Abstract
Background
Changes in acetabular or hip center of rotation (HCOR) commonly occur during acetabular component preparation during total hip arthroplasty (THA). HCOR displacement in mediolateral or superoinferior directions is known to influence offset and leg length, but the incidence and range of HCOR change in the anteroposterior direction is less understood as the sagittal plane cannot be measured on standard anteroposterior radiographs. This study assessed the 3-dimensional displacement of HCOR after cup implantation and evaluated for potential factors associated with increased acetabular component translations.
Methods
A total of 894 THAs were performed using a posterior, lateral, or direct anterior approach. Only intraoperative data from the navigation device were included in the analysis. All THAs performed between September 2015 and October 2017 were included. Paired t-tests were used to compare native HCOR and new HCOR values.
Results
The mean HCOR displacement in 3 directions was 4.97mm medially (P < .001), 0.83mm superiorly (P < .001), and 0.64mm posteriorly (P < .001). Subgroup analysis revealed greater posterior HCOR displacement with the anterior approach than the lateral/posterior approach (2.32mm vs 0.44mm; P < .001). Increasing medial HCOR displacement also resulted in increased superior and posterior HCOR displacement across surgical cases (P < .001).
Conclusions
HCOR displacement is commonly observed in medial, superior, and posterior directions. HCOR changes are influenced by surgical approach, potentially secondary to patient positioning, with greater posterior HCOR displacement observed in anterior cases. Surgeons should be aware of these factors, particularly in cases with deficient or reduced posterior column bone stock.
Keywords: Hip center of rotation, New hip center, Total hip arthroplasty, Direct anterior THA, Computer-assisted navigation
Introduction
Reaming and placement of the acetabular component during total hip arthroplasty (THA) often results in a displacement of the native hip center of rotation (HCOR) [1]. Significant mediolateral (M-L) or superoinferior (S-I) HCOR displacement may lead to several deleterious postoperative outcomes, including leg length discrepancy (LLD), abnormal gait patterns, accelerated bearing surface wear, component loosening, and dislocation [[2], [3], [4]]. However, HCOR displacements in the anteroposterior (A-P) direction are poorly characterized, as this direction of displacement cannot be measured on standard A-P radiographs.
Prior publication on changes in HCOR has emphasized that medialization of the acetabular component, with restoration of cumulative offset, optimizes hip biomechanics as the abductor moment arm increases, while joint reaction force decreases with a concomitant reduction in the risk of premature wear [3,[5], [6], [7], [8], [9], [10], [11], [12]]. However, excessive medial HCOR displacement that is not restored on the femoral side leads to a reduction of global offset, which may negatively affect hip biomechanics, reduce range of motion until osseous impingement, and increase the risk of dislocation [[2], [3], [4],8]. Conversely, significant lateral HCOR displacement decreases the lever arm strength of the abductor muscle and may contribute to implant loosening because of inadequate bony support [3,9]. Several studies have investigated the optimal HCOR in the M-L direction, but currently, there is no consensus, and it may be important to consider the patient anatomy when establishing ideal HCOR in the M-L direction [1,4,8,13].
Significant HCOR change in the S-I direction influences overall leg length and can lead to unexpected LLD [7], a common reason for dissatisfaction after THA and the leading cause of litigation against orthopaedic surgeons [14]. Discrepancies as small as 5 mm can be perceived by most patients [15,16] and can compromise gait and joint stability [7,17]. Significant superior HCOR displacement can also reduce abductor strength and increase the risk of implant loosening and premature wear, particularly in the setting of a cemented acetabular component with conventional polyethylene [3,5,7,9,18].
Interestingly, little is known regarding changes in HCOR displacement in the sagittal plane, and the impact of A-P displacement on clinical outcomes and complications has not been reported. Quantifying changes in the sagittal plane before and after acetabular component insertion is challenging, as this displacement cannot be measured on standardized postoperative A-P radiographs [4]. Specifically, the 2-dimensional nature of the A-P radiograph prevents visualization of HCOR A-P displacement. However, biomechanical simulations have demonstrated an altered moment arm and decreased power-generating capacity of the extensors and flexors resulting from HCOR A-P displacement [5,19]. In addition, anterior HCOR displacement may contribute to minimized hip loads [5,19]. Despite the potential biomechanical and clinical consequences of HCOR A-P displacement, quantitative assessment of HCOR A-P alteration after surgical intervention has not been previously reported.
The primary aim of the present study was to calculate the average 3-dimensional (3D) change in HCOR (in M-L, S-I, and A-P directions) before and after acetabular component implantation in navigated THA cases. The second aim of the study was to assess whether changes in HCOR were dependent on the surgical approach.
Material and methods
A multicenter retrospective review of 894 computer-assisted THAs was performed. All THAs were performed using the same 3D computer-assisted navigation system (Intellijoint Surgical, Inc., Kitchener, ON, Canada), and intraoperative HCOR measurements were recorded for all cases. All THAs performed via the posterior, lateral, or direct anterior surgical approaches between September 2015 and October 2017 were included. For this study, only deidentified intraoperative data from the device were collected and analyzed. No demographic or patient data were included in the current analysis; therefore, this study was exempt from review by institutional review boards at the hospital sites and did not require explicit patient consent. Surgical cases were excluded from analysis if preoperative or postoperative HCOR values were not recorded by the navigation device during surgery. All data received were deidentified and stored locally in accordance with HIPAA guidelines.
Computer-assisted navigation
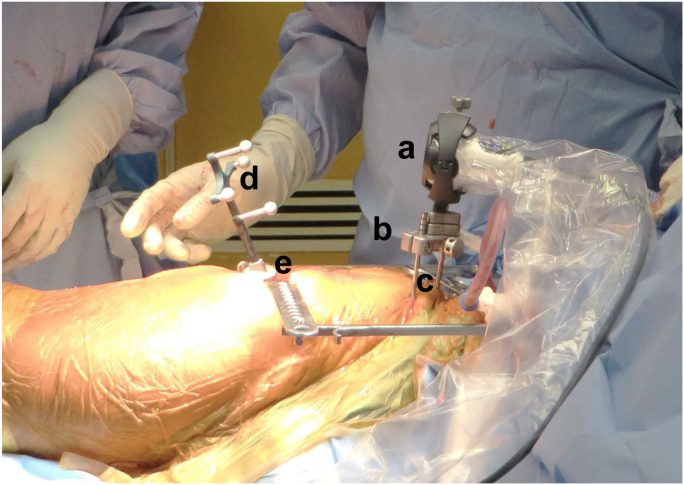
The Intellijoint HIP navigation system (Intellijoint HIP; Intellijoint Surgical, Inc., Kitchener, ON, Canada) consists of a camera, probe, and tracker located within the sterile field and a workstation monitor located outside of the sterile field (Fig. 1). Detailed explanations of the navigation device for lateral, posterior, and direct anterior approaches have been previously described [20,21]. The navigation tool measures kinematic HCOR, where the native HCOR is recorded by placing the tracker on the femoral platform, located on the operative greater trochanter, and articulating the leg to capture a wide range of angular motion with the camera. The system plots the position of the tracker on the surface of a sphere that rotates about an axis, where the center of the sphere represents hip center (Fig. 2). For new HCOR, the same process is repeated with the tracker atop the impactor attached to a liner impactor ball. Internal evaluation and validation have shown this navigation device is able to accurately measure displacements in HCOR placement within 0.4 mm ± 0.4 mm.
Figure 1.
The camera (a), enclosed in a sterile drape, attaches to the pelvic platform (b) via 2 pelvic screws (c). The tracker (d) is magnetically attached to the femoral platform (e). The camera captures movements of the tracker and relays the information to a workstation for review by the surgeon.
Figure 2.

For kinematic hip center measurements, the tracker of the navigation tool is attached to the operative leg and articulated to capture a wide range of angular motion with the camera (a). The system plots the position of the tracker on the surface of a sphere that rotates about an axis, where the center of the sphere represents the hip center (b). Any displacement in M-L, S-I, and A-P directions is recorded by the navigation device. A-P, anteroposterior; M-L, mediolateral; S-I, superoinferior.
Outcome variables
Native HCOR and new HCOR measurements after cup and liner implantation were recorded in M-L, S-I, and A-P directions. To observe trends in HCOR movement, the difference between native HCOR and new HCOR was calculated for each case and defined as the HCOR displacement (Fig. 3). The mean HCOR displacement was calculated for M-L, S-I, and A-P directions. A proportion analysis was conducted to identify surgical cases with reported HCOR displacements >3 mm and >5 mm in each direction. The absolute values of HCOR displacements were recorded to identify surgical cases with combined HCOR displacements >3 mm and >5 mm, where combined HCOR displacement was defined as >3 mm or >5 mm HCOR displacement in M-L, S-I, and A-P directions collectively. A subgroup analysis of the cohort was conducted to evaluate HCOR displacement stratified by the surgical approach. Specifically, device data obtained from surgeries performed via the direct anterior approach were compared with data from surgeries performed via the posterior and lateral surgical approaches [20,21]. The latter were grouped together in the final analysis, as the vast majority of cases were performed via the posterior approach, so much so that a subgroup analysis comparing posterior and lateral approach results would not be statistically meaningful. All surgeons performing direct anterior THA in the present study were trained and had completed their respective learning curves associated with direct anterior THA before data collection for this study [22]. A second subgroup analysis of the cohort was conducted to examine HCOR A-P and S-I displacements stratified by medial HCOR displacement. Surgical cases demonstrating a medial HCOR displacement were grouped with the following displacement increments: 0-2 mm, 2-4mm, 4-6 mm, 6-8 mm, 8-10 mm, and >10 mm. HCOR A-P and S-I displacements were then observed across subgroups.
Figure 3.
Directions of HCOR displacement. HCOR, hip center of rotation.
Statistical analysis
This retrospective study was observational in design, and statistical comparisons were made with alpha set a priori at 0.05. Paired t tests were used to compare native HCOR and new HCOR values across surgical cases and to evaluate HCOR displacement stratified by surgical approach. Pearson’s r, one-way ANOVA, and Student t-tests were used to compare HCOR A-P and S-I displacements relative to medial HCOR displacement. All results are presented as mean (standard deviation).
Results
HCOR displacement
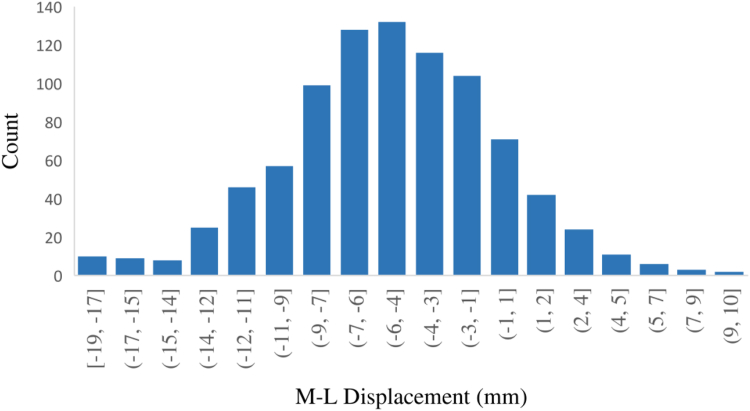
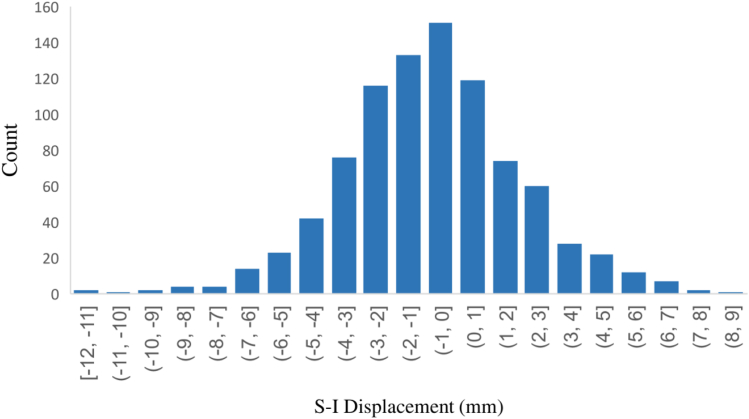
In total, 894 cases were included in the analysis. In the M-L direction, HCOR was displaced medially by a mean of 4.97 mm ± 4.53 mm (P < .001). The distribution of M-L displacement is depicted in Figure 4. In the S-I direction, HCOR was displaced by a mean of 0.83 mm ± 2.76 mm superiorly (P < .001), whereas in the A-P direction, a mean of 0.64 mm ± 2.76 mm of posterior movement (P < .001) was observed (Figure 5, Figure 6, respectively).
Figure 4.
The distribution of HCOR displacement in the M-L direction, across 894 cases of THA performed between September 2015 and October 2017. HCOR, hip center of rotation; M-L, mediolateral; THA, total hip arthroplasty.
Figure 5.
Distribution of HCOR displacement in the S-I direction pooled from 894 cases of THA performed between September 2015 and October 2017. HCOR, hip center of rotation; S-I, superoinferior; THA, total hip arthroplasty.
Figure 6.
The distribution of HCOR displacement in the A-P direction, across 894 cases of THA performed between September 2015 and October 2017. A-P, anteroposterior; HCOR, hip center of rotation; THA, total hip arthroplasty.
Proportion analysis
Medial displacement of HCOR was >3 mm in 605 of 894 (67.7%) cases and >5 mm in 438 of 894 (49.0%) hips. HCOR was lateralized >3 mm and >5 mm in only 34 of 894 (3.8%) and 14 of 894 (1.6%) hips, respectively. Overall, 81 of 894 (9.1%) surgical cases demonstrated a combined HCOR displacement of >3 mm, and 10 of 894 (1.1%) surgical cases demonstrated a combined HCOR displacement of >5 mm. Proportional analysis data are summarized in Table 1.
Table 1.
Proportional analysis summary of HCOR displacement according to the anatomic direction.
| HCOR |
HCOR direction |
|||||
|---|---|---|---|---|---|---|
| Displacement | Superior |
Inferior |
Medial |
Lateral |
Anterior |
Posterior |
| Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | |
| >3 mm | 175 (19.6) | 71 (7.9) | 605 (67.7) | 34 (3.8) | 68 (7.6) | 156 (17.4) |
| >5 mm | 52 (5.8) | 21 (2.4) | 438 (49.0) | 14 (1.6) | 24 (2.7) | 53 (5.9) |
HCOR, hip center of rotation.
Subgroup analysis for surgical approach
In total, 797 cases were performed using the posterior or lateral surgical approach, whereas 97 cases were performed via the direct anterior approach. In the anterior cohort, significant mean HCOR displacements of 4.44 mm ± 5.22 mm and 2.32 mm ± 3.67 mm were observed in the medial and posterior directions, respectively (P < .001). Superior displacement of 0.57 mm ± 4.14 mm was observed in the S-I direction (P = .18). In the lateral/posterior THA cohort, HCOR displacements of 5.03 ± 4.44 mm medially and 0.44 mm ± 2.56 mm posteriorly (P < .001) were observed, with 0.86 mm ± 2.54 mm of superior displacement noted in the S-I direction (P < .001). A statistical significance was observed between surgical approaches for HCOR A-P displacement, where anterior cases exhibited significantly greater posterior HCOR displacement than lateral/ posterior cases (2.32 mm vs 0.44 mm, P < .001). No statistical differences were observed between surgical approaches for HCOR S-I displacement (P = .49) or M-L displacement (P = .29). HCOR displacement data stratified by anterior THA and lateral/posterior THA are summarized in Table 2, Table 3, respectively.
Table 2.
HCOR displacement summary for THA cases performed with the anterior approach.
| Measurement | Superior-inferior direction | Medial-lateral direction | Anterior-posterior direction |
|---|---|---|---|
| Mean (mm) | 0.57 | 4.44 | 2.32 |
| SD (mm) | 4.14 | 5.22 | 3.67 |
| Direction | Superior | Medial | Posterior |
| Rangea (mm) | −12.0 to 8.4 | −8.8 to 17.7 | −11.8 to 4.0 |
| P-value | .18 | <.001 | <.001 |
HCOR, hip center of rotation; THA, total hip arthroplasty; SD, standard deviation. Bold values indictate statistical significance (P < .05).
Negative values indicate displacement in the inferior, lateral, or posterior direction.
Table 3.
HCOR displacement summary for THA cases performed with the lateral approach.
| Measurement | Superior-inferior direction | Medial-lateral direction | Anterior-posterior direction |
|---|---|---|---|
| Mean (mm) | 0.86 | 5.03 | 0.44 |
| SD (mm) | 2.54 | 4.44 | 2.56 |
| Direction | Superior | Medial | Posterior |
| Range (mm)a | −8.2 to 6.7 | −7.4 to 18.5 | −8.0 to 7.0 |
| P-value | <.001 | <.001 | <.001 |
HCOR, hip center of rotation; THA, total hip arthroplasty; SD, standard deviation.
Bold values indictate statistical significance (P < .05).
Negative values indicate displacement in the inferior, lateral, or posterior direction.
Subgroup analysis for medial HCOR displacement
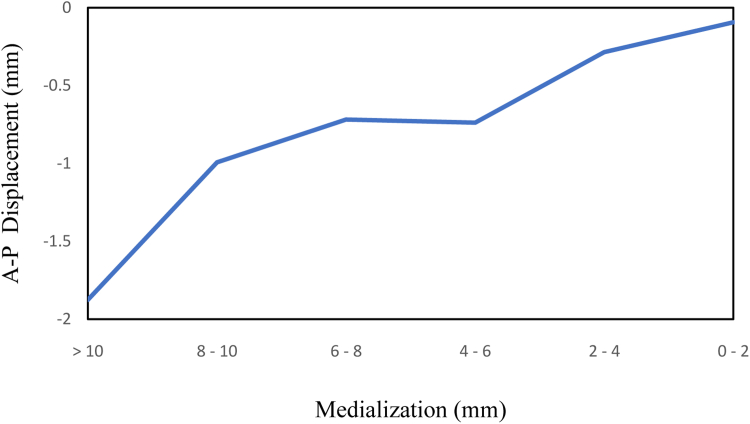
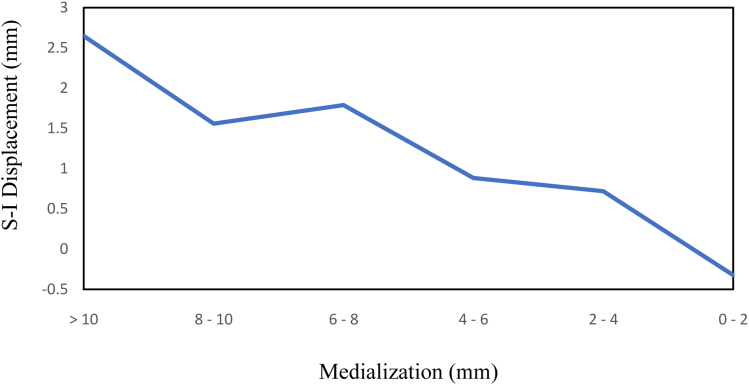
Overall, an increase in posterior HCOR displacement, ranging from 0.09 mm to 1.88 mm, was observed with incremental increases in medial HCOR displacement (Table 4; r = 0.20). A similar increase in superior displacement was observed, ranging from 0.32 mm of inferior displacement in the lowest medial displacement subgroup to 2.65 mm of superior displacement in the largest medial displacement subgroup (Table 5, r = 0.34). The relationship between increasing medial HCOR displacement and A-P and S-I HCOR displacement is depicted in Figure 7, Figure 8, respectively. One-way ANOVA demonstrated a significant difference in HCOR A-P and S-I displacements between subgroups (P < .001). Detailed comparisons of HCOR A-P and S-I subgroups are summarized in Table 6, Table 7, respectively.
Table 4.
Trends in postoperative A-P displacement when categorized by increasing medial displacement.
| Medialization | A-P displacement |
|||
|---|---|---|---|---|
| Mean (mm) | SD (mm) | Direction | Count | |
| 0-2 mm | 0.09 | 2.46 | Posterior | 110 |
| 2-4 mm | 0.28 | 2.54 | Posterior | 146 |
| 4-6 mm | 0.73 | 2.58 | Posterior | 170 |
| 6-8 mm | 0.72 | 2.55 | Posterior | 153 |
| 8-10 mm | 0.99 | 3.24 | Posterior | 82 |
| >10 mm | 1.88 | 3.06 | Posterior | 119 |
A-P, anteroposterior.
Table 5.
Trends in postoperative S-I displacement when categorized by increasing medial displacement.
| Medialization | S-I displacement |
|||
|---|---|---|---|---|
| Mean (mm) | SD (mm) | Direction | Count | |
| 0-2 mm | 0.32 | 1.98 | Inferior | 110 |
| 2-4 mm | 0.72 | 2.39 | Superior | 146 |
| 4-6 mm | 0.88 | 2.19 | Superior | 170 |
| 6-8 mm | 1.79 | 2.37 | Superior | 153 |
| 8-10 mm | 1.56 | 2.44 | Superior | 82 |
| >10 mm | 2.65 | 3.25 | Superior | 119 |
S-I, superoinferior.
Figure 7.
Increased postoperative medial displacement is weakly associated with postoperative posterior displacement (r = 0.20). A-P, anteroposterior.
Figure 8.
Increased postoperative medial displacement is weakly associated with postoperative superior displacement (r = 0.34). S-I, superoinferior.
Table 6.
Summarized P-values for comparison of A-P displacements when categorized by increasing medial displacement.
| Medialization | 0-2 mm | 2-4 mm | 4-6 mm | 6-8 mm | 8-10 mm | >10 mm |
|---|---|---|---|---|---|---|
| 0-2 mm | 0.54 | 0.04 | 0.04 | 0.03 | <0.001 | |
| 2-4 mm | 0.54 | 0.12 | 0.14 | 0.07 | <0.001 | |
| 4-6 mm | 0.04 | 0.12 | 0.95 | 0.50 | <0.001 | |
| 6-8 mm | 0.04 | 0.14 | 0.95 | 0.47 | <0.001 | |
| 8-10 mm | 0.03 | 0.07 | 0.50 | 0.47 | 0.05 | |
| >10 mm | <0.001 | <0.001 | <0.001 | <0.001 | 0.05 |
A-P, anteroposterior.
Bold values indictate statistical significance (P < .05).
Table 7.
Summarized P-values for comparison of S-I displacements when categorized by increasing medial displacement.
| Medialization | 0-2 mm | 2-4 mm | 4-6 mm | 6-8 mm | 8-10 mm | >10 mm |
|---|---|---|---|---|---|---|
| 0-2 mm | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| 2-4 mm | <0.001 | 0.52 | <0.001 | 0.01 | <0.001 | |
| 4-6 mm | <0.001 | 0.52 | <0.001 | 0.03 | <0.001 | |
| 6-8 mm | <0.001 | <0.001 | <0.001 | 0.48 | 0.01 | |
| 8-10 mm | <0.001 | 0.01 | 0.03 | 0.48 | 0.01 | |
| >10 mm | <0.001 | <0.001 | <0.001 | 0.01 | 0.01 |
S-I, superoinferior.
Bold values indictate statistical significance (P < .05).
Discussion
HCOR is an important contributor to the restoration of hip biomechanics and to establishing stability and survivability of the prosthetic hip joint after THA. Clinical studies investigating postoperative changes in HCOR vary in terms of proposed optimal displacement, and little is known regarding HCOR A-P displacement in particular. This study observed mean changes in HCOR of 4.97 mm of medial displacement, 0.83 mm of superior displacement, and 0.64 mm of posterior displacement after THA. Surgical approach influenced HCOR displacement, with the direct anterior approach associated with increased posterior HCOR compared with the lateral/posterior approach. In addition, there was a weak linear relationship between the amount of medial HCOR displacement and posterior and superior HCOR displacement. This not only suggests changes in HCOR are influenced by surgical approach but intraoperative processes such as amount of medial reaming could also lead to associated patterns in collective HCOR displacement in the medial, superior, and posterior directions.
Medial HCOR displacement is commonly observed, as adequate peripheral bony support is required to properly seat the acetabular component and reduce the likelihood of loosening [3,9]. Although medial HCOR displacement is generally associated with increased hip function, improved implant survivorship, and decreased risk of premature wear, excessive medialization results in medial bone loss and the risk of a reduction in global offset if not adequately restored on the femoral side [[2], [3], [4],6,8]. Reduction of global acetabular offset has been associated with an increased risk of postoperative dislocation [23]. Previous studies have suggested that the optimal HCOR M-L displacement range is between ±5 mm and ±7.5 mm, to maintain global offset values, decrease the risk of dislocation, and reduce wear of the implant [1,4,13]. Interestingly, the amount of medial displacement may be more extreme in cases of severe anatomic deformity, that is, hip dysplasia, where upward of 30 mm of medial HCOR displacement has been reported to achieve adequate bony coverage [24,25]. The results of our study mirror those of other studies and recommendations [2,3,6], with a mean of 4.97 mm ± 4.5 mm of medial HCOR displacement observed.
HCOR S-I displacement influences postoperative offset and leg length [1,3,7]. Significant superior HCOR displacement in particular may lead to negative postoperative outcomes such as reduced abductor strength, implant loosening, and risk of premature wear [3,5,7,9,18]. In contrast, moderate inferior displacement can increase abductor strength and joint stability and reduce the risk of premature wear [5,6,9]. However, optimal HCOR S-I displacement is controversial. Jolles et al [26] suggest an inferior HCOR displacement <2 mm to decrease the risk of dislocation. Our study, however, demonstrated a mean superior HCOR displacement of 0.83 mm ± 2.76 mm, consistent with prior studies. In particular, Dastane et al [1] suggested a HCOR S-I displacement threshold of ±3 mm, whereas Bjarnason et al [3] suggested ±5 mm, to maintain global offset and promote joint survivorship. In the present study, a proportion analysis revealed that only 1 in 5 cases (20%) demonstrated superior HCOR displacement >3 mm, suggesting a ±3 mm threshold may not be consistently achievable. Consequently, surgeons should take care in avoiding this potential suboptimal positioning, which has adverse mechanical consequences. However, it is important to note that parameters such as global offset and leg length are heavily influenced by implant selection. While HCOR S-I displacement is likely a result of the reaming process [2,27], undesirable HCOR S-I displacement may be corrected during the trialing phase of surgery. Based on these findings, surgeons who rely solely on restoration of femoral length and do not incorporate the S-I change in acetabular position may be unintentionally increasing LLD in nearly 20% of patients.
Clinical studies regarding HCOR displacement in the A-P direction are scarce. Although biomechanical models have demonstrated the potential for anterior HCOR displacement to minimize hip loads and posterior HCOR displacement to reduce power generation of the hip flexors and extensors [5,19], such outcomes have yet to be established in a clinical setting. One limitation may be that HCOR A-P position is impossible to assess on plain A-P radiographs, which are 2-dimensional. Indeed, while several clinical studies have used A-P radiographs to examine outcomes resulting from HCOR changes in M-L and S-I directions, movement in the A-P direction was excluded from each analysis [2,3,6]. However, a report by Sariali et al [4] in which computed tomography scans were used to characterize 3D patterns in the hip center for patients who experienced dislocation after anterior THA, described a posterior HCOR displacement of 5 mm in the dislocation group compared with the preoperative HCOR. The mechanism for how posterior HCOR displacement may increase the risk of postoperative dislocation is currently not understood but could be related to decreased lateral compartment muscle forces and possibly alterations in the contact zone between the femoral head and acetabular component during activities of daily living. In the present study, 3D computer-assisted navigation revealed a mean posterior HCOR displacement of 0.64 mm ± 2.76 mm, with 5.9% of study hips demonstrating posterior displacement >5 mm. Interestingly, when stratified by the surgical approach, the anterior cohort showed 1.88 mm more posterior HCOR displacement than the mean for lateral and posterior cases (P < .001). These findings suggest that surgical approach influences HCOR displacement in the A-P direction. However, further clinical analysis is required to better understand the significance of these results.
Medial HCOR displacement is commonly reported, and we investigated if an increase in medial HCOR displacement also results in increased A-P and S-I displacement. Medial HCOR displacement was weakly correlated with posterior HCOR displacement (r = 0.20) and superior HCOR displacement (r = 0.34). Cases with >10 mm medial HCOR displacement had significantly more posterior and superior displacement (P < .001). As these directional displacements match with the overall mean displacements observed in this report, the reaming process may be accountable for this relationship; however, this has yet to be examined directly [2,27].
From a clinical perspective, this study is among the first to address how the THA surgical approach impacts HCOR displacement. Although studies have shown preoperative and postoperative changes in HCOR have an impact on joint functionality, the relationship of how HCOR relates to patient biomechanics is not fully defined. Therefore, it is challenging to confidently assess how some of subtle changes in displacement affect clinical outcomes. However, we did observe HCOR displacement depends on the surgical approach. Finding the association between approach and HCOR merits further investigations into if and how this relationship impacts component survivability, joint functionality, and clinical outcomes. Better understanding of how each direction of HCOR displacement is affected by the approach and the clinical impact it may have may help inform decision-making when developing a patient’s preoperative treatment plan, with different approaches being opted for based on native patient anatomy.
This study has limitations. The retrospective and observational study design prevented capture of potentially relevant data points including patient demographics, diagnosis, surgical details, and outcomes. In addition, the lack of a control group limits the strength of the conclusions. Given that all patients in this study underwent navigated THA, there is the possibility the data collected are not reflective of data from non-navigated THA procedures; however, there is no apparent reason why the data collected would differ based on the use of navigation. The device provides no real-time data on reaming depth or direction, so any changes to HCOR are entirely a result of surgeon technique and are independent of the navigation device. Regardless, the goal of this study was to specifically characterize trends in HCOR displacement across a large study population. The present report included a considerable sample size of 894 cases and is one of the first studies to evaluate HCOR A-P displacement. In addition, the subgroup analysis for surgical approach was limited by the disparity in sample size between lateral/posterior and direct anterior cases because of lower utilization by anterior approach surgeons at the time of data collection. However, this observation corresponds with a report by Chechik et al [28] that indicates the direct anterior approach is less used in the United States, and the authors could not control for this retrospectively. Intraoperative device HCOR measurements are relative to the patient positioning captured at the time of registration; therefore, any deviations from the true patient position at registration may be reflected when capturing HCOR [29,30]. This is of particular importance with respect to the small yet significant difference in A-P HCOR displacement observed between anterior and lateral/posterior cases. With respect to registration, this imageless navigation device relies on probing specific skeletal landmarks through soft tissue to register anatomic reference planes and patient position. There is some concern that tissue distribution may affect the registration accuracy, which in the context of this study may increase the error associated with measuring HCOR displacement. However, registration error associated with tissue displacement has been dismissed if patient is properly palpated and the navigation device is used as advised [31]. In addition, this device is able to account for intraoperative movement of the pelvis, therefore reducing any error associated with movement during the THA procedure.
Conclusions
This study evaluated the postoperative mean HCOR displacement in 3 dimensions using intraoperative data from a large cohort of computer-assisted THA. The results of this study highlight the ability of computer-assisted navigation to assist with measuring changes in the hip center and provide descriptive information on the mean and range of displacement of HCOR in the A-P direction, which is not quantifiable on A-P radiographs. In addition, the present report highlighted significant differences in HCOR A-P displacement when stratified by the surgical approach, suggesting HCOR may be influenced by patient positioning and reaming technique. Further clinical studies are required to address the clinical outcomes associated with varying 3D HCOR displacements in a large study population.
Conflict of interest
Jeffrey M. Muir and Jessica R. Benson report paid employment and stock or stock options in Intellijoint Surgical. Iain R. Lamb reports employment in Intellijoint Surgical. Peter K. Sculco reports paid consultancy from Intellijoint Surgical. The other author reports no conflict of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2020.04.003.
Appendix A. Supplementary data
References
- 1.Dastane M., Dorr L.D., Tarwala R., Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clin Orthop Relat Res. 2011;469(2):429. doi: 10.1007/s11999-010-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim S.C., Lim Y.W., Kwon S.Y., Jo W.L., Ju S.H., Park C.J. Level of surgical experience is associated with change in hip center of rotation following cementless total hip arthroplasty: a radiographic assessment. PLoS One. 2017;12(5):1. doi: 10.1371/journal.pone.0178300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bjarnason J.A., Reikeras O. Changes of center of rotation and femoral offset in total hip arthroplasty. Ann Transl Med. 2015;3(22):355. doi: 10.3978/j.issn.2305-5839.2015.12.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sariali E., Klouche S., Mamoudy P. Investigation into three dimensional hip anatomy in anterior dislocation after THA. Influence of the position of the hip rotation centre. Clin Biomech. 2012;27(6):562. doi: 10.1016/j.clinbiomech.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 5.Delp S.L., Maloney W. Effects of hip center location on the moment-generating capacity of the muscles. J Biomech. 1993;26(4-5):485. doi: 10.1016/0021-9290(93)90011-3. [DOI] [PubMed] [Google Scholar]
- 6.Tezuka T., Inaba Y., Kobayashi N. Effects of hip joint center location and femoral offset on abductor muscle strength after total hip arthroplasty. Mod Rheumatol. 2015;25(4):630. doi: 10.3109/14397595.2014.988863. [DOI] [PubMed] [Google Scholar]
- 7.Bhaskar D., Rajpura A., Board T. Current concepts in acetabular positioning in total hip arthroplasty. Indian J Orthop. 2017;51(4):386. doi: 10.4103/ortho.IJOrtho_144_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terrier A., Levrero Florencio F., Rüdiger H.A. Benefit of cup medialization in total hip arthroplasty is associated with femoral anatomy. Clin Orthop Relat Res. 2014;472(10):3159. doi: 10.1007/s11999-014-3787-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoder S.A., Brand R.A., Pedersen D.R., O’Gorman T.W. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res. 1988;228:79. [PubMed] [Google Scholar]
- 10.Asayama I., Chamnongkich S., Simpson K.J., Kinsey T.L., Mahoney O.M. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20(4):414. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Bonnin M.P., Archbold P.H.A., Basiglini L., Selmi T.A., Beverland D.E. Should the acetabular cup be medialised in total hip arthroplasty? Hip Int. 2011;21(4):428. doi: 10.5301/HIP.2011.8582. [DOI] [PubMed] [Google Scholar]
- 12.Charnley J. Springer-Verlag; New York, NY: 1979. Low friction arthroplasty of the hip: theory and practice. [Google Scholar]
- 13.Karachalios T., Hartofilakidis G., Zacharakis N., Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty. The role of the center of rotation. Clin Orthop Relat Res. 1993;296:140. [PubMed] [Google Scholar]
- 14.Maloney W.J., Keeney J.A. Leg length discrepancy after total hip arthroplasty. J Arthroplasty. 2004;19(4 Suppl 1):108. doi: 10.1016/j.arth.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 15.Sykes A., Hill J., Orr J. Patients’ perception of leg length discrepancy post total hip arthroplasty. Hip Int. 2015;25(5):452. doi: 10.5301/hipint.5000276. [DOI] [PubMed] [Google Scholar]
- 16.Konyves A., Bannister G.C. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87–B(2):155. doi: 10.1302/0301-620x.87b2.14878. [DOI] [PubMed] [Google Scholar]
- 17.Nam D., Sculco P.K., Abdel M.P., Alexiades M.M., Figgie M.P., Mayman D.J. Leg-length inequalities following THA based on surgical technique. Orthopedics. 2013;36(4):e395. doi: 10.3928/01477447-20130327-11. [DOI] [PubMed] [Google Scholar]
- 18.Delp S.L., Wixson R.L., Komattu A.V., Kocmond J.H. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res. 1996;328:137. doi: 10.1097/00003086-199607000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Johnston R.C., Brand R.A., Crowninshield R.D. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am. 1979;61:639. [PubMed] [Google Scholar]
- 20.Paprosky W.G., Muir J.M. Intellijoint HIP®: a 3D mini-optical navigation tool for improving intraoperative accuracy during total hip arthroplasty. Med Devices Evid Res. 2016;9:401. doi: 10.2147/MDER.S119161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parvizi J., Benson J.R., Muir J.M. A new mini-navigation tool allows accurate component placement during anterior total hip arthroplasty. Med Devices Evid Res. 2018;11:95. doi: 10.2147/MDER.S151835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muir J.M. Intellijoint Surgical, Inc.; Kitchener, Ontario, Canada: 2016. The learning curve for a new surgical mini - navigation system for total hip arthroplasty: a review of cases using Intellijoint HIP® (White paper) [Google Scholar]
- 23.Padgett D.E., Warashina H. The unstable total hip replacement. Clin Orthop Relat Res. 2004;420:72. doi: 10.1097/00003086-200403000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Montalti M., Castagnini F., Giardina F., Tassinari E., Biondi F., Toni A. Cementless total hip arthroplasty in crowe III and IV dysplasia: high hip center and modular necks. J Arthroplasty. 2018;33(6):1813. doi: 10.1016/j.arth.2018.01.041. [DOI] [PubMed] [Google Scholar]
- 25.Nawabi D.H., Meftah M., Nam D., Ranawat A.S., Ranawat C.S. Durable fixation achieved with medialized, high hip center cementless THAs for crowe II and III dysplasia. Clin Orthop Relat Res. 2014;472(2):630. doi: 10.1007/s11999-013-3187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jolles B.M., Zangger P., Leyvraz P.-F. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17(3):282. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 27.Meermans G., Doorn J Van, Kats J.-J. Restoration of the centre of rotation in primary total hip arthroplasty. Bone Joint J. 2016;98–B(12):1597. doi: 10.1302/0301-620X.98B12.BJJ-2016-0345.R1. [DOI] [PubMed] [Google Scholar]
- 28.Chechik O., Khashan M., Lador R., Salai M., Amar E. Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg. 2013;133(11):1595. doi: 10.1007/s00402-013-1828-0. [DOI] [PubMed] [Google Scholar]
- 29.Cross M., Schwarzkopf R., Miller T., Bogner E., Muir J., Vigdorchik J. Improving registration accuracy during total hip arthroplasty: a cadaver study of a new, 3D mini-optical navigation system. Hip Int. 2018;28(1):33. doi: 10.5301/hipint.5000533. [DOI] [PubMed] [Google Scholar]
- 30.Jaramaz B., DiGioia A.M., 3rd, Blackwell M., Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. 1998;(354):70. doi: 10.1097/00003086-199809000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Richolt J.A., Effenberger H., Rittmeister M.E. How does soft tissue distribution affect anteversion accuracy of the palpation procedure in image-free acetabular cup navigation? An ultrasonographic assessment. Comput Aided Surg. 2005;10(2):87. doi: 10.3109/10929080500229447. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.