Abstract
Background
Facing the social panic and substantial shortage of medical resources during the coronavirus disease 2019 (COVID-19) outbreak, providing psychological first-aid to inpatients is essential for their rehabilitation and the orderly operating of medical systems. However, the closed-ward environment and extreme shortage of onsite mental health workers have limited the use of traditional face-to-face diagnosis and psychological interventions.
Aim
To develop a mental health intervention model for inpatients that can be applied during a widespread epidemic, such as COVID-19.
Methods
In a medical team stationed in Leishenshan Hospital, Wuhan, China, we integrated onsite and online psychological support resources to implement a graded psychological intervention system. The onsite psychiatrist established trust with the patients and classified them into categories according to their symptom severity. While face-to-face evaluation and intervention are critical for effective online support, the online team effectively extended the scope of the ‘first-aid’ to all patients.
Conclusion
This integrated onsite and online approach was effective and efficient in providing psychological interventions for inpatients during the crisis. Our model provides a realistic scheme for healthcare systems in or after the COVID-19 epidemic and also could be adopted in areas of the world with insufficient mental healthcare resources.
Keywords: mental health, depression
Strengths and limitations of this study.
This study presents a practical and resource-efficient model of psychological intervention for inpatients in a big disaster, such as the COVID-19 epidemic. This study demonstrates a real-world application of integrated online- and onsite-psychological intervention.
The effectiveness of the program should be further examined using case-control studies.
Inpatients with COVID-19 need psychological first-aid
The sudden outbreak of COVID-19 (a highly infectious disease with about a 6% mortality rate), as well as the substantial shortage of local healthcare providers, personal protective equipment (PPE) and resuscitation devices, has led many to experience panic.1 2 At the end of January 2020, people in Wuhan flooded to the hospitals for diagnosis and treatment, waited in long lines for a hospital bed, witnessed sudden death and suffered from the illness itself. A study in China found that in the first 2 months of 2020, patients with COVID-19 widely suffered from anxiety, depression and other stress-related symptoms.3 Studies have shown that psychological reactions due to catastrophic events have adverse effects on physical recovery.4 Early psychological intervention through face-to-face care and support can help rebuild trust and self-confidence, reduce physical and mental symptoms and prevent post traumatic stress disorder (PTSD).5 The WHO suggested that psychological first-aid should be provided to those who were impacted when a disaster occurred, as well as in the days or weeks following the disaster, with particular focus on groups that need more attention, including those who lack social support and who are severely affected and in poor health condition.6
Difficulties in providing regular psychological first-aid
Compared with the usual settings for psychological intervention, we faced the following difficulties in providing psychological first-aid to inpatients in this disaster. First, there was a considerable imbalance between the very limited number of psychological healthcare workers and the widespread, emergent needs of the inpatients. While most of the local mental health workers in Wuhan had been exhausted from the great increase of help seekers, the number of psychological workers from the reinforcement medical teams was limited. There were only 250 professional mental health workers (around 0.625%) in the reinforcement medical teams to Hubei Province, China. In our case, the first author of this paper was the only psychiatrist in a 156-member medical team, which took charge of more than 90 beds in two general wards and 32 beds in the intensive care unit wards in Leishenshan Hospital, Wuhan, China. In contrast, stress-related and trauma-related symptoms were common to inpatients.3 This discrepancy between clinical demands and limited resources calls for a highly efficient solution.
Second, the psychological difficulties of patients changed rapidly, requiring interventions to adapt to their needs in a timely fashion. At the early stage of the pandemic, most of the psychological distress came from the considerable insufficiency of healthcare resources and panic in the community. Many patients had experienced the panic wave of rushing to hospitals and waiting for hospitalisation at the end of January; most patients had family members who were infected and some patients had witnessed or heard of the sudden deaths of their family members due to the infection. Later on, the major stressors changed to uncertainties in the treatment and recovery processes. Some patients worried they would be kept in the hospital for a very long period due to their infection or even afraid of being thrown away by society, and some were exhausted by the constantly updating test standards. As a result, most of the patients who filled out our questionnaires reported stress symptoms, such as increased vigilance, depression, anxiety, irritability, flashbacks and nightmares, feelings of being discriminated against, or rejected, and loneliness. These symptoms fluctuated periodically due to ever changing stressors and aggravated the patients' chest distress, palpitations, and other physical symptoms. These dynamic changes and the considerable individual variability have challenged the traditional intervention approaches.
Third, the closed-ward environment has impacted the effectiveness of psychological interventions and limited the application of face-to-face psychological interventions. The design of the infectious disease hospital emphasised biomedical safety and fast-construction (The Leishenshan Hospital had 2000 beds and was built in 10 days), at the cost of comfortableness. In the closed ward with white board walls and various ventilation pipes on the roof, patients may feel they were in the temporary plank house on a construction site. This environment could induce depression and uneasiness in patients. Further, the closed wards make it difficult for face-to-face communication with the patients. Wearing air-tight PPE with protective glasses, one would have to bear pressure on the lips and foggy glasses when talking.
Taken together, the above factors have substantially limited the application and effectiveness of the traditional face-to-face psychological diagnosis and interventions. It is essential to develop a highly efficient psychological first-aid scheme that can provide full coverage for patients’ psychological difficulties.
Development of an onsite-online psychological first-aid model
A potential solution to overcome the shortage of onsite psychological health workers and facilitate communication with patients is a web-based psychological intervention. However, the effectiveness of web-based psychological first-aid is influenced by a few factors. First, in only using an online intervention, mental health workers outside Hubei Province were unlikely to understand the specific experience and related stress symptoms of patients with COVID-19 as opposed to more conventional mental symptoms. Furthermore, the communications only through online chat were not effective in establishing trust, which is critical for effective intervention, especially in or after disaster. Therefore, a combination of onsite and online methods is necessary to elaborate the advantages of both online and face-to-face psychological intervention.
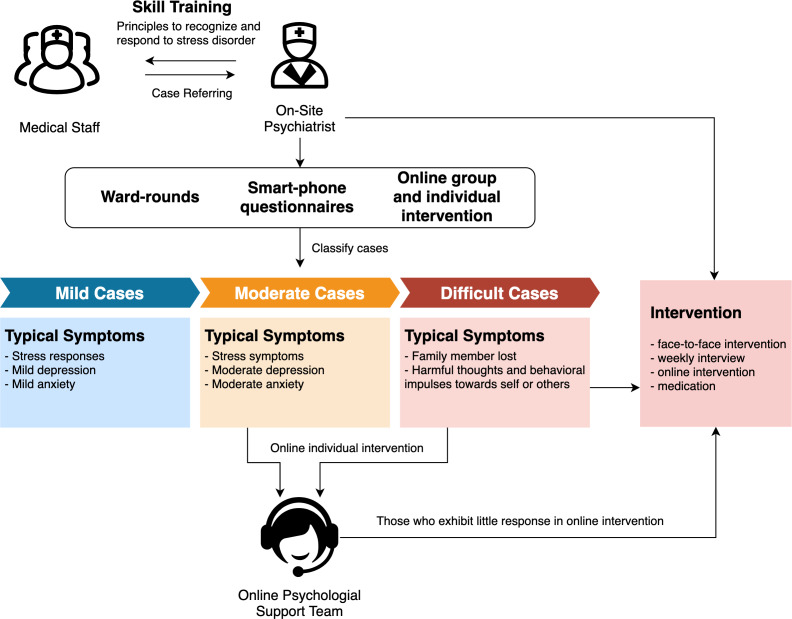
Figure 1 presents a scheme of our integrated onsite-online psychological intervention model. We first organized an online mental health team with 35 qualified psychotherapists recruited from the whole country, coordinated by an onsite psychiatrist. A rapid assessment, sorting and treatment process was developed by integrating online and offline methods. The psychiatrist went into the ward and briefly communicated with each patient to establish initial trust and categorised the patients into different conditions for appropriate interventions. The information regarding the conditions of the patients was transferred to the online team.
Figure 1.
Integrated onsite and online psychological intervention model.
We invited the patients to join online chat groups using their smartphones. The groups were provided with psychoeducation, as well as simple methods based on cognitive behavioural therapy techniques and social support. Discussions were led regarding what stress and trauma reactions or symptoms are, how to overcome the feelings of fear, helplessness, guilt, how to cope with symptoms and how to deal with the feelings of being discriminated. We also provided information to the patients on rehabilitation, emotional regulation and sleep. Another critical role of the online chat group was that we identified individuals who needed further individualised interventions. In addition, the onsite psychiatrist’s weekly follow-up rounds provided necessary onsite help for some difficult cases and maintained the effectiveness of the online consultation for other patients.
We also provided educational online talks and learning materials to other medical staff working at the same site. The information helped the medical staff to identify stress-related symptoms in their daily communications with the patients, so that they could refer patients to the onsite psychiatrist for further diagnosis and intervention.
Essential factors in the model and practical recommendations
The heart of this psychological first-aid model is the integration and coordination of onsite and online mental health resources. While face-to-face evaluation and intervention are critical for effective online support, the online team effectively extended the scope of the psychological first-aid to all patients.
Establishing the initial trust with the patients in the first brief contact is an essential point to ensure the effectiveness of the online intervention. We found that a high frequency of online individual psychocounselling, at least three sessions per week, at the beginning were usually required for patients who need it. We found that establishing the initial trust with the patients in the first brief contact is essential to make the online consultation effective. For more accessible communication in a closed ward, the onsite psychiatrist wrote her name and department on the protective gown to let the patients know her quickly by reading the text besides oral self-introduction. It is important for patients who have poor identification and orientation due to anxiety to build relationship and trust quickly. By starting from asking brief semiopen questions such as, ‘Did you sleep well? How is your appetite?’, the onsite psychiatrist could perform the initial evaluation and sort patients with different mental conditions without irritating patients (figure 1). Weekly follow-up rounds are also necessary to maintain the depth of the online consultation. For patients who had lost a family member(s), depressive patients who had negative thoughts or passive behaviors or patients who tended to meltdown due to severe anxiety, an offline session could often lead to a significant improvement.
The efficient communication and understanding between the onsite psychiatrist and the online team is another essential factor in the model. With the ward rounds, the onsite psychiatrist got the first-hand information of the conditions of the patients and timely transferred a summary table to the online team. During shift meetings, the onsite psychiatrist and the online team worked through each patient’s case to discuss the symptoms and potential intervention strategies for the patient. These shift meetings ensured the alignment of the onsite and online teams to provide precise and effective interventions to all patients.
Voices from the inpatients
The self-reports from the patients support the effectiveness of this model. Many patients have proactively written thank-you letters to the psychiatrist to express their improvements. They commented: ‘Not only was my body treated but also the heart’; ‘In my most difficult time, I was pulled up by a psychiatrist; thus, I did not fall into the black hole due to the disease and fear’ and ‘When I first came here, I felt very nervous, feeling increased chest distress and palpitations. It was psychological counselling that helped me in time to adjust my emotions. It was the first time for me to feel the spirit is the primary weapon of recovery against the backdrop of this disaster.’
In one case, the patient lost his father in the outbreak, and his infected mother, who was also in quarantine, was unaware of her husband's death. The patient had moderate depressive symptoms according to the questionnaire, but he was very passive in expressing himself during the first contact and following online counselling. However, continuous online contacts helped to build trust between him and the psychiatrist gradually. In the second week of offline consultation, the patient burst into tears and talked about his sorrow and worry. After that, his online interactions became active, and his symptoms improved. Our practice shows that, in the case of insufficient professional staff on site, the programme we created was suitable for the psychological assistance of socially isolated patients during the sudden outbreak of this highly infectious disease.
Implications
Many countries have reached a consensus on the goal and significance of psychological assistance for large-scale disasters, and that the implementation needs to be more flexible according to the characteristics of the disasters and accessibility of medical resources. The outbreak of the COVID-19 pandemic is a severe challenge to resources related to psychological services and routine diagnosis and treatment in various countries. We feel that this combination of onsite and online approaches can achieve more efficient psychological interventions for promoting rehabilitation, facilitating psychological adaptation and preventing PTSD. This model has been adopted from several wards to the whole hospital with more than 2000 beds. We believe it could be adopted and adapted further all over the world in a similar dangerous disaster situation which lacks onsite mental health workers, and also in the areas, countries or cultures where mental healthcare is underdeveloped and resources are scarce. Further well-designed research is needed to demonstrate efficacy of this model in the future.
Biography
Wenhong Cheng is the chief physician of Department of Psychiatry at Shanghai General Hospital and the associate chief physician of the Department of Child and Adolescent Psychiatry at Shanghai Mental Health Center, both affiliated to Shanghai Jiao Tong University School of Medicine. She is a psychiatrist as well as a psychotherapist. She is the deputy director of the Cognitive-Behavioral Therapy group, and the Child and Adolescent Psychiatry Group of the Chinese Psychiatrist Association. She is also the director of the Child and Adolescent Psychiatry group of the Shanghai Medical Association. In addition, she is the director of the Mental Health Group of the Lei Shen Shan Hospital in Wuhan, China. Her main research interests include the psychopathological mechanisms and psychological intervention effects of childhood anxiety and mood disorders, and trauma related mental health.
Footnotes
Contributors: WC: study design, data collection, data interpretation, literature search, writing. FZ: data collection, data interpretation, data analysis. YH: study design, data interpretation. ZY: data interpretation, data analysis, figures, writing. JL: study design, data interpretation.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon request.
References
- 1.Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 2020;33:e10021:e100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao Q, Hu C, Feng R, et al. Investigation of the mental health of patients with novel coronavirus pneumonia. Chin J Neurol 2020;53. [Google Scholar]
- 3.Ryder AL, Azcarate PM, Cohen BE. Ptsd and physical health. Curr Psychiatry Rep 2018;20:116. 10.1007/s11920-018-0977-9 [DOI] [PubMed] [Google Scholar]
- 4.Birur B, Moore NC, Davis LL. An evidence-based review of early intervention and prevention of posttraumatic stress disorder. Community Ment Health J 2017;53:183–201. 10.1007/s10597-016-0047-x [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Psychological first aid: guide for field workers, 2011. Available: https://apps.who.int/iris/bitstream/handle/10665/44615/9786188273719-gre.pdf
- 6.Inter-Agency standing Committee reference group for mental health and psychosocial support in emergency settings. Briefing note on addressing mental health and psychosocial aspects of COVID-19 outbreak 2020:1–20.