Abstract
Purpose
As our hospitals conserve and re-allocate resources during the COVID-19 crisis, there is urgent need to determine how best to continue caring for breast cancer patients. During the time window before the COVID-19 critical peak and particularly thereafter, as hospitals are able to resume cancer operations, we anticipate that there will be great need to maximize efficiency to treat breast cancer. The goal of this study is to present a same-day protocol that minimizes resource utilization to enable hospitals to increase inpatient capacity, while providing care for breast cancer patients undergoing mastectomy and immediate breast reconstruction during the COVID-19 crisis.
Methods
IRB exempt patient quality improvement initiative was conducted to detail the operationalization of a novel same-day breast reconstruction protocol. Consecutive patients having undergone immediate breast reconstruction were prospectively enrolled between February and March of 2020 at Massachusetts General Hospital during the COVID-19 crisis. Peri-operative results and postoperative complications were summarized.
Results
Time interval from surgical closure to patient discharge was 5.02 ± 1.29 h. All patients were discharged home, with no re-admissions or emergency department visits. No postoperative complications were observed.
Conclusion
This report provides an instruction manual to operationalize a same-day breast reconstruction protocol, to meet demands of providing appropriate cancer treatment during times of unprecedented resource limitations. Pre-pectoral implant-based breast reconstruction can be the definitive procedure or be used as a bridge to autologous reconstruction. Importantly, we hope this work will be helpful to our patients and community as we emerge from the COVID-19 pandemic.
Electronic supplementary material
The online version of this article (10.1007/s10549-020-05739-7) contains supplementary material, which is available to authorized users.
Keywords: COVID-19, Breast reconstruction, Protocol, Same-day, Coronavirus
Introduction
As healthcare networks across USA brace for an influx of patients infected with COVID-19, it remains imperative that we consider how to prioritize surgical care delivery. Every hospital must, therefore, develop case-selection protocols based on clinical acuity and available resources in the context of an effective COVID-19 response strategy [1]. There is perhaps not a more relevant time for the deliberate allocation of medical resources through prioritization of high acuity and life-threatening cases than during the current COVID-19 pandemic [2, 3]. The need to redistribute resources, healthcare personnel, and inpatient beds is common across all medical disciplines during times of disproportionate medical demand [2, 4–6]. In surgical oncology and plastic surgery, where patients with extensive tumor burden or higher cancer stage may need to be prioritized for mastectomy, the decision of whether or not to perform breast reconstruction is an important consideration. In fact, two weeks into March, as the USA began to broadly implement a COVID-19 emergency response plan, the American Society of Plastic Surgeons (ASPS) issued a position statement, acknowledging the significant resource utilization commanded by immediate breast reconstruction and the need for streamlining of operative technique to alleviate financial burden in such an unprecedented time [7].
An effort to minimize resource utilization and improve surgical efficiency not only requires optimization of existing protocols, but also innovation of medical practice through implementation of telemedicine services and transition to same-day surgery, where patients are discharged on the day of surgery.[8] Previous studies have demonstrated the safety and efficacy of same-day mastectomy and breast reconstruction, largely relying on extensive perioperative planning and postoperative recovery protocols to simplify surgical course and minimize patient morbidity [9–11]. Prior implementation of an enhanced recovery protocol at our institution has decreased the need for opioid analgesia and length of hospital stay following mastectomy and implant-based breast reconstruction, thereby limiting the need for inpatient admission during the immediate postoperative period [12]. Similarly, Vuong et al. reported successful implementation of a pilot postmastectomy home recovery program, demonstrating low rates of emergency department visits or re-admission for discharged patients [13]. In a recent study conducted by Keehn et al., the authors reported the release of nearly 831 hospital beds across 13 hospitals in Alberta, Canada, per year due to their same-day surgery pathway, with no difference in postoperative complication or hospital re-admission when compared to those admitted overnight per traditional mastectomy protocol [14].
In order to limit resource utilization during this crisis, we have operationalized a same-day mastectomy and breast reconstruction protocol. Clearly, when a hospital is overwhelmed with COVID-19 demands, only life-threatening procedures will be carried out. During times of case surge, each team and hospital should observe local health board and national society guidance with regard to elective procedures such as breast reconstruction. Breast reconstruction requires additional resources (personnel and PPE, extends the operating room time, increase risk of additional visits or operations in cases of complications). As we are observing in March 2020, hospitals across the country, even within the same state, can have very disparate experiences with regard to the acuity of COVID-19 surge. Therefore, preceding the surge or subsequently thereafter, as resource bandwidth permits performance of oncologic procedures, we propose that the use of a reduced resource mastectomy and breast reconstruction protocol may help to meet the demand for mastectomy and breast reconstruction procedures. Preceding the COVID-19 crisis, we had assembled a multidisciplinary team at our institution to adapt a same-day surgery protocol, in an attempt to decrease healthcare expenditure, increase inpatient capacity, while maintaining a high level of care to patients undergoing mastectomy and immediate implant-based breast reconstruction. This quality improvement project engaged the following stakeholders: surgical oncologist, plastic surgeons, anesthesiologists, operating room administrators, recovery room nursing staff, pre-operative care team, case managers, and patients. We refined this pathway to better address the challenges posed to hospital networks by the COVID-19 crisis, chief among them the minimization of viral exposure at the patient level and the reduction of resource utilization at the hospital level, by incorporating virtual patient portal and telehealth services for pre-operative and postoperative consultation and patient evaluation. Here, we describe our experience with this same-day mastectomy and immediate breast reconstruction to patients with breast cancer in the setting of the COVID-19 pandemic. We are motivated to share this simple playbook with the hope that this approach can be helpful to our community, so that we can continue to provide care to patients afflicted with breast cancer during this crisis.
Methods
Study design and population
The work presented here is a patient quality improvement initiative; therefore, review by an IRB was not necessary. Consecutive patients having undergone mastectomy with immediate breast reconstruction via novel same-day surgery protocol were prospectively enrolled in the study between February and March of 2020 at Massachusetts General Hospital. Patients who underwent unilateral or bilateral mastectomy with subsequent tissue expander or direct-to-implant breast reconstruction were included. Importantly, only those patients who lived within 2-h of the hospital and had appropriate at-home support, as determined through shared decision making with the patient, were eligible for the same-day discharge protocol. The remaining inclusion criteria are depicted in Fig. 1. Patient demographics, oncologic and clinical data, and operative metrics were extracted from the medical record.
Fig. 1.
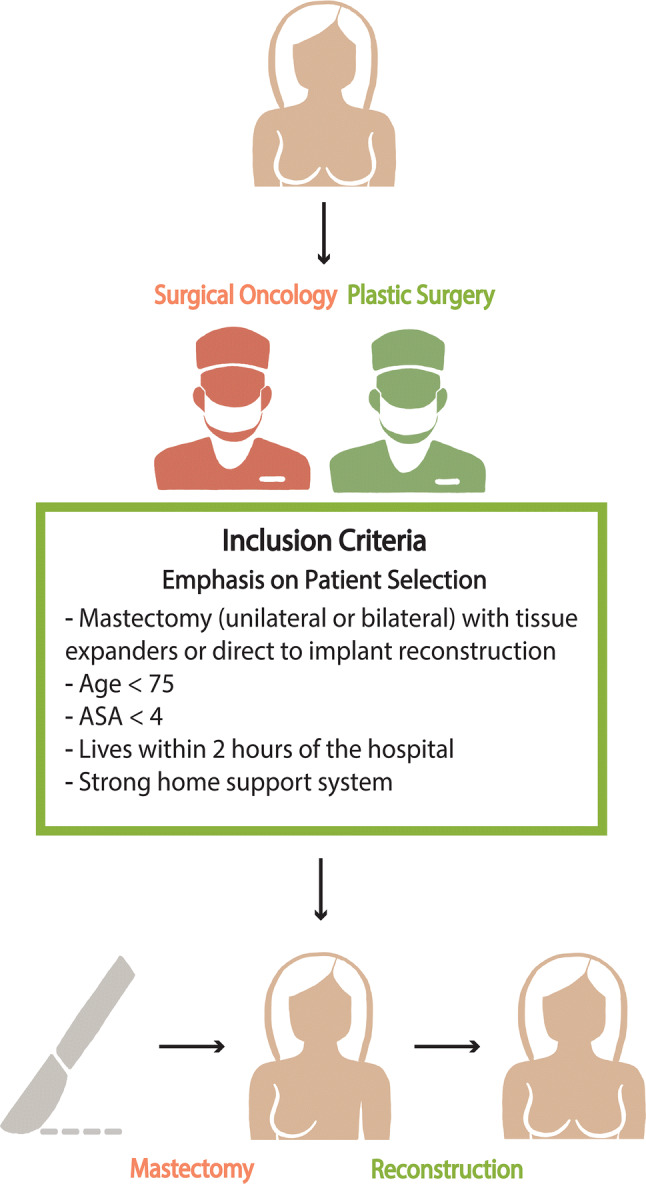
Inclusion criteria for patients selected for same-day mastectomy and immediate breast reconstruction
Prioritization of treatment by cancer stage
During March 2020, our breast surgical oncology section was mandated to create guidelines for prioritization of breast cancer operations that should not be delayed, and those that could safely be postponed. All operations in our institutions after this date would require approval from our section chief and ultimately the chair of the department of surgery prior to being performed. These guidelines required a collaborative effort with our multidisciplinary team – surgical oncology, plastic surgery, radiation oncology, medical oncology, breast imaging, and breast pathology. See Supplemental Fig. 1 for the COVID guidelines that were used to approve the mastectomies that were performed during March 2020. There are 3 patients in our cohort whose operation was performed prior to implementation of our institution COVID-19-related prioritization of breast surgery operations. This study reports the results of a quality improvement project, and unlike a study protocol, there were no strict exclusion criteria. All consecutive patients during this window of time were offered the same-day option and the results are reported. In our practice, patients with a known pre-operative positive node and a known indication for PMRT are counseled regarding increased risk of postoperative complications. As we continue to evolve surgical techniques, we found that muscle-sparing pre-pectoral implant placement can mitigate capsular contracture and decrease revision rates compared to subpectoral technique [15]. Patients who were not offered immediate reconstruction included those who were active smokers.
Same-day surgery pathway
A perioperative pathway was developed in collaboration with a multidisciplinary team at Massachusetts General Hospital for same-day immediate implant-based breast reconstruction (Fig. 2). A concomitant enhanced recovery after surgery (ERAS) protocol was also conceived in conjunction with our anesthesia colleagues. The perioperative pathway focuses on three main areas of patient contact: pre-operative, day of surgery, and postdischarge. This pathway was adjusted in light of the COVID-19 outbreak in order to minimize patient visits to the hospital.
Fig. 2.
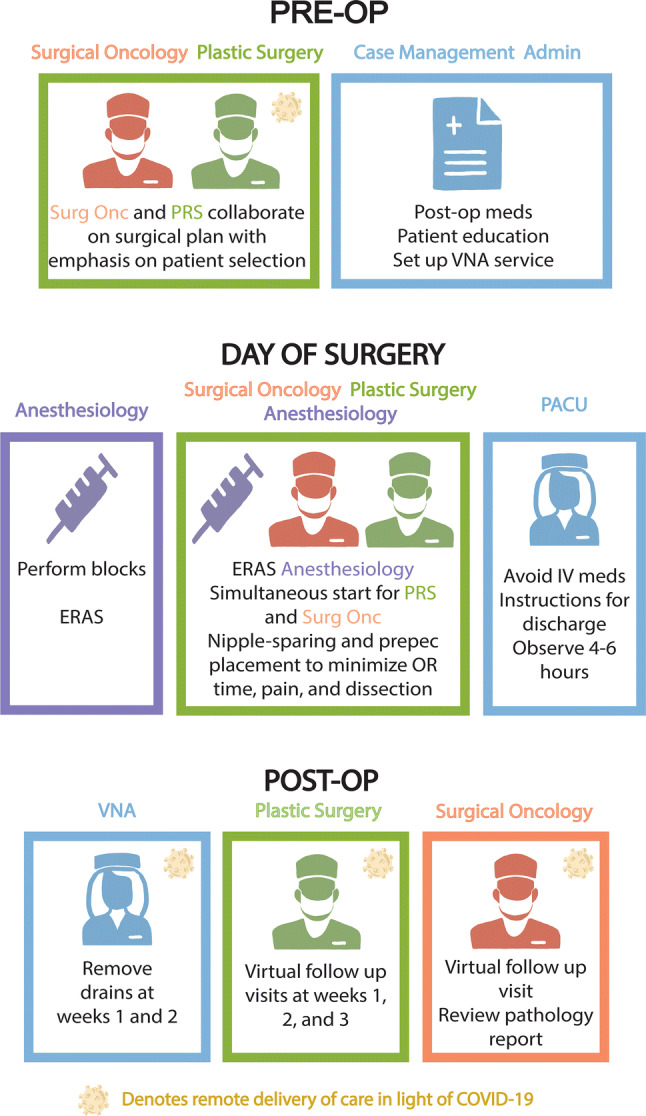
Same-day mastectomy and immediate breast reconstruction protocol, modified in the setting of COVID-19 to convert in-person pre-operative and postoperative evaluations to online visits. Importantly, drain management and removal are facilitated by visiting nursing services in an attempt to minimize nosocomial viral exposure and decrease resource utilization
Pre-operative
Patients were initially seen in the surgical oncology clinic after diagnosis of breast cancer was confirmed. Once it was determined that the patient would need a mastectomy for treatment of their breast cancer (unilateral or bilateral) they were educated by the surgical oncology team with regards to our perioperative pathway. This visit included information regarding the role of a paravertebral block to reduce postoperative nausea and vomiting, shorten time to oral pain medications, and decreased length of stay. Data regarding the efficacy of our ERAS protocol was reviewed and day surgery was offered to all patients who met inclusion criteria. Patients were then referred to plastic surgery for consultation regarding reconstruction. Given the current climate within the context of COVID-19 crisis, many patients underwent surgical oncology and plastic surgery consultation via video conferencing with patient pictures viewed by the plastic surgeon via a HIPAA approved secured system. Patients were provided educational materials newly created by the multidisciplinary team to limit the need for in-person postoperative visits, including access to online videos to review wound and drain care. Prescriptions for all medications needed postoperatively were sent electronically by the plastic surgery clinic to patient’s pharmacy. A referral to the hospitals case manager was initiated at this pre-operative visit to ensure that a visiting nurse was scheduled for a home visit on postoperative day (POD) #1. Pre-operative medications (Gabapentin, Tylenol, and Celebrex) were ordered by the surgical oncology clinic to be given the day of surgery upon arrival to the pre-operative area. All members of the surgical team, anesthesia, peri-op nursing, and case managers were alerted to the upcoming cases and prepared to maximize likelihood of same-day discharge.
Day of surgery
Upon arrival to the pre-operative area, routine evaluation was performed by the nursing staff and a patient checklist was made to ensure completion of perioperative tasks (Fig. 3). Pre-operative medications were then administered. Paravertebral blocks are performed by the anesthesia pain team as part of the ERAS protocol. Once in the operating room, the planned surgical procedures were performed by the surgical oncologist and plastic surgery teams. The tissue plane of implant placement was largely determined by the thickness of the mastectomy skin flap. In cases of robust mastectomy skin flaps with sufficient subcutaneous tissue thickness, the breast implant was placed in the pre-pectoral space and the reconstruction was usually carried out in a single-stage. If the mastectomy skin flap was thin or viability judged to be suboptimal clinically, a tissue expander was placed in the subpectoral plane. Tumor size or oncologic characteristics did not influence the decision to perform pre-pectoral versus subpectoral reconstruction, the determinant of implant placement location and single versus staged approach is determined by mastectomy skin flap viability, which is supported by the literature [16, 17]. Anesthetic was administered using a strict total intravenous anesthesia (TIVA) protocol along with administration of at least two anti-emetics in order to maximize patient comfort and avoid postoperative nausea and vomiting.
Fig. 3.
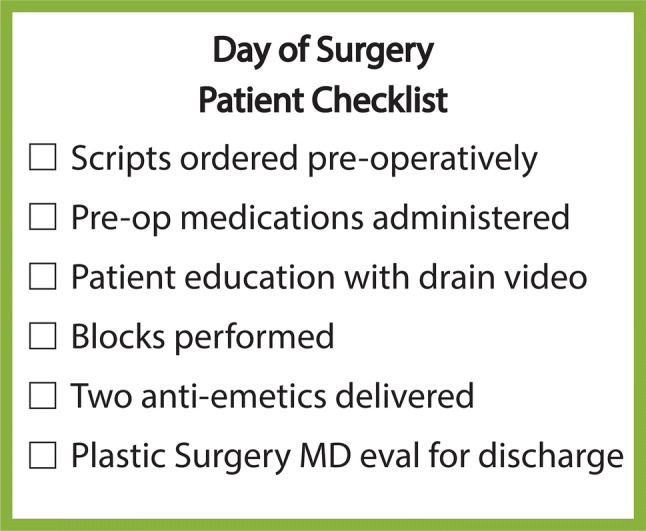
Peri-operative checklist for the same-day mastectomy and immediate breast reconstruction protocol
After transfer to the recovery room, patients were eating, ambulating, and receiving oral medications for pain control. They were monitored for four hours and ultimately assessed by a representative from the surgical team to evaluate for signs of hematoma and readiness to be discharged. At this point, a discharge order was written and nursing reviews discharge information and drain care. Visiting nursing association (VNA) services are arranged prior to the day of surgery, with patients having already received their prescriptions, thereby simplifying discharge.
Post discharge
All patients were contacted through virtual patient portal by the plastic surgery clinic one day after discharge to ensure that the patient was doing well and to answer any questions. Our standard before the crisis was to have a first postoperative appointment for three consecutive weeks, with one drain removed at week 1, last drain removed at week 2, and patient checked for seroma, and final healing at week 3. During the crisis, in an effort to minimize patient travel and limit nosocomial viral exposure, these visits were converted to virtual with visiting nurses performing drain removal at the patient’s home or local hospital.
Data collection and statistical analysis
Variables recorded for each patient were age at surgery, laterality of cancer, type of mastectomy, neoadjuvant chemotherapy, mastectomy type (nipple-sparing v. skin-sparing), axillary management (axillary lymph node dissections and sentinel node biopsies), and reconstruction type (direct-to-implant or tissue expander reconstruction). Primary endpoints of interest include operating time, disposition (admission vs. discharge), time interval between surgical closure and discharge, re-admission rate, and emergency department presentation. The following postoperative complications were identified: hematoma requiring a return trip to the operating room, infection requiring a return trip to the operating room.
Data was analyzed using SPSS 25 (IBM Corp., Armonk, NY). Summary statistics were calculated for patient demographics, clinical and surgical characteristics, and primary and secondary endpoints. Patient demographics (age and BMI) were compared to those reported in prior publications from our institution using a two-sided unpaired t-test test for continuous variables.
Results
Patient demographic and clinical characteristics
We enrolled a total of 15 patients. The mean age of the women at the time of surgery was 45.38 ± 6.86 years. Eleven patients underwent unilateral mastectomy while four patients underwent bilateral mastectomy. Eleven patients underwent mastectomy with sentinel lymph node biopsy compared with three patients who underwent mastectomy with axillary lymph node dissection. Nipple-sparing mastectomy was performed in 11 (73.33%) patients, while skin-sparing mastectomy was performed in 4 (26.67%). Direct-to-implant immediate breast reconstruction was performed in 11 breasts and tissue-expander-based reconstruction in 8 breasts. In addition, implant placement in the pre-pectoral plane (n = 11, 57.90%) outpaced submuscular reconstruction (n = 8, 42.10%). Importantly, the decision for adjuvant chemotherapy and postmastectomy radiation is dependent on evaluation of tumor oncotype, the results of which often return weeks after mastectomy. As such, data regarding oncologic management is largely incomplete. Importantly, four breasts demonstrated simultaneous DCIS and IDC pathologies. The remaining oncologic characteristics are detailed in Table 1. Further, reconstruction at the time of mastectomy is not dependent on whether the patient will need adjuvant chemotherapy or adjuvant radiation therapy. The rate of prior irradiation in our patient population was 6.67% (n = 1), with four patients having undergone neoadjuvant chemotherapy (26.67%). Patient demographics are presented in Table 1. Of note, when comparing patient demographics to patient cohorts in previous publications from our institution, we could not identify a statistically significant difference in age (p = 0.60) and BMI (p = 0.94).
Table 1.
Clinical characteristics
| Patient characteristics | n (%) |
|---|---|
| Patient demographics | 15 |
| Average age ± SD, years | 45.20 ± 7.06 |
| BMI ± SD, kg/m2 | 24.80 ± 4.58 |
| Smoking | 0 (0.00) |
| Diabetes | 0 (0.00) |
| Obese | 2 (13.33) |
| Neoadjuvant chemotherapy | 3 (20.00) |
| Prior radiation | 1 (6.67) |
| Oncologic characteristicsa | |
| BRCA carrier | 1 (6.67) |
| PALB2 carrier | 0 (0.00) |
| PTEN carrier | 0 (0.00) |
| Negative genetic testing | 8 (53.33) |
| IDCb | 8 (42.11) |
| Grade 1 | 2 (25.00) |
| Grade 2 | 2 (25.00) |
| Grade 3 | 4 (50.00) |
| DCISb | 15 (78.95) |
| Grade 1 | 0 (0.00) |
| Grade 2 | 5 (33.33) |
| Grade 3 | 10 (66.67) |
| T-size | |
| T1 | 9 (60.00) |
| T2 | 3 (20.00) |
| T3 | 2 (13.33) |
| Unknown | 1 (6.67) |
| Nodal status | |
| N0 | 9 (60.00) |
| N1 | 1 (6.67) |
| N2 | 2 (13.33) |
| N3 | 1 (6.67) |
| Unknown | 2 (13.33) |
| Sentinel node biopsy | 11 (73.33) |
| Axillary lymph node dissection | 3 (20.00) |
| Procedure laterality | |
| Unilateral | 11 (73.33) |
| Bilateral | 4 (26.67) |
| Implant placementb | |
| Pre-pectoral | 11 (57.90) |
| Subpectoral | 8 (42.10) |
| Mastectomy type | |
| Skin-Sparing | 4 (26.67) |
| Nipple-Sparing | 11 (73.33) |
| Reconstruction stageb | |
| Single-stage (DTI) | 11 (57.90) |
| Two-stage (TE) | 8 (42.10) |
SD standard deviation, BMI body mass index, IDC invasive ductal carcinoma, DCIS ductal carcinoma in-situ, DTI direct-to-implant, TE tissue expander
aGiven variability in time interval of pathologic evaluation, oncotype for 4 cases were recorded per core needle biopsy. Additionally, genetic testing results were for 4 patients were unknown given short follow-up duration
bDenotes data presented by breast (n = 19)
Evaluation of efficacy endpoints
The mean operative time for mastectomy with immediate breast reconstruction was 151.27 ± 33.14 min (2.52 ± 0.55 h). In contrast, the average time of mastectomy without reconstruction was 80.54 ± 24.34 min (1.34 ± 0.41 h) (n = 13). The time interval from surgical closure to discharge for patients that underwent mastectomy and reconstruction was 301.27 ± 77.13 min (5.02 ± 1.29 h) and time to discharge without reconstruction was 249.29 ± 113.58 min (4.15 ± 1.89 h), where 6 patients were excluded from this comparison as they were admitted due to associated comorbid conditions. Patients without reconstruction were older, more likely to have undergo chemotherapy and have comorbid medical conditions. Therefore, reconstruction added 1 h and 20 min to the total case time and less than 1 h to the time interval from surgical closure to discharge. In bilateral cases, the plastic surgeon begins reconstruction after one breast is removed to work concurrently with the surgical oncologist in order to minimize operative time. All patients enrolled in the same-day immediate breast reconstruction protocol were discharged home, with no re-admission or emergency department visits (Table 2). During virtual visits, patients were questioned about any local emergency room visits for postoperative complications and these responses were corroborated by independent review of external medical records.
Table 2.
Efficacy outcomes for same-day immediate breast reconstruction
| Efficacy endpoints | n (%) |
|---|---|
| Mean operative time ± SD, minutes | 151.27 ± 33.14 |
| Mean time interval to discharge ± SD, minutes | 301.27 ± 77.13 |
| Re-admissions | 0 (0.00) |
| Emergency department visits | 0 (0.00) |
SD standard deviation
Evaluation of safety endpoints
No postoperative complications were observed for patients undergoing same-day immediate breast reconstruction with 30-day postoperative follow-up. Importantly, incidence of hematoma was not observed in the 24-h postoperative period, during which time a patient would otherwise have been admitted and monitored for development of early complication. All of our patients were seen by a visiting nurse on either POD #1 or POD #2. Drains were removed without difficulty either by VNA or qualified healthcare provider locally without requiring the patient to return to our hospital. We reduced the number of postoperative visits from 2 visits per patient, which was standard protocol prior to same-day surgery implementation, to 0 visits per patient postimplementation.
Discussion
Given the rapid spread of COVID-19 and the need for deliberate resource prioritization, the implementation of a resource-limited operative protocol for immediate implant-based breast reconstruction is of critical importance. Same-day mastectomy and immediate breast reconstruction have been proposed as safe, economic methods of conferring oncologic and reconstructive treatment, while reducing resources and inpatient volume on hospital systems [18, 19]. These protocols have yet to be widely implemented, and few studies have been conducted to demonstrate reliability of technique. The present study serves as a pilot, demonstrating the safety and efficacy of a novel same-day surgery pathway for immediate breast reconstruction at our hospital using virtual and telehealth operative consultation and evaluation during the growing COVID-19 crisis. At the time of writing, Massachusetts ranks fourth in the USA in the number of COVID-19 cases, with our hospital currently treating over 40 COVID-19 patients in the ICU. We are not yet overwhelmed by the surge of patients and, as such, are still able to carry out operations for symptomatic and high stage cancer patients at this time. By performing essential postoperative assessments through remote telemedicine or at-home visits, we hope to reserve availability of inpatient beds for COVID-19 cases and decrease the risk of transmission to patients recovering from immediate breast reconstruction.
Development and implementation of a same-day surgery protocol requires extensive communication and collaboration among primary stakeholders, in an effort to target areas of traditional operative course that can be consolidated or made remote. In light of the COVID-19 pandemic, in-person pre-operative visits were foregone in favor of online evaluation, providing patients with access to educational videos and informative documents to facilitate shared decision making. Importantly, postoperative management was conducted via telemedicine, with the plastic surgeon assessing for immediate complication or the need for in-person evaluation within 24 h of reconstruction. Subsequent 1-week and 2-week visits were conducted virtually, with VNA services utilized for drain removal. These modifications to the existing same-day surgery protocol minimized risk of viral exposure to patients recovering from surgery, particularly important in this patient population that may need to undergo immune compromising chemotherapy [20, 21].
In this report, the average time interval between operation and discharge was 5.02 ± 1.29 h, with no re-admissions or emergency department visits, which is significantly lower than the national average of overnight admission in hospitals employing traditional postmastectomy protocols [22, 23]. Our institution performs an estimated 350–400 immediate breast reconstructions annually. The implementation of a same-day surgery pathway could save the hospital an equivalent number of inpatient bed days, thereby significantly reducing cost and increasing capacity. We recognize that the number of patients in our pilot study is small and our median follow up was 8 days. However, none of the patients experienced complication, demonstrating same-day immediate breast reconstruction to be a safe alternative to conventional treatment paradigm [24–29].
Essential in the development of a successful perioperative pathway is the use of appropriate patient selection criteria. In the case of COVID-19, resource allocation should be prioritized based on tumor burden and cancer grade, thereby providing timely oncologic treatment and breast reconstruction to those with the most immediate need. Non-essential procedures that may provide modest psychologic and physiologic benefit, such as contralateral prophylactic mastectomy, can be avoided in favor of decreasing complications associated with the contralateral breast, which could strain limited medical resources during the postoperative period [30–32]. Recent studies from our group have demonstrated comparable safety profile between direct-to-implant pre-pectoral reconstruction and traditional subpectoral reconstruction [33]. For patients with PMRT, pre-pectoral breast reconstruction is associated with lower rates of capsular contracture and need for revision compared with subpectoral implant placement [15]. In addition, for cases where autologous breast reconstruction is planned, immediate implant placement within the pre-pectoral space can be used as a “space-holder” during the time of crisis as a bridge to subsequent autologous reconstruction when feasible. Since pre-pectoral breast reconstruction is far less resource intensive than autologous free tissue breast reconstruction, a larger number of patients can be treated with this “space-holder,” complete adjunctive chemotherapy or radiation, then complete autologous free tissue transfer at a later date.
Prioritization of patients with high-grade cancer may uniformly increase the baseline operative risk of the entire patient cohort, with greater pre-operative morbidity associated with tumor burden and the tendency toward axillary lymph node dissection, which have previously been demonstrated to be independent risk factors for infection [34–36]. It is important to consider the relative benefit of immediate implant placement versus primary closure and delayed reconstruction. Infection in a patient without prosthesis placement can be successfully treated with oral or intravenous antibiotics. In contrast, infection in those with immediate reconstruction will almost certainly require unplanned return to the operating room resulting in higher resource utilization in the already limited setting of the COVID-19 crisis.
The success of implant-based breast reconstruction is contingent on the viability of the mastectomy skin flap. Patients were counseled that if during surgery the mastectomy skin flap was judged to have viability issues clinically, the implant will not be placed, and the skin flap will be closed after excision of the ischemic area of concern. In all the cases examined, we did not abort implant placement. While autologous reconstruction may improve the viability of the overlying mastectomy skin flap in some instances, the additional resources required for autologous reconstruction renders it difficult to apply during the COVID-19 surge when capacity and resources are limiting factors.
Invariably, the need for resource conservation will continue to rise as cases of COVID-19 increase. For example, the utilization of personal protective equipment (PPE) during COVID-19 for elective operations can be a source of concern for many hospitals around the country. At the time of writing, many hospitals have implemented N95 recycling programs and PPE does not appear to be limiting necessary procedures. Additionally, this pathway of same-day mastectomy and reconstruction is proposed to also be useful during emergence from the COVID-19 surge, where capacity is still under strain as hospitals work through the backlog of patients awaiting oncologic operations.
In the event that patient demand far exceeds supply, hospital networks will need to scale-back on the number of mastectomy and breast reconstruction cases performed, instead diverting resources to treatment efforts for COVID-19. However, in the time interval before or after the peak incidence of COVID-19 surge, we anticipate a tenable need for efficient surgical practice to alleviate the expected backlog of breast cancer cases resulting from the re-allocation of resources toward COVID-19. The merit of this same-day surgery protocol is the ability to safely and efficiently decrease resource utilization, while implementing virtual patient visits to meet the challenges posed by COVID-19. We acknowledge the limitation of the small sample size and short follow-up duration in the present study. However, this patient cohort was well matched compared to those in previous publications from our institution, namely in age and BMI, suggesting that these patients are representative of the patient cohort that normally undergoes mastectomy and immediate breast reconstruction [37]. In addition, immediate postoperative complications that require hospital re-admission and operative management, namely hematoma, tend to occur within 3 days of breast reconstruction [38]. As such, nearly one week of follow-up should be sufficient to identify postoperative hematoma in patients at risk for implant loss and in need of salvage procedures. Therefore, we felt it necessary to disseminate this information in a timely manner given the escalation of the COVID-19 crisis, especially if this protocol can be helpful to our community. Additionally, it stands to reason that this same-day surgery pathway may not be generalizable across all institutions given likely limitations in accessibility, resource funding, and telemedicine capabilities. The success of this same-day protocol does demonstrate that a transition to outpatient surgical facilities for breast reconstruction may be feasible in the near future, given appropriate patient selection, pre-operative counseling, surgical planning, and resource optimization. We hope that this successful implementation of a same-day protocol for immediate breast reconstruction will serve as a framework for other institutions to incorporate techniques or develop efficient, cost-effective pathways for immediate breast reconstruction during these unprecedented times.
Conclusion
This early experience demonstrates that an efficient mastectomy and immediate breast reconstruction can be operationalized to meet acute constraints of hospital capacity and resources. This perioperative pathway can be readily modified to utilize virtual patient visits in the setting of the COVID-19 crisis to conserve resources, increase inpatient capacity, and minimize viral exposure for patients recovering from surgery. This work is particularly timely given the acute need for well-defined protocols for oncologic and reconstructive procedures during the COVID-19 pandemic.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to acknowledge the Procedure Case Transition Workgroup and Operating Room leadership for making the Same Day Surgery protocol possible: Bethaney Daily, Caroline Horgan, Allison Koehler, Alison Laws, Teresa MacDonald, Ann O’Brien, Patrice Osgood, Janet Quigley, Andrew Sherburne, Dale Spracklin, Marianne Turner, and Shin Hae Yoon. This project was initiated as a quality improvement effort. No additional funding supported this work.
Author contributions
NS—Author made substantial contributions to the acquisition of data, interpretation of data, drafting of the work, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. NR—Author made substantial contributions to the acquisition of data, interpretation of data, drafting of the work, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. ET—Author made substantial contributions to the acquisition of data, interpretation of data, drafting of the work, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. OA—Author made substantial contributions to the acquisition of data, interpretation of data, drafting of the work, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. DE—Author made substantial contributions to the conception and design of the work, interpretation of data, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. ECL—Author made substantial contributions to the conception and design of the work, interpretation of data, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work. MS—Author made substantial contributions to the conception and design of the work, interpretation of data, substantively revised draft of work, approved the submitted version and agreed to be both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
Funding
No funds were received for this study.
Compliance with ethical standards
Conflict of interest
Author ECL has consultant agreements with, but is explicitly not a speaker for, Musculoskeletal Transplant Foundation and Allergan Inc., manufacturers of FlexHD and AlloDerm, respectively. Author NS declares that she has no conflict of interest. Author NR declares that she has no conflict of interest. Author ET declares that she has no conflict of interest. Author OA declares that he has no conflict of interest. Author DE declares that he has no conflict of interest. Author MS declares that she has no conflict of interest.
Ethical approval
This work is a clinical quality improvement, patients were followed prospectively. No IRB review is needed for clinical quality improvement that meets standard of care. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This work is a clinical quality improvement, patients were followed prospectively. Informed consent was obtained as per routine standard of care. No additional consent is needed for clinical quality improvement that meets standard of care.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Michelle Specht and Nikhil Sobti have equally contributed to the manuscript as co-first authors.
References
- 1.Brindle M, Gawande A. Managing COVID-19 in Surgical Systems. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, Zhang C, Boyle C, Smith M, Phillips JP. Fair Allocation of Scarce Medical Resources in the Time of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 3.Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8(4):e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Timbie JW, Ringel JS, Fox DS, Waxman DA, Pillemer F, Carey C, Moore M, Karir V, Johnson TJ, Iyer N, Hu J, Shanman R, Larkin JW, Timmer M, Motala A, Perry TR, Newberry S, Kellermann AL. Allocation of scarce resources during mass casualty events. Evid Rep Technol Assess (Full Rep) 2012;207:1–305. [PMC free article] [PubMed] [Google Scholar]
- 5.Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423–431. doi: 10.1016/S0140-6736(09)60137-9. [DOI] [PubMed] [Google Scholar]
- 6.Biddison ELD, Gwon HS, Schoch-Spana M, Regenberg AC, Juliano C, Faden RR, Toner ES. Scarce resource allocation during disasters: a mixed-method community engagement study. Chest. 2018;153(1):187–195. doi: 10.1016/j.chest.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Plastic Surgeons (2020) ASPS Statement on Breast Reconstruction in the face of COVID-19 Pandemic. https://www.plasticsurgeryorg/. Accessed 2 April 2020.
- 8.Kadhim M, Gans I, Baldwin K, Flynn J, Ganley T. Do surgical times and efficiency differ between inpatient and ambulatory surgery centers that are both hospital owned? J Pediatr Orthop. 2016;36(4):423–428. doi: 10.1097/BPO.0000000000000454. [DOI] [PubMed] [Google Scholar]
- 9.Panda N, Solsky I, Haynes AB. Redefining shared decision-making in the digital era. Eur J Surg Oncol. 2019;45(12):2287–2288. doi: 10.1016/j.ejso.2019.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cordeiro E, Jackson T, Cil T. Same-day major breast cancer surgery is safe: an analysis of short-term outcomes using NSQIP data. Ann Surg Oncol. 2016;23(8):2480–2486. doi: 10.1245/s10434-016-5128-0. [DOI] [PubMed] [Google Scholar]
- 11.Cordeiro E, Zhong T, Jackson T, Cil T. The safety of same-day breast reconstructive surgery: an analysis of short-term outcomes. Am J Surg. 2017;214(3):495–500. doi: 10.1016/j.amjsurg.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 12.McGugin CJ, Coopey SB, Smith BL, Kelly BN, Brown CL, Gadd MA, Hughes KS, Specht MC. Enhanced recovery minimizes opioid use and hospital stay for patients undergoing mastectomy with reconstruction. Ann Surg Oncol. 2019;26(11):3464–3471. doi: 10.1245/s10434-019-07710-3. [DOI] [PubMed] [Google Scholar]
- 13.Vuong B, Graff-Baker AN, Yanagisawa M, Chang SB, Mentakis M, Shim V, Knox M, Romero L, Kuehner G. Implementation of a post-mastectomy home recovery program in a large, integrated health care delivery system. Ann Surg Oncol. 2019;26(10):3178–3184. doi: 10.1245/s10434-019-07551-0. [DOI] [PubMed] [Google Scholar]
- 14.Keehn AR, Olson DW, Dort JC, Parker S, Anderes S, Headley L, Elwi A, Estey A, Crocker A, Laws A, Quan ML. Same-day surgery for mastectomy patients in Alberta: a perioperative care pathway and quality improvement initiative. Ann Surg Oncol. 2019;26(10):3354–3360. doi: 10.1245/s10434-019-07568-5. [DOI] [PubMed] [Google Scholar]
- 15.Sobti N, Weitzman RE, Nealon KP, Jimenez RB, Gfrerer L, Mattos D, Ehrlichman RJ, Gadd M, Specht M, Austen WG, Liao EC. Evaluation of capsular contracture following immediate pre-pectoral versus subpectoral direct-to-implant breast reconstruction. Sci Rep. 2020;10(1):1137. doi: 10.1038/s41598-020-58094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gfrerer L, Liao EC. Technique refinement in pre-pectoral implant breast reconstruction with vicryl mesh pocket and acellular dermal matrix support. Plast Reconstr Surg Glob Open. 2018;6(4):e1749. doi: 10.1097/GOX.0000000000001749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Srinivasa DR, Holland M, Sbitany H. Optimizing perioperative strategies to maximize success with pre-pectoral breast reconstruction. Gland Surg. 2019;8(1):19–26. doi: 10.21037/gs.2018.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shahbazi S, Woods SJ. Influence of physician, patient, and health care system characteristics on the use of outpatient mastectomy. Am J Surg. 2016;211(4):802–809. doi: 10.1016/j.amjsurg.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 19.Qin C, Antony AK, Aggarwal A, Jordan S, Gutowski KA, Kim JY. Assessing outcomes and safety of inpatient versus outpatient tissue expander immediate breast reconstruction. Ann Surg Oncol. 2015;22(11):3724–3729. doi: 10.1245/s10434-015-4407-5. [DOI] [PubMed] [Google Scholar]
- 20.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel Coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 hospitalized patients with 2019 Novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bian J, Krontiras H, Allison J. Outpatient mastectomy and breast reconstructive surgery. Ann Surg Oncol. 2008;15(4):1032–1039. doi: 10.1245/s10434-007-9762-4. [DOI] [PubMed] [Google Scholar]
- 23.Kruper L, Xu XX, Henderson K, Bernstein L, Chen SL. Utilization of mastectomy and reconstruction in the outpatient setting. Ann Surg Oncol. 2013;20(3):828–835. doi: 10.1245/s10434-012-2661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seth AK, Hirsch EM, Kim JY, Dumanian GA, Mustoe TA, Galiano RD, Fine NA. Hematoma after mastectomy with immediate reconstruction: an analysis of risk factors in 883 patients. Ann Plast Surg. 2013;71(1):20–23. doi: 10.1097/SAP.0b013e318243355f. [DOI] [PubMed] [Google Scholar]
- 25.Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg. 2003;112(2):467–476. doi: 10.1097/01.PRS.0000070727.02992.54. [DOI] [PubMed] [Google Scholar]
- 26.Fischer JP, Wes AM, Tuggle CT, Nelson JA, Tchou JC, Serletti JM, Kovach SJ, Wu LC. Mastectomy with or without immediate implant reconstruction has similar 30-day perioperative outcomes. J Plast Reconstr Aesthet Surg. 2014;67(11):1515–1522. doi: 10.1016/j.bjps.2014.07.021. [DOI] [PubMed] [Google Scholar]
- 27.Fischer JP, Nelson JA, Au A, Tuggle CT, 3rd, Serletti JM, Wu LC. Complications and morbidity following breast reconstruction–a review of 16,063 cases from the 2005–2010 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(2):104–114. doi: 10.3109/2000656X.2013.819003. [DOI] [PubMed] [Google Scholar]
- 28.Wink JD, Fischer JP, Nelson JA, Serletti JM, Wu LC. Direct-to-implant breast reconstruction: an analysis of 1612 cases from the ACS-NSQIP surgical outcomes database. J Plast Surg Hand Surg. 2014;48(6):375–381. doi: 10.3109/2000656X.2014.899240. [DOI] [PubMed] [Google Scholar]
- 29.Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109(7):2265–2274. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 30.Allen RJJ, Sobti N, Patel A, Matros E, McCarthy CM, Dayan JH, Disa JJ, Mehrara BJ, Morrow M, Pusic AL, Nelson JA (2020) Laterality and patient-reported outcomes following autologous breast reconstruction with free abdominal tissue: an 8-year examination of BREAST-Q data. Plast Reconstr Surg In Press [DOI] [PMC free article] [PubMed]
- 31.King TA, Sakr R, Patil S, Gurevich I, Stempel M, Sampson M, Morrow M. Clinical management factors contribute to the decision for contralateral prophylactic mastectomy. J Clin Oncol. 2011;29(16):2158–2164. doi: 10.1200/JCO.2010.29.4041. [DOI] [PubMed] [Google Scholar]
- 32.Portschy PR, Kuntz KM, Tuttle TM. Survival outcomes after contralateral prophylactic mastectomy: a decision analysis. J Natl Cancer Inst. 2014 doi: 10.1093/jnci/dju160. [DOI] [PubMed] [Google Scholar]
- 33.Nealon KP, Weitzman RE, Sobti N, Gadd M, Specht M, Jimenez RB, Ehrlichman R, Faulkner HR, Austen WG, Jr, Liao EC. Pre-pectoral direct-to-implant breast reconstruction: safety outcome endpoints and delineation of risk factors. Plast Reconstr Surg. 2020;145(5):898e–908e. doi: 10.1097/PRS.0000000000006721. [DOI] [PubMed] [Google Scholar]
- 34.Nealon KP, Sobti N, Gadd M, Specht M, Liao EC. Assessing the additional surgical risk of contralateral prophylactic mastectomy and immediate breast implant reconstruction. Breast Cancer Res Treat. 2020;179(2):255–265. doi: 10.1007/s10549-019-05460-0. [DOI] [PubMed] [Google Scholar]
- 35.Madsen RJ, Esmonde NO, Ramsey KL, Hansen JE. Axillary lymph node dissection is a risk factor for major complications after immediate breast reconstruction. Ann Plast Surg. 2016;77(5):513–516. doi: 10.1097/SAP.0000000000000653. [DOI] [PubMed] [Google Scholar]
- 36.Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Giuliano AE, American College of Surgeons Oncology G Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007;25(24):3657–3663. doi: 10.1200/JCO.2006.07.4062. [DOI] [PubMed] [Google Scholar]
- 37.Sobti N, Ji E, Brown RL, Cetrulo CL, Jr, Colwell AS, Winograd JM, Austen WG, Jr, Liao EC. Evaluation of acellular dermal matrix efficacy in prosthesis-based breast reconstruction. Plast Reconstr Surg. 2018;141(3):541–549. doi: 10.1097/PRS.0000000000004109. [DOI] [PubMed] [Google Scholar]
- 38.Grippaudo FR, Renzi L, Costantino B, Longo B, Santanelli F. Late unilateral hematoma after breast reconstruction with implants: case report and literature review. Aesthet Surg J. 2013;33(6):830–834. doi: 10.1177/1090820X13496249. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


