Abstract
During the coronavirus disease 2019 (COVID-19) pandemic, cancer centers must implement effective measures to protect patients and staff from infection with the novel coronavirus. A critical component of this effort is the timely identification of patients undergoing treatment who have COVID-19. Limitations on testing make such efforts challenging. However, the specialty of radiation oncology is unique in its use of computed tomography (CT) imaging for image guidance, and these CT studies have the potential to identify patients with COVID-19 even before they develop symptoms. Several organizations have developed published guidelines for radiologists to identify characteristic findings of COVID-19 on thoracic CT scans. The present article describes these recommendations in order to educate radiation oncologists on how to identify potential cases of COVID-19 and empower physicians in our field to optimally protect patients and staff.
The recent global spread of the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and its associated disease, coronavirus disease 2019 (COVID-19), has led to rapid and unprecedented changes in the practice of radiation oncology worldwide. For radiation oncology centers, a critical component of effective response is the reliable identification of patients undergoing radiation therapy who may be infected with the virus. Patients with cancer appear to be at higher risk for COVID-19 than the general population, and they may be more likely to experience a severe clinical course.1 Additionally, patients undergoing radiation therapy may be likely vectors for the virus because they are treated in a confined vault with limited ventilation, and they must interact with multiple health care workers on a daily basis. Thus, even a single patient undergoing radiation therapy who is infected with SARS-CoV-2 represents a high risk to other patients and staff.
The task of identifying patients with COVID-19 is particularly challenging given that patients may be asymptomatic for a period after initial infection.2 Ideally, all patients undergoing radiation therapy would undergo testing by reverse transcriptase polymerase chain reaction (RT-PCR) or assays for antibodies to SARS-CoV-2. However, at the present time, the limited availability of such tests in many centers might make such a strategy difficult to use. Currently, many centers have implemented screening procedures, such as daily temperature checks and verbal screening to identify patients who may have been exposed to the virus.3
As radiation oncologists grapple with how best to identify patients with COVID-19 in our centers, computed tomography (CT) may prove useful. The practice of radiation oncology uniquely uses CT imaging for both treatment simulation and image guidance. A busy center with a high rate of use of cone beam CT (CBCT) or CT on rails (CTOR) might be expected to perform dozens of thoracic CT scans in a day, and, in most centers, the majority of these scans are never formally interpreted by a radiologist.
Although the specificity of CT for COVID-19 infection is low owing to overlap with other disease processes, the sensitivity appears to be as high as 98% in symptomatic patients.4 Several authors have published their descriptions of the usual CT findings, and, more recently, several organizations, including the Radiologic Society of North America (RSNA), the Dutch Radiologic Society, and the British Society of Thoracic Imaging have published reporting frameworks for chest CT studies in patients with suspected COVID-19.5,6 The findings of ground glass opacities (GGOs) with peripheral and multifocal distribution seem to be the most specific pattern found with COVID-19 pneumonia (classified as typical within the RSNA framework), and in our experience, multifocal peripherally distributed rounded GGOs and multilobar peripheral GGOs have correlated well with RT-PCR positive disease. Central and peribronchovascular GGOs can represent COVID-19 pneumonia, but this pattern technically qualifies as indeterminate per the RSNA consensus statement and appears to be less specific for COVID-19. Consolidation without GGOs is infrequently associated with COVID-19 and qualifies as an atypical pattern for disease. Table 1 summarizes the imaging classifications published by RSNA.7 Examples of typical and indeterminate pattern CT findings (per the RSNA classification system) are provided in Figure 1, Figure 2, Figure 3 to 4.
Table 1.
Categories suggested by the RSNA for reporting imaging findings in patients suspected to have COVID-19
| RSNA classification | GGOs | Other findings |
|---|---|---|
| Typical appearance | Rounded, multifocal, bilateral, with peripheral distribution | “Reverse halo sign” (central cavitation) may be present in later stages of disease Consolidation may be present |
| Indeterminate appearance | Nonrounded, unilateral, nonperipheral, or lacking specific distribution | Consolidation may be present |
| Atypical appearance | Focal distribution or absent | Isolated lobar or segmental consolidation Discrete small nodules Cavitation Tree-in-bud opacities Interlobular septal thickening, pleural effusion |
| Negative for pneumonia | Absent | None |
Abbreviations: COVID-19 = Coronavirus Disease 2019; GGO = ground glass opacities; RSNA = Radiologic Society of North America.
Figure 1.
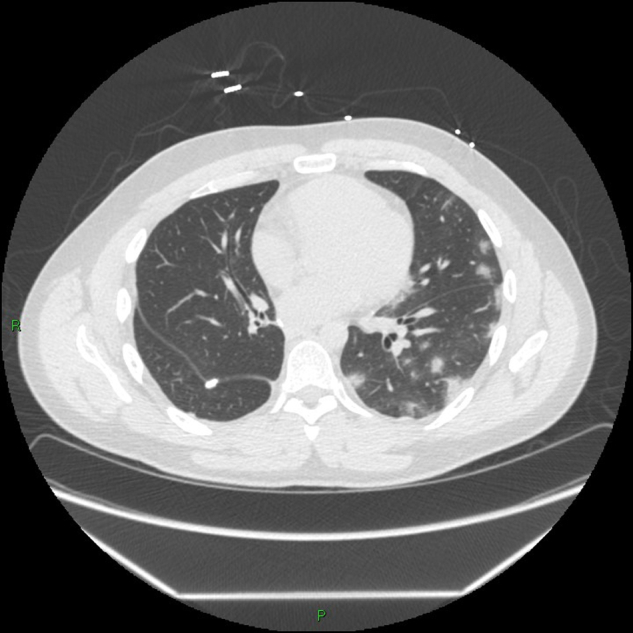
Typical computed tomography pattern associated with coronavirus disease 2019 of multifocal rounded and peripheral ground glass opacities.
Figure 2.
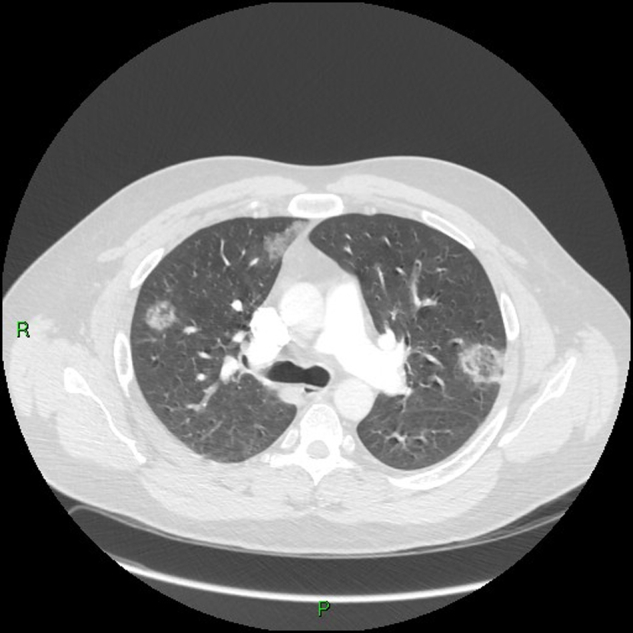
Typical computed tomography pattern with multifocal peripheral ground glass opacities with reverse halo sign (often seen later in the course of disease).
Figure 3.
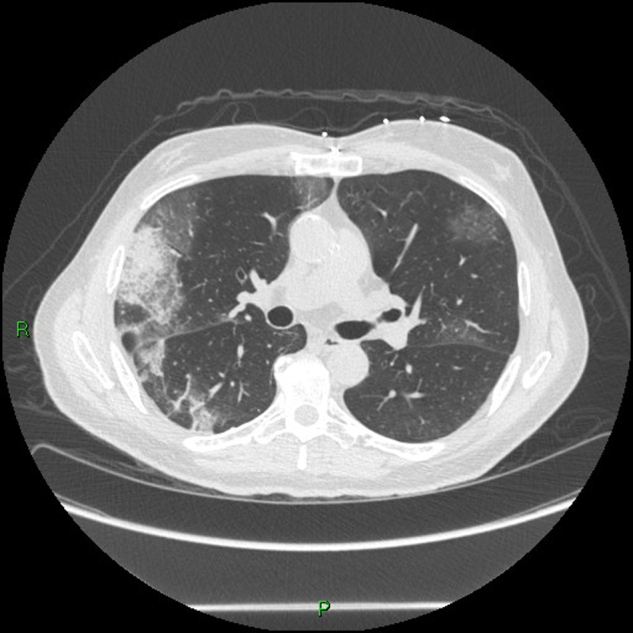
Typical chest computed tomography findings in cases from the cruise ship Diamond Princess with Coronavirus Disease 2019. Pattern with dominant peripheral ground glass opacities pattern which is multifocal and multilobar.
Figure 4.
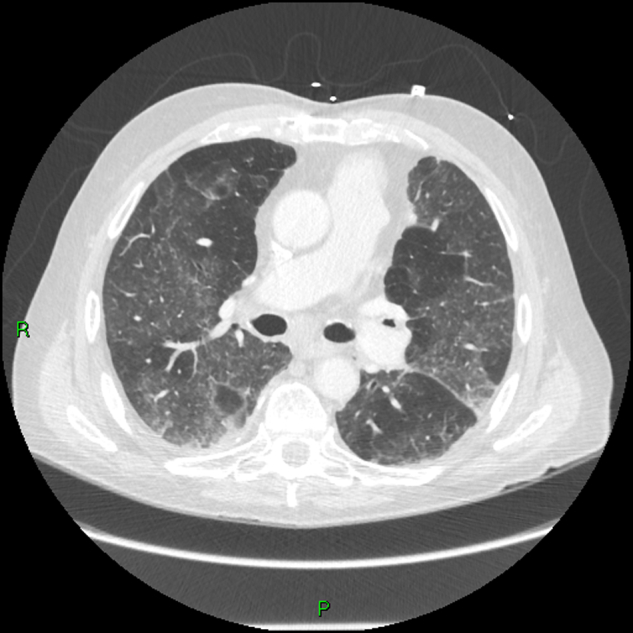
Indeterminate computed tomography pattern with multifocal diffuse ground glass opacities (GGO) distribution without dominant peripheral GGO or rounded GGO pattern.
Several recent case reports highlight 2 primary mechanisms by which image guidance CT studies may help to diagnose patients with COVID-19. First, these studies may identify radiographic abnormalities in patients who develop respiratory symptoms while undergoing radiation therapy. In a report from Denmark, for example, the authors describe a patient with locally advanced non-small cell lung cancer who developed cough, fever, and myalgias and subsequently tested positive for SARS-CoV-2. On retrospective review of the patient’s daily CBCT imaging, the authors noted that there had been multifocal pulmonary GGOs present 36 hours before the onset of symptoms.8 Similarly, in a report from Maimonides Cancer Center in Brooklyn, New York, the authors retrospectively reviewed CBCT images from a patient who had developed COVID-19 symptoms during the second week of radiation therapy for treatment of breast cancer. In this case, bilateral peripheral GGOs were present on CBCT imaging taken 2 days before symptom onset.9
At least 2 published reports describe how CT for image guidance has prospectively identified radiographic changes of COVID-19 in asymptomatic patients. Both of these reports describe patients whose new diagnoses of COVID-19 were detected when CBCT or CTOR performed on the first day of radiation therapy demonstrated new GGOs that had not been seen on the CT simulation done days to weeks earlier.10,11 In one of these cases, the imaging findings prompted a laboratory test which confirmed COVID-19.
These cases serve as important reminders for radiation oncologists to review image guidance CT scans carefully, particularly in the midst of the COVID-19 pandemic. Additionally, the possibility of identifying COVID-19 on CT might influence how physicians choose to perform daily imaging of patients who are receiving thoracic radiation therapy. In some cases, orthogonal kV x-ray images and CT-based images may offer relatively equivalent utility in terms of positional verification. However, 2-dimensional kV imaging may be less likely to identify COVID-19 related changes. Therefore, radiation oncologists might elect to choose CT-based image guidance for this reason. Finally, if a patient is undergoing CT simulation for treatment of a nonthoracic target, the physician might consider extending the field of view to include the lungs, acknowledging that such an approach would increase the imaging radiation dose to the patient. At least one center, Northwell Health in New York, is developing a clinical trial to evaluate such an approach.
When typical findings of COVID-19 are seen on CT imaging, the patient should be considered a person under investigation, and RT-PCR testing for COVID-19 is warranted even if the patient is asymptomatic. Clinicians should inform the infection control department at their facility and should implement isolation protocols as suggested by the Centers for Disease Control and local public health authorities. It is also critical to provide adequate personal protective equipment for health care workers interacting with such a patient. Physicians should decide whether to continue radiation therapy on an individual basis. A hypothetical “decision tree,” such as the one proposed by Rivera et al, may be useful to assess the appropriateness of initiation or completion of radiation therapy in patients with COVID-19 or persons under investigation.12
In considering the expansion of the role of CT imaging in Radiation Oncology, there are a number of important stipulations. First, although CT is sensitive for detecting COVID-19 in symptomatic patients, as noted above, the sensitivity is substantially lower in patients who do not have symptoms. A retrospective review of cases of COVID-19 on the Diamond Princess cruise ship reported that, within the cohort of patients who were asymptomatic upon diagnosis, CT opacities were identified in 54% of cases.13 As CBCT and CTOR yield a lower image quality compared with diagnostic CT, the sensitivity of these studies for COVID-19 may be even lower. Second, using CT in a diagnostic capacity in a Radiation Oncology center introduces additional work for physicians and staff. In particular, in settings in which radiation therapists, as opposed to physicians, are responsible for overseeing image guidance, implementing additional steps into the workflow may prove difficult. Third, physicians should consider the potential risks of delivering additional radiation dose to patients when using CT imaging compared with 2-dimensional kV imaging or in extending the field of view to include the lungs. Finally, as incidental findings of COVID-19 are likely to be rare in radiation oncology, physicians may face a difficult learning curve in their accurate identification.
As the COVID-19 pandemic continues, radiation oncologists must be vigilant about identifying potentially infected patients in their clinics. To that end, careful review of radiation therapy imaging studies, along with an understanding of characteristic radiographic signs of COVID-19 infection, represent an important opportunity to protect both patients and staff.
Footnotes
Sources of support: The authors have received no financial support or grant funding related to this manuscript.
Disclosures: The authors declare no conflicts of interest applicable to this manuscript.
References
- 1.Liang W., Guan W., Cher R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rothe C Schunk M., Sothmann P. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Z, Wang G, He J. Active and effective measures for the care of patients with cancer during the COVID-19 spread in China [e-pub ahead of print]. JAMA Oncol. 10.1001/jamaoncol.2020.1198. Accessed April 10, 2020. [DOI] [PubMed]
- 4.Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR [e-pub ahead of print]. Radiology. 10.1148/radiol.2020200432. Accessed April 10, 2020. [DOI] [PMC free article] [PubMed]
- 5.Prokop M., van Everdingen W., van Rees Vellinga T. CO-RADS–A categorical CT assessment scheme for patients with suspected COVID-19: Definition and evaluation. Radiology. 2020;40:E8–E15. doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.British Society Of Thoracic Imaging Thoracic imaging in COVID-19 infection guidance for the reporting radiologist. Version 2, March 16, 2020. https://www.bsti.org.uk/standards-clinical-guidelines/clinical-guidelines/bsti-covid-19-guidance-for-the-reporting-radiologist/ Available at: Accessed May 25, 2020.
- 7.Simpson S., Kay F., Abbara S. Radiological Society of North America Expert Consensus Statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suppli MH, de Blanck SR, Elgaard T, et al. Early appearance of COVID-19 associated pulmonary infiltrates during daily radiotherapy image guidance for lung cancer. J Thorac Onco, in press. [DOI] [PMC free article] [PubMed]
- 9.Youssef I, Donahue B, Flyer M, et al. Covert Covid-19: CBCT lung changes in an asymptomatic patient receiving radiotherapy. Adv Radiat Oncol. 2020;5:715-721. [DOI] [PMC free article] [PubMed]
- 10.McGinnis G.J., Ning M.S., Nitsch P.L. Rapid detection of asymptomatic COVID-19 by CT image guidance for stereotactic ablative radiotherapy. J Thorac Oncol. 2020;15:1085–1087. doi: 10.1016/j.jtho.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samson P, Ning MS, Shaverdian N, et al. Clinical and radiographic presentations of COVID-19 among patients receiving radiation therapy for thoracic malignancies. Adv Radiat Oncol. 2020;5:700-704. [DOI] [PMC free article] [PubMed]
- 12.Rivera A, Ohri N, Thomas E, et al. The impact of COVID-19 on radiation oncology clinics and cancer patients in the US. Adv Radiat. 2020;5:538-543. [DOI] [PMC free article] [PubMed]
- 13.Inui S., Fujikawa A., Jitsu M. Chest CT findings in cases from the cruise ship ‘Diamond Princess’ with Coronavirus Disease 2019 (COVID-19) Radiol Cardiothorac Imaging. 2020;2 doi: 10.1148/ryct.2020200110. [DOI] [PMC free article] [PubMed] [Google Scholar]


