Abstract
Objectives
We aimed to systematically review the published literature regarding adults with clinical suspicion of pneumonia that compares the accuracy of lung ultrasonography (LUS) performed by non-imaging specialists to other reference standards in diagnosing and evaluating the severity of community-acquired pneumonia. Moreover, we aimed to describe LUS training and the speciality of the physician performing LUS, time spent on the LUS procedure and potential harms to patients.
Materials and methods
We searched MEDLINE, Embase, CINAHL, Web of Science and Cochrane Central Register of Controlled Trials up until May 2019. We included studies that used LUS to diagnose pneumonia, but also confirmed pneumonia by other means. Publications were excluded if LUS was performed by a sonographer or radiologist (imaging specialists) or performed on other indications than suspicion of pneumonia. Two review authors screened and selected articles, extracted data and assessed quality using Quality Assessment of Diagnostic Accuracy Studies 2.
Results
We included 17 studies. The sensitivity of LUS to diagnose pneumonia ranged from 0.68 to 1.00; however, in 14 studies, sensitivity was ≥0.91. Specificities varied from 0.57 to 1.00. We found no obvious differences between studies with low and high diagnostic accuracy. The non-imaging specialists were emergency physicians, internal medicine physicians, intensivists or ‘speciality not described’. Five studies described LUS training, which varied from a 1-hour course to fully credentialed ultrasound education. In general, the methodological quality of studies was good, though, some studies had a high risk of bias.
Conclusion
We found significant heterogeneity across studies. In the majority of studies, LUS in the hands of the non-imaging specialists demonstrated high sensitivities and specificities in diagnosing pneumonia. However, due to problems with methodology and heterogeneity there is a need for larger studies with uniform and clearly established criteria for diagnosis and blinding.
PROSPERO registration number
Prospectively registered in PROSPERO (CRD42017057804).
Keywords: ultrasonography, respiratory infections, general medicine (see internal medicine), primary care
Strengths and limitations of this study.
This is the first systematic review to focus specifically on lung ultrasonography to diagnose community-acquired pneumonia in adults in the hands of non-imaging specialists physicians working clinically.
We rigorously followed the Cochrane recommendations for conducting systematic literature reviews and searched five major databases using a broadly defined search string.
We distinguished between imaging specialists defined as sonographers or radiologists and non-imaging specialist defined as physician working clinically, even though some physicians working clinically may have an experience with ultrasonography similar to that of an imaging specialist.
Introduction
Community-acquired pneumonia (CAP) is a frequent and serious health concern, leading to increased morbidity and mortality if not detected and treated properly.1 2 CAP accounts for 2.5% of all patient contacts in Danish general practice3 and globally causes countless hospital admissions, laboratory tests and imaging procedures.4
Today, the typical imaging procedures for diagnosing pneumonia are CT scan of the chest and chest X-ray (CXR), with CT considered the gold standard.5 However, far from all patients have these imaging procedures performed due to high radiation dose, high costs and low availability.6
An alternative mode of imaging is lung ultrasonography (LUS). The advantages of LUS are absence of radiation, high availability and low cost.7 Moreover, LUS can be performed as a bedside point-of-care test to supplement the physician’s clinical examination. Numerous reviews and meta-analyses indicate that LUS has excellent accuracy for the diagnosis of pneumonia in adults.8–13 None of the existing literature, however, differentiates between LUS operators despite the fact that ultrasound generally is considered a highly user-dependent imaging modality.14 To our knowledge, no previous review has focussed solely on the accuracy of LUS in the hands of physicians working clinically.
The aim of this study was to systematically review the published literature regarding adults with clinical suspicion of pneumonia that compares the accuracy of LUS performed by physicians working clinically (non-imaging specialists) to other reference standards in diagnosing and evaluating the severity of CAP. Moreover, to describe LUS training and the speciality of the physician performing LUS, time spent on the LUS procedure and potential harms to patients.
Methods
Data sources and search strategy
This review was prospectively registered in PROSPERO. We followed the Cochrane guideline15 for conducting a systematic literature review, and the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline for reporting the results. The literature search was conducted by a medical librarian and JJS in February 2017 and updated in May 2019. We searched the following databases: MEDLINE and Embase via Ovid, CINAHL via Ebsco, Web of Science and Cochrane Central Register of Controlled Trials.
The search terms ‘ultrasonography’ and ‘pneumonia’ were used in combination and with thesaurus terms (online supplementary e-appendix 1). Reference lists of included articles and identified reviews were evaluated manually for further eligible studies. Patients or the public were not involved in our research. All data relevant to the study are included in the article or uploaded as online supplementary information.
bmjopen-2019-036067supp001.pdf (2MB, pdf)
Eligibility and selection of studies
Studies were eligible if a full-text paper with original data was available, the paper described the use of LUS for diagnosing CAP in adults (≥18 years) and the diagnosis of CAP was confirmed by other means, for example, other imaging. Hence, we included all diagnostic accuracy studies that used any reference standard other than LUS. Studies were excluded if not published in English, Danish, Norwegian, or Swedish, if LUS was performed on other indications than suspicion of pneumonia, if LUS was performed by an imaging specialist or if the pneumonia was considered to be ventilator-associated or nosocomial. We defined an imaging specialist as a sonographer or radiologist, and a non-imaging specialist as a physician working clinically.
Two review authors (JJS and PSH or MPH) independently screened the titles and abstracts of all studies identified. Any disagreements were resolved by consensus or by consulting other review authors (CAA and MBJ).
Two review authors (JJS and PSH or MPH) independently extracted data using an adapted version of the Cochrane data exaction template (online supplementary e-appendix 2). We contacted study authors when information about the physician performing the LUS was incomplete or missing, or if important data could not be derived directly from the published study.
Methodological assessment
Methodological quality of the selected studies was evaluated according to the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2).16 Two reviewers (JJS and PSH or MPH) independently performed the assessment of methodological quality. Any disagreements were resolved by consensus or by consulting a third review author (CAA).
Patient and public involvement
No patient involved.
Results
The database search identified 7285 individual, non-duplicate articles, and one potential article was identified through the reference lists (figure 1). Twelve studies had little or no information about the physician performing LUS17–28 and we contacted the corresponding authors of these studies. Based on additional information provided by the study authors, two studies were included18 27 and two studies were excluded.21 25 No elaboration was available for the remaining eight studies. They were thoroughly assessed and four were included, as they clearly described the scanning physicians as a non-imaging specialist physician working clinically.17 19 20 22 The remaining four studies were excluded.23 24 26 28
Figure 1.
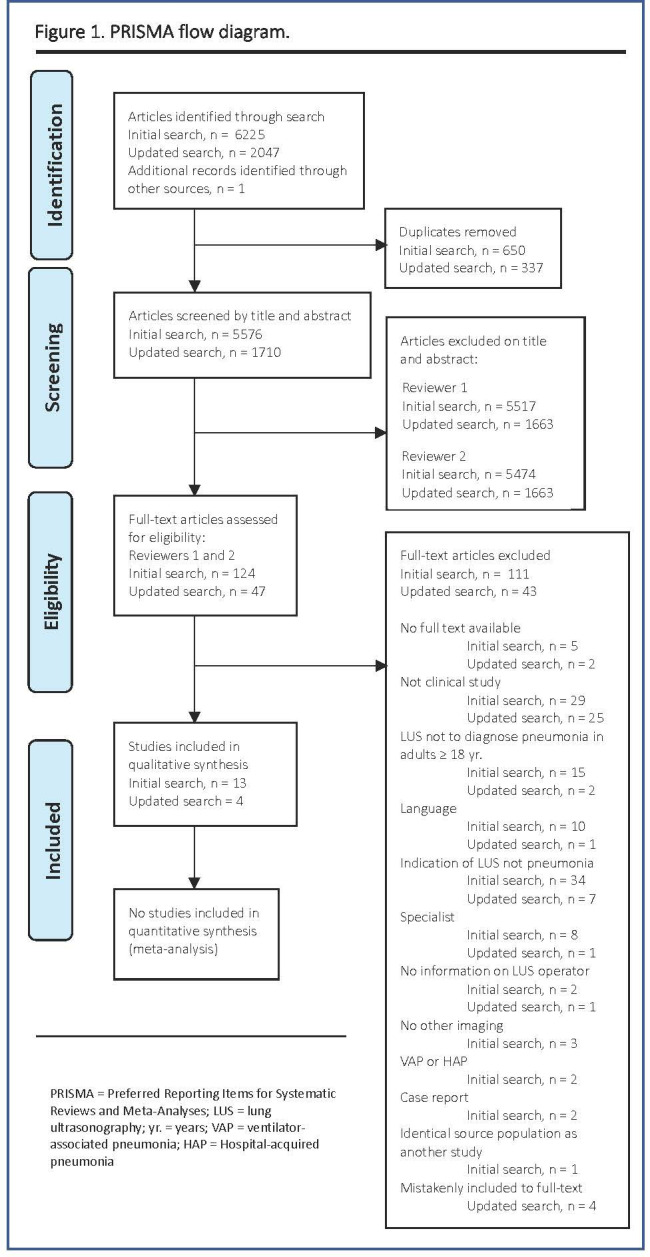
PRISMA flow diagram. HAP, hospital-acquired pneumonia; LUS, lung ultrasonography; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; VAP, ventilator-associated pneumonia; yr, years.
One study included both patients with CAP and nosocomial pneumonia.29 However, data on the CAP subgroup was obtained by correspondence with the study authors.
In total, 17 studies describing LUS in the hands of the non-imaging specialist to diagnose CAP in adults were included17–20 22 27 29–39 (figure 1).
Study characteristics
The studies were published between 1996 and 2019; 16 were prospective diagnostic accuracy cohort studies, and one was a retrospective study27 (online supplementary e-table 1).
The majority of studies included patients admitted to hospital, although one multi-centre study enrolled both hospitalised patients and outpatients20 (table 1). The studies included between 11 and 356 adult patients with a mean age from 34.0 to 84.8 years, of whom between 47% and 93% were men. Two studies included only patients aged ≥65 years.27 36
Table 1.
Diagnostic accuracy of LUS
| Study | Setting | Reference standard | Hours or days of LUS training | Experience in LUS or US in general | Pneumonia positive (n) / Total number of patients examined for pneumonia (N) | Sensitivity (95% CI) | Specificity (95% CI) |
| Amatya et al38 | ED | CT | 1 hour | 1 week | 44/62 | 0.91 (0.78 to 0.98)§ | 0.61 (0.36 to 0.83)§ |
| Corradi et al18 | ED | CT | – | >10 years* | 44/62† | 0.68 (0.52 to 0.81)§ | 0.95 (0.75 to 1.00)§ |
| Fares et al22 | ICU | CT | – | – | 30/38 | 0.93 (0.78 to 0.99)§ | 0.75 (0.35 to 0.97)§ |
| Karimi et al39 | ED | CT | – | – | 280/280 | 0.94 (0.90 to 0.96) | Not calculable |
| Liu et al31 | ED | CT | 28 hours | >50 scans | 112/179 | 0.95 (0.89 to 0.98)§ | 0.99 (0.92 to 1.00)§ |
| Nazerian et al32 | ED | CT | – | >1 year | 87/285 | 0.83 (0.73 to 0.90) | 0.96 (0.92 to 0.98) |
| Taghizadieh et al35 | ED | CT | – | – | 29/30 | 1.00 (0.95 to 1.00) | Not calculable |
| Parlamento et al34 | ED | CXR/CT | – | >10 years | 32/49 | 0.97 (0.84 to 1.00)§ | No conclusive data |
| Reissig et al20 | Multicentre‡ | CXR/CT | – | >100 scans | 226/356 | 0.93 (0.89 to 0.96) | 0.98 (0.89 to 0.96) |
| Unluer et al37 | ED | CXR/CT | 6 hours | – | 28/72 | 0.96 (0.82 to 1.00) | 0.84 (0.70 to 0.93) |
| Benci et al17 | Department of infectious diseases | QA | – | – | 37/80 | 1.00 (0.91 to 1.00)§ | 1.00 (0.92 to 1.00)§ |
| Bitar et al29 | ICU | QA | – | – | 11/11 | 0.99a | 0.80a |
| Bourcier et al30 | ED | QA | 2 days | – | 123/144 | 0.95 (0.90 to 0.98)§ | 0.57 (0.34 to 0.78)§ |
| Cipollini et al27 | Medicine /geriatric ward |
QA | – | >1 year | 128/128 | 0.82 (0.74 to 0.88)§ | Not calculable |
| Cortellaro et al19 | ED | QA | – | – | 81/120 | 0.99 (0.93 to 1.00) | 0.95 (0.83 to 0.99) |
| Pagano et al33 | ED | QA | – | >2 years | 68/105 | 0.99 (0.94 to 1.00) | 0.65 (0.56 to 0.67) |
| Ticinesi et al36 | Geriatric ward | QA | – | >1 year | 97/169 | 0.92 (0.86 to 0.97) | 0.94 (0.89 to 0.99) |
*Data collected by correspondence with author.
†Hemithoraxes.
‡Two university hospitals, seven hospitals of internal medicine, one hospital of pulmonary medicine, two practices, two EDs.
§95% CI calculated from true positives, false negatives, true negatives and false negatives. (Clopper-Pearson method).
-, not described; CXR, chest X-ray; ED, emergency department; ICU, intensive care unit; LUS, lung ultrasonography; QA, qualitative assessment; US, ultrasonography.
The signs and symptoms of pneumonia described in the American Thoracic Society guidelines (cough, pleuritic pain, sputum production, fever and dyspnoea) were used as inclusion criteria in nine studies19 20 22 29 31 33–36 and six studies based inclusion on comparable, but not identical, criteria.17 27 30 37–39 The remaining two studies only included patients with respiratory complaints like cough, dyspnoea, chest pain or haemoptysis leading to a chest CT being ordered.18 32
Definition of pneumonia based on LUS varied across studies. Still, presence of subpleural or alveolar consolidation or a tissue-like lesion was part of the definition in all studies except one, in which no definition was described.35 The physicians performing and interpreting LUS were generally blinded to the reference standard; however, in four studies, this matter was unclear.17 22 27 35 The definitions of pneumonia, blinding, scanning procedure and characteristics of LUS are listed in online supplementary e-table 2. The reference standard varied from CT, qualitative assessment of the final diagnosis based on clinical, laboratory and microbiological data, including CXR or chest CT results, and CXR combined with CT when LUS and CXR were discordant (table 1).
Overall, the methodological quality of the included studies, according to QUADAS-2, was good (online supplementary e-table 3). Some studies, however, had a high risk of bias regarding flow and timing due to heterogeneity in the reference standard between patients, and high risk of bias in patient selection due to the exclusion of patients with pulmonal or cardiac comorbidities. The study populations, severity of condition (intensive care unit vs non-intensive care unit), and the reference standard were heterogeneous across studies. As a result, the specific requirements for including results in a meta-analysis (eg, comparable populations, LUS performer and reference standard), were neither met by the included studies nor by a subgroup of included studies.
Diagnostic accuracy of LUS
Diagnostic accuracy is presented in table 1. The sensitivity of LUS to diagnose CAP ranged from 0.68 (95% CI, 0.52 to 0.81) to 1.00 (95% CI, 0.95 to 1.00); in 14 of the 17 studies, it was ≥0.91. The specificity could be calculated in 13 of the studies. It varied from 0.57 (95% CI, 0.34 to 0.78) to 1.00 (95% CI, 0.92 to 1.00), but in seven studies, it was ≥0.94. We found no systematic differences between studies with low and high diagnostic accuracy in terms of study setting, participant training or experience, or choice of reference standard. Inter-observer agreement was reported in two studies with κ-values of 0.83 and 0.90.32 36
The studies by Liu et al and Amatya et al were the two studies of highest methodological quality (online supplementary e-Table 3). Both studies compared LUS to CT (table 1) and LUS was performed by emergency physicians whose prior experience and training was described (table 2). However, they differed with regards to procedure and characteristics of LUS in terms of areas examined and definition of pneumonia on LUS (online supplementary e-Table 2). They found sensitivities of, respectively, 0.95 (95% CI, 0.89 to 0.98) and 0.91 (95% CI, 0.78 to 0.98) and specificities of 0.99 (95% CI, 0.92 to 1.00) and 0.61 (95% CI, 0.36 to 0.83).
Table 2.
Speciality of non-specialists, experience and training in LUS
| Study | Number of and speciality of physicians performing LUS | Prior experience in LUS or ultrasonography in general | Description of training in LUS | Time consumption on LUS |
| Amatya et al38 | Four emergency resident physicians | One week of performing LUS in the ED. | One hour lecture on LUS. Five pre-enrolment LUS scans and interpretation reviewed by expert sonographer. | 7 min 9 s (SD 1 min 57 s) |
| Corradi et al18 | One intensivist with PhD in US* | More than 10 years of experience in LUS* | – | – |
| Fares et al22 | A single physician | – | – | – |
| Karimi et al39 | Trained emergency residents under supervision of the attending emergency specialist in charge | – | – | – |
| Liu et al31 |
Three emergency physicians | At least 50 cases of LUS examination | Twenty-eight hours course based on US emergency medicine guidelines issued by the American College of Emergency Physicians in 2001 | – |
| Nazerian et al32 |
Four internal medicine and emergency medicine attending physicians. Four resident physicians (two internal medicine and two emergency medicine) | Attending physicians; at least 5 years of experience in POC-US Resident physicians; at least 1 year of training in emergency US | – | – |
| Taghizadieh et al35 | One emergency specialist | – | – | – |
| Parlamento et al34 | One emergency physician | Thirty years of experience in general and cardiac US and 10 years of training in LUS | – | <5 min |
| Reissig et al20 |
Experienced physicians (number and speciality not described) | At least 100 chest US procedures done prior to study | – | – |
| Unluer et al37 | Three attending emergency physicians | – | Three hours of didactic and 3 hours of hands-on thoracic US taught by an experienced radiology specialist to learn the diagnostic criteria of alveolar consolidation | <10 min |
| Benci et al17 | Physicians (number and speciality not described) | Considerable experience in US techniques | – | – |
| Bitar et al29 | Intensivist (number not described) | – | – | – |
| Bourcier et al30 | Five emergency physicians | – | Two days of theoretical formation alternating with practical ultrasounds sessions in groups of three people | – |
| Cipollini et al27 | Internal medicine specialist* | More than 1 year of bedside US experience* | – | – |
| Cortellaro et al 19 | One expert operator | – | – | <5 min |
| Pagano et al33 |
Five trained emergency physicians | More than 2 years of experience in LUS | – | – |
| Ticinesi et al36 | Three internal and emergency medicine physicians | More than 1 year of bedside US experience | Level one of training completed according to the guidelines by the EFSUMB | – |
*Data collected by correspondence with author.
-, not described; EFSUMB, European Federation of Societies for Ultrasound in Medicine and Biology; LUS, lung ultrasonography; POC-US, point-of-care ultrasonography; US, ultrasonography.
None of the studies compared sonographic findings to clinical outcomes. Three studies assessed the severity of pneumonia in patients with either CURB-6518 22 or Pneumonia Outcome Research Team score,34 but these were not compared with LUS findings.
Bourcier et al30 stratified their results according to onset of symptoms of pneumonia (<24 hours versus >24 hours). They found that LUS (sensitivity of 0.97) was significantly more effective than CXR (sensitivity of 0.30) in diagnosing pneumonia when time from clinical onset was <24 hours.
Speciality and training of non-imaging specialists
Information about speciality, experience and training of physicians performing LUS is presented in table 2. LUS was performed by emergency physicians, internal medicine physicians and by intensivists, while four studies did not declare the specific speciality of the non-imaging specialists.17 19 20 22 Nine studies reported that physicians had previous experience with LUS or ultrasonography in general.17 18 20 27 31–34 38 Prior experience of performing LUS varied from 1 week in the emergency department to more than 10 years of clinical experience.
Five studies described a LUS training programme for the participating physicians.30 31 36–38 Two studies provided a reference for an established educational programme,31 36 whereas the remaining studies described training specifically designed for their study.30 37 38 All training programmes included both theoretical and practical sessions. A large variation in the extent of the training programmes was noted, ranging from a few hours at a course facility37 to completion of a European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB)14 level one qualification.36 Four studies reported the time spent performing LUS, which was overall <10 min.
Potential harms to patients
Twelve studies reported false positive results from LUS, and 14 studies described false negative results (table 3). Corradi et al reported a high number of false negative results as they found 14 (22%) false negative hemithorax LUS examinations.18 However, five of these were reported in patients with bilateral pneumonia, in whom LUS examination only detected pneumonia in one hemithorax. Moreover, Corradi et al described that LUS-positive pneumonia were larger in diameter (81±55 mm) and close to the pleural line (1±3 mm).18 Likewise, more studies described false negative results that were mainly seen in patients with small consolidations where pneumonia did not reach the pleura.20 22 30 32
Table 3.
Potential harms to patients
| Study | True positive LUS results, N (%) | False positive LUS results, N (%) | False negative LUS results, N (%) | True negative LUS results, N (%) |
Nature of false positive LUS results |
| Amatya et al38 | 40 (64.5) | 7 (11.3) | 4 (6.5) | 11 (17.7) | Three bronchiectasis, two interstitial lung diseases, one tuberculosis and one normal lung |
| Corradi et al18 | 30* (46.8) | 1* (1.6) | 14* (22.0) | 19* (29.6) | – |
| Fares et al22 | 28 (73.7) | 2 (5.3) | 2 (5.3) | 6 (15.7) | – |
| Karimi et al39 | 263 (93.9) | 0 (0.0) | 17 (6.1) | 0 | – |
| Liu et al31 | 106 (59.2) | 1 (0.6) | 6 (3.4) | 66 (36.8) | – |
| Nazerian et al32 | 72 (25.3) | 9 (3.1) | 15 (5.3) | 189 (66.3) | Three cancers, three parenchymal impaired ventilation not due to infection and three pulmonary fibrosis |
| Taghizadieh et al35 | 29 (96.7) | 1 (3.3) | 0 | 0 | – |
| Parlamento et al34 | 31 (63.3) | 0 (0.0) | 1 (2.0) | 17 ((34.7) | – |
| Reissig et al20 | 211 (59.3) | 3 (0.8) | 15 (4.2) | 127 (35.7) | – |
| Unluer et al37 | 27 (37.5) | 7 (9.7) | 1 (1.4) | 37 (51.4) | Four pulmonary embolisms and three exacerbations of COPD |
| Benci et al17 | 37 (46.3) | 0 (0.0) | 0 (0.0) | 43 (53.7) | – |
| Bitar et al29 | – | – | – | – | – |
| Bourcier et al30 | 117 (81.2) | 9 (6.3) | 6 (4.2) | 12 (8.3) | Four sepsis of other origin, two pulmonary embolisms, one ARDS, one pulmonary fibrosis and one acute anaemia. |
| Cipollini et al27 | 105 (82.0) | – | 23 (18.0) | – | – |
| Cortellaro et al19 | 80 (66.7) | 2 (1.7) | 1 (0.8) | 37 (30.8) | One congestive heart failure and one subphrenic abscess with lung atelectasia |
| Pagano et al33 | 67 (63.8) | 13 (12.4) | 1 (1.0) | 24 (22.8) | Seven exacerbations of COPD, two congestive heart failure, three cancers and one pulmonary infarction |
| Ticinesi et al36 | 88 (52.1) | 3 (1.8) | 8 (4.7) | 70 (41.2) | Two pulmonary embolisms and one cancer |
* Hemithoraxes.
-, not described; ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; LUS, lung ultrasonography; N, number.
Parlamento et al reported two incidental findings of subpleural consolidations in patients without pneumonia.34 In both cases, LUS findings were verified by chest CT scan and confirmed to be, respectively, an atelectasis caused by a large pleural effusion and a case of pulmonary embolism.
Discussion
To our knowledge, this is the first systematic review to focus specifically on LUS to diagnose CAP in adults in the hands of non-imaging specialists physicians working clinically. These non-imaging specialists were emergency physicians, internal medicine physicians, intensivists or unclassified physicians and obtained LUS sensitivities and specificities that were typically above 0.90. We found no overall difference in diagnostic accuracy when compared with study setting or the physicians’ speciality, experience or training. Importantly, the variation in sensivitity and specificity was found across reference standards. No study compared sonographic findings to the severity of pneumonia. Only a few studies described LUS training of the non-imaging specialists, and these training programmes varied from short lectures to fully accredited ultrasound education.
We highlighted the results of Liu et al and Amatya et al due to the quality of the studies, but the studies were not completely comparable in other parameters. Both studies found high and comparable sensitivities of 0.95 (95% CI, 0.89 to 0.98) and 0.91 (95% CI, 0.78 to 0.98), respectively. However, in Amatya et al, LUS specificity was 0.61 (95% CI, 0.36 to 0.83) and significantly lower than the specificity in Liu et al of 0.99 (95% CI, 0.92 to 1.00). According to Amatya et al, this was due to a higher prevalence of pulmonal co-morbidities which resulted in false positive LUS results. Low specificity may lead to over-diagnosis of pneumonia and inappropriate use of antibiotics.
The diagnostic accuracy of LUS for diagnosing pneumonia described in this review is consistent with results from previous reviews that made no distinction between imaging specialists and physicians working clinically.8–13 Recently, Orso et al obtained a pooled sensitivity of 0.92 and a specificity of 0.93 in a review based on studies performed in emergency departments.40 Of course, the majority of LUS operators were emergency physicians, corresponding to the non-specialists in the present review. Consequently, Orso et al and this study have included many of the same studies. However, Orso et al also included studies with imaging specialists and patients with ‘acute respiratory failure’. Our review included LUS performed by non-imaging specialists from different specialties and in different settings. One study was even partly conducted in outpatient settings with non-hospitalised patients.20 Importantly, the results of this particular study did not differ from the remaining studies. Hence, LUS might also be applied on non-hospitalised patients with suspected CAP, which supports the vision that LUS could be a useful tool for any clinician in the future.41
Non-imaging specialists working in primary care are first in line to see patients with CAP and general practitioners have already begun using point-of-care ultrasound.42 43 The results by Bourcier et al suggest that LUS is a better diagnostic tool for achieving an early diagnosis (≤24 hours from clinical onset) compared with CXR. The ability of LUS to accurately diagnose pneumonia early in the course of the disease may improve outcomes for patients attending primary care.43 Furthermore, improved diagnostic performance in patients with suspected CAP may reduce the need for antibiotics. On the other hand, the size of pulmonary lesions might be smaller in the early stages of disease and the results indicate that the usability of LUS to diagnose CAP is compromised by its inability to visualise pulmonary lesions that are not in contact with the pleura. However, according to Lichtenstein et al who looked for lung consolidation in intensive care patients, this occurred in only 1.5% cases of lung consolidation44. Due to a lower prevalence and less severe disease in a general practice population, further evaluation of LUS for the diagnosis of CAP in general practice is required.
LUS is a user-dependent examination and several guidelines14 45 46 stress that diagnostic performance requires sufficient training to gain the necessary competencies. A meta-analysis by Tsou et al found a significant difference in diagnostic accuracy between LUS performed by ‘advanced’ versus ‘novice’ sonographers in the diagnosis of pneumonia in children.47 However, they defined ‘novice sonographers’ as physicians with little or no prior LUS experience or training (≤7 days); most of the non-imaging specialists in the present review would be classified as ‘advanced sonographers’ according to this definition. Though, the learning curve appears steep from paediatric data and in a randomised controlled trial by Jones et al,48 they found that substitution of CXR with LUS when evaluating children suspected of having pneumonia was feasible and safe, also in the hands of novice sonographers (≤25 examinations). Today, there are no guidelines or recommendations specifying the amount of training or level of competence needed to perform LUS.49 50 As this review has shown, however, these competencies can be reached by the non-imaging specialist physician even after a short, tailored training programme. To ensure that physicians maintain and develop skills over time and learn to incorporate LUS findings into clinical decision-making, longitudinal training elements must be incorporated into the training programmes.50
This study describes the different specialties of the non-imaging specialists and demonstrates great heterogeneity in their prior experience and training in LUS. However, sensitivities and specificities are comparable, thereby implying that LUS can be performed by physicians in various specialties, and by less experienced physicians, with comparable results to those of physicians with considerable experience in LUS.
Limitations
The aim of this study was to describe the diagnostic accuracy of LUS for diagnosing CAP when performed by physicians with considerably less ultrasound experience than imaging specialists. In four of the included studies, the speciality of the physician was not reported.17 19 20 22 These studies were included as we assessed from the clinical setting that the physicians were not radiologists or sonographers. The results from these four studies did not differ from the remaining studies. Furthermore, while some of the physicians had extensive experience with LUS,17 18 34 and their ultrasonography competencies may be compared with those of an imaging specialist, we did not find, in general, that sensitivity and specificity increased with experience. Comparison of studies was difficult due to sparse information on the non-imaging specialists’ training, their experience with LUS and the heterogeneity in the reference standards used. Due to the significant heterogeneity across studies, it was not appropriate to pool data and perform a meta-analyses.
Conclusion
We found significant heterogeneity across studies. In the majority of studies, LUS in the hands of the non-imaging specialists demonstrated high sensitivities and specificities in diagnosing pneumonia. However, due to problems with methodology and heterogeneity, there is a need for larger studies with uniform and clearly established criteria for diagnosis and blinding.
Supplementary Material
Footnotes
Contributors: JJS is the guarantor of the study. JJS, PSH, MPH, MBBJ, OG and CAA contributed to the concept, design and drafting of the study. JJS, PSH and MPH conducted the systematic search strategy and the review. All authors revised critically and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1.Polverino E, Torres Marti A. Community-acquired pneumonia. Minerva Anestesiol 2011;77:196–211. [PubMed] [Google Scholar]
- 2.Meehan TP, Fine MJ, Krumholz HM, et al. Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA 1997;278:2080–4. 10.1001/jama.1997.03550230056037 [DOI] [PubMed] [Google Scholar]
- 3.Bjerrum L. Luftvejsinfektioner - diagnose og behandling, 2014: 30–5. [Google Scholar]
- 4.Prina E, Ranzani OT, Torres A. Community-acquired pneumonia. Lancet 2015;386:1097–108. 10.1016/S0140-6736(15)60733-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Syrjälä H, Broas M, Suramo I, et al. High-resolution computed tomography for the diagnosis of community-acquired pneumonia. Clin Infect Dis 1998;27:358–63. 10.1086/514675 [DOI] [PubMed] [Google Scholar]
- 6.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84. 10.1056/NEJMra072149 [DOI] [PubMed] [Google Scholar]
- 7.Sartori S, Tombesi P. Emerging roles for transthoracic ultrasonography in pulmonary diseases. World J Radiol 2010;2:203–14. 10.4329/wjr.v2.i6.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Accuracy of lung ultrasonography in the diagnosis of pneumonia in adults: systematic review and meta-analysis. Chest 2017;151:374–82. 10.1016/j.chest.2016.10.039 [DOI] [PubMed] [Google Scholar]
- 9.Long L, Zhao H-T, Zhang Z-Y, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a meta-analysis. Medicine 2017;96:e5713. 10.1097/MD.0000000000005713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia Y, Ying Y, Wang S, et al. Effectiveness of lung ultrasonography for diagnosis of pneumonia in adults: a systematic review and meta-analysis. J Thorac Dis 2016;8:2822–31. 10.21037/jtd.2016.09.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chavez MA, Shams N, Ellington LE, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res 2014;15:50. 10.1186/1465-9921-15-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye X, Xiao H, Chen B, et al. Accuracy of lung ultrasonography versus chest radiography for the diagnosis of adult community-acquired pneumonia: review of the literature and meta-analysis. PLoS One 2015;10:e0130066. 10.1371/journal.pone.0130066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alzahrani SA, Al-Salamah MA, Al-Madani WH, et al. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J 2017;9:6. 10.1186/s13089-017-0059-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minimum training requirements for the practice of medical ultrasound in Europe. Ultraschall Med 2010;31:426–7. 10.1055/s-0030-1263214 [DOI] [PubMed] [Google Scholar]
- 15.Deeks JJ BP, Gatsonis C. Cochrane Handbook for systematic reviews of diagnostic test accuracy version 1.0.0. The Cochrane collaboration, 2009. http://srdta.cochrane.org/ [Google Scholar]
- 16.Whiting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 17.Benci A, Caremani M, Menchetti D. Sonographic diagnosis of pneumonia and bronchopneumonia. Ultraschall Med 1996;4:169–76. 10.1016/S0929-8266(96)00195-4 [DOI] [Google Scholar]
- 18.Corradi F, Brusasco C, Garlaschi A, et al. Quantitative analysis of lung ultrasonography for the detection of community-acquired pneumonia: a pilot study. Biomed Res Int 2015;2015:1–8. 10.1155/2015/868707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cortellaro F, Colombo S, Coen D, et al. Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department. Emerg Med J 2012;29:19–23. 10.1136/emj.2010.101584 [DOI] [PubMed] [Google Scholar]
- 20.Reissig A, Copetti R, Mathis G, et al. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest 2012;142:965–72. 10.1378/chest.12-0364 [DOI] [PubMed] [Google Scholar]
- 21.Nafae R, Eman SR, Mohamad NA, et al. Adjuvant role of lung ultrasound in the diagnosis of pneumonia in intensive care unit-patients. Egypt J Chest Dis Tuberc 2013;62:281–5. 10.1016/j.ejcdt.2013.04.007 [DOI] [Google Scholar]
- 22.Fares Auf M-N. Role of transthoracic ultrasound in detection of pneumonia in ICU patients. Med J Cairo Univ 2015;83:307–14. [Google Scholar]
- 23.Targhetta R, Chavagneux R, Bourgeois JM, et al. Sonographic approach to diagnosing pulmonary consolidation. J Ultrasound Med 1992;11:667–72. 10.7863/jum.1992.11.12.667 [DOI] [PubMed] [Google Scholar]
- 24.Elkholy MM, Mohammad HA, Osman NM, et al. Accuracy of gray scale and color doppler sonographic mapping in diagnosis of pneumonia in adult. Egypt J Chest Dis Tuberc 2016;65:491–8. 10.1016/j.ejcdt.2015.12.014 [DOI] [Google Scholar]
- 25.Sperandeo M, Carnevale V, Muscarella S, et al. Clinical application of transthoracic ultrasonography in inpatients with pneumonia. Eur J Clin Invest 2011;41:1–7. 10.1111/j.1365-2362.2010.02367.x [DOI] [PubMed] [Google Scholar]
- 26.Alawaji OM, Yones DK, Almalki MA, et al. Value of lung ultrasonography for the diagnosis of acute pneumonia in emergency department, multicenter study in Medina, Saudi Arabia. Indo Am J Pharm Sci 2019;6:1441–50. [Google Scholar]
- 27.Cipollini F, Mirauta CM. Bedside lung ultrasound in the diagnosis of pneumonia in very old patients. Ital J Med 2018;12:126–30. 10.4081/itjm.2018.981 [DOI] [Google Scholar]
- 28.D'Amato M, Rea G, Carnevale V, et al. Assessment of thoracic ultrasound in complementary diagnosis and in follow up of community-acquired pneumonia (CAP). BMC Med Imaging 2017;17:52. 10.1186/s12880-017-0225-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bitar ZI, Maadarani OS, El-Shably AM, et al. Diagnostic accuracy of chest ultrasound in patients with pneumonia in the intensive care unit: a single-hospital study. Health Sci Rep 2019;2:e102. 10.1002/hsr2.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bourcier J-E, Paquet J, Seinger M, et al. Performance comparison of lung ultrasound and chest x-ray for the diagnosis of pneumonia in the ED. Am J Emerg Med 2014;32:115–8. 10.1016/j.ajem.2013.10.003 [DOI] [PubMed] [Google Scholar]
- 31.Liu X-lei, Lian R, Tao Y-kang, Tao YK, et al. Lung ultrasonography: an effective way to diagnose community-acquired pneumonia. Emerg Med J 2015;32:433–8. 10.1136/emermed-2013-203039 [DOI] [PubMed] [Google Scholar]
- 32.Nazerian P, Volpicelli G, Vanni S, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med 2015;33:620–5. 10.1016/j.ajem.2015.01.035 [DOI] [PubMed] [Google Scholar]
- 33.Pagano A, Numis FG, Visone G, et al. Lung ultrasound for diagnosis of pneumonia in emergency department. Intern Emerg Med 2015;10:851–4. 10.1007/s11739-015-1297-2 [DOI] [PubMed] [Google Scholar]
- 34.Parlamento S, Copetti R, Di Bartolomeo S. Evaluation of lung ultrasound for the diagnosis of pneumonia in the ED. Am J Emerg Med 2009;27:379–84. 10.1016/j.ajem.2008.03.009 [DOI] [PubMed] [Google Scholar]
- 35.Taghizadieh A, Ala A, Rahmani F, et al. Diagnostic accuracy of chest X-ray and ultrasonography in detection of community acquired pneumonia; a brief report. Emerg 2015;3:114–6. [PMC free article] [PubMed] [Google Scholar]
- 36.Ticinesi A, Lauretani F, Nouvenne A, et al. Lung ultrasound and chest X-ray for detecting pneumonia in an acute geriatric ward. Medicine 2016;95:e4153. 10.1097/MD.0000000000004153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Unluer EE, Karagoz A, Senturk GO, et al. Bedside lung ultrasonography for diagnosis of pneumonia. Hong Kong J Emerg Med 2013;20:98–104. 10.1177/102490791302000205 [DOI] [Google Scholar]
- 38.Amatya Y, Rupp J, Russell FM, et al. Diagnostic use of lung ultrasound compared to chest radiograph for suspected pneumonia in a resource-limited setting. Int J Emerg Med 2018;11:8. 10.1186/s12245-018-0170-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karimi E. Comparing sensitivity of ultrasonography and plain chest radiography in detection of pneumonia; a diagnostic value study. Arch Acad Emerg Med 2019;7:e8. [PMC free article] [PubMed] [Google Scholar]
- 40.Orso D, Guglielmo N, Copetti R. Lung ultrasound in diagnosing pneumonia in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med 2018;25:312–21. 10.1097/MEJ.0000000000000517 [DOI] [PubMed] [Google Scholar]
- 41.Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012;38:577–91. 10.1007/s00134-012-2513-4 [DOI] [PubMed] [Google Scholar]
- 42.Andersen CA, Holden S, Vela J, et al. Point-of-care ultrasound in general practice: a systematic review. Ann Fam Med 2019;17:61–9. 10.1370/afm.2330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sorensen B, Hunskaar S. Point-of-care ultrasound in primary care: a systematic review of generalist performed point-of-care ultrasound in unselected populations. Ultrasound J 2019;11:31. 10.1186/s13089-019-0145-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lichtenstein DA, Lascols N, Mezière G, et al. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 2004;30:276–81. 10.1007/s00134-003-2075-6 [DOI] [PubMed] [Google Scholar]
- 45.Ultrasound TSoPoC Guidelines for point of care ultrasound utilization in clinical practice, 2017. Available: https://spocus.org/Practice-Guidelines
- 46.Medicine IFfE Point of care ultrasound curriculum guidelines, 2014. Available: https://www.ifem.cc/wp-content/uploads/2016/03/IFEM-Point-of-Care-Ultrasound-Curriculum-Guidelines-2014.pdf
- 47.Tsou P-Y, Chen KP, Wang Y-H, et al. Diagnostic accuracy of lung ultrasound performed by novice versus advanced sonographers for pneumonia in children: a systematic review and meta-analysis. Acad Emerg Med 2019;26:1074–88. 10.1111/acem.13818 [DOI] [PubMed] [Google Scholar]
- 48.Jones BP, Tay ET, Elikashvili I, et al. Feasibility and safety of substituting lung ultrasonography for chest radiography when diagnosing pneumonia in children: a randomized controlled trial. Chest 2016;150:131–8. 10.1016/j.chest.2016.02.643 [DOI] [PubMed] [Google Scholar]
- 49.Pietersen PI, Madsen KR, Graumann O, et al. Lung ultrasound training: a systematic review of published literature in clinical lung ultrasound training. Crit Ultrasound J 2018;10:23. 10.1186/s13089-018-0103-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Olgers TJ, Azizi N, Blans MJ, et al. Point-of-care ultrasound (PoCUS) for the internist in acute medicine: a uniform curriculum. Neth J Med 2019;77:168–76. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-036067supp001.pdf (2MB, pdf)


