development are essential, although limitations of these models (especially dilution of instruction) must be kept in mind and addressed using other mechanisms such as refresher courses and mentorship or preceptor programs. Additionally, given the increasing familiarity with and use of technology, non-traditional training mechanisms such as the use of messaging applications and other mobile technology-based training tools should be considered, especially as they can be effective mechanisms to extend training beyond face-to-face interactions and/or to continue training during protracted and/or complex emergencies [47,48,49].
These programs also highlight the inability to simply transfer EM curricula from one setting to another. Some fundamental concepts can be shared, as is evidenced by international guidelines for curricula, and there are several groups that have offered open-access materials that are already adapted to low-resource settings to varying degrees (Table 5). In order to be effective, however, the development of curricula – whether abbreviated or a full residency program – must be preceded by needs assessments, focus-group discussions, and knowledge of the epidemiology and burden of disease as well as the culture of practice, instruction, learning, and assessment of the implementation site [50,51,52]. Additionally, language barriers must be overcome both in instruction as well as in written and electronic materials [53]. Finally, there must be inter-sectoral engagement and collaboration between the health and education sectors in order to recruit, develop, and sustain a quality workforce that is matched to overall service delivery capacity and population needs [54].
Table 5.
Sample list of curricula and content resources.
| Organization | Resources | Website* |
|---|---|---|
| Global Health Emergency Medicine (GHEM) | Teaching modules | http://ghem.ca/modules/ |
| African Federation for Emergency Medicine (AFEM) | Curricula, lecture bank, ultrasound lecture bank | https://afem.africa/resources/ |
| World Health Organization (WHO) | Full short course | https://www.who.int/emergencycare/publications/Basic-Emergency-Care/en/ |
| International Student Association of Emergency Medicine (ISAEM) and the International Emergency Medicine Education Project (iEM) | Medical student resources |
https://isaem.net/ https://iem-student.org |
| International Federation for Emergency Medicine | General guidelines; curricula outlines | https://www.ifem.cc/ |
| OPENPediatrics | Pediatric-specific resources | https://www.openpediatrics.org/ |
| Emergency Ultrasound Teaching | Ultrasound-specific resources | http://emergencyultrasoundteaching.com/ |
| Free, Open-Access Medical Education Resources | One list of general resources | https://rebelem.com/focused-foamed-the-learners-lens/ |
| American College of Emergency Physicians (ACEP) International Section | General resources from an EM organization | https://www.acep.org/how-we-serve/sections/international-emergency-medicine/free-educational-resources/ |
* Accessed: May 2019; the authors do not specifically endorse any particular resource, nor do they verify the accuracy of the content listed at the sites above.
Finally, in order to continue to advance EM training and the overall provision of emergency care, programs must include training in quality improvement (QI) and research, topics not traditionally taught in many medical and nursing schools in low-resource settings. To illustrate this point, less than half of the programs mention a component of QI and/or research, and only two of the manuscripts have a local first author [31,44]. Furthermore, in order to determine which methods of training are most effective, we must move beyond metrics regarding knowledge acquisition and attitude and eventually look to patient-, community-, and population-based outcomes [55]. Only three of the manuscripts evaluate patient and/or clinical outcomes as a result of their training programs [20,26,31].
Despite ongoing work to develop metrics and quality indicators for emergency care and research and to provide guidance in the development of emergency care systems (as evidenced by the WHO’s Emergency, Trauma and Acute Care Program), there is still very little research that has focused specifically on the impact of training programs [9,56,57,58,59,60,61,62,63]. These programs are an integral part of the foundation of a sustainable emergency care system, not only at the facility level, but indirectly within the community and the pre-hospital system as well, therefore, further investigation of and research on these programs is imperative to sustain and to continue to expand EM as a specialty and emergency care systems globally.
Limitations
Overall, we used only four search engines and excluded programs in the gray literature without peer review (i.e. abstracts) – an area in which many more programs are likely highlighted based on an informal review of the excluded abstracts. Also, our results are limited to manuscripts only in English. Additionally, the search terms used to define this rapidly changing and developing field were difficult to specify, leading to one additional manuscript that was identified on informal review that could have been included in this study [64]. Furthermore, partnerships are also not always made explicit in many manuscripts; since our study focused on programs developed through educational partnerships, we may have missed manuscripts in the screening process where this was not clearly defined [65]. This challenge further emphasizes the need for standardization of practice and sharing of knowledge and experience in this field. Finally, our scoring process was developed from tools used in other reviews and was not formally tested with our results; however, it has been used to evaluate literature in field of global EM, and post hoc review demonstrated that the conclusions drawn from the high-scoring manuscripts were representative of the larger group [19]. Despite these limitations, however, this study still identifies a broad range of EM training programs, and it highlights programmatic components essential for effective partnerships and successful implementation.
Conclusions
Training in EM is an essential component to developing strong emergency care systems. This study identifies a broad range of EM training programs developed through partnerships that are representative of the programs that exist globally and highlight programmatic components essential to the development of effective programs. Sharing knowledge and practice across high- and low-resource settings can be an effective mechanism for the global development of programs within a specialty, however significant adaptation to the educational setting as well as true investment and partnership must occur, even for short-term programs. Even when all of the complexities and components are addressed, there are still limitations to this practice. Short-term programs need to expand beyond the few topics that are represented now, and we must invest in comprehensive, long-term emergency care training and professional development programs. Finally, as tools and guidance regarding the development of emergency care systems increase, a strong focus on strengthening educational practices as well as evaluating their impact through research is imperative.
Additional Files
The additional files for this article can be found as follows:
Search Strings.
Scoring Rubric.
Acknowledgements
We would like to thank the librarians of Brigham and Women’s Hospital as well as the Harvard Countway Library of Medicine – particularly Jacqueline Cellini – for their assistance with the development of and the execution of the search.
Competing Interests
Several of the reviewers were authors of manuscripts involved/included in the study. Reviewers did not screen or score their own manuscripts. The authors endorse no other competing interests regarding this review.
Author Contribution
The authors listed here have all contributed significantly to this work and the preparation of the manuscript. MR, SK, MN, MB, KC, SR, AT, HG, and TR conceptualized the project. MR designed the study. MR, NL, MB, SK, MN screened the manuscripts. MR, NL, MB, SK, MN, MB, KC, SR, and AT scored the manuscripts. MR drafted the manuscript. All authors reviewed and edited the final manuscript.
References
- 1.World Health Organization. WHA 60.22 Health Systems: Emergency-care Systems 2007. Geneva: Sixtieth World Health Assembly; http://www.wpro.who.int/mnh/A60_R22-en.pdf. [Google Scholar]
- 2.World Health Organization. WHA 68.15. Strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage 2015. Geneva: Sixty-eighth World Health Assembly; http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_R15-en.pdf?ua=1. [Google Scholar]
- 3.World Health Organization. WHA 72.16. Emergency care systems for universal health coverage: ensuring timely care for the acutely ill and injured 2019. Seventy-second World Health Assembly; Geneva: http://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R16-en.pdf. [Google Scholar]
- 4.Chang C, Abujaber S, Reynolds T, Camargo C, Obermeyer Z. Burden of emergency conditions and emergency care usage: New estimates from 40 countries. Emergency Medicine Journal. 2016; 33(11): 794–800. DOI: 10.1136/emermed-2016-205709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson P, Petrino R, Halpern P, Tintinalli J. The globalization of emergency medicine and its importance for public health. Bulletin of the World Health Organization. 2006; 84(10): 835–9. DOI: 10.2471/BLT.05.028548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson P, Suter R, Mulligan T, Bodiwala G, Razzak J, Mock C. International Federation for Emerency Medicine (IFEM) Task Force on Access and Availability of Emergency Care. World Health Assembly Resolution 60.22 and its importance as a health care policy tool for improving emergency care access and availability globally. Annals of Emergency Medicine. 2012; 60(1): 35–44. DOI: 10.1016/j.annemergmed.2011.10.018 [DOI] [PubMed] [Google Scholar]
- 7.Razzak J, Kellermann A. Emergency medical care in developing countries: is it worthwhile? Bulletin of the World Health Organization. 2002; 80(11): 900–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Cameron P, Hobgood C, Mulligan T. Developments in international emergency medicine. Emergency Medicine Australasia. 2009; 21(5): 339–41. DOI: 10.1111/j.1742-6723.2009.01211.x [DOI] [PubMed] [Google Scholar]
- 9.Calvello E, Broccoli M, Risko N, Theodosis C, Totten V, Radeos M, Seidenberg P, Wallis L. Emergency care and health systems: Consensus-based recommendations and future research priorities. Academic Emergency Medicine. 2013; 20: 1278–88. DOI: 10.1111/acem.12266 [DOI] [PubMed] [Google Scholar]
- 10.International EM Core Curriculum and Education Committee for the International Federation for Emergency Medicine. International Federation for Emergency Medicine model curriculum for emergency medicine specialists. CJEM. 2011; 13(2): 109–21. DOI: 10.2310/8000.2011.110446 [DOI] [PubMed] [Google Scholar]
- 11.International Federation for Emergency Medicine. Member Organizations. 24 December 2018. www.ifem.cc. Accessed: 2 May 2019. https://www.ifem.cc/membership/member-organisations/.
- 12.Arnold J. International emergency medicine and the recent development of emergency medicine worldwide. Annals of Emergency Medicine. 1999; 33(1): 97–103. DOI: 10.1016/S0196-0644(99)70424-5 [DOI] [PubMed] [Google Scholar]
- 13.Arnold J, Holliman C. Lessons learned from international emergency medicine development. Emergency Medicine Clinics of North America. 2005; 23(1): 133–47. DOI: 10.1016/j.emc.2004.10.001 [DOI] [PubMed] [Google Scholar]
- 14.Alagappan K, Schafermeyer R, Holliman C, et al. International emergency medicine and the role for academic emergency medicine. Academic Emergency Medicine. 2007; 14(5): 451–6. DOI: 10.1197/j.aem.2007.01.003 [DOI] [PubMed] [Google Scholar]
- 15.Kirsch T, Holliman C, Hirshon J, Doezema D. The development of international emergency medicine: a role for U.S. emergency physicians and organizations. SAEM International Interest Group. Academic Emergency Medicine. 1997; 4(10): 996–1001. DOI: 10.1111/j.1553-2712.1997.tb03667.x [DOI] [PubMed] [Google Scholar]
- 16.Nowacki A, Landes M, Azazh A, Puchalski Ritchie L. A review of published literature on emergency medicine training programs in low- and middle-income countries. International Journal of Emergency Medicine. 2013; 6(1): 26 DOI: 10.1186/1865-1380-6-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holliman C, Kirsch T, Green G, Wolfson G, Tom P. Guidelines for evaluation of international emergency medicine assistance and development projects. Annals of Emergency Medicine. 1997; 30(6): 811–5. DOI: 10.1016/S0196-0644(97)70054-4 [DOI] [PubMed] [Google Scholar]
- 18.The World Bank. World Bank Country and Lending Groups. Accessed 2 May 2019. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 19.Becker T, Trehan I, Hayward A, et al. Global emergency medicine: A review of the literature from 2017. Academic Emergency Medicine. 2018; 25: 1287–98. DOI: 10.1111/acem.13456 [DOI] [PubMed] [Google Scholar]
- 20.Becker T, Tafoya C, Osei-Ampofo M, et al. Cardiopulmonary ultrasound for critically ill adults improves diagnostic accuracy in a resource-limited setting: The AFRICA trial. Tropical Medicine and International Health. 2017; 22(12): 1599–1608. DOI: 10.1111/tmi.12992 [DOI] [PubMed] [Google Scholar]
- 21.Cioè-Peña E, Granados J, Wrightsmith L, Henriquez-Vigil A, Moresky R. Development and implementation of a hospital-based trauma response system in an urban hospital in San Salvador, El Salvador. Trauma. 2017; 19(2): 118–26. DOI: 10.1177/1460408616672491 [DOI] [Google Scholar]
- 22.Crouse H, Vaides H, Torres F, et al. Quality and effectiveness of a pediatric triage training program in a Guatemalan public hospital. Pediatric Emergency Care. 2016; 32(8): 252–8. DOI: 10.1097/PEC.0000000000000277 [DOI] [PubMed] [Google Scholar]
- 23.Denny S, Minteer W, Fenning R, et al. Ultrasound curriculum taught by first-year medical students: A four-year experience in Tanzania. World Journal of Emergency Medicine. 2018; 9(1): 33–40. DOI: 10.5847/wjem.j.1920-8642.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henwood P, Mackenzie D, Rempell J, et al. Intensive point-of-care ultrasound training with long-term follow up in a cohort of Rwandan physicians. Tropical Medicine and International Health. 2016; 21(12): 1531–8. DOI: 10.1111/tmi.12780 [DOI] [PubMed] [Google Scholar]
- 25.Kapoor R, Sandoval M, Avendaño L, et al. Regional scale-up of an Emergency Triage Assessment and Treatment (ETAT) training programme from a referral hospital to primary care health centres in Guatemala. Emergency Medicine Journal. 2016; 33: 611–7. DOI: 10.1136/emermed-2015-205057 [DOI] [PubMed] [Google Scholar]
- 26.Kesinger M, Nagy L, Sequeira D, Charry J, Puyana J, Rubiano A. A standardized trauma care protocol decreased in-hospital mortality of patients with severe traumatic brain injury at a teaching hospital in a middle-income country. Injury. 2014; 45: 1350–4. DOI: 10.1016/j.injury.2014.04.037 [DOI] [PubMed] [Google Scholar]
- 27.Merchant A, Outhay M, Gonzaléz-Calvo L, et al. Training laypersons and hospital personnel in basic resuscitation techniques: An approach to impact the global trauma burden in Mozambique. World Journal of Surgery. 2015; 39: 1433–7. DOI: 10.1007/s00268-015-2966-z [DOI] [PubMed] [Google Scholar]
- 28.McCredie V, Shrestha G, Acharya S, et al. Evaluating the effectiveness of the Emergency Neurological Life Support educational framework in low-income countries. International Health. 2018; 10: 116–24. DOI: 10.1093/inthealth/ihy003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meaney P, Sutton R, Tsima B, et al. Training hospital providers in basic CPR skills in Botswana: Acquisition, retention and impact of novel training techniques. Resuscitation. 2012; 83(12): 1484–90. DOI: 10.1016/j.resuscitation.2012.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reynolds T, Noble J, Paschal G, et al. Bedside ultrasound training at Muhimbili National Hospital in Dar es Salaam, Tanzania and Hospital San Carlos in Chiapas, Mexico. African Journal of Emergency Medicine. 2016; 6: 125–31. DOI: 10.1016/j.afjem.2016.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Senarathna L, Buckley N, Dibley M, et al. Effect of a brief outreach educational intervention on the translatino of acute poisoning treatment guidelines to practice in rural Sri Lankan hospitals: A cluster randomized controlled trial. PLoS One. 2013; 8(8): e71787 DOI: 10.1371/journal.pone.0071787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stolz L, Muruganandan K, Bisanzo M, et al. Point-of-care ultrasound education for non-physician clinicians in a resource-limited emergency department. Tropical Medicine and International Health. 2015; 20(8): 1067–72. DOI: 10.1111/tmi.12511 [DOI] [PubMed] [Google Scholar]
- 33.Tafoya C, Tafoya M, Osei-Ampofo M, Oteng R, Becker T. Sustainable resuscitation ultrasound education in a low-resource environment: The Kumasi experience. The Journal of Emergency Medicine. 2017; 52(5): 723–30. DOI: 10.1016/j.jemermed.2017.01.050 [DOI] [PubMed] [Google Scholar]
- 34.Wanjiku G, Janeway H, Foggle J, et al. Assessing the impact of an emergency trauma course for senior medical students in Kenya. African Journal of Emergency Medicine. 2017; 7: 167–71. DOI: 10.1016/j.afjem.2017.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stanley L, Min T, Than H, et al. A tool to improve competence in the management of emergency patients by rural clinical health workers: A pilot assessment on the Thai-Myanmar border. Conflict and Health. 2015; 9(11): 1–9. DOI: 10.1186/s13031-015-0041-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rouhani S, Israel K, Leandre F, Pierre S, Bollman B, Marsh R. Addressing the immediate need for emergency providers in resource-limited settings: The model of a six-month emergency medicine curriculum in Haiti. International Journal of Emergency Medicine. 2018; 11(22): 1–7. DOI: 10.1186/s12245-018-0182-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reynolds T, Mfinanga J, Sawe H, Runyon M, Mwafongo V. Emergency care capacity in Africa: A clinical and educational initiative in Tanzania. Journal of Public Health Policy. 2012; 33: S126–37. DOI: 10.1057/jphp.2012.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pean C, Davis K, Merrill R, et al. Neer-peer emergency medicine for medical students in Port-au-Prince, Haiti: An example of rethinking global health interventions in developing countries. Annals of Global Health. 2015; 81(2): 276–82. DOI: 10.1016/j.aogh.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 39.Niyogi A, Villona B, Rubenstein B, Hubbard S, Baiden F, Moresky R. In-service training of physician assistants in acute care in Ghana: Challenges, successes, and lessons learned. African Journal of Emergency Medicine. 2015; 5: 144–9. DOI: 10.1016/j.afjem.2015.01.006 [DOI] [Google Scholar]
- 40.Mahadevan S, Walker R, Kalanzi J, et al. Comparison of online and classroom-based formats for teaching emergency medicine to medical students in Uganda. Academic Emergency Medicine Education and Training. 2018; 2(1): 5–9. DOI: 10.1002/aet2.10066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meshkat N, Teklu S, Hunchak C, TAAAC-EM and the Global Health Emergency Medicien (GHEM) organization at the Division of Emergency Medicine University of Toronto. Design and implementation of a postgraduate curriculum to support Ethiopia’s first emergency medicine residency training program: the Toronto Addis Ababa Academic Collaboration in Emergency Medicine (TAAAC-EM). BMC Medical Education. 2018; 18(1): 71 DOI: 10.1186/s12909-018-1140-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keyes C, Rodriguez-Gomez G, Quesada-Rodriguez D, Waller J. The Costa Rican emergency medicine residency: Design and implementation of a new specialty training program in Central America. Annals of Emergency Medicine. 1999; 34(6): 790–5. DOI: 10.1016/S0196-0644(99)70108-3 [DOI] [PubMed] [Google Scholar]
- 43.Hammerstedt H, Maling S, Kasyaba R, et al. Addressing World Health Assembly Resolution 60.22: A pilot project to create access to acute care services in Uganda. Annals of Emergency Medicine. 2014; 64(5): 461–8. DOI: 10.1016/j.annemergmed.2014.01.035 [DOI] [PubMed] [Google Scholar]
- 44.Aggarwal P, Galwankar S, Kalra O, Bhalla A, Bhoi S, Sundarakumar S. The 2014 Academic College of Emergency Experts in India’s Education Development Committee (EDC) White Paper on establishing an academic department of emergency medicine in India – guidelines for staffing, infrastructure, resources, curriculum, and training. Journal of Emergencies, Trauma, and Shock. 2014; 7(3): 196–208. DOI: 10.4103/0974-2700.136866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lim A, Geduld H, Checkett K, Sawe H, Reynolds T. Pioneering small-group learning in Tanzanian emergency medicine: investigating acceptability for physician learners. African Journal of Health Professions Education. 2017; 9(1): 24–8. DOI: 10.7196/AJHPE.2017.v9i1.692 [DOI] [Google Scholar]
- 46.Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach, Third Edition Baltimore: Johns Hopkins University Press; 2016. [Google Scholar]
- 47.Edgcombe H, Paton C, English M. Enhancing emergency care in low-income countries using mobile technology-based training tools. Archives of Disease in Childhood. 2016; 101(12): 1149–52. DOI: 10.1136/archdischild-2016-310875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haile-Mariam T, Koffenberger W, McConnell H, Widamayer S. Using distance-based technologies for emergency medicine training and education. Emergency Medicine Clinics of North America. 2005; 23(1); 217–29. DOI: 10.1016/j.emc.2004.09.003 [DOI] [PubMed] [Google Scholar]
- 49.Raiman L, Antbring R, Mahmood A. WhatsApp messenger as a tool to supplement medical education for medical students on clinical attachment. BMC Medical Education. 2017; 17(1): 7 DOI: 10.1186/s12909-017-0855-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hobgood C, Anantharaman V, Bandiera G, et al. International Federation for Emergency Medicine model curriculum for emergency medicine specialists. Emergency Medicine Australasia. 2011; 23(5): 541–53. DOI: 10.1111/j.1742-6723.2011.01489.x [DOI] [PubMed] [Google Scholar]
- 51.Atkinson P, Bowra J, Lambert M, Lamprecht H, Noble V, Jarman B. International Federation for Emergency Medicine point of care ultrasound curriculum. CJEM. 2015; 17(2): 161–70. DOI: 10.1017/cem.2015.8 [DOI] [PubMed] [Google Scholar]
- 52.Hobgood C, Anantharaman V, Bandiera G, et al. International Federation for Emergency Medicine. International Federation for Emergency Medicine model curriculum for medical student education in emergency medicine. Emergency Medicine Journal. 2010; 27(10): 766–9. DOI: 10.1136/emj.2009.087775 [DOI] [PubMed] [Google Scholar]
- 53.Iserson K. The REEME project: A cooperative model for sharing international medical education materials. The Journal of Emergency Medicine. 2008; 35(1): 95–9. DOI: 10.1016/j.jemermed.2007.07.075 [DOI] [PubMed] [Google Scholar]
- 54.Celletti F, Reynolds T, Wright A, Stoertz A, Dayrit M. Education a new generation of doctors to improve the health of populations in low- and middle-income countries. PLoS Medicine. 2011; 8(10): e1001108 DOI: 10.1371/journal.pmed.1001108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moore D Jr, Green J, Gallis H. Achieving desired results and improved outcomes: Integrating planning and assessment throughout learning activities. Journal of Continuing Education in the Health Professions. 2009; 29(1): 1–15. DOI: 10.1002/chp.20001 [DOI] [PubMed] [Google Scholar]
- 56.Aluisio A, Mbanjumucyo G, Barry M, Karim N, Levine A. Impact of implementation of emergency medicine training on emergency department mortality in Kigali, Rwanda: An interrupted time-series quasi-experimental design. Annals of Emergency Medicine. 2017; 70(4, Supplement): S78 DOI: 10.1016/j.annemergmed.2017.07.220 [DOI] [Google Scholar]
- 57.Abujaber S, Chang C, Reynolds T, Mowafi H, Obermeyer Z. Developing metrics for emergency care research in low- and middle-income countries. African Journal of Emergency Medicine. 2016; 6(3): 116–124. DOI: 10.1016/j.afjem.2016.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Broccoli M, Moresky R, Dixon J, et al. Defining quality indicators for emergency care delivery: Findings of an expert consensus process by emergency care practitioners in Africa. BMJ Global Health. 2018; 3(1): e000479 DOI: 10.1136/bmjgh-2017-000479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aaronson E, Marsh R, Guha M, Schuur J, Rouhani S. Emergency department quality and safety indicators in resource-limited settings: An environmental survey. International Journal of Emergency Medicine. 2015; 8(1): 39 DOI: 10.1186/s12245-015-0088-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Holliman C, VanRooyen M, GB G, et al. Planning recommendations for international emergency medicine and out-of-hospital care system development. Academic Emergency Medicine. 2000; 7(8): 911–7. DOI: 10.1111/j.1553-2712.2000.tb02070.x [DOI] [PubMed] [Google Scholar]
- 61.Thomas, T. Developing and implementing emergency medicine programs globally. Emergency Medicine Clinics of North America. 2005; 23(1): 177–97. DOI: 10.1016/j.emc.2004.09.005 [DOI] [PubMed] [Google Scholar]
- 62.Kobusingye O, Hyder A, Bishai D, Hicks E, Mock C, Joshipura M. Emergency medical systems in low- and middle-income countries: Recommendations for action. Bulletin of the World Health Organization. 2005; 83(8): 626–31. [PMC free article] [PubMed] [Google Scholar]
- 63.Hodkinson P, Wallis L. Emergency medicine in the developing world: A Delphi study. Academic Emergency Medicine. 2010; 17(7): 765–74. DOI: 10.1111/j.1553-2712.2010.00791.x [DOI] [PubMed] [Google Scholar]
- 64.Busse H, Azazh A, Teklu S, et al. Creating change through collaboration: A twinning partnership to strengthen emergency medicine at Addis Ababa University/Tikur Anbessa Specialized Hospital – A model for international medical education partnerships. Academic Emergency Medicine. 2013; 20(12): 1310–18. DOI: 10.1111/acem.12265 [DOI] [PubMed] [Google Scholar]
- 65.Caruso N, Chandra A, Kestler A. Development of emergency medicine in Botswana. African Journal of Emergency Medicine. 2011; 1(3): 108–12. DOI: 10.1016/j.afjem.2011.08.002 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Strings.
Scoring Rubric.


