Abstract
This study sought to understand the acceptability and feasibility of office-based nurse care management in medium to large rural primary care practices. A qualitative assessment of Care Management Plus (a focused medical home model for complex patients) implementation was conducted using semistructured interviews with 4 staff cohorts. Cohorts included clinician champions, clinician partners, practice administrators, and nurse care managers. Seven key implementation attributes were: a proven care coordination program; adequate staffing; practice buy-in; adequate time; measurement; practice facilitation; and functional information technology. Although staff was positive about the care coordination concept, model acceptability was varied and additional study is required to determine sustainability.
Keywords: medical informatics applications, nursing care management, organizational innovation, patient care team, patient care management, primary care, rural
CHRONIC illness care dominates the clinic schedules of family physicians, general internists, and many pediatricians (Colwill, Cultice, & Kruse, 2008; Wise, 2007). The typical adult primary care clinician coordinates care for their panel of Medicare patients with 229 other physicians in 117 different practices (Pham, O’Malley, Bach, Saiontz-Martinez, & Schrag, 2009). Data from the National Health Interview Survey reported that 2% of all children had a chronic illness that limited their activities in 1962 as compared with 8% of children in 2003 (Wise, 2007). Given these challenges of addressing chronic care needs in practices designed to deliver acute care, many organizations currently encourage the integration of care coordination into primary care clinics.
Care coordination is a foundational component of primary care as defined by the Institute of Medicine (Institute of Medicine, 1994) and is one of the 7 principles of the patient-centered medical home (American Academy of Family Physicians, 2007). A 2007 Agency for Health Care Research and Quality (AHRQ) technical report listed 49 definitions for care coordination and related concepts (McDonald et al., 2007). The National Quality Forum endorsed care coordination as a function of primary care that helps ensure the patient’s needs and preferences for health services and information sharing across people and sites are met over time. Coordination maximizes the value of services delivered to patients by facilitating beneficial, efficient, safe, and high-quality patient experiences and improved health care outcomes (National Quality Forum, 2009).
Studies exploring efforts to implement care coordination to improved chronic illness care have demonstrated the monumental challenges practices face. Casalino found that 2 major factors contributing to the care management process for chronic illness were external incentives and information technology (Casalino et al., 2003). Bodenheimer found that the 2 most common facilitators were strong leadership and an organizational culture that placed a high value on quality; while barriers included inadequate information technology, reimbursements unrelated to quality, poor financial position, physician resistance, and physician time constraints (Bodenheimer et al., 2004). A qualitative study of small and medium size clinics implementing the chronic care model identified too many competing priorities, lack of specificity and agreement about the care process changes desired and lack of physician engagement as challenges (Hroscikoski et al., 2006).
In primary care settings, coordination of care has been of poor quality with adverse health care outcomes and poor satisfaction among providers and patients (O’Malley, Tynan, Cohen, Kemper, & Davis, 2009; Schoen et al., 2007; Smith et al., 2005). Models have been proposed to develop a systematic approach to providing care for complex patients with multiple medical needs. Initially, many of these approaches were started by payers; recently, models began to integrate care coordination into primary care practices. These models are more likely to be present in larger practices, often operated by hospitals and health care systems. One model, Care Management Plus (CM+), has been shown to be effective by demonstrating positive clinical and economic outcomes in a large health system (Dorr et al., 2006; Dorr, Wilcox, Brunker, Burdon, & Donnelly, 2008). Dissemination of a care management model such as CM+ to smaller practice settings has not previously been studied, despite the fact that three-fourths of primary care practices employ 5 or fewer physicians (Hing & Burt, 2008).
Although a number of studies have examined the facilitators and barriers to primary care redesign efforts from the vantage point of the clinician or organizational characteristics (Bodenheimer et al., 2004; Casalino et al., 2003), few studies on practice change have explored perceptions by practice role of a care coordination intervention. Therefore, we undertook this qualitative assessment to explore divergences and convergence among the views of the clinician champions, clinicians, administrators, and nurse care managers (NCMs) regarding efforts to incorporate nurse care management into a diverse group of rural, mid-sized family medicine, and pediatric practices.
METHODS
Study aims
The present study was a collaborative partnership between the Oregon Rural Practice-Based Research Network (ORPRN), CM+ research team, and 6 primary care clinics in rural Oregon. Our study was in response to the AHRQ Master Contract Task Order request to assess the clinical impact of and business case for nurse-based care management.
This qualitative analysis explored convergence and divergence in perceptions among the 4 practice cohorts (clinician champion, clinicians, administration, and care managers) regarding implementation of nurse care management in mid-sized, rural primary care practices. Data presented are one component of the overall mixed methods evaluation procedure. The Oregon Health & Science University institutional review board approved this study.
Study design
The study utilized a matched design with staggered implementation among the 6 clinics, such that there were 3 immediate intervention practices and 3 delayed intervention control practices. The AHRQ Task Order emphasized recruiting practices that were health information technology enabled and of sufficient size to test the care coordination intervention. Each intervention practice was matched to a control practice based on criteria including size, specialty (pediatric or adult care), insurance of patient panel (prevalence of Medicaid, Medicare, or private insurance), presence of a care manager, level of expertise with chronic illness care, electronic medical record functionality, organizational leadership, and primary care orientation. Table 1 describes the characteristics of the 6 clinics. The 2-year project began in October 2007. The first group implemented nurse care manager services over 18 months and the second group of clinics implemented 12 months later over 6 months.
Table 1.
Summary of Key Characteristics of Selected Clinicsa
| Clinic |
||||||
|---|---|---|---|---|---|---|
| Characteristic | A | D | E | F | C | B |
| Intervention group | Immediate | Immediate | Immediate | Delayed | Delayed | Delayed |
| Specialty | Family medicine | Family medicine | Pediatrics | Family medicine | Family medicine | Pediatrics |
| Physician clinicians | 9 | 4 | 4 | 3 | 7 | 5 |
| Nonphysician clinicians | 3 | 4 | 0 | 4 | 4 | 2 |
| Active patients in practice | 11,312 | 9,936 | 6,180 | 6,627 | 12,647 | 12,813 |
| Ownership | Not for profit | Private practice | Private practice | Not for profit | Not for profit | Private practice |
| % Female | 50% | 60.3% | 53% | 61% | 60% | 49.5% |
| Patient age–changed to average age | ||||||
| Average age | 38.33 | 41.58 | 8.38 | 42.13 | 38.93 | 12.12 |
| Overall payment breakdown | ||||||
| Medicare | 31% | 17% | 20% | 17% | 22.6% | 0% |
| Medicaid | 17% | 42% | 30% | 20% | 22.6% | 54% |
| Private | 40% | 37% | 20% | 55% | 22.2% | 43% |
| No insurance | 8% | 3% | 10% | 3% | 32.1% | 2% |
| Racial/ethnic composition of patient population | ||||||
| % White | 96% | 99% | 98.5% | 98.5% | 96.4% | 96.6% |
| % Hispanic | 30% | 1% | 3% | 0.5% | 16% | 38% |
| Electronic health record | NextGen | Centricity | Practice one | Epic | Epic | Misys healthcare |
Data from 2007 ORPRN Practice Member Survey.
Intervention
We utilized CM+, a care coordination model developed by Dorr and colleagues (Dorr, Wilcox, McConnell, Burns, & Brunker, 2007; Dorr et al., 2008), as the intervention framework. Care Management Plus incorporates several components, including training care managers around both disease-specific education and principles of care management as well as equipping clinics with the care management tracking software. The care manager software includes a tracking database, patient summary sheets, and messaging systems to help providers access care plans, remind them about best practices, and facilitate communication among the health care team (Figure 1).
Figure 1.
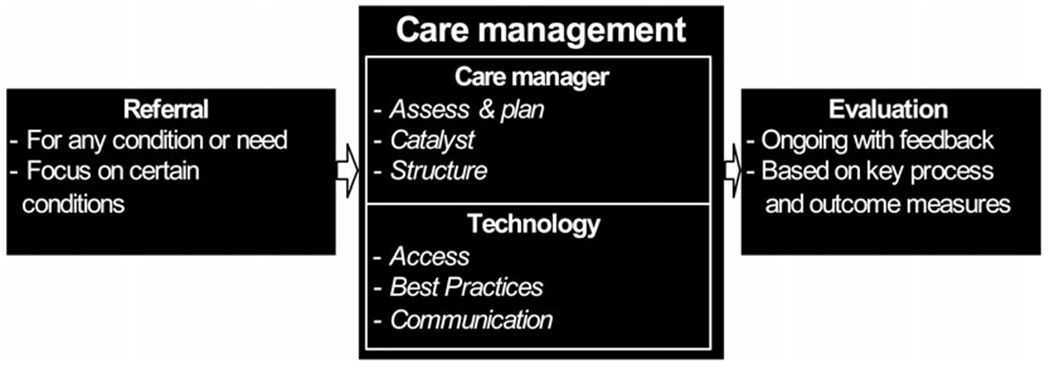
Components of the Care Management Plus Program.
Care Management Plus website, http://caremanagementplus.org/about.html. Figure adapted with permission.
Practice recruitment/settings
We used targeted recruitment of primary care practice members of ORPRN. We selected practices based on geographic spread, presence of an electronic health record, having 4 or more providers, expressed interest to participate, and an ability to match between clinics on size, ownership, and specialty. Practices agreed to appoint a care manager and provider lead, participate in the CM+ training, use the IT tools, and track and complete care coordination tasks. Clinics used their own funds to hire the care manager, and only received reimbursement for data collection.
Interview participants
At each practice members of 4 cohorts were eligible to participate in the interviews: clinician champions, clinicians, practice administrators/managers, and nurse care managers. Participation in the postintervention interviews was restricted to those who participated in the preintervention interviews. We identified the clinician champion as the physician who provided the initial contact to bring the study into the clinic and provided overall advice and guidance in its implementation. Both physicians and nonphysician providers (physician assistants and nurse practitioners) were included under the clinician cohort. Administrative staff included practice managers and/or clinic administrators and the nurse care management cohort consisted of those who had been selected to fill this position.
Qualitative design
We conducted one-on-one semistructured interviews with eligible participants at the 6 participating clinics. Interviews occurred prior to the start of the intervention at each site and again approximately 1 year later. Because of the delayed intervention study design, we interviewed clinics involved in the immediate intervention in January 2008 and January 2009 whereas delayed intervention clinics were interviewed in November and December 2008 with postintervention interviews in September of 2009. Preintervention interviews explored respondent perceptions of ideal outcomes from participation, barriers to implementation, and understanding regarding the current practice change (Appendix 1). Postintervention questions explored perceived success with implementation, facilitators, and barriers to implementation, and steps needed to move the project forward.
Analyses
Detailed field notes were taken during each key informant interview and transcribed for coding and thematic analysis. Responses from the immediate intervention and delayed intervention practices were analyzed simultaneously. We used grounded theory (Glaser & Strauss, 1967; Strauss & Corbin, 1998) for data coding, as this approach allowed themes to emerge directly from the respondent language rather than forcing responses into a predetermined coding template. Four authors (L.F., M.D., P.M., J.M.) independently reviewed and coded the interviews, then met as small groups of 2 or 3 to discuss individual codes, and finally met as a unified group to reconcile the emergent qualitative themes. This iterative process and triangulation by multiple analysts is an important source of rigor in qualitative research, and helps to assure the robustness and trustworthiness of themes (Cohen & Crabtree, 2008a, 2008b; Frankel, 1999; Miller & Crabtree, 1999).
RESULTS
Forty-five preintervention interviews and 36 postintervention interviews were conducted with members of the 4 clinic cohorts. Participant training characteristics are summarized in Table 2.
Table 2.
Training Characteristics of Qualitative Interview Participants
| Cohort | Preintervention | Postintervention |
|---|---|---|
| Clinician champion | 6 | 6 |
| Clinician partners | ||
| Physician | 14 | 10a |
| PA or NP | 8 | 6b |
| Practice administrator | 6 | 6 |
| Nurse care manager | 11 | 8c |
| Total | 45 | 36 |
Four physicians left the practices or retired during the study.
Two nonphysician clinicians were unavailable for postintervention interviews.
Three NCMs did not participate in the postintervention interviews. Two RNs were trained but never served as NCMs in their practices. One NCM left practice prior to the postintervention interview.
Analysis consolidated themes into 4 categories: (1) barriers to delivering chronic illness care, (2) perceived challenges of practice change associated with implementing nurse care management, (3) reported barriers and facilitators of successful implementation, and (4) resources necessary to maintain the care coordination intervention.
BARRIERS TO CHRONIC DISEASE MANAGEMENT
Our participants reported various challenges with delivering chronic illness care in the current medical system, including both patient and clinic factors as summarized in Table 3.
Table 3.
Barriers to Chronic Disease Management in Current Practice and Preimplementation Perceptions of Challenges Associated With Nurse Care Management
| Barriers to Chronic Disease Management in Current Practice | Barriers to Practice Change (ie, Implementing Nurse Care Management) | |
|---|---|---|
| Patient factors | Behavioral barriers Lack of patient resources |
Resistance to behavior change |
| Clinic factors | Access to care | Clarifying role definitions |
| Time: payment structure and 15-minute office visits | Resource concerns: time and money | |
| No patient registries and reminders | Change is hard IT implementation challenges |
Patient barriers
Participants emphasized that patient behaviors presented challenges to delivering chronic illness care. All 4 cohorts identified a lack of patient compliance with treatment plans or “buy-in” regarding personal ownership of the disease and their responsibility to self manage. Likewise, all cohorts mentioned a lack of patient physical and social resources such as transportation, insurance coverage, and health literacy as barriers.
Access to care
Across the 4 cohorts there was strong congruence with the sentiment that there were just too few primary care providers. Clinicians reported feeling overwhelmed and unable to provide the desired continuity of care. Administrators and care managers echoed this stating, “there is too much patient demand” and emphasizing that patients cannot always get in to “their” doctors when needed. One clinician also noted that access to specialists for Medicaid referrals was a significant barrier.
Time
Associated with inadequate provider supply was a perception across cohorts that “there was just not enough time.” The champion, clinician, and care managers felt that not having time for education was the result of too many patient visits. As one provider stated, “I’m just trying to keep them alive this week.” Another clinician reiterated this statement saying that effective care for the chronically ill was hampered mostly by the time the providers have available, and the problem of trying to manage a chronic illness when the patient was in the clinic for some other acute illness. Although care managers and administration acknowledged that time for patient education or care coordination was a barrier to chronic illness care, they also emphasized that staff other than the clinicians could complete these tasks.
Patient registries and reminders
Cohorts identified they lacked systems to track patients needing follow-up or to proactively manage populations. Many respondents reported that “closing the loop” was a problem for patient care. For example, one clinician stated he did not know what happens when patients fail to show for follow-up appointments, and the clinic had no system in place for outreach to get them back in. Nurse care managers also mentioned that clinicians are often part-time and there is not enough information for adequate cross coverage.
PERCEIVED BARRIERS TO NCM IMPLEMENTATION
Our respondents perceived many challenges that could occur when implementing CM+ into their clinical settings (see Table 3). Many of these barriers were associated with managing practice change.
Role definitions
All 4 cohorts commented that understanding the job descriptions and roles of the nurse care manager was a potential barrier. Participants mentioned the importance of getting clinic-wide buy-in and fears about “stepping on people’s toes.” One practice administrator voiced her concern that staff “not knowing how to operate as a team” would be the biggest barrier to program adoption.
Resource concerns—time and money
The 4 cohorts strongly agreed that time and money were key barriers to integrating CM+. Clinics struggled with identifying funds for the NCM position. As one NCM succinctly stated, her concern was “who will do it and how will it be paid for.” Time for both the management of the NCM role and for prioritizing NCM tasks was commonly perceived as the biggest challenge to adoption.
Change is hard
Various respondents across the 4 cohorts indicated that “any change within the practice is hard” and that adoption of the CM+ program would be no different. One clinician commented “anything that breaks the flow of how things are currently conducted, even if it is not done well, [is a barrier].” One clinician noted that asking NCMs to provide care coordination could result in staff resistance.
IT implementation challenges
Clinician champions and the clinicians reported that there may be technical challenges in implementing CM+; and several clinician champions reported that having the NCM do double entry into both the CM+ tracking system and the clinic’s EHR would be a barrier. In addition, limited IT support at the practice and challenges getting software to interface with the clinic EHR were seen as potential sources of frustration by the clinicians and clinician champions. Prior to implementing CM+, neither the administration nor the nurse care managers mentioned that IT might be a barrier.
IDEAL OUTCOMES AND OUTCOMES ACHIEVED
As summarized in Table 4, 6 ideal outcomes were associated with implementing nurse care management. Following implementation, respondents identified 4 key areas where they perceived “success” with CM+ implementation (see Table 4). These achievements paralleled the ideal outcomes and included incorporating NCM into routine care, having a more systematic way to coordinate patient care and follow-up, finding preliminary evidence of improved patient care, and receiving positive responses from both clinician and patient NCM users. Although there was considerable heterogeneity in the level at which CM+ had been integrated into each practice, in general, clinician champions, clinicians, office managers, and care managers felt they were moving in the right direction toward meeting their ideal outcomes. However, many also expressed that it was “too early to tell” and that they lacked data to confirm their perceptions.
Table 4.
Qualitative Themes Associated With Ideal Outcomes From Participation in the Nurse Care Manager Study, Postimplementation Successes, and Facilitators and Challenges to Successful Implementation
| Preimplementation Interviews Ideal Outcomes | Postimplementation Interviews |
||
|---|---|---|---|
| Postimplementation Successes | Facilitators of Success | Challenges to Success | |
| Care coordination and patient follow-up | NCM incorporated into routine care | NCM is “the right person for the job” | Finding the right person for the NCM role |
| Improved patient outcomes/quality of care | Systematic way to track care and communicate outcomes | Leadership across cohorts | Limited clinic resources (ie, time, financing, personnel) |
| Increased clinic efficiency | Improved patient care and clinical/community services | Developing a team-based care approach | Lack of support from clinic administration/management |
| Improved team care | Positive response from CMP “users” (patients and clinicians) | Practice facilitation | Integrating the NCM role takes time |
| Increased patient self-management | Prioritizing the time to change | Resistance to change (clinician or staff behaviors) | |
| Enhanced information sharing through health IT | Having systems in place prior to implementation | Technical barriers | |
| Limited patient resources | |||
FACILITATORS OF SUCCESSFUL NCM IMPLEMENTATION
Numerous facilitators were identified, which helped the practices implement the CM+ program (see Table 4).
NCM is “the right person for the job”
A key facilitator of success identified by the clinician champion, clinicians, and administration was that “you must get the right people for the job.” One lead clinician said that the key factor to successful implementation of nurse care management is that “they [clinic NCMs] are the right people for the job and care deeply about getting it right. They want to make it succeed.” Practice clinicians and administration echoed these sentiments.
Leadership and accountability
All 4 cohorts emphasized providing time and support for successful NCM implementation was based on the leadership of the clinician champion, administration, and nurse care manager team. These partners were important in developing the structure for NCM referrals, establishing the scope of work that NCMs could perform, and bringing the energy, and enthusiasm to the project to move the change forward. One clinician emphasized how important it was to organize the system to successfully implement CM+ through “clarity of task, direction from leadership, organization of the team, and empowerment of staff.”
Developing the team-based care approach
Lead clinicians emphasized how they needed to prioritize the NCM’s time and to use the NCM in support of their practice activities. As one clinician stated, “it’s nice to know there is something else to offer these patients other than another normal office visit.” Administration emphasized the importance of getting “buy-in” from all people in the clinic, including care managers, clinicians, and other back office staff as a key to successful implementation. The care managers described the importance of building trust among the clinic cohorts, marketing the role of the NCM to the clinicians (to facilitate uptake), and receiving patient referrals through a “warm handoff,” which facilitates relationship development with the patient. These examples all demonstrate movement toward team-based approaches to care.
Practice facilitation
Clinician champions, administration, and care managers emphasized the value of practice facilitation by the ORPRN project team to provide encouragement, ensure regular communication, and help problem solve issues such as software utilization. One clinician champion commented “[the ORPRN facilitator’s] interventions were needed to get things going after the slow start” and a NCM commented “[she] was always willing to do what was needed to get the process up and running.” Another administrator commented that “it was good to have a connection with Oregon Health and Science University and that gave the group the feeling they were doing important work and part of something bigger.”
BARRIERS TO SUCCESSFUL IMPLEMENTATION
Interviews also identified several obstacles to successful implementation of the CM+ program (see Table 4).
Finding the right person for the NCM role
All cohorts emphasized the importance of finding staff with the appropriate attributes as a vital component of implementing CM+. Some participants expressed challenges with locating the right person for the job, whereas others commented that a NCM had been hired, but they did not want the position. One nurse unwillingly had the duties of the NCM added on to her current tasks as the clinic chronic disease manager; she stated, “[I] wasn’t the right person to hire as the Care Manager. [I] never really wanted the job … the personality and attributes … should be more important than the credentials. [Clinic administration] thought I would change and learn.”
Limited clinic resources
All cohorts identified the barriers associated with inadequate clinician supply and the challenges that placed on scheduling. The administration and nurse care managers emphasized that in cases where staffing was inadequate, often NCMs were pulled back into traditional nursing duties rather than focusing their time on care coordination and proactive patient management. In comparison, clinicians identified that staffing issues resulted when the best nurses were removed from their previous roles to serve in the capacity of a care manager. In parallel, but unrelated to our project design, one pediatric practice received a grant from an insurance company to hire a full time care manager. This administrator commented, “if we didn’t have a grant to cover the cost of the care manager, the program would not have happened.”
Lack of support from clinic administration/management
If clinic administration was not on board, nurse care management implementation was dead in the water. As one lead clinician stated, “If administration doesn’t support it, it won’t happen.”
Integrating the NCM role takes time
All cohorts emphasized that integrating care management was a slow process. Many respondents expressed that it took a while for the clinicians to recognize what the NCMs do and to use their services. As one administrator commented, the “staff [were] learning how to work as a team.” In regard to what he would have changed regarding NCM implementation, one clinician stated that he “would have used the services of the care manager earlier.” He expressed that people need to experience things to trust the process and people. Care managers echoed this perception stating that “[use of NCM] increased a bit once the clinicians had a good experience with the process… .providers need to develop a better mind-set that they have another “team member” to rely upon.” In addition, as one clinician champion explained, sometimes other clinicians perceived that the NCMs were not readily available to them, thus the clinic had to develop a system for communicating where and how to utilize the NCMs.
Resistance to change
All cohorts identified challenges associated with getting clinicians to work as team members. One clinician champion lamented about how “hard it has been selling [NCM] to the doctors.” Some NCMs echoed this sentiment, stating that getting the doctors to get on board was a challenge to implementation. One administrator mentioned that it was difficult to get care managers to take on additional tasks, particularly if the project was building on their previous duties.
Technical barriers
Some clinics experience technical difficulties getting the CM+ software installed and functioning in their clinics. In these cases, technical difficulties were identified across all cohorts as a barrier to implementation. Some clinicians and administrators noted that lack of functionality in their EHR systems compounded these challenges.
Limited patient resources
Limited patient resources including transportation, understanding, skills with selfmanagement, or community supports were also identified as barriers to implementation.
DISCUSSION
These interviews across 6 diverse rural primary care practices provide insight regarding the challenges to delivering chronic illness care as well as the barriers and facilitators to successfully implementing care coordination for complex patients. Our qualitative results found considerable congruence among the 4 practice roles (clinician champions, clinician partners, practice administrators, and nurse care managers). The comments across these cohort roles reflect barriers that have been reported in other studies of changing practice care patterns including time, money, and staffing (Bodenheimer et al., 2004; Hroscikoski et al., 2006; Solberg, 2007).
In general, clinician responses closely mirrored those of the clinic champion. Comments by these cohorts focused on clinic functioning, access to care, and timely service, and management of their patients. Although responses across the cohorts revealed similar themes, practice administrators tended to focus on maximizing clinic efficiency, and NCMs emphasized the specific tasks and functions they performed in their roles.
Five resources were frequently mentioned as important to sustain this type of practice change: increased staffing, a viable financial model, clinician buy-in and support, relevant measures and accurate data, and a functional interface between the CM+ software and the EHR. The results from our study of implementing a care coordination program such as CM+ in nonacademic, midsized rural primary care settings indicate 7 “light switches” that need to be turned on to ensure the availability of these resources and the overall success of the program.
A proven care coordination program. Care Management Plus provided an evidence-based program with published results that demonstrate improved practice efficiency, quality of care, and economic viability (Dorr et al., 2007). Our study represented an opportunity for rural clinics to systematically implement a care coordination program that had proven effective in other primary care settings. Using CM+ as the intervention connected these individual clinics to a larger organizational mission, provided standardized training regarding the roles and responsibilities of the NCMs, and integrated an IT system designed for population management and care coordination.
Adequate staffing for care coordination. Practices required resources to adequately staff for the care coordination intervention. These included identifying the financial resources to hire a NCM, as well as locating and appointing a qualified individual to the role. The need for financial sustainability was most often mentioned by the clinician partners with general agreement by the clinician champion and practice administrator. As mentioned earlier, all cohorts felt that a key element to successful implementation of CM+ was identifying the “right person” as the NCM. On the basis of the assumption that nurses, medical assistants, or other support staff were already performing some aspects of care coordination in each clinic setting, this study encouraged practices to develop a NCM position and to fill it with existing staff. Allocating staff time to this new or expanded role meant filling nursing and medical assistant gaps created by the care model. Whether or not NCMs were new to the role, in most cases they looked for support, encouragement, and direction from the clinician champion, practice administration, and research team.
Buy-in across the practice. Leadership from practice administration and buy-in across the practice were key elements of successfully implementing CM+. In many clinics the vision of the clinician champion and support of practice administration set a strong foundation for the necessary practice changes. However, diffusion of the vision to clinician partners and staff was an on-going process that required dedicated time. Creating this shared vision was facilitated with team meetings, role definitions, and the passage of time during which clinicians had positive experiences with the care management process. Unlike previous studies, the clinicians in our study were not driven to change by extrinsic factors (ie, financial incentives, orders from the health system, or promotion), which may commonly occur in larger organizations. Clinicians and their staff were driven by the intrinsic motivation that the current system of chronic illness care is inadequate and that there are better models.
Time for change. Integration of CM+ into these clinics required dedicated time for change. This includes time for the NCMs to develop their roles and responsibilities, for clinicians to learn when and how to utilize this new resource, and for the practice as a whole to enhance their team-based approach to delivering care. Clinician and staff shortages, large patient panel sizes, and the need to generate revenue represented challenges to allocating time for change. Besides the day-to-day time requirements, research indicates practice change takes longer than 12 to 24 months (Counsell et al., 2007; Gagnon, Schein, McVey, & Bergman, 1999; Sledge et al., 2006).
Measurement. Collecting, reporting, and reflecting on outcome measures are the fifth switch. Many of our participants felt that CM+ implementation was going well, but they lacked quantitative data to confirm these impressions. Studies have shown that measurement is a tool to overcoming physician resistance (Wolfson et al., 2009). The clinician partners and practice administrators targeted the need for accurate measures demonstrating economic and clinical benefits of integrating CM+.
Practice facilitation. The sixth switch was the need for ongoing facilitation of practice change, both internally and externally. Skilled external facilitation by the Practice Enhancement Research Coordinators and the CM+ project team provided the coaching necessary to keep the practices engaged with the care coordination intervention (American Academy of Family Physicians, 2009; Nutting et al., 2009). Practice Enhancement Research Coordinators were an ongoing presence who served as a liaison between the practices and the research team and stepped in to intervene when blockades arose through activities such as addressing the challenges of IT implementation, facilitating connections between NCMs at the 6 implementation sites, gathering quality measure data, and keeping an eye to the overall project timeline.
Functional health information technology. Health information technology capacity and functioning was important to many of the participants. The NCM and practice administrators expressed a desire for an interface between the CM+ software and the EHR.
STUDY STRENGTHS AND LIMITATIONS
Our study utilized a relatively unexplored methodological approach to evaluate perceptions to practice change across cohorts between practices, as opposed to case studies by individual clinic settings. Interviewing diverse members of the clinic staff, in addition to the clinicians, allowed us to obtain deeper understanding of underlying issues, silent majority, and minority viewpoints of implementing care management into small primary care practices. Exploration of perceptions by role in the practice emphasized the work of others, which indicates that development of a practice team is necessary to effectively implement care coordination for a defined patient population (Bodenheimer, Chen, & Bennett, 2009; Solberg, 2007). However, reporting on the perceptions of clinic staff by role across a diverse set of practices did not allow us to elaborate on the practice characteristics that influenced the participants’ perceptions.
A strength and limitation of the present study is therefore that the practices reflect a high degree of heterogeneity in terms of specialty, ownership, size, degree of rurality, and history of prior practice redesign efforts. A limitation is that small practices, which provide much of primary care in rural areas, were not included in the study. The findings from our study came from health information technology enabled medium- to large-sized practices that have increasing relevance to rural communities. Our rural network reflects increasing practice size as the mean ORPRN practice has increased from 3.63 clinicians in 2005 to 4.27 clinicians in 2007 (Fagnan et al., 2007). Nationally, the Community Tracking Study from the Center for Studying Health System Change notes that physicians are moving away from solo and 2 physician practices toward mid-sized single specialty groups of 6 or more physicians (Liebhaber & Grossman, 2007). Homogeneity among the practices was reflected by their being primary care, rural, members of ORPRN, and having not previously implemented a program of care coordination with a trained nurse care manager. With this qualitative report we did not analyze the responses by practice where contextual factors influenced care coordination implementation and adoption and we look forward to addressing this in a future manuscript. Despite variations in these contextual factors, our analyses allowed us to identify prominent barriers and facilitators to implementing CM+ across diverse practices and personnel roles in small, rural clinics.
Finally, many of our participants reported that it was too soon to tell if their perceptions of CM+ implementation corresponded with quantitative data about the practice achievements in redesigning care. Future studies should allow ample time for integrating practice change and evaluating success using both qualitative and quantitative approaches.
CONCLUSION
The qualitative results we present are informative for family medicine and pediatric practices wanting to implement a nurse care management program. Results from these “early adopter” practices indicate that practice change is hard, requires time, and is supported by practice reflection and on-going facilitation.
Acknowledgments
The research team thanks the 6 practices that made this intervention a priority in their busy clinical settings. Your visionary dedication to maximizing care delivery inspires us all. The team wishes to acknowledge the guidance and feedback provided by the Task Order Officer, David Lanier, MD, Center for Primary Care, Prevention and Clinical Partnerships, Agency for Health Care Research and Quality.
This project was supported by contract number HHSA2902007100016I (Task Order 5) from the Agency for Healthcare Research and Quality. Additional support from a Clinical and Translational Science Award to Oregon Health & Science University, NIH/NCRR 1UL1 RR02414-01.
Appendix 1. Pre- and Postintervention Semistructured Interview Questions
Preintervention semistructured questions:
What would be the ideal outcome for you and the clinic in participating in this study?
What are the current barriers to effective care, especially for the chronically ill for you and the clinic?
To you, which individuals or organizations are most interested in the success of the project and why? (For example: patients, staff, community-based agencies, administration, payers, purchasers like large employers)
What is your understanding about what the care manager will do?
What are the potential barriers or challenges to adopting the program?
You have indicated you have disease registries in the ORPRN survey. How do you use your disease registries currently?
Postintervention semistructured questions:
Overall, how do you think implementation of the Care Management Plus system worked for the clinic? Your ideal outcomes pre-intervention were identified, how closely were they met?
During the preintervention interviews you identified as potential barriers to implementing this model. Are they still barriers?
What are the current barriers to effective care, especially for the chronically ill for you and the clinic?
Who (personal or organizational position) was most helpful in implementing the Care Management Plus model? Why?
What is the most important lesson you have learned regarding the implementation of the nurse care manager?
Describe any community organizational linkages that you feel occurred as a result of implementing Care Management Plus.
Looking back, with your current knowledge, what would you have done differently?
Going forward, what 3 things do you need to continue to effectively use the practice-based nurse care manager program?
What advice or input would you like to share with the project staff regarding what has worked well and what could be done differently in the implementation of the project?
Footnotes
The authors report no conflicts of interest.
Contributor Information
Lyle J. Fagnan, Oregon Rural Practice-based Research Network, Department of Family Medicine, Oregon Clinical & Translational Science Institute, Portland.
David A. Dorr, Oregon Rural Practice-based Research Network, Department of Medical Informatics & Clinical Epidemiology, Oregon Clinical & Translational Science Institute, Portland.
Melinda Davis, Oregon Rural Practice-based Research Network, Department of Family Medicine, Oregon Clinical & Translational Science Institute, Portland.
Paul McGinnis, Oregon Rural Practice-based Research Network, Oregon Clinical & Translational Science Institute, Portland.
Jo Mahler, Oregon Rural Practice-based Research Network, Oregon Clinical & Translational Science Institute, Portland.
Molly McCarthy King, Oregon Rural Practice-based Research Network, Department of Medical Informatics & Clinical Epidemiology, Oregon Clinical & Translational Science Institute, Portland.
LeAnn Michaels, Oregon Rural Practice-based Research Network, Oregon Clinical & Translational Science Institute, Portland.
REFERENCES
- American Academy of Family Physicians (2009). The Effect of Facilitation in Fostering Practice. Retrieved November 2, 2009, from http://www.transformed.com/pdf/FacilitationFosteringPractice.pdf
- American Academy of Family Physicians, A. A. o. P., American College of Physicians, American Osteopathic Association. Joint principles of the patient-centered medical home (2007). Retrieved May 26, 2008, from www.medicalhomeinfo.org/Joint%20Statement.pdf.
- Bodenheimer T, Chen E, & Bennett HD (2009). Confronting the growing burden of chronic disease: can the U.S. health care workforce do the job? Health Affairs (Millwood), 28(1), 64–74. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wang MC, Rundall TG, Shortell SM, Gillies RR, Oswald N, et al. (2004). What are the facilitators and barriers in physician organizations’ use of care management processes? Joint Commission Journal of Quality Safety, 30(9), 505–514. [DOI] [PubMed] [Google Scholar]
- Casalino L, Gillies RR, Shortell SM, Schmittdiel JA, Bodenheimer T, Robinson JC, et al. (2003). External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA, 289(4), 434–441. [DOI] [PubMed] [Google Scholar]
- Cohen DJ, & Crabtree BF (2008a). Evaluative criteria for qualitative research in health care: controversies and recommendations. Annals of Family Medicine, 6(4), 331–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DJ, & Crabtree BF (2008b). Using Qualitative Methods in Healthcare Research: A Comprehensive Guide for Designing, Writing, Reviewing and Reporting Qualitative Research. Retrieved June 22, 2009, 2008, from http://www.qualres.org/
- Colwill JM, Cultice JM, & Kruse RL (2008). Will generalist physician supply meet demands of an increasing and aging population? Health Affairs (Millwood), 27(3), w232–w241. [DOI] [PubMed] [Google Scholar]
- Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, Stump TE, et al. (2007). Geriatric care management for low-income seniors: a randomized controlled trial. JAMA, 298(22), 2623–2633. [DOI] [PubMed] [Google Scholar]
- Dorr DA, Wilcox A, Burns L, Brunker CP, Narus SP, & Clayton PD (2006). Implementing a multidisease chronic care model in primary care using people and technology. Disease Management, 9(1), 1–15. [DOI] [PubMed] [Google Scholar]
- Dorr DA, Wilcox A, McConnell KJ, Burns L, & Brunker CP (2007). Productivity enhancement for primary care providers using multicondition care management. American Journal of Managed Care, 13(1), 22–28. [PubMed] [Google Scholar]
- Dorr DA, Wilcox AB, Brunker CP, Burdon RE, & Donnelly SM (2008). The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. Journal of the American Geriatrics Society, 56(12), 2195–2202. [DOI] [PubMed] [Google Scholar]
- Fagnan LJ, Morris C, Shipman S, Holub J, King A, & Angier H (2007). Characterizing a practice-based research network: Oregon Rural Practice-Based Research Network (ORPRN) survey tools. Journal of American Board Family Medicine, 20(2), 204–219. [DOI] [PubMed] [Google Scholar]
- Frankel R (1999). Standards of qualitative research (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Gagnon AJ, Schein C, McVey L, & Bergman H (1999). Randomized controlled trial of nurse case management of frail older people. Journal of the American Geriatrics Society, 47(9), 1118–1124. [DOI] [PubMed] [Google Scholar]
- Glaser B, & Strauss A (1967). The discovery of grounded theory. New York: Aldine. [Google Scholar]
- Hing E, & Burt CW (2008). Characteristics of office-based physicians and their medical practices: United States, 2005–2006. Vital Health Statistics, 13(166), 1–34. [PubMed] [Google Scholar]
- Hroscikoski MC, Solberg LI, Sperl-Hillen JM, Harper PG, McGrail MP, & Crabtree BF (2006). Challenges of change: a qualitative study of chronic care model implementation. Annals of Family Medicine, 4(4), 317–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (1994). Defining primary care: An interim report. Washington DC: National Academy Press. [Google Scholar]
- Liebhaber A, & Grossman JM (2007). Physicians moving to mid-sized, single-specialty practices. Track Reports, 18, 1–5. [PubMed] [Google Scholar]
- McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. (2007). Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies: Volume 7-Care Coordination In AHRQ (Eds.) (Vol. 7), Retrieval January 24, 2010, from http:www.ahrq.gov/clinic/tp/caregaptp.htm [PubMed] [Google Scholar]
- Miller WL, & Crabtree BF (1999). The dance of interpretation (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- National Quality Forum (2009). National Quality Forum launches project to increase patient safety and decrease waste by improving coordination of healthcare. Retrieved 11 January 2009, from http://input.qualityforum.org/news/releases/Care%20Coordination.pdf
- Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, & Stange KC (2009). Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Annals of Family Medicine, 7(3), 254–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley AS, Tynan A, Cohen GR, Kemper N, & Davis MM (2009). Coordination of care by primary care practices: strategies, lessons and implications. Research Briefs, 12, 1–16. [PubMed] [Google Scholar]
- Pham HH, O’Malley AS, Bach PB, Saiontz-Martinez C, & Schrag D (2009). Primary care physicians’ links to other physicians through Medicare patients: the scope of care coordination. Annals of Internal Medicine, 150(4), 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoen C, Osborn R, Doty MM, Bishop M, Peugh J, & Murukutla N (2007). Toward higher-performance health systems: adults’ health care experiences in seven countries, 2007. Health Affairs (Millwood), 26(6), w717–w734. [DOI] [PubMed] [Google Scholar]
- Sledge WH, Brown KE, Levine JM, Fiellin DA, Chawarski M, White WD, et al. (2006). A randomized trial of primary intensive care to reduce hospital admissions in patients with high utilization of inpatient services. Disease Management, 9(6), 328–338. [DOI] [PubMed] [Google Scholar]
- Smith PC, Araya-Guerra R, Bublitz C, Parnes B, Dickinson LM, Van Vorst R, et al. (2005). Missing clinical information during primary care visits. JAMA, 293(5), 565–571. [DOI] [PubMed] [Google Scholar]
- Solberg LI (2007). Improving medical practice: a conceptual framework. Annals of Family Medicine, 5(3), 251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss A, & Corbin J (1998). Basics of qualitative research: Techniques and procedures for developing grounded theory (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Wise PH (2007). The future pediatrician: the challenge of chronic illness. Journal of Pediatrics, 151 (Suppl. 5), S6–S10. [DOI] [PubMed] [Google Scholar]
- Wolfson D, Bernabeo E, Leas B, Sofaer S, Pawlson G, & Pillittere D (2009). Quality improvement in small office settings: an examination of successful practices. BMC Family Practices, 10, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]


