Abstract
Background/purpose
The clinical diagnosis of temporomandibular joint (TMJ) degenerative joint disease (DJD) is based primarily on radiographic features of the condyle and articular eminence. The purpose of this study was to compare the reliability, sensitivity, and specificity of using plain radiography to that of cone-beam computerized tomography (CBCT) in identifying different types of osseous degenerative features in the TMJ condyle.
Materials and methods
The panoramic radiography (PANO), TMJ quadruple radiography (TMJQR) and CBCT images of 29 patients’ TMJs were retrieved from a computer database and independently evaluated by a young oral surgeon and a senior TMD specialist. The examiners diagnosed osseous degenerative features on the radiographic images. The radiologist-assisted CBCT diagnoses were used as a reference standard and the reliability, sensitivity, and specificity of using the three radiographic modalities were statistically analyzed.
Results
There were cases of indeterminate diagnoses using the PANO and TMJQR due to superimposition from surrounding structures, but none using CBCT. Reliability was generally poor when using PANO and TMJQR for detecting osseous degenerative features of the TMJ condyle but good to excellent when using CBCT. The sensitivity and specificity in the use of PANO and TMJQR were typically below acceptable, but the levels were generally satisfactory when using CBCT.
Conclusion
CBCT is superior to plain radiographic modalities for diagnosing osseous degenerative features of TMJs with regard to indeterminate cases, reliability, sensitivity, and specificity. It is recommended that CBCT can be used as an effective tool in identifying TMJ osteoarthritis.
Keywords: TMJ, Osseous degenerative features, Panoramic radiography, TMJ quadruple Radiography, Cone-beam computerized tomography
Introduction
“Temporomandibular disorders” (TMD) is a collective term that has been long used since the early 1980s to describe a group of clinical disorders occurring in the musculoskeletal components of the masticatory system.1 The Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) has differentiated 12 common TMD,2 one of which is degenerative joint disease (DJD). The Axis I of DC/TMD suggests that a combined clinical and radiographic assessment helps better diagnose DJD. An increasing number of studies have recently focused on the degenerative changes of the osseous component of the TMJ.3, 4, 5
The clinical diagnosis of TMJ DJD is based primarily on radiographic features of the condyle and articular eminence, including deviation in form, surface erosion, subcortical sclerosis, subcortical cyst, osteophyte formation, and bony ankylosis.2,6, 7, 8 Several radiographic techniques such as panoramic radiography (PANO), TMJ radiography, and computerized tomography (CT) have been used in TMJ image diagnostics.6,9, 10, 11 Some panoramic machines have special functions that enable the images of the opened and closed mouth view of both TMJ condyles to be viewed on a single radiograph; such technique is called TMJ quadruple radiography (TMJQR). Cone-beam CT (CBCT) has been highly recommended as an alternative imaging technique for the diagnosis of degenerative changes of the TMJ due to lower radiation exposure compared to conventional CT.12,13
The purpose of this paper is to compare the reliability, sensitivity, and specificity of using PANO, TMJQR and CBCT by a junior examiner and a senior examiner in identifying TMJ osseous degenerative features, such as deviation in form, surface erosion, subcortical cyst, subcortical sclerosis, and osteophyte. This study was approved by the Research Ethics Committee at the National Taiwan University Hospital in Taipei, Taiwan (201904088RINA).
Materials and methods
Consecutive outpatients seeking treatment at the Department of Dentistry at National Taiwan University Hospital between January and April 2019 for symptoms such as pain and noises in the TMJ region during jaw movement and/or difficulty when opening the mouth were included in this study. During the clinical evaluation, they also received PANO and TMJQR as routine image examinations. If DJD in at least one TMJ was suspected, a CBCT examination was ordered to confirm the diagnosis. The clinical examination procedure followed the recommendation in DC/TMD.2 This retrospective study retrieved 29 patients’ PANO, TMJQR, and CBCT images from the database; a total of 58 TMJs were analyzed.
Image acquisition
Panoramic and TMJ quadruple radiographies: Veraviewepocs 2D (J. Morita Mfg. Corp., Kyoto, Japan) and i-Dixel software were used for scanning digital PANO and TMJQR. The parameter setting followed the standard scanning protocol provided by the manufacturer (high resolution mode with a default setting of 65 kV and 5 mA, 1.3× magnification). The radiographs were acquired with proper subject positioning as recommended by the manufacturer of the equipment. The PANO showed the maxilla and mandible, including dentition and both condyles located in the TMJ fossa. In some cases, the TMJs could be superimposed by surrounding bony structures of the cranial base (Fig. 1).
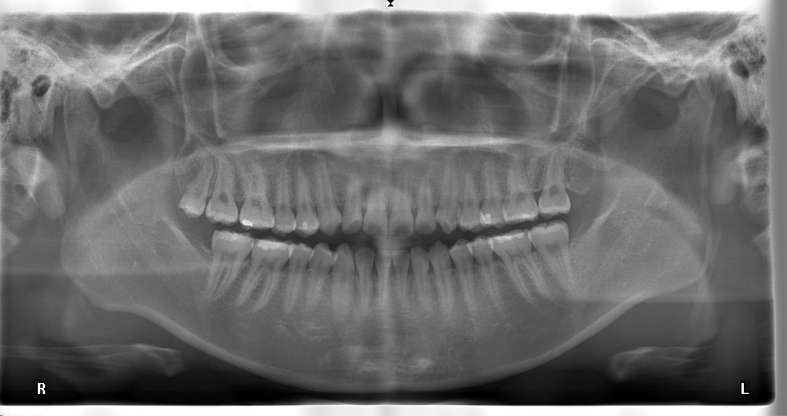
Figure 1.
An example of the panoramic radiograph from one of the patients. It showed the maxilla and mandible, including the dentition and both of the condyles located in the TMJ fossa. In this case, the left and right TMJs were partially superimposed by surrounding bony structures of the cranial base.
The TMJQR showed the condyles of the left and right TMJs at two jaw positions: one with the mouth closed and the condyle in the fossa and the other with the mouth opened as wide as possible and the condyle out of the fossa (Fig. 2). When the TMJ was out of the fossa, the superimposition of the condyle by the surrounding bony structures was able to be avoided. The TMJQR provided an extra opportunity to examine the morphology of the TMJ from a slightly different projection angle compared with PANO. However, in some patients who had limited range of mouth opening, their TMJs may still remain in the fossa.
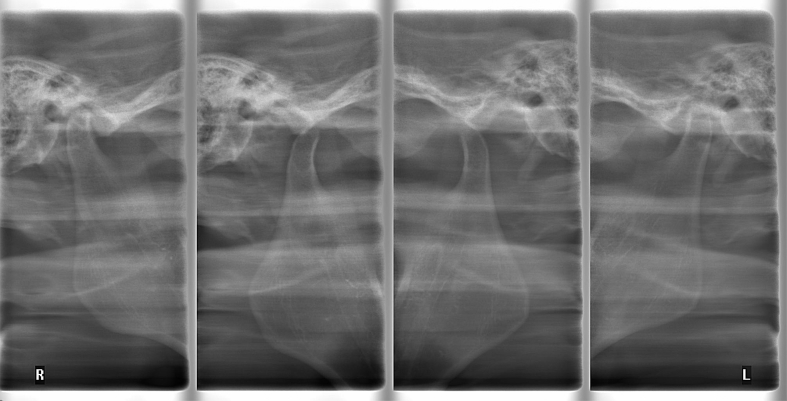
Figure 2.
The TMJ quadruple radiograph from the same subject presented in Fig. 1. The images at the far left and far right showed the right and left TMJ condyles in the fossa when the mouth was closed; the condyles were superimposed by the surrounding bony structures. The images at the central left and central right showed the condyles out of the fossa when the mouth was widely opened. Even in this case when the TMJs were out of the fossa, it was still not easy for the examiners to judge if there were any osseous degenerative features in the TMJ condyles.
Cone-beam CT: The 3DX Accuitomo (J Morita Mfg. Corp., Kyoto, Japan) was used for the CBCT scan. A standardized scanning protocol (90 kVp, 5 mA, 30.8 s, FOV 6 × 6 cm, with a high resolution of 0.125 mm voxel size, approximate effective dose = 114 μSv1) was followed during the image acquisition. The examiners used the One Volume Viewer software (i-Dixel 3DX Vision 2.2.1.3T, J Morita Mfg. Corp.) to move or rotate the volume rendered image and the slice images. The slice images allowed the examiners to analyze the CBCT images slice-by-slice for TMJ osseous degenerative features on axial, frontal, and sagittal planes. Using the mouse to double click an image allowed for magnification and better evaluation of osseous degenerative features (Fig. 3).
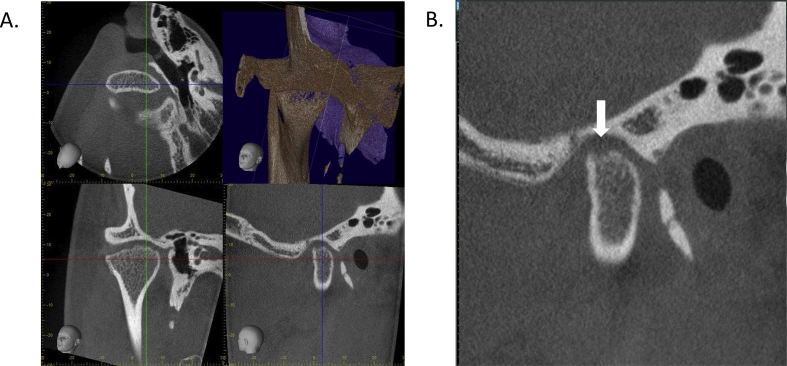
Figure 3.
The cone-beam CT images of the right TMJ of the same patient in Figure 1, Figure 2 on the i-Dixel3DXsoftware. A. The volume rendered image (upper-right), the slice images of the axial view (upper-left), the front view (lower-left), and sagittal view (lower-right). The three cursor lines can be moved by use of the computer mouse to implement the slice-by-slice examination of the condyle. B. The magnified sagittal view. The arrow points to a surface erosion that was superposed by surrounding bony structure in the panoramic radiograph image presented in Fig. 1 and could be overlooked by examiners when viewing the TMJ quadruple radiograph in image presented in Fig. 2.
Two examiners reviewed and interpreted each radiographic image independently. The junior examiner (Examiner 1) had completed a combined post-graduate and clinical training in oral surgery and had 4 years of limited exposure to TMD patients. The senior examiner (Examiner 2) had 29 years of experience specializing in TMD and orofacial pain. The junior examiner had spent two months, two times per week, staying with the senior examiner in the TMD/Orofacial Pain Clinic for calibration of image diagnosis before the study was initiated. All images were labeled with codes by two radiographers from the Department of Radiology so that the examiners were blind to the clinical histories and diagnoses of these patients. The analysis criteria for TMJ osseous degenerative features followed the guideline published by Ahmad et al.6 and the “worst case” principle was followed when diagnosis for each osseous degenerative feature was made during the image examination. The observed changes of the osseous component in the three radiographic modalities included deviation in form, surface erosion, subcortical cyst, subcortical sclerosis, and osteophyte. Table 1 described the definition for each feature. Examples of osseous degenerative features in CBCT were displayed in Fig. 4.
Table 1.
Definition for the osseous degenerative features observed in the TMJ condyle.
| Nomenclature | Definition Criteria |
|---|---|
| Deviation in form | A departure from normal shape, such as concavity in the cortical outline, attributable to surface erosion, osteophytes, hyper or hypoplasia. |
| Surface erosion | Reduced density or a loss of continuity of the articular cortical outline. |
| Subcortical cyst | A radiolucent cavity beneath the articular surface that looked different from normal bone marrow patterns. |
| Subcortical sclerosis | An increased calcification density relative to adjacent bone marrow. |
| Osteophyte | A sclerotic border with marginal hypertrophy and beak-like angular formation of osseous tissue arising from the articular surface. |
Note. Adapted from Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107: 844–60.
Figure 4.
Examples of osseous degenerative features observed in CBCT: A. Deviation in form; B. Subcortical cyst; C. Subcortical sclerosis; D. Osteophyte; E. Bony ankyloses; F. Calcified chondromatosis. Surface erosioncan be seen on the condylar surface in images A, B, C, D, and F.
When each observation was completed, a diagnosis was made to categorize the joint as normal (no degenerative change), indeterminate, or osseous degeneration. The criteria for each diagnosis was provided in Table 2. The diagnoses were further categorized as negative (normal or indeterminate) versus positive (frank osseous degeneration) for each TMJ. In order to establish a diagnostic reference standard, a senior radiologist was invited to review the CBCT images again and discuss with the two examiners until a consensus was reached among the two examiners and the radiologist. The agreed upon CBCT diagnosis was then used as a reference standard for assessments of the reliability, sensitivity, and specificity of the three radiographic modalities by the two examiners for detecting osseous degenerative features in the condyle.
Table 2.
Diagnosis for the osseous TMJ degenerative changes from panoramic radiograph, TMJ quadruple radiograph, and cone-beam computerized tomography.
|
|
|
|
|
|
|
|
|
|
Statistics
Inter-examiner agreement of the three radiographic modalities were estimated using the kappa (κ) statistic. The two examiners’ diagnostic reliability of PANO and TMJQR compared to the agreed CBCT diagnosis as the standard reference was also estimated using the κ statistic. Fleiss et al.14 have suggested that κ values of <0.40 are considered to be poor reliability, values from 0.40 to 0.75 are considered to be fair to good reliability, and values of >0.75 are considered to be excellent reliability. The sensitivity and specificity of the three radiographic modalities, using the agreed CBCT diagnoses as the standard reference, were also calculated. Acceptable values of sensitivity and specificity for a definitive diagnosis were considered as following: sensitivity ≥70% and specificity ≥95%.15 One-way and two-way ANOVA tests were used to determine the differences among the effects of radiographic modalities, examiners on the inter-examiner agreement, and the reliability, sensitivity, and specificity of diagnosing TMJ osseous degenerative features by the use of the three radiographic modalities. All statistical analyses were conducted using SPSS version 20 (IBM Corp. Armonk, NY, USA).
Results
Twenty-nine patients went through the above-mentioned clinical and radiographic examinations from January to April in 2019. Only one of these patients was male, and twenty-eight of them were female. The youngest patient was 13 years old and the oldest was 67 years old. The mean age of these participants was 38.6 ± 17.4 (mean ± S.D.) years old. A total of 58 TMJs were examined. Based upon the clinical and radiographic examinations which we pooled together after the image examination, 11 TMJs were diagnosed as normal (with no pain nor osseous degenerative changes), four as arthralgia (with pain or tenderness but no osseous degenerative changes), seven as osteoarthrosis (with osseous degenerative changes but no pain), and 36 as osteoarthritis (with both pain and osseous degenerative changes).
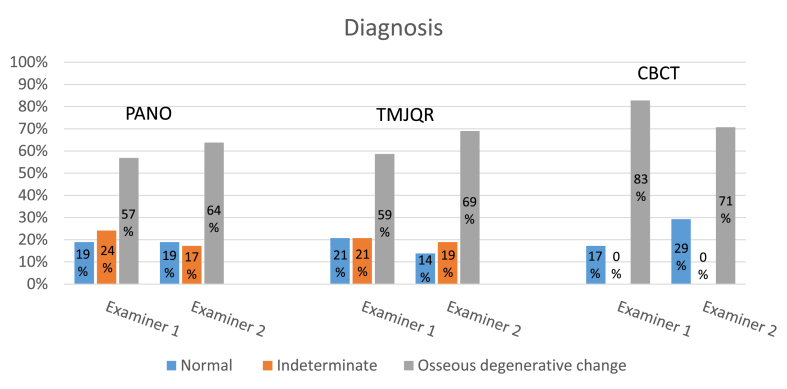
For diagnoses of osseous degenerative features based on PANO and TMJQR images, there were cases classified as indeterminate due to superimposition by adjacent bony structures, improper patient positioning or movement, or poor image quality. In contrast, there were no indeterminate diagnoses when using CBCT imaging by the two examiners (Fig. 5) and the radiologist.
Figure 5.
There are indeterminate cases using the two plain radiographies due to structure superimposition or positioning of the patients; there were no indeterminate cases using CBCT.
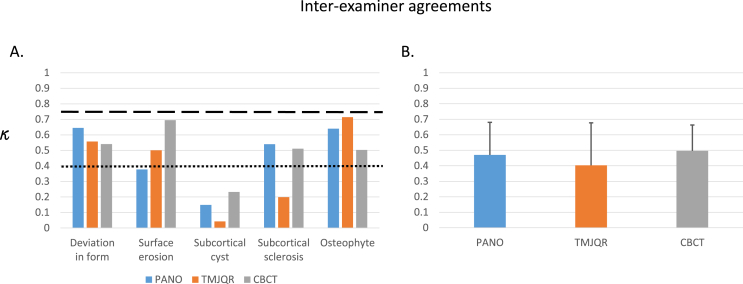
Inter-examiner agreement varied when using different radiographic modalities in diagnosing different degenerative features (Fig. 6A). Agreement was fair to good (κ = 0.501–0.714) in diagnosing deviation in form and osteophyte, but was poor in diagnosing subcortical cyst (κ = 0.043–0.232). Agreement was also fair to good in diagnosing surface erosion and subcortical sclerosis (κ = 0.501–0.695), except for surface erosion diagnosis using PANO (κ = 0.377) and for subcortical sclerosis diagnosis using TMJQR (κ = 0.199). There was no significant difference in inter-examiner agreement among the three radiographic modalities (F = 0.238, p = .792, one-way ANOVA test, see Fig. 6B).
Figure 6.
A. Inter-examiner agreements (κ) for diagnosis of TMJ degenerative features. The dotted line labels the κ values of0.40 and the dashed line labels the κ values of 0.75. B. Comparison of the inter-examiner agreements among using the three radiographic modalitiesshows no significant difference (p > .05, one-way ANOVA test).
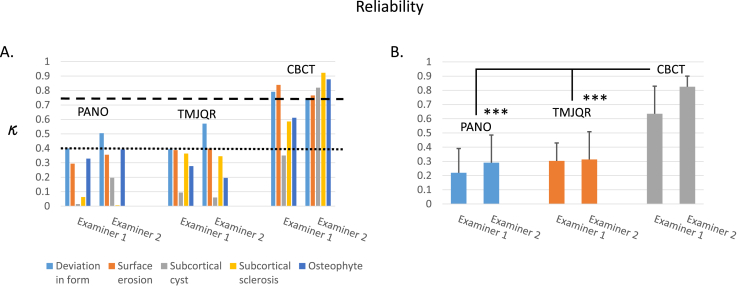
With the agreed upon CBCT diagnosis as the reference standard, the reliabilities of both examiners using PANO and TMJQR for detecting degenerative changes of the TMJ condyle were poor (κ = 0.015–0.399), with the exception of the experienced examiner being able to make a fair to good diagnosis for deviation in form when examining the PANO and TMJQR (κ = 0.505 and 0.571, respectively). However, both examiners were able to make nearly excellent to excellent diagnoses for all TMJ osseous degenerative features by using CBCT (κ = 0.743–0.877), with the exception that the junior examiner had some difficulty identifying subcortical cyst (κ = 0.350). The reliability of using the three radiographic modalities in diagnosing osseous degenerative features are summarized in Fig. 7A. There were no significant differences between the two examiners (F = 2.25, p = .146, two-way ANOVA test) nor significant interaction between the modality and examiner factors (F = 0.766, p = .476) in the reliability of diagnosing osseous degenerative features using the three radiographic modalities by the two examiners. However, there was a significant difference among the three radiographic modalities (F = 24.80, p < .001). The post-hoc analysis showed significantly higher reliability using CBCT than using PANO and TMJQR (both p < .001, Bonferroni test). No significant differences appeared between PANO and TMJQR (p = .756). The statistical analysis for reliability was shown in Fig. 7B.
Figure 7.
A. Reliability (κ) for diagnosis of TMJ osseous degenerative features using the three modalities by the two examiners. The dotted line labels the κ values of 0.40 and the dashed line labels the κ values of >0.75. B. Comparison of the reliability for identification of TMJ osseous degenerative features using the three modalities by the two examiners. There were significantly higher reliabilities using CBCT than using PANO and TMJQR (∗∗∗p < .001, post-hoc analysis, Bonferronitest).
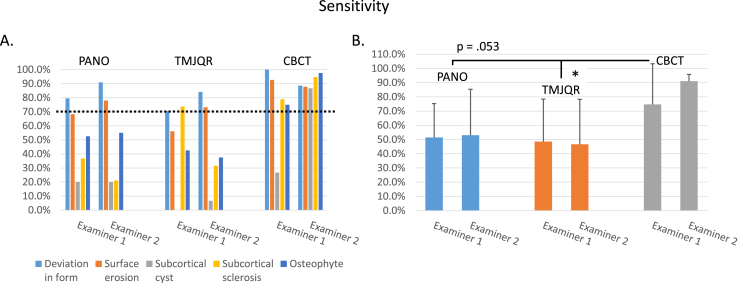
The sensitivity and specificity of the three radiographic modalities, using the agreed upon CBCT diagnosis as the reference standard, are shown in Figure 8, Figure 9. Both examiners used PANO and TMJQR to identify deviation in form with sensitivities above the acceptable 70% level (70.5–90.9%). The senior examiner also managed to identify surface erosion with a >70% level of sensitivity using PANO (78.0%) and TMJQR (73.2%). However, the sensitivities of the two examiners using the two plain radiographies in diagnosing subcortical cyst, subcortical sclerosis, and osteophyte were far below the acceptable level (0–55%), except in that the junior examiner identified subcortical sclerosis with a sensitivity of 73.7% using PANO. On the other hand, both examiners identified all osseous degenerative features with satisfactory sensitivities (75–100%) when using CBCT, except in that the junior examiner had some difficulties identifying subcortical cyst with CBCT (26.7%). The two-way ANOVA test showed a significant difference in sensitivity among the three radiographic modalities (F = 5.068, p = .015). The post-hoc analysis showed the difference occurred between CBCT and TMJQR (p = .022), while nearly significant difference was found between CBCT and PANO (p = .053), and no difference was found between PANO and TMJQR (p = 1.0). There was also no significant difference between the two examiners (F = 0.21, p = .592) nor significant interaction between the modality and examiner factors (F = 0.24, p = .725; see Fig. 8B).
Figure 8.
A. Sensitivity using the three modalities by the two examiners in diagnosing different TMJ osseous degenerative features. The dotted line indicates the acceptable 70% for sensitivity. B. Comparison of the sensitivities for identification of TMJ osseous degenerative features using the three modalities by the two examiners. There was a significantly higher sensitivity using CBCT than using TMJQR (∗p < .05, post-hoc analysis, Bonferronitest) and a nearly significant difference between CBCT and PANO.
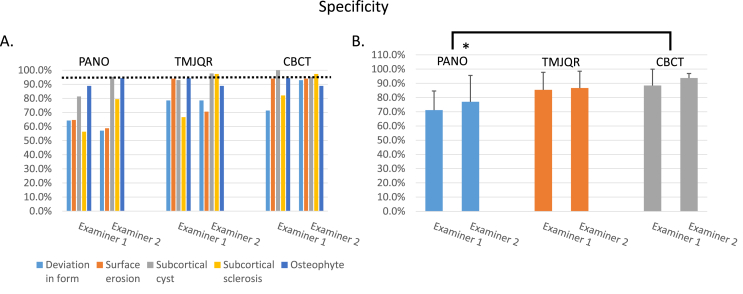
Figure 9.
A. Specificity using the three modalities by the two examiners in diagnosing different TMJ osseous degenerative features. The dotted line indicates the acceptable 95% for specificity. B. Comparison of the specificities for identification of TMJ osseous degenerative features using the three modalities by the two examiners. Using CBCT had a significantly higher specificity than using PANO (∗p < .05, post-hoc analysis, Bonferronitest).
The specificities of using the three radiographic modalities in identifying osseous degenerative features varied. Stable and near satisfactory or satisfactory specificity (>95%) was achieved only when CBCT was used by the senior examiner to diagnose the five osseous degenerative features (Fig. 9A). A significant difference in specificity was found among the three radiographic modalities (F = 4.74, p = .018). The post-hoc analysis showed that the significant difference was between CBCT and PANO (p = .019) and no significant differences was found between CBCT and TMJQR (p = .138) or between PANO and TMJQR (p = 1.0). There were also no significant differences in specificity between the two examiners (F = 0.81, p = .377) nor significant interaction between the modality and examiner factors (F = 0.098, p = .907; see Fig. 9B).
Discussion
In this study, we adopted the criteria published by Ahmad et al. for interpreting radiographic images and compared the inter-examiner agreements, reliabilities, sensitivities and specificities of using PANO, TMJQR and CBCT in identifying different osseous degenerative features in the TMJs.6 We have demonstrated indeterminate cases using the two plain radiographies due to structure superimposition or positioning of the patients while no indeterminate cases were encountered using CBCT by clinicians who are not radiologists. The inter-examiner agreements of using the three radiographic modalities to identify the osseous degenerative features were fair to good, at best, and were poor when the examiners tried to identify subcortical cysts. The reliabilities of both examiners when using PANO and TMJQR were generally poor but were nearly excellent or excellent when using CBCT. Both the junior and senior examiners could use CBCT to identify most osseous degenerative features with satisfactory sensitivities, but the sensitivities when using PANO and TMJQR in diagnosing osseous degenerative features were usually below the acceptable 70% level. And only the senior examiner using CBCT could identify osseous degenerative features with consistent and acceptable specificity.
Similarities in indeterminate rates, low reliabilities, sensitivities and specificities when using PANO and TMJQR to diagnose different TMJ osseous degenerative features suggest that the mouth opened and closed views of both TMJs on TMJQR did not produce a substantial advantage over PANO in diagnosing DJD. These findings also agree with previous studies that PANO and its derivative TMJQR have poor reliability and low sensitivity, compared with CT, for detecting TMJ-related osseous changes and suggest that plain imaging modalities have limited utility for assessing the TMJs.6,16
The observed image on a plain radiography is a two-dimensional presentation of a three-dimensional structure. Cadaveric condyles exhibit significant variations in shape and angulation; the exact radiographic position of the lateral and medial poles and the articulating surface cannot be consistently predicted on PANO, despite knowing the horizontal and vertical angulation of the condyle on the cadaveric skulls.17 Only limited areas of the condyle can be visually assessed on plain radiographies. Poor patient positioning during the acquisition of plain radiographs exaggerates the condition; the image may be distorted and cease to be useful for diagnosis. In addition, images of the same joint vary in different jaw positions of mouth opening, as well as in different projection angles of the radiographic beams.18 If the condyle is located in the TMJ fossa, the image of the joint is also likely to be superimposed by adjacent bony structures of the cranial base. Accurate diagnosis of osseous degenerative features relies heavily on the resolution of the margin of these features on the radiographic images. Superimposition by the bony condylar component and/or the surrounding bony structures blurs the margins. It has been shown that osteophytes cannot be clearly identified if they are not located on the anterolateral aspect of the joint.19 Given the aforementioned conditions, precise condylar morphology cannot be depicted on plain radiographic images and thus determining the presence of pathologic changes in the TMJs is generally not possible using the traditional plain radiographs. The inherent limitation of PANO and TMJQR explains the low reliability, sensitivity, and specificity of using these plain radiographic modalities by examiners. However, the experienced examiner can still make a reliable diagnosis for deviation in form, which is the sum of all osseous changes in the joint, with acceptable sensitivity by using PANO and TMJQR. The PANO also provides extra information concerning osseous and odontogenic pathologies in the maxilla and mandible and has been recommended as a screening tool for the evaluation of orofacial osseous pathology.6,20,21 Many clinicians commonly use the panoramic radiograph in daily practice due to its relatively low cost compared with CBCT. Its potential to rule out dental or other mandibular diseases that contribute to orofacial pain should not be ignored.
CBCT software allows examiners to inspect and analyze images from all angles without superimposition of bony structures, explaining why neither examiners nor the radiologist encountered any indeterminate cases when using CBCT. CBCT images display precise localization and the extent of morphological changes in the TMJ condyle and fossa.9,10 Its usefulness has been extensively discussed in relevant literature,9,22 and the use of CBCT for a reliable diagnosis of osseous degeneration has been highly recommended.6,21 Our results agree with previous studies in the superiority of CBCT in revealing more detailed degenerative changes in the TMJ bony structures than conventional plain radiographic methods and demonstrate a special advantage in the diagnosis of TMJ DJD.23,24 The reliabilities of the senior examiner when using CBCT were nearly excellent or excellent, and they were good to excellent for the junior examiner, suggesting that the diagnostic accuracy of using CBCT can be improved by experience accumulation and calibration. Nevertheless, the cases of generally acceptable sensitivity and less than acceptable specificity levels when using CBCT also indicate that more studies are necessary to validate the usefulness of CBCT in diagnosing osseous degenerative features. More importantly, it takes information acquired from clinical examination, together with the CBCT analysis, to make a differential diagnosis between osteoarthritis and osteoarthrosis.
Significantly lower levels of reliability, sensitivity, and specificity when using PANO and TMJQR compared to when using CBCT, paired with no significant differences in diagnostic reliability, sensitivity and specificity between the senior and the junior examiners using the two plain radiographic modalities, indicate a common inherent limitation shared by PANO and TMJQR that cannot be attributed to the varying level of experience between the examiners. Yet, PANO is useful in detecting radiolucent and radiopaque lesions in the maxilla and mandible and odontogenic pathologies. The mouth opened view of TMJQR helps detect TMJ condyle translation and coronoid hyperplasia. Each of these two modalities contribute individual advantages for dental clinicians and cannot fully substitute the function of the other. We suggest that PANO and TMJQR should be included in the diagnostic system during screening evaluations of TMD and orofacial pain.
Previous studies have shown low inter-examiner agreement using plain radiography for detecting TMJ osseous degeneration.16,25 The inter-examiner agreement in this study varies when diagnosing different osseous degenerative features, ranging from poor to good (κ = 0.043–0.714). Agreement was fair to good in diagnosing deviation in form and osteophyte, but poor in diagnosing subcortical cyst. The observed deformation in TMJ can be a deviation of a normal joint (e.g. hyperplasia or hypoplasia) with no clinical symptoms or it could be a real reflection of TMJ pathology with any combination of surface erosion, subcortical cyst, sclerosis or osteophyte. Osteophytes are relatively easy to identify because they appear as beak-like objects that stand out from the smooth cortical surface of the condyle, while subcortical cysts seldom are observed alone and appear more often concurrently with surface erosion or osteophyte.6,26 This could have attributed to the apparent difficulty the junior examiner faced when trying to identify subcortical cyst. Surface erosion is one of the osseous degenerative features frequently observed in TMJ as well as in other joints.6,27, 28, 29, 30 However, it is easy to overlook surface erosion if it is not located on the cortical outline on a plain radiographic image. Localized subcortical sclerosis was viewed as a sign of remodeling, a function of age and not a prediction of the progression of osseous degeneration by some researchers.6 Generalized subcortical sclerosis, however, is associated with cartilage degradation and has been considered to be a sign of osseous degeneration.31 We found it difficult to differentiate localized and general subcortical sclerosis and considered both an osseous degenerative feature of the TMJ in this study.
In this study, we focused only on analyzing the osseous degenerative changes of the TMJ condyles on radiographic images. The osseous degenerative features in the temporal component of TMJ and their topographic distribution in both components were not clear. Pain with the potential to be affected by psychosocial and behavioral factors was also not considered in this study. More studies are necessary to address these issues in order to elucidate the relationship between osseous degenerative changes and clinical symptoms of TMD patients.
In conclusion, the CBCT is superior for cases of indetermination and showed higher levels of reliability, sensitivity, and specificity to that of plain radiographic modalities for diagnosing DJD of TMJs due to its capability of allowing clinicians to inspect and analyze the TMJ morphology from all angles without superimposition of bony structures. It is recommended that CBCT can be used as an effective tool to confirm indecisive and doubtful osseous degenerative changes in TMJ before initiating any long-term and high-cost treatments such as orthodontic treatment and orthognathic surgery. PANO and TMJQR also have special advantages in detecting pathologies in the maxilla and mandible and should be included in the diagnostic system during the screening evaluations of TMD and orofacial pain.
Acknowledgments
The paper is funded by Research Project of National Taiwan University Hospital: 109-4450.
References
- 1.Laskin D., Greenfield W., Gale E. The President's conference on the examination, diagnosis and management of temporomandibular disorders. Chicago: American Dental Association.Kopp S. Topographical distribution of sulfated glycosaminoglycans in the surface layers of the human temporomandibular joint. J Oral Pathol. 1983;7:283–294. doi: 10.1111/j.1600-0714.1978.tb01812.x. [DOI] [PubMed] [Google Scholar]
- 2.Schiffman E., Ohrbach R., Truelove E. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and Research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache. 2014;28:6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Embree M., Ono M., Kilts T. Role of subchondral bone during early-stage experimental TMJ osteoarthritis. J Dent Res. 2011;90:1331–1338. doi: 10.1177/0022034511421930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiao K., Niu L.N., Wang M.Q. Subchondral bone loss following orthodontically induced cartilage degradation in the mandibular condyles of rats. Bone. 2011;48:362–371. doi: 10.1016/j.bone.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 5.Wang X.D., Kou X.X., He D.Q. Progression of cartilage degradation, bone resorption and pain in rat temporomandibular joint osteoarthritis induced by injection of iodoacetate. PloS One. 2012;7 doi: 10.1371/journal.pone.0045036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmad M., Hollender L., Anderson Q. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–860. doi: 10.1016/j.tripleo.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalladka M., Quek S., Heir G. Temporomandibular joint osteoarthritis: diagnosis and long-term conservative management: a topic review. J Indian Prosthodont Soc. 2014;14:6–15. doi: 10.1007/s13191-013-0321-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao Y.P., Zhang Z.Y., Wu Y.T. Investigation of the clinical and radiographic features of osteoarthrosis of the temporomandibular joints in adolescents and young adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:e27–e34. doi: 10.1016/j.tripleo.2010.09.076. [DOI] [PubMed] [Google Scholar]
- 9.Alexiou K.E., Stamatakis H.C., Tsiklakis K. Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography. Dentomaxillofacial Radiol. 2009;38:141–147. doi: 10.1259/dmfr/59263880. [DOI] [PubMed] [Google Scholar]
- 10.Cevidanes L.H.S., Hajati A.-K., Paniagua B. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:110–117. doi: 10.1016/j.tripleo.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ludlow J.B., Davies K.L., Tyndall D.A. Temporomandibular joint imaging: a comparative study of diagnostic accuracy for the detection of bone change with biplanar multidirectional tomography and panoramic images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:735–743. doi: 10.1016/s1079-2104(05)80259-8. [DOI] [PubMed] [Google Scholar]
- 12.Cohnen M., Kemper J., Möbes O. Radiation dose in dental radiology. Eur Radiol. 2002;12:634–637. doi: 10.1007/s003300100928. [DOI] [PubMed] [Google Scholar]
- 13.Hashimoto K., Arai Y., Iwai K. A comparison of a new limited cone beam computed tomography machine for dental use with a multi-detector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:371–377. doi: 10.1067/moe.2003.120. [DOI] [PubMed] [Google Scholar]
- 14.Fleiss J.L., Levin B., Paik M.C. 3rd ed. John Wiley & Sons; Hoboken (NJ): 2003. Statistical methods for rates and proportions; pp. 598–626. [Google Scholar]
- 15.Dworkin S.F., LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 16.Crow H.C., Parks E., Campbell J.H. The utility of panoramic radiography in temporomandibular joint assessment. Dentomaxillofacial Radiol. 2005;34:91–95. doi: 10.1259/dmfr/24863557. [DOI] [PubMed] [Google Scholar]
- 17.Fallon S.D., Fritz G.W., Laskin D.M. Panoramic imaging of the temporomandibular joint: an experimental study using cadaveric skulls. J Oral Maxillofac Surg. 2006;64:223–229. doi: 10.1016/j.joms.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 18.Mawani F., Lam E., Heo G. Condylar shape analysis usingpanoramic radiography units and conventional tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:341–348. doi: 10.1016/j.tripleo.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 19.Masood F., Katz J.O., Hardman P.K. Comparison of panoramic radiography and panoramic digital subtraction radiography in the detection of simulated osteophytic lesions of the mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:626–631. doi: 10.1067/moe.2002.121704. [DOI] [PubMed] [Google Scholar]
- 20.Brooks S.L., Brand J.W., Gibbs S.J. Imaging of the temporomandibular joint: a position paper of the American academy of oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:609–618. doi: 10.1016/s1079-2104(97)90128-1. [DOI] [PubMed] [Google Scholar]
- 21.Ferreira L.A., Grossmann E., Januzzi E. Diagnosis of temporomandibular joint disorders: indication of imaging exams. Brazi J Otorhinolaryngol. 2016;82:341–352. doi: 10.1016/j.bjorl.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Honda K., Larheim T.A., Maruhashi K. Osseous abnormalities of the mandibular condyle: diagnostic reliability of cone beam computed tomography compared with helical computed tomography based on an autopsy material. Dentomaxillofacial Radiol. 2006;35:152–157. doi: 10.1259/dmfr/15831361. [DOI] [PubMed] [Google Scholar]
- 23.dos Anjos Pontual M.L., Freire J.S., Barbosa J.M. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofacial Radiol. 2012;41:24–29. doi: 10.1259/dmfr/17815139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krisjane Z., Urtane I., Krumina G. The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: a cone-beam CT study. Int J Oral Maxillofac Surg. 2012;41:690–695. doi: 10.1016/j.ijom.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 25.Schmitter M., Gabbert O., Ohlmann B. Assessment of the reliability and validity of panoramic imaging for assessment of mandibular condyle morphology using both MRI and clinical examination as the gold standard. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:220–224. doi: 10.1016/j.tripleo.2005.07.039. [DOI] [PubMed] [Google Scholar]
- 26.Akerman S., Kopp S., Rohlin M. Macroscopic and microscopic appearance of radiologic findings in temporomandibular joints from elderly individuals. An autopsy study. Int J Oral Maxillofac Surg. 1988;17:58–63. doi: 10.1016/s0901-5027(88)80232-7. [DOI] [PubMed] [Google Scholar]
- 27.Honey O.B., Scarfe W.C., Hilgers M.J. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: comparisons with panoramic radiology and linear tomography. Am J Orthod Dentofacial Orthop. 2007;132 doi: 10.1016/j.ajodo.2005.10.032. 429–8. [DOI] [PubMed] [Google Scholar]
- 28.Koyama J., Nishiyama H., Hayashi T. Follow-up study of condylar bony changes using helical computed tomography in patients with temporomandibular disorder. Dentomaxillofacial Radiol. 2007;36:472–477. doi: 10.1259/dmfr/28078357. [DOI] [PubMed] [Google Scholar]
- 29.Derek T., Cooke V., Kelly B.P. Radiographic grading for knee osteoarthritis. A revised scheme that relates to alignment and deformity. J Rheumatol. 1999;26:641–644. [PubMed] [Google Scholar]
- 30.Pattrick M., Hamilton E., Wilson R. Association of radiographic changes of osteoarthritis, symptoms, and synovial fluid particles in 300 knees. Ann Rheum Dis. 1993;52:97–103. doi: 10.1136/ard.52.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burr D.B., Schaffler M.B. The involvement of subchondral mineralized tissues in osteoarthrosis: quantitative microscopic evidence. Microsc Res Tech. 1997;37:343–347. doi: 10.1002/(SICI)1097-0029(19970515)37:4<343::AID-JEMT9>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]