Abstract
Our objective was to describe and evaluate an innovative approach to combining worksite wellness and ergonomics, with an emphasis on retention and absenteeism during the intervention. The study enrolled 280 employee participants in a 3-year cluster randomized, controlled trial conducted at The University of Iowa, 5 local businesses, and 1 regional business. Our results showed a 90% retention rate with lower estimated absenteeism (although not statistically significant) in the intervention group compared with the control group. This type of highly interactive and integrated short intervention has the capacity to result in high levels of participation with the potential to reduce absenteeism.
Keywords: employee absenteeism, ergonomics, health promotion, health protection, worksite wellness
INTRODUCTION
Over the past decade, wellness programs have been developed to reduce organizational costs and maximize employee productivity.1 While there are many programs that focus on health protection and health promotion separately,2,3 few have combined these 2 important elements within 1 worksite intervention.4 By combining these 2 programs, persons managing each one in a worksite setting are brought together to collaborate in fulfilling worker benefits that have the potential to reduce overall employee absenteeism.
Many health promotion studies have focused on providing information5–9 to workers that might help them in knowing what to do (educational content) but not why it is important (value). In a meta-analysis, the inclusion of education-only programs was prohibited because these programs infrequently included evaluation data.1 Three programs have focused on participation in workplace interventions as an important element in mental health and job performance.10–12 Similarly, novel interventions like the one in this study have the potential to be less directive and more interactive than education-only programs. It allows the participants to guide the concepts covered during the session discussions.
The Be Engaged:
Help Integrate Promotion/Protention (Be Hipp) program helped integrate workplace health promotion and protection while examining the effectiveness of participatory group counseling (intervention) compared with quarterly newsletters (control) as a means of modifying behaviors toward healthier habits. In this article, we describe the study outcomes of intervention, retention, and worksite absenteeism.
MATERIALS AND METHODS
Study design
The Be Hipp study was a cluster randomized trial examining the effectiveness of counseling as a means of integrating health protection and promotion interventions with emphasis on group participation. Participants were screened to exclude people who did not plan to remain in their job for 3 years, people with work schedules that would not permit them to attend a monthly group lunch session, and people who were currently working with a health coach and/or fitness trainer. The cluster randomization was implemented to reduce cross-talk (contamination) among office mates. Clusters were formed on the basis of department and worksite location. Clusters were block randomized into intervention (interactive participatory monthly group lunch sessions) and control (quarterly newsletters) arms to maintain size. This attention to detail in separating control and intervention groups is a mark of optimum study design allowing for maximization of group data separation and fidelity of intervention and control group protocols.
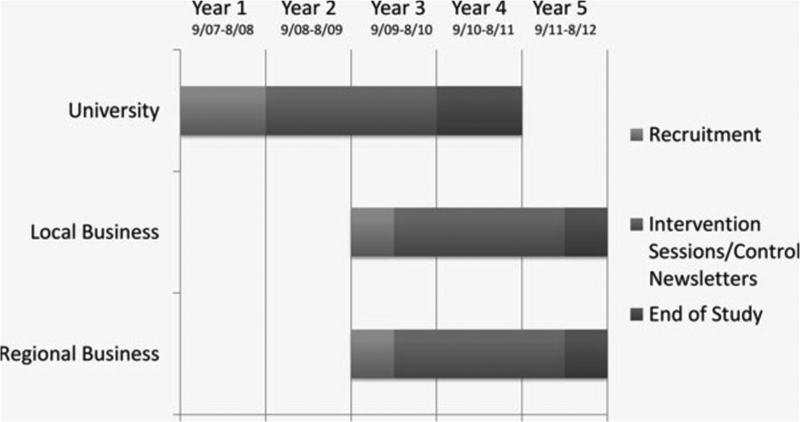
Recruitment
Three rounds of recruitment were completed to enroll workers with primarily sedentary job duties, all in the state of Iowa: The University of Iowa, small to medium-sized local businesses, and a regional insurance company. We included 5 local business sites because of a flood that precluded us from randomizing only at The University of Iowa. As a result of the economic downturn during our study, additional local sites were reluctant to become involved and we added a regional insurance company.
Recruitment strategies included presentations on the study to worksites where sedentary jobs were the norm. Presentations to these groups included a description of the study with reference to the 2 groups, intervention and control. In addition, recruitment occurred through the use of table tents, small advertisements for the study on tables in The University of Iowa cafeteria, and group meetings in areas near worksites. After attending an information session, workers interested in participating were seen individually to assess eligibility, provide consent, and complete baseline measures.
A river on the university campus separates the medical campus from other academic colleges and departments. Recruitment strategies were employed on both sides of the river to allow for a natural cluster randomization. Sixty-nine participants were enrolled during this round of recruitment, with 36 participants randomized to the control arm and 33 to the intervention arm. To meet study participant goals, recruitment efforts turned to local businesses employing office workers in sedentary jobs that spanned national testing services, engineering, and law consulting. Local company management or human resource personnel were contacted by phone to assess interest and their potential participant pool. After agreement from company management to offer study participation to employees, recruitment was implemented as previously described. Round 2 of recruitment yielded 5 small to medium-sized businesses that were cluster randomized by business. Randomization occurred by business size with the small and medium-sized businesses paired. Businesses were in separate locations to prevent contamination. Three control sites included a total of 53 participants and 2 intervention sites included a total of 51 participants for a totalof104participants in this cohort.
Round 3 of recruitment moved to a large regional insurance company. The physical layout of this worksite allowed for cluster randomization by department to prevent crosstalk contamination and, therefore, included both control and intervention arms. Recruitment procedures were initiated, resulting in 107 (54 intervention, 53 control) employees providing consent and baseline data completing our needed sample size of 280 participants. The University of Iowa Institutional Review Board approved the study activities before initiating at each site.
Measures
After signing the consent, participants were given a unique name code and password that was linked to their data collection measures. Measures were collected on all participants at baseline (immediately following consent signing), year 1 and year 2. Individual assessments included measured height and weight and an online survey. Data collection personnel were trained on obtaining standardized height and weight measures. Height was measured in centimeters to the nearest tenth in street clothes without shoes using a portable height board (ShorrBoard, Shorr Productions, Olney, Maryland). Weight was measured in street clothes without shoes using a portable scale (Seca Model 770, Hanover, Maryland). Weight was measured in kilograms to the nearest tenth. Body mass index (BMI) was calculated from these measures for each participant. The online survey was completed at the visit with study staff present. Participants were provided their unique name code and password to allow them to log on to complete the Web-based survey.
The survey consisted of the following 6 validated instruments.
The Demographic and Personal Health Questionnaire provided information about characteristics (eg, birthdate, race, gender), personal health (diabetes, hypothyroidism, rheumatoid arthritis and other collagen vascular disease, renal failure, pregnancy, and prior upper extremity and spine disorders), and history of injury or trauma to the upper extremities and spine. Some of these data appear in Tables 1 and 2.
The Stanford Health and Lifestyle Assessment was used to obtain information about the respondent’s physical activity, nutrition, stress and mental health, alcohol and tobacco, health knowledge and attitudes, medical history, biometrics (eg, blood pressure and blood glucose), and readiness to change health habits.13
The 36-Item Short Form Health Survey, version 2 (SF-36v2) was also used for questions on physical and mental health. The SF-36v2 has been used extensively in epidemiologic research, including many studies of back pain and musculoskeletal illness.14
The Karasek Questionnaire assessed workers’ perceived psychological demands, scope of decision making, social support, physical demands, and job security.15
The Nordic Questionnaire16 was modified to assess data on self-reported musculoskeletal symptoms. Employees in blue collar or service occupations or in low supervisory, technical, clerical, or routine occupations are at higher risk for work-related injury and also have a higher prevalence of lifestyle-related risk factors than professional job classes.17–19 Therefore, they are an important target group for integrated health protection and health promotion interventions. Musculoskeletal disorders of the upper extremity and lower back are common injuries to these workers and will be the particular focus of health protection in this project since ergonomic intervention and prevention can be effective.20,21
The Work Limitations Questionnaire was included as part of the online survey to address on-the-job performance and the possible impact of chronic conditions and treatment. Worksite health promotion/ protection programs increasingly make an effort to document the impact of chronic health problems and their treatment on productivity. Thus, this 25-item questionnaire assessed how health may have affected workers performing certain parts of their jobs.22 Data on absenteeism were collected on an annual basis from the company human resource personnel or from the study participant depending on the method used by the business for compensating time, that is, sick time or paid time off.
Table 1.
Baseline Demographic Data for Be Hipp Intervention and Control Participants
| Intervention | Control | ||
|---|---|---|---|
| (N = 138) | (N = 142) | P | |
| Sex | |||
| Male | 38 | 29 | .2072 |
| Female | 100 | 113 | |
| Age | 49.4 | 50.6 | .2337 |
| Ethnicity | |||
| White | 132 | 139 | .3753 |
| Hispanic | 2 | 1 | |
| Black | 0 | 1 | |
| Asian | 4 | 1 | |
| Education | |||
| HS grad | 21 | 24 | .7199 |
| Tech/trade/AA | 48 | 43 | |
| College grad + | 69 | 75 | |
| Income | |||
| <15 000 | 1 | 0 | .2286 |
| 15–34, 999 | 13 | 21 | |
| 35–74, 999 | 46 | 52 | |
| 75 000 + | 68 | 58 |
Table 2.
Study Retention
| Intervention Arm | Control Arm | |||||
|---|---|---|---|---|---|---|
| Baseline | Intervention | Intervention | Baseline | Intervention | Intervention | |
| Year 0 | Year 1 | Year 2 | Year 0 | Year 1 | Year 2 | |
| Total recruitment | ||||||
| N Observations | ||||||
| 138 | 138 | 128 | 142 | 142 | 136 | |
| N Retained throughout year | ||||||
| 138 | 128 | 124 | 142 | 136 | 127 | |
| Excluded: Dropped out of study | ||||||
| 0 | 0 | 0 | 0 | 0 | 0 | |
| Excluded: Left employment | ||||||
| 0 | 10 | 4 | 0 | 6 | 9 | |
| Pregnancy leave during intervention | ||||||
| 0 | 1 | 1 | 0 | 0 | 1 | |
| % Data collected of retained(a) | ||||||
| 100 | 99 | 99 | 100 | 100 | 99 | |
| % Data collected of baseline year 0 | ||||||
| 100 | 92 | 89 | 100 | 96 | 89 | |
| Recruitment round 1 | ||||||
| N Observations | ||||||
| 33 | 33 | 32 | 36 | 36 | 35 | |
| N Retained throughout year | ||||||
| 33 | 32 | 32 | 36 | 35 | 33 | |
| Excluded: Dropped out of study | ||||||
| 0 | 0 | 0 | 0 | 0 | 0 | |
| Excluded: Left employment | ||||||
| 0 | 1 | 0 | 0 | 1 | 2 | |
| Pregnancy leave during intervention | ||||||
| 0 | 0 | 0 | 0 | 0 | 0 | |
| % Data collected of retained(a) | ||||||
| 100 | 100 | 100 | 100 | 100 | 100 | |
| % Data collected of baseline year 0 | ||||||
| 100 | 97 | 97 | 100 | 97 | 92 | |
| Recruitment round 2 | ||||||
| N Observations | ||||||
| 51 | 51 | 47 | 53 | 53 | 50 | |
| N Retained throughout year | ||||||
| 51 | 47 | 46 | 53 | 50 | 45 | |
| Excluded: Dropped out of study | ||||||
| 0 | 0 | 0 | 0 | 0 | 0 | |
| Excluded: Left employment | ||||||
| 0 | 4 | 1 | 0 | 3 | 5 | |
| Pregnancy Leave During Intervention | ||||||
| 0 | 1 | 0 | 0 | 0 | 0 | |
| % Data collected of retained(a) | ||||||
| 100 | 98 | 100 | 100 | 100 | 100 | |
| % Data collected of baseline year 0 | ||||||
| 100 | 90 | 90 | 100 | 94 | 85 | |
| Recruitment round 3 | ||||||
| N Observations | ||||||
| 54 | 54 | 49 | 53 | 53 | 51 | |
| N Retained throughout year | ||||||
| 54 | 49 | 46 | 53 | 51 | 49 | |
| Excluded: Dropped out of study | ||||||
| 0 | 0 | 0 | 0 | 0 | 0 | |
| Excluded: Left employment | ||||||
| 0 | 5 | 3 | 0 | 2 | 2 | |
| Pregnancy leave during intervention | ||||||
| 0 | 0 | 1 | 0 | 0 | 1 | |
| % Data collected of retained(a) | ||||||
| 100 | 100 | 98 | 100 | 100 | 98 | |
| % Data collected of baseline year 0 | ||||||
| 100 | 91 | 83 | 100 | 96 | 91 | |
Data not included for employees who went on pregnancy leave during the intervention.
Study timeline
Study intervention and control group description
The intervention arm included 138 employees who participated in interactive participatory monthly group sessions. There were a total of 10 intervention groups: 3 at the University, 4 at local businesses, and 3 from a regional business. The control arm included 142 employees from 5 different sites, 1 at the University, 3 for the local business, and 1 for the regional insurance company that received quarterly newsletters.
The intervention group included a novel interactive participatory half-hour session that used the key principles of self-determination theory: competency, autonomy, and relatedness to build motivation for lifestyle behavior change. Self-determination theory provided the theoretical framework for the design of the intervention and guided the manner in which each topic was addressed.23 The principles of self-determination theory were woven into each session. The group selected the topic for each of the monthly sessions with interactive discussions around these topics and facilitated by the study staff. Each session focused on 1 of 4 key topic areas: nutrition, physical activity, stress management, and ergonomics. See Table 3 for examples of session titles from each topic area.
Table 3.
Select Intervention Session Titles by Key Topic Area
| Topic Area | Session Title |
|---|---|
| Nutrition | Mindful eating |
| Snack attack | |
| Mediterranean eating style | |
| Vegetables: Variety and easy preparation ideas | |
| Physical activity | The power of moving |
| Personal choice and physical activity | |
| Strength training | |
| Building motivation for physical activity | |
| Stress management | Demand/control model of workplace stress |
| Strengthening type B behaviors for stress management | |
| Reducing stress through social support | |
| Stress/food craving connection | |
| Ergonomics | Recommended computer monitor placement |
| 1-min work stretches | |
| Keyboard/mouse positioning | |
| Ask the ergonomics expert—guest speaker |
The goal of group facilitators was to capitalize on the group process and build motivation for making healthful lifestyle choices. They encouraged group participants to share relevant life experiences, resources, and ideas for change. These sessions contrasted from the traditional didactic format of “lunch and learns,” which are typical in many worksite wellness programs. Traditional formats focus on giving information rather than discussing topics chosen and discussed by the employees.
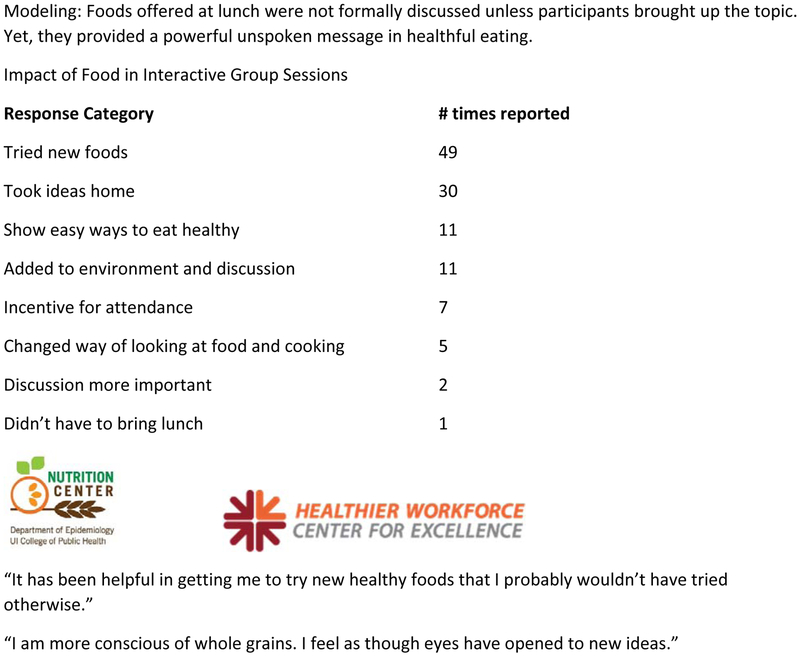
Modeling of healthy food choices was a central intervention strategy.24,25 A lunch featuring tasty, healthful food selections was provided at each intervention group session. While recipes were available for key items, group facilitators deliberately refrained from telling group members how healthy the menu items were. Rather, foods offered at lunch were not formally discussed unless participants brought up the topic. This approach provided an unspoken message that healthful eating is satisfying and enjoyable.
Participants in the control group received quarterly newsletters that addressed the intervention session topics covered during a 3-month period. Featured recipes during the same time period were also included. The newsletters were designed with a colorful layout and engaging format. The newsletters were delivered to university participants through campus mail. Newsletters were mailed to the businesses and distributed to participants through their mailbox or workstation.
Newsletters also served as a tool for notifying the research team that an employee had left the place of employment. A total of 17 employees in the control arm left their place of employment and, therefore, were no longer eligible for study participation. A study limitation is that we had no way of knowing whether participants actually read the newsletters. We did have a good response to end-of-study questions about the value of the newsletter.
Statistical analysis
The power calculation was based on summary scales from the SF-36v2 since there is an extensive literature for this instrument on its sensitivity in measuring clinically significant changes in scores.14 Power calculations were difficult with the other outcome measures since the intervention was novel and lacked the studies to be able to estimate effect size. Using the study design, 140 participants would be required in the intervention group and 140 participants in the control group to detect a 3-point difference in group scores for either the Physical Component Summary or Mental Components Summary scales of the SF-36v2. These sample sizes are based on α: .05, 2-tailed; power: 80% with variance estimates from the general US population. Two-point differences on both scales are clinically significant. For instance, persons with osteoarthritis in the Medical Outcomes Study had an average 2-point reduction in Physical Component Summary score over 1 year. As another example, persons in the Medical Outcomes Study who sustained a myocardial infarction had 1.6-point increase in Mental Components Summary score, on average, a year after myocardial infarction.
The emphasis of this study was on examining effects on primary outcomes-absenteeism, Physical Component Summary, and Mental Components Summary as measured by higher scores in the F-36v2, which are accepted and important measures in evaluating separate health protection and health promotion programs. Resource constraints limit sample size, thus limiting the statistical power to examine secondary outcomes. Nevertheless, secondary outcomes were examined from an exploratory perspective that could lead to future pilot studies.
Simple descriptive statistics were used to compare the intervention and control groups across all study population variables later used in regression models. T tests and χ2 statistics were used to assess differences at baseline between the intervention group and control group on sex, age, ethnicity, education, and income. Finally, descriptive statistics were used to compute overall study retention rates, including the proportion of individuals in the intervention and control arms who dropped out of the study, left employment, or became pregnant during the intervention.
Ordinary least squares regression models were used to estimate the effect of the intervention on employee absenteeism hours, comparing the intervention study arm with the control arm. The purpose of this analysis was to assess whether the Be Hipp intervention had an impact on reducing average annual absenteeism hours in the intervention arm in year 1 or year 2 after controlling for other factors. The control arm and baseline year were the referent groups. The model included as covariates the variables shown in Table 1 to control for the effects of age, gender, annual income, and education.
We chose not to control for race/ethnicity as there was not sufficient variation in this variable. In addition, we also controlled for BMI measured at baseline after participants gave their consent to join the study, as previously described. Finally, we included calendar year dummy variables to control for the external effect of secular trend. Two models were run: the first model included the entire population in the intervention and control arms; the second model excluded individuals who left employment, took pregnancy leave, or had missing BMI data (at any point during the 3-year study period).
RESULTS
This study used a cluster randomized design to minimize chance of the intervention and control groups differing in demographic characteristics: sex, age, ethnicity, education, and income. As Table 1 shows, the study groups were closely matched at baseline. The variables had a normal distribution and no additional transformations were necessary.
Study participant retention
Participant retention was high in both the intervention group (90%) and the control group (89%) as shown in Table 2. In fact, participant evaluations of the group sessions indicated an interest in the sessions continuing beyond the length of the study. Retention findings, based on attendance at the monthly sessions, show that participants were able to devote 30 minutes of time each month to a health promotion and protection program without interfering with their usual work routines at a retention rate of nearly 90% across a 2-year intervention.
Absenteeism
The estimated impact of the Be Hipp intervention on absenteeism hours in the intervention arm is shown in Table 4. The impact of baseline BMI, annual income, and college graduation status on absenteeism hours during the period is also shown. Results for both the entire population and restricted population models are displayed. There was no statistical difference in absenteeism hours between the intervention arm and control arm at baseline. The β coefficient on absenteeism hours for the intervention arm in year 1 for the entire population model was −6.63 (P = .114). Although not statistically significant at the conventional level of P value of less than .05, the estimate nears significance in year 1. The interpretation of the point estimate is that the impact of the intervention in year 1 was to reduce absenteeism by 6.63 hours per participant, all other factors held equal. None of the other results for the impact of the Be Hipp intervention on absenteeism hours in year 1 or year 2 for either model were close to achieving statistical significance.
Table 4.
Ordinary Least Squares Regression Model Results: Effect of Be Hipp Intervention on Absenteeism Hours(a)
| Restricted | ||
|---|---|---|
| Entire Population β | Populationb β | |
| Coefficient on | Coefficient on | |
| Absenteeism Hours | Absenteeism Hours | |
| Intervention Arm (vs control arm at baseline) | 1.432 (.744) | −1.226 (.793) |
| Intervention arm in year 1c | −6.632 (.114) | −2.326 (.597) |
| Intervention arm in year 2c | −6.758 (.304) | −3.224 (.634) |
| Body mass index (at baseline) | 0.886d (.002) | 0.810d (.005) |
| Annual Income ≥$50 000 (at baseline) | −8.446 (.060) | −8.851 (.057) |
| College graduate (at baseline) | −11.08d (.008) | −11.58d (.008) |
| Observationse | 789 | 717 |
Model controlled for age, gender, secular trend (year), baseline body mass index, annual income, and education.
Excluding individuals who left employment, took pregnancy leave, or had missing body mass index data.
Control arm and the baseline year are the referent groups.
P values (within parentheses) are clustered at the individual level (P < .01).
Observations are equal to number of participant-years.
The effect of the secondary covariates was also examined, included as control variables and measured at baseline. The results showed that college graduates had significantly (P <.01) lower absenteeism hours, with 11.1 to 11.6 fewer hours absent from work per individual per year. Also, those earning an annual income of $50 000 or more at baseline had results nearing statistical significance (P = .06), with fewer hours absent than those earning less than $50 000 annually. Finally, those individuals at higher baseline BMI had significantly (P < .01) more absenteeism hours throughout the time period. In fact, for every 1 unit increase in baseline BMI, there was a 0.81 to 0.90 unit increase in absenteeism hours per individual per year.
Participant exit questionnaire
At the final data collection visit, participants were asked to complete an open-ended 6-question survey on the influence of Be Hipp on health behaviors and their satisfaction with the program. Survey results were coded into themes for qualitative analysis. Figure 2 shows that participants in the group intervention sessions tried new foods and took ideas home. Be Hipp participants in both groups commonly reported increased awareness and knowledge about health and wellness topics. Employees indicated personal interaction as an important component in wellness programming. Action oriented behaviors—such as improved eating habits and increased physical activity—were more commonly cited among participants in the intervention group than in the newsletter group (data not shown).
Figure 2.
Participant survey-intervention. From Healthier Workforce Center for Excellence. Used with permission.
DISCUSSION
There are few current studies that include the combination of worksite health protection and promotion combined with high levels of employee participation. It is difficult to compare our study with others where knowledge dissemination was more of a focus than lifestyle change with active participant involvement. The 3 studies that most clearly represent the focus of our study intervention are contrasted with our study in terms of retention; none of these studies looked at absenteeism, the second outcome emphasized in this article.
For our study, one of the key positive outcomes involved the high retention rates throughout this intervention. Comparing our study with the research conducted by Tsutsumi et al,10 with both studies using a participatory approach, our 90% participation rates are substantially greater than the 50% participation in the target population of the Tsutsumi study. The study by Tsutsumi et al indicated that more women than men and older rather than younger workers were lost to follow-up. This retention difference in gender and age was not an observation in the study presented here. As the researchers in the study by Tsutsumi et al indicated, exaggerated or reduced associations may occur given their small sample size. It should also be noted that the study by Tsutsumi et al focused on mental health, environmental improvement, and job redesign rather than retention and absenteeism, thus making the objectives and corresponding outcomes different from our study.
A second study conducted by Eriksen and colleagues11 focused on stress management and physical exercise using an integrated participatory health program. While the original study design was a randomized controlled trial, the retention rates in the intervention arm of the study were quite low, with 20% of the participating workers dropping out of the intervention. This dropout rate is a concern and in stark contrast to the 90% participation rate of the study presented here.
A third study by Konradt and colleagues12 involved teleworkers and focused on stress, strain, and coping styles using an intervention that minimally emphasized worker participation. Researchers in this study contacted 50 teleworkers requesting participation with 17 agreeing and only 11 answering questionnaires that would contribute data. These data were compared with those of 12 teleworkers in a control group. The researchers do not identify why only 17 teleworkers agreed to participate and why 6 members of this group of 17 dropped out of the study. The sessions in this study by Konradt et al lasted for 5 hours with a 1-hour break, making this a very different type of session from the ones described here. The study by Konradt et al appeared to have less involvement by the workers in making decisions about topics to be discussed.
Limitations
The study presented in this article was limited by the economic downturn in our state at the time of study recruitment. Eliciting study subjects’ participation was more difficult given concerns about layoffs and job eliminations. In addition, we were in the midst of a flood during our recruitment process with added concerns due to difficulties getting to the worksite for a period of time and loss of space due to building renovations following the flood. Remaining flexible to accommodate changing environmental/economic events is an important aspect of worksite research. When it is difficult for an employee to participate in a program, building in the ability for participants to negotiate a plan to remain in the study is important, that is, e-mail follow-up for interactive sessions and data collection visits.
CONCLUSION
The Self-Determination Theory provided the framework for a highly interactive and integrated intervention. Although not statistically significant, estimates for absenteeism hours were in the right direction and nearing significance in the first intervention year. In addition, this study showed a high rate of retention throughout the 3-year study period. Therefore, programs that encourage active learning while providing autonomy to decide how to incorporate health behavior change seem to increase long-term participation. These findings may have implications in the design of future research to study worksite wellness programs.
Figure 1.
Figure 1 presents the study timeline with enrollment, intervention sessions, and control newsletters shown for each of the study site types: The University of Iowa, 5 local businesses, and 1 regional business. The study was conducted over the course of 5 years with enrollment of the 3 study site types staggered along with additional rounds of recruitment due to unforeseen challenges listed previously.
Acknowledgments
The authors acknowledge all of the participants in this study who made their data collection possible. The authors also acknowledge Maria O. Scott, MPH, for her assistance in finalizing this article. Centers for Disease Control and Prevention funded this research (grant # 1U19OH008868). The authors have no pharmaceutical or industry support. The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
REFERENCES
- 1.Parks KM, Steelman LA. Organizational wellness programs: a meta-analysis. J Occup Health Psychol.2008;13(1):58–68. [DOI] [PubMed] [Google Scholar]
- 2.Esmaeilzadeh S, Ozcan E, Capan N. Effects of ergonomic intervention onwork-related upper extremity musculoskeletal disorders among computer workers: a randomized controlled trial. Int Arch Occup Environ Health. 2014;87(1):73–83. [DOI] [PubMed] [Google Scholar]
- 3.Gazmararian JA, Elon L, Newsome K, Schild L, Jacobson KL. A randomized prospective trial of a worksite intervention program to increase physical activity. Am J Health Promot. 2013;28(1):32–40. [DOI] [PubMed] [Google Scholar]
- 4.Loeppke RR, Schill AL, Chosewood LC, et al. Advancing workplace health protection and promotion for an aging workforce. J Occup Environ Med. 2013;55(5):500–506. [DOI] [PubMed] [Google Scholar]
- 5.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karlqvist L, Gard G. Health-promoting educational interventions: a one-year follow-up study. Scand J Public Health. 2013;41(1):32–42. [DOI] [PubMed] [Google Scholar]
- 7.Katz DL, O’Connell M, Yeh MC. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep. 2005;54(RR-10):1–12. [PubMed] [Google Scholar]
- 8.Kazutaka K. Practical ways to facilitate ergonomics improvements in occupational health practice. Hum Factors. 2012;54(6):890–900. [DOI] [PubMed] [Google Scholar]
- 9.Stokes GC, Henley NS, Herget C. Creating a culture of wellness in workplaces. N C Med J. 2006;67(6):445–448. [PubMed] [Google Scholar]
- 10.Tsutsumi A, Nagami M, Yoshikawa T, Kazutaka K, Kawakami N. Participatory intervention for workplace improvements on mental health and job performance among blue-collar workers: a cluster randomized controlled trial. J Occup Environ Med. 2009;51:554–563. [DOI] [PubMed] [Google Scholar]
- 11.Eriksen HR, Ihlebaek C, Mikkelsen A, Gronningsaeter H, Sandal GM, Ursin H. Improving subjective health at the worksite: a randomized controlled trial of stress management training, physical exercise and an integrated health programme. Occup Med. 2002;52(7):383–391. [DOI] [PubMed] [Google Scholar]
- 12.Konradt U, Schmook R, Wilm A, Hertel G. Health circles for teleworkers: selective results on stress, strain and coping styles. Health Educ Res. 2000;15(3):327–338. [DOI] [PubMed] [Google Scholar]
- 13.Hill A, Korolkova A. Employee wellness programs: collegiate recreation trends research. NIRSA White Paper. 2014; April: 1–25. http://www.nirsa.org/docs/Discover/Research/NIRSA_Employee_Wellness-Whitepaper-2014.pdf. Accessed October 28, 2014. [Google Scholar]
- 14.Turner-Bowker DM, Bartley BJ, Ware JE. SF-36 R Health Survey and “SF” Bibliography: Third Edition (1988–2000). Lincoln, RI: QualityMetric Incorporated; 2002. [Google Scholar]
- 15.Karasek RA, Gordon G, Pietroskovsky C, Frese M, Pieper C, Schwartz J. Job Content Instrument: Questionnaire and User’s Guide. Los Angeles/Lowell, MA: University of Southern California/University of Massachusetts; 1985. [Google Scholar]
- 16.Kuorinka I, Jonsson B, Kilbom A, et al. Standardized Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. [DOI] [PubMed] [Google Scholar]
- 17.Committee to Assess Worksite Preventive Health Program Needs for NASA Employees. Integrating Employee Health—A Model Program for NASA. Washington, DC: Institute of Medicine; 2005. [Google Scholar]
- 18.Fried V, Prager K, MacKay A, Xia H. Chartbook on Trends in the Health of Americans. Health, United States, 2003. Hyattsville, MD: National Center for Health Statistics; 2003. [Google Scholar]
- 19.Giovino G, Pederson L, Trosclair A. The prevalence of selected cigarette smoking behaviors by occupation in the United States In: The National Institute for Occupational Safety and Health (NIOSH), ed. Work, Smoking and Health: A NIOSH Scientific Workshop. Washington, DC: 2000. [Google Scholar]
- 20.Bernard BP. In: NIOSH, ed. Musculoskeletal Disorders and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back.Washington, DC: U.S. Department of Health & Human Services; 1997. [Google Scholar]
- 21.National Research Council, Institute of Medicine. Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities. Washington, D.C.: National Academy Press; 2001. [PubMed] [Google Scholar]
- 22.Lerner DJ, Amick BC III, Rogers WH, Malspeis S, Bungay K. The Work Limitations Questionnaire: a self-administered instrument for assessing on-the-job work disability. Med Care. 2001;39(1):72–85. [DOI] [PubMed] [Google Scholar]
- 23.Patrick H,Williams GC. Self-determination theory: its application to health behavior and complementarity with motivational interviewing. Int J Behav Nutr Phys Act. 2012;9:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cruwys T, Bevelander KE, Hermans RC. Social modeling of eating: a review ofwhen and why social influence affects food intake and choice [published online ahead of print August 28, 2014]. Appetite. 2015;86:3–18. doi: 10.1016/j.appet.2014.08.035. [DOI] [PubMed] [Google Scholar]
- 25.Couch SC, Glanz K, Zhou C, Sallis JF, Saelens BEJ. Home food environment in relation to children’s diet quality and weight status. Acad Nutr Diet. 2014;114(10):1569–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]