COVID-19 has shined a spotlight on the inequities inherent to our healthcare systems worldwide [[1], [2], [3]]. Disparities can occur at each step of the clinical care continuum in the pandemic response, from public health messaging, social distancing, diagnostic testing, to the delivery of healthcare in the outpatient and inpatient settings, including at the end of life.
In the United States, data from New York City, Boston, and Los Angeles have shown that the Hispanic/Latinx community, of whom many are limited English proficient (LEP), account for a disproportionately large percentage of COVID-19 hospitalizations and deaths [2]. Several lay press accounts highlight the likely contribution of language barriers to these disparities [4]. We need to respond to the unique needs of LEP individuals and families during the pandemic, particularly given that our response to the SARS-COV2 virus will likely persist several months, perhaps years, beyond the acute flattening of the curve.
Eight percent of the US population is LEP, defined as speaking English less than very well [5]. We know from years of research that patients with LEP experience disparities in timely receipt of public health messaging, understanding of important health information, and access to insurance and health care [6]. We know that patients with LEP often experience poor patient-clinician communication and worse health outcomes [7]. The good news is that we also know how to overcome health care disparities due to language and how to provide equitable care to LEP populations, lessons we should apply during the COVID-19 pandemic.
First, we need to make sure predominantly LEP communities have equitable access to linguistically and culturally tailored information about COVID-19: the symptoms, testing and how to take care of themselves and their families if they need to quarantine or self-isolate.
Second, public health measures should take into account the unique social and economic stressors communities with large LEP populations frequently face. LEP communities usually have sizeable numbers of individuals who cannot afford to take time off work and/or do not have the ability to self-isolate given multi-family living conditions [7]. These communities need monetary and housing resources to shelter in place.
Third, access to COVID-19 testing must be equitable. Obviously, there needs to be information available about testing – who should be tested and how to get tested – that it is free through public health channels and available in languages other than English. This testing should be available in areas with large LEP communities and accessible through public transportation or other means, as disparities in access to transportation are higher for these populations [8].
Fourth, in the outpatient setting, COVID-19 infected LEP individuals require information about the disease and necessary clinical care in a language they can understand. This can occur either via clinicians fully fluent in the patient’s preferred language or professional interpreter services, provided in-person or remotely. When available, language-concordant physicians are preferred because they provide better care for LEP patients in many circumstances compared to professional medical interpreters, which results in better outcomes [9]. Clinicians’ language skills should be evaluated using known validated tests [10]. The recent quick pivot to telehealth visits, with physicians and interpreters often working from home, has upended usual systems for accessing professional interpreters. Health care organizations should instruct clinicians on how to use existing interpreter services during telehealth visits to bridge the language barrier, whether it is by videoconference or telephone. In ongoing work in the outpatient setting, we have found that patients rate interpretation over video to be higher quality than over the telephone.
Fifth, in the inpatient setting, we need to overcome the unique challenges of communicating with LEP patients during the pandemic. In emergency departments and hospitals, available staffing, including interpreters, is minimized. Clinicians are necessarily reducing the time they spend in patient rooms to reduce risk and personal protective equipment use. Loud background noise from makeshift negative pressure machines, the muffling of voices under masks, and challenges in accessing necessary equipment to engage remote interpreters, all exacerbate language barriers. Clinicians are overwhelmed and stressed, and understandably tempted to “get by” using non-fluent language skills or smart phone translation applications [9,11]. However, we know that physicians use of their non-fluent skills or these apps can lead to errors with the potential for significant harm [9,11]. The importance of proper communication is even more critical during end of life conversations, particularly for those who are without visitors and isolated from their families and communities.
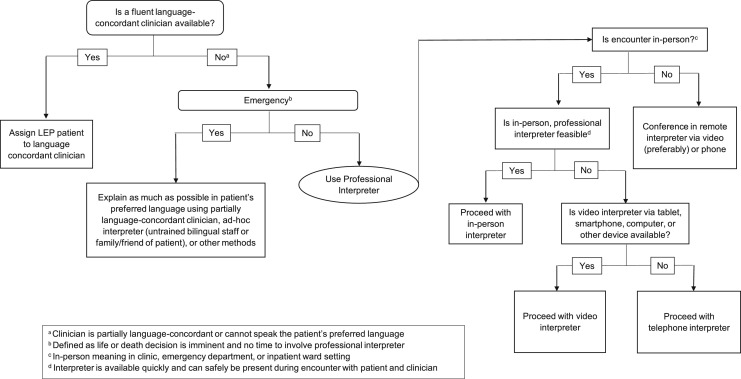
As in the outpatient setting, inpatient care for LEP patients is ideally provided by a fluent language-concordant clinician. If not available, professional interpreters should be used. The use of clinicians’ phones to access professional interpreters is less ideal in the pandemic due to the need to keep clinicians’ equipment free from contamination. Video interpreters are our first-line recommendation. Hospitals may have access to video interpreters that feature their own staff or a contract agency. The interface may be an in-room television, patient assigned tablets, or patient personal smartphones. In the absence of video interpreters, telephone interpreters should be used.
Fig. 1 shows an algorithmic approach to overcoming language barriers for LEP patients and provides recommendations that reflect the realities of delivering care under current difficult circumstances. In summary, best practices for providing equitable care to LEP communities during the COVID-19 pandemic – access to information in a patient’s preferred language, fluent language concordant clinicians, and professional interpreters – remain the same as in the days before SARS-COV-2. We acknowledge that these best practices may not always be practical given the strain COVID-19 conditions have placed on our health care systems and providers.
Fig. 1.
An Algorithm to Overcome Language Barriers for Limited English Proficient Patients.
While we – who have the benefit of speaking the dominant language – strive for equity because it is our moral obligation, it is also to our pragmatic collective benefit. Regardless of preferred language, our individual health during this pandemic is tied to that of our neighbor, whether they be in the same neighborhood, city, state, or nation. Addressing disparities will help contain the spread of COVID-19 within our nations. Clear communication is a powerful tool in the fight against COVID-19. Let’s make sure everyone has access to it.
Acknowledgements
Dr. Diamond was supported by Memorial Sloan Kettering Cancer Center Support Grant/Core Grant (P30 CA008748), and NCI K07 CA184037.
References
- 1.Bibbins-Domingo K. This time must be different: disparities during the COVID-19 pandemic. Ann. Intern. Med. 2020 doi: 10.7326/M20-2247. [Epub ahead of print 28 April 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Essien U.R., Venkataramani A. JAMA Health Forum; 2020. Data and Policy Solutions to Address Racial and Ethnic Disparities in the COVID-19 Pandemic.https://jamanetwork.com/channels/health-forum/fullarticle/2765498 April 28. [DOI] [PubMed] [Google Scholar]
- 3.UN News; 2020. “COVID-19 Pandemic Exposes Global ‘frailties and Inequalities’: UN Deputy Chief.”.https://news.U.N.org/en/story/2020/05/1063022 May 2. [Google Scholar]
- 4.Goldberg E. New York Times; 2020. When Coronavirus Care Gets Lost in Translation.https://www.nytimes.com/2020/04/17/health/covid-coronavirus-medical-translators.html#click=https://t.co/GKeBeNA5XQ April 17. [Google Scholar]
- 5.Zong J., Batalova J. Migration Policy Institute; 2015. The Limited English Proficient Population in the United States.http://www.migrationpolicy.org/article/limited-english-proficient-population-united-states July 8. [Google Scholar]
- 6.Karliner L.S., Jacobs E.A., Chen A.H., Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv. Res. 2007;42(April (2)):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Premji S., Krause N. Disparities by ethnicity, language, and immigrant status in occupational health experiences among Las Vegas hotel room cleaners. Am. J. Ind. Med. 2010;53:960–975. doi: 10.1002/ajim.20860. [DOI] [PubMed] [Google Scholar]
- 8.Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J. Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diamond L.C., Izquierdo K., Canfield D., Matsoukas K., Gany F. A systematic review of the impact of patient-physician non-english language concordance on quality of care and outcomes. J. Gen. Intern. Med. 2019;34(August (8)):1591–1606. doi: 10.1007/s11606-019-04847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diamond L.C., Chung S., Ferguson W., Gonzalez J., Jacobs E., Gany F. Relationship between self-assessed and tested non-english language proficiency among primary care providers. Med. Care. 2014;52(5):435–438. doi: 10.1097/MLR.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khoong E.C., Steinbrook E., Brown C., Fernandez A. Assessing the use of google translate for Spanish and Chinese translations of emergency department discharge instructions. JAMA Intern. Med. 2019;179(4):580–582. doi: 10.1001/jamainternmed.2018.7653. [DOI] [PMC free article] [PubMed] [Google Scholar]