Abstract
Background
E-cigarette or vaping has become an increasingly popular alternative to smoking tobacco. In September 2019 multiple cases of confirmed E-cigarette or vaping product use associated lung injury were published. However, there is limited knowledge regarding the pathologic mechanism of this condition.
Methods
We performed a systematic literature review in PubMed and EMBASE aiming to obtain additional clinical data on confirmed E-cigarette or vaping product use associated lung injury cases with lung biopsy results. With this information we hope to determine whether this condition is related to a histopathological pattern of acute lung injury instead of lipid deposits.
Results
Seven articles were reviewed and a total of 27 cases were included. Imaging findings predominantly showed presence of diffuse bilateral ground glass opacities. A majority of patients had complete resolution of the disease. The most common histopathological pattern was organizing pneumonia present in almost half of the patients. Other frequently occurring patterns included diffuse alveolar damage and acute fibrinous pneumonitis; lipoid pneumonia was found in one case.
Conclusion
The underlying pathophysiological mechanism in E-cigarette or vaping product use associated lung injury is most likely acute lung injury related to direct inhalant-mediated parenchymal inflammation.
Keywords: Vaping-associated lung injury, Acute lung injury, Histology, Lung biopsy
Highlights
-
•
Majority of cases with confirmed EVALI had diffuse bilateral ground glass opacities pattern.
-
•
Diffuse ground glass opacities are more associated with typical patterns (organizing pneumonia and diffuse alveolar damage).
-
•
Histological patterns are more consistent with acute lung injury than lipids deposition.
-
•
Damage to the lung parenchyma appears to be more related to direct inhaled toxin and/or thermal injury.
-
•
Variation of the pathologic findings could be secondary to the different types of possible noxious agents.
1. Introduction
E-cigarette or vaping has become increasingly popular owing to its wishful role as a safer alternative to smoking. It involves delivery of nicotine or tetrahydrocannabinol (THC) by inhalation of heated e-liquids containing several other chemicals including propylene glycol, glycerin and vitamin E acetate that are mixed with various flavors and fragrances [1]. In September 2019 multiple cases of E-Cigarette or Vaping Product Use Associated Lung Injury (EVALI) were published [2], and since then the understanding of this condition has evolved. However, there is limited knowledge regarding the pathologic mechanism of the condition. The aim of this study is to coalesce the updated literature regarding cases of confirmed EVALI with lung biopsy so we can foster a better understanding of the physiopathology of this condition.
2. Methods
2.1. Case report
We reviewed data from the clinical database of Trinitas Regional Medical Center to identify possible cases of EVALI with lung biopsy between June 2018 and April 2020. In addition, medical records from the patients included were analyzed in order to obtain information regarding clinical course, laboratory data, comorbidities, imaging and biopsy results. Retrieved data was stored in an electronic database. Only one patient was found during this period that fulfilled criteria for confirmed cases of EVALI as per diagnostic criteria [3] and also had lung biopsy results.
2.2. Literature review
We performed a systematic literature review in PubMed and EMBASE aiming to obtain additional clinical data on confirmed EVALI cases with lung biopsy results. Search strategies used both free-text and MeSH terms related to the topic involved (EVALI cases with lung biopsy). Articles were selected by title and abstract evaluation. Full-text analysis was done and subsequently included in the review.
3. Results
3.1. Case presentation
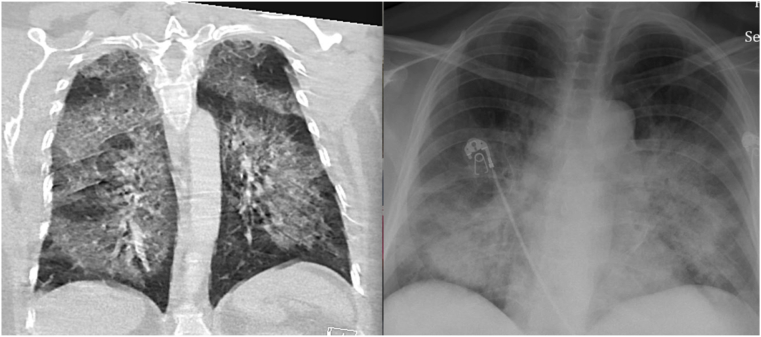
We present a 52-year old female with a past medical history of vaping THC who presented with complaints of persistent shortness of breath. She was initially placed on Bilevel positive airway pressure (BiPAP) due to tachypnea and desaturation to 83% on room air. Patient was afebrile with no overt clinical or laboratory evidence of infection. Initial chest X-ray (CXR) showed bilateral airspace opacities (Fig. 1). Given unexplained tachycardia, a computed tomography (CT) pulmonary angiogram was done and was significant for diffuse bilateral ground-glass opacity (DB GGO) (Fig. 1). The patient had to be intubated shortly after as she deteriorated on BiPAP. Due to an acute increase in her white blood cell count to 14,000, infectious work up was ordered including urine, blood and respiratory cultures; she was also placed on broad spectrum antibiotics.
Fig. 1.
Imaging findings in EVALI. A. Chest CT Pulmonary angiogram, coronal view: bilateral diffuse ground glass opacities. B. Portable CXR: bilateral patchy reticulonodular opacities.
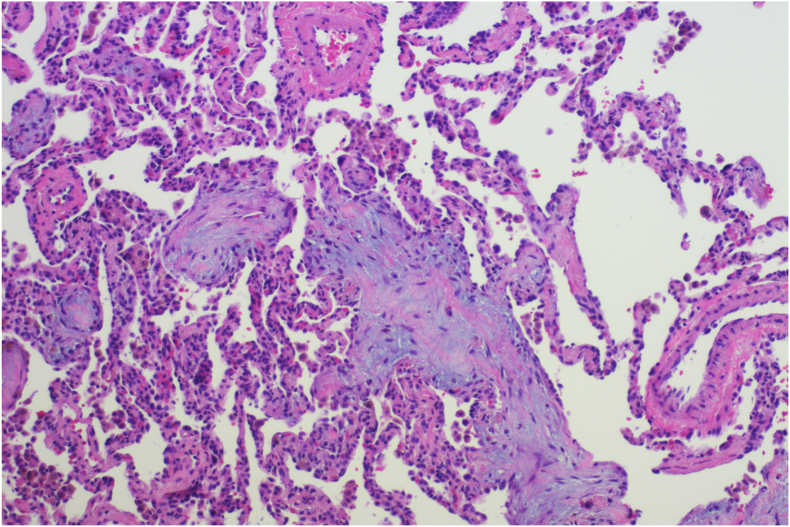
Due to a lack of clinical response and a negative infectious work up, patient was placed on IV methylprednisolone and a bronchoalveolar lavage (BAL) was scheduled, which had to be deferred due to lack of consent at that time. Due to unimproved clinical status, lack of clear diagnosis and persistent infiltrates on CXR, a video-assisted thoracoscopic surgery was performed with tissue biopsies done showing organizing pneumonia (OP) (Fig. 2). After the successful wedge resection and clinical improvement on the steroids, the patient was successfully extubated 2 days later. She was finally diagnosed with confirmed EVALI as infectious causes were not found, CXR & CT showed typical findings, positive history of vaping in the last 90 days and all alternative diagnosis were ruled out. Patient was discharged on oral steroids for a total of 10 days and repeat CXR 3-weeks after discharge showed complete resolution of infiltrates.
Fig. 2.
Lung specimen obtained by Video-Assisted Thoracoscopic Surgery. Hematoxylin and eosin stain x200 showing fibromyxoid plugs (Masson bodies) consisting of exudative materials including connective tissue components, fibrin and fibroblast within alveolar spaces and ducts consistent with organized pneumonia.
3.2. Literature review
Seven articles were selected for review. Two of them were relatively large case series in which all of the cases had a lung biopsy [4,5]; the largest article found had 98 cases however 51% (n = 50) were confirmed and 6.1% (n = 6) of them had a lung biopsy [3]. Three articles were case reports with one of them adding a literature review [6]. The last article was an extensive review of EVALI with four cases reports included in the description [7].
We present a total of 27 confirmed cases of EVALI with lung biopsy results (Table 1). Cases from Layden et al. were excluded as the results of lung biopsies were not clear. Patients had a mean age of 38.5 years and majority were male. Regarding chest CT findings, 89% (n = 24) of cases had diffuse bilateral ground glass opacities (DB GGO); rest of the patients reported bilateral reticulonodular opacities in 3.7% (n = 1), bilateral nodules in 3.7% (n = 1) and one had a CXR showing bilateral infiltrates without chest CT scan results.
Table 1.
Imaging characteristics, histopathology and prognosis of all patients with lung biopsy-confirmed EVALI.
| Author | Cases | Age (yr) (Mean) | CT Scan Findings | Histopathology Pattern | Outcomes |
|---|---|---|---|---|---|
| Khan et al. [6] | 1 | 40 | DB GGO | OP | Resolution |
| Butt et al. [4] | 11 | 33.7 | DB GGO (9/11) BRN (1/11) CXR Bl (1/11) |
AFP (1/11) OP (2/11) AFP + OP (4/11) DAD (4/11) |
Resolution (5/11) Death (2/11)c Unknown (4/11) |
| Mukhopadhyay et al. [5] | 8 | 29.2 | DB GGO (8/8) | OP (6/8) DAD (2/8) |
Resolution (7/8) Death (1/8) c |
| Kligerman et al. [7] | 4 | 27.5 | DB GGO (4/4) | OP (2/4) DAD (1/4) OP/DAD (1/4) |
Resolution (1/4) Death (1/4)c Unknown (2/4) |
| Remolina et al. | 1 | 52 | DB GGO | OP | Resolution |
| Madsen et al.b [9] | 1 | 45 | BN | MNG | Resolution |
| Layden et al. [3] | 50 | 21 | Unknown | OP, DAD, GP a | Unknown |
| Visvam et al. [10] | 1 | Unknown | DB GGO | LP | Resolution |
DB GGO: Diffuse bilateral ground-glass opacity, BRN: Bilateral reticulonodular infiltrates, CXR: Chest X-ray, Bl: bilateral infiltrates, BN: Bilateral nodules, OP: Organizing Pneumonia, AFP: Acute Fibrinous Pneumonitis, DAD: Diffuse Alveolar Damage, GP: Granulomatous Pneumonitis, MNG: Multinucleated Giant Cells, LP: Lipoid Pneumonia.
Unknown frequency.
Not confirmed EVALI.
Dead associated with DAD.
Pathology results of the cases showed that 48% (n = 13) had OP, 26% (n = 7) diffuse alveolar damage (DAD), 15% (n = 4) a combination of Acute Fibrinous Pneumonitis (AFP) with OP, and the rest of them showed AFP in 3.7% (n = 1), lipoid pneumonia (LP) in 3.7% (n = 1) and in 3.7% (n = 1) it was not clear between OP or early DAD. Finally, 63% (n = 17) of patients had complete resolution of symptoms and imaging findings. There was no outcome reported in 22% (n = 6) of the cases and 15% (n = 4) of patients died. DAD was present in all patients who died.
4. Discussion
We conducted a case report and literature review to increase the understanding of the histopathology of patients with EVALI. Currently there are extensive reports regarding epidemiology and clinical manifestation about the condition, however studies evaluating the pathophysiology are sparse. Here, we present a confirmed case of EVALI with tissue biopsy that will add more information to the current knowledge of the disease and promote further research in order to answer critical questions of this novel pathology.
4.1. Imaging findings in EVALI
In our case, the patient developed bilateral infiltrates in the CXR and subsequently a chest CT angiogram was done showing DB GGO, which was the most common pattern found in our review. During the evaluation of the included articles we found no controversy about the different imaging findings of this pathology [[3], [4], [5], [6], [7],9,10]. As we reported the majorities of these confirmed cases with lung biopsy have DB GGO in the chest CT scan and was more related with typical histological patterns, like OP and DAD. The only patient that showed bilateral nodules in the chest CT scan had multinucleated giant cells in the biopsy [9], which is an unusual result in this condition. This could suggest that in patients with probable EVALI and a non-typical chest CT scan pattern, the need of lung biopsy could be essential to guide an accurate diagnosis. In that case the biopsy was done to rule out malignancy, and the diagnosis of EVALI was probable.
4.2. Histopathologic pattern in confirmed EVALI
Our patient's biopsy result showed OP, which is one of the most common forms of histology results in EVALI. In our literature review, majority of cases showed OP, followed by DAD and AFP for a combined total of 96% [[3], [4], [5], [6], [7],9,10]. This suggests that the majority of confirmed EVALI have a histopathologic pattern related to acute lung injury which is typically associated with direct chemical inflammation, indicating a possible existence of a direct insult from the inhaled toxin and/or thermal injury to the lung parenchyma. The two largest case series reports concur with this hypothesis, corroborating that the variation of the pathologic findings could be secondary to different types of possible noxious agents [4,5]. This is supported by Kligerman et al., when they described that there are 288 E-cigarettes models with over 15,500 distinct flavors and combinations [7] indicating that inhaled particles are commonly unknown and could vary in each patient. This makes the understanding of EVALI a pathophysiologic challenge as multiple agents may be involved that have the potential to cause their own pathology. As a result, we believe that focus must be directed on diagnosing EVALI as part of a spectrum of variable clinical manifestations and not enclose these patients in a typical presentation.
Initial studies of EVALI proposed that this condition was a result of oil deposition causing LP as most of the BAL analysis found lipid laden macrophages. We found a letter to the editor that could explain this hypothesis [8] suggesting that the way the biopsy specimens are handled, lipids may be washed out and persistent positive staining for lipids found in the BAL fluid means that it should also be present in the tissue specimen. Finally, they stated that BAL analysis should be sufficient to establish the diagnosis of EVALI; a conclusion we have to disagree with based on this review. More recent literature drifts away from this hypothesis suggesting that the pathology is more related to acute lung injury caused by either inhaled toxins and/or thermal injury [4,5]. After review of the 27 biopsy results, we found that majority of cases are related to an acute lung injury pattern such as OP and DAD, and only 1 case reported LP. Butt et al., argues that the above-mentioned technique to handle BAL specimens should not obscure the diagnosis of LP. Additionally, they mention that current staining techniques cannot differentiate between endogenous and exogenous lipids due to the poor specificity of these tests (Lipid laden macrophages could be seen in any accumulation of lipids due to epithelial injury, cell debris, surfactants and endogenous lipids from cell membranes) [8]. As a result, we concur that performing lipid stains should not be recommended in BAL analysis or lung biopsy since it would be unable to distinguish EVALI from other causes of acute lung injury.
In conclusion, advances in the understanding of the clinical findings and histopathology of EVALI have been made and continue to evolve. Currently, the chest imaging patterns are clear and current studies agree that DB GGO is the classic finding in this pathology. Additionally, we must continue with the idea that EVALI is likely a result of direct lung damage by inhaled agents causing acute lung injury as highlighted by the most common pattern in the histopathology of this review. We also want to use this article to acknowledge that this disease is ever-present in all medical care settings, and we believe that primary care workers and physicians in community hospitals should be aware of the possibility and management of EVALI.
Funding
There was not funding involve in the developed of this paper.
CRediT authorship contribution statement
Jorge Cedano: Conceptualization, Methodology, Writing - original draft, Data curation. Anuraag Sah: Conceptualization, Writing - original draft, Data curation. Ricardo Cedeno-Mendoza: Writing - original draft. Heidi Fish: Writing - review & editing. Carlos Remolina: Writing - review & editing, Supervision.
Declaration of competing interest
None of the authors declared any conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101122.
Contributor Information
Jorge Cedano, Email: jorgea91@gmail.com.
Anuraag Sah, Email: sah.anuraag@gmail.com.
Ricardo Cedeno-Mendoza, Email: ricardo_cedenom@hotmail.com.
Heidi Fish, Email: hfish@trinitas.org.
Carlos Remolina, Email: carlos_remolina@yahoo.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gordon T., Fine J. Concerning the suspects in vaping-associated EVALI. N. Engl. J. Med. 2020;382:755–756. doi: 10.1056/NEJMe2001065. [DOI] [PubMed] [Google Scholar]
- 2.Blount B.C., Karwoski M., Shields P.G. Vitamin E acetate in bronchoalveolar-lavage fluid associated with EVALI. N. Engl. J. Med. 2020;382:697–705. doi: 10.1056/NEJMoa1916433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Layden J., Ghinai I., Pray I. Pulmonary illness related to E-cigarette use in Illinois & Wisconsin - final report. N. Engl. J. Med. 2020;382:903–916. doi: 10.1056/NEJMoa1911614. [DOI] [PubMed] [Google Scholar]
- 4.Butt Y.M., Smith M.L., Tazelaar H.D. Pathology of vaping-associated lung injury. N. Engl. J. Med. 2019;381(18):1780–1781. doi: 10.1056/NEJMc1913069. [DOI] [PubMed] [Google Scholar]
- 5.Mukhopadhyay S., Mehrad M., Dammert P. Lung biopsy findings in severe pulmonary illness. Am. J. Clin. Pathol. 2020;153:30–39. doi: 10.1093/ajcp/aqz182. [DOI] [PubMed] [Google Scholar]
- 6.Khan M.S., Khateeb F., Akhtar J. Organizing pneumonia related to electronic cigarette use: a case report and review of literature. Clin. Res. J. 2018;12:1295–1299. doi: 10.1111/crj.12775. [DOI] [PubMed] [Google Scholar]
- 7.Kligerman S., Raptis C., Larsen B. Radiologic, pathologic, clinical, and physiologic findings of electronic cigarette or vaping product use–associated lung injury (EVALI): evolving knowledge and remaining questions. Radiology. 2020;294:491–505. doi: 10.1148/radiol.2020192585. [DOI] [PubMed] [Google Scholar]
- 8.Davidson K.R. Fox DL more on the pathology of vaping-associated lung injury. N. Engl. J. Med. 2020;382:387–390. doi: 10.1056/NEJMc1914980. [DOI] [PubMed] [Google Scholar]
- 9.Madsen L.R., Krarup N., Bergmann T. Cancer that went up in smoke: pulmonary reaction to e-cigarettes imitating metastatic cancer. Chest. 2016;149(3):65–67. doi: 10.1016/j.chest.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Viswam D., Trotter S., Burge P.S. Respiratory failure caused by lipoid pneumonia from vaping e-cigarettes. Br. Med. J. 2018;224:350. doi: 10.1136/bcr-2018-224350. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.