Highlights
-
•
Patients with mental illness may be at higher risk for contracting COVID-19, and environmental factors place inpatient psychiatric facilities at substantial risk for local outbreaks.
-
•
Here, we described an operational algorithm for testing and triage for COVID-19 designed to reduce the risk of intra-institutional outbreaks in inpatient psychiatric facilities.
-
•
We developed this algorithm while treating 47 COVID-19-positive and 158 Covid-19-negative psychiatric inpatients in a large freestanding psychiatric hosptial near new york city between march and april 2020.
Abstract
Psychiatric patients are at high risk for contracting COVID-19, and inpatient psychiatric units face substantial risks of institutional outbreaks. Here, the authors describe an algorithm for testing and triage in a large psychiatric facility designed to prevent local COVID-19 transmission. The algorithm is based on expert opinion and clinical experience between March and April of 2020, during which the institution cared for 47 COVID-19 positive psychiatric inpatients. The implementation of the algorithm is designed to mitigate COVID-19 transmission, preserve the safest and least restrictive treatment environment for psychiatric inpatients, and provide a model adaptable to other institutional settings.
1. Introduction
Inpatient psychiatric facilities face unique challenges during the COVID-19 (coronavirus disease 2019) pandemic. Patients with severe mental illness may be at higher risk of COVID-19 infection because of limited access to resources in the community, high rates of residence in population-dense dwellings such as shelters or supportive housing, and difficulty accessing or integrating public health recommendations designed to reduce rates of transmission (Shinn and Viron, 2020 Apr 28). Within inpatient psychiatric units, the environment may increase the risk of viral transmission as patients commonly share spaces such as bedrooms, bathrooms, and dining facilities and participate in group therapeutic activities (Li, 2020 Apr 23). Acute psychiatric syndromes may also interfere with patients’ ability to adhere to or accept interventions designed to reduce transmission including social distancing, use of masks, and nasal swab COVID-19 testing (Fahed et al., 5). Together, these behavioral and environmental factors place inpatient psychiatric facilities at substantial risk for local outbreaks of COVID-19. Other facilities have reported drastic infection spread, including a South Korean psychiatric unit where 101 out of 103 patients contracted the virus (Ying et al., 10).
In a commentary highlighting the challenges COVID-19 presents to psychiatric facilities, (Li, 2020 Apr 23) Li notes that "few published accounts are available on operational changes in response to COVID-19, especially in psychiatry." Here, we present an algorithm for COVID-19 patient screening, testing, isolation, and treatment, developed at a large inpatient psychiatric facility near the U.S. epicenter of COVID-19 infections in the greater New York region. This algorithm was designed to prevent and mitigate COVID-19 transmission in a psychiatric hospital with multiple inpatient services treating COVID-19 positive and COVID-19 negative patients on a self-contained campus and was implemented between March and April 2020. During this time 205 patients were tested and 47 were positive for COVID-19.
2. Hospital structure
Prior to the pandemic, patients presented to the hospital's psychiatric evaluation center where they underwent a diagnostic evaluation. They were then admitted to one of 13 inpatient units depending on diagnostic and demographic variables such as presenting diagnosis, age, gender, and the location of available beds. These procedures were significantly modified to mitigate transmission when community spread of COVID-19 became widespread in the region.
During the acute phase of the pandemic, we created three distinct spaces within the hospital.
2.1. The COVID-19 negative units
COVID-19 negative units are reserved for patients who tested negative immediately prior to admission. Patients are assigned to interaction cohorts of up to 6 patients. The size of the cohort groups was chosen to implement social distancing, as recommended by the Center for Disease Control (CDC) by maintaining 6 feet distance during therapeutic group activities. Patients wear surgical masks when in common areas including dining rooms and in spaces for group therapeutic activities. Unit clinicians including psychiatrists and nurses determine patient assignment to the cohorts. Double rooms in which patient beds cannot be moved out of a six-foot radius are converted to single rooms. Staff on these units wear surgical masks but not full personal protective equipment (PPE), as per recommendations from the larger hospital system's department of Infection Control and Prevention.
The possibility of a false-negative test (Woloshin et al., 5) and the length of the incubation period of COVID-19 raises the likelihood that a patient with occult COVID-19 infection may develop symptoms such as fever above 38.0 °Celsius, cough, shortness of breath, or diarrhea (Guan et al., 30) after initial admission to the COVID-19 Negative unit. If this occurs, the symptomatic patient is declared a Person Under Investigation (PUI) and placed in a single room on their current unit with contact and droplet isolation precautions (Precautions to Prevent Transmission of Agents, 2020). If they are able to maintain isolation precautions, they remain on the COVID-19 Negative unit pending test results. If they are unable to adhere to contact and droplet precautions, they are transferred to the COVID-19 Positive unit.
If a patient on a COVID-19 Negative unit converts to COVID-19 positive, the hospital system's Office of Infection Control and Prevention provides a consultation and recommendations for contact tracing to asses exposure risk to other patients and staff and whether to close the unit to additional patient admissions until the possibility of local spread has been ruled out. Patients and staff who are felt to have had a significant exposure to the COVID-19 positive individual are tested or retested. Staff and patients with less significant exposure are observed for COVID-like symptoms, and they continue to use surgical masks and practice social distancing according to local procedure on the COVID-19 Negative unit.
2.2. The holding area for untested persons
Patients requiring psychiatric admission who were not tested prior to admission are triaged to the Holding Area. In our facility, a portion of a designated unit separated from the remainder of the unit by a physical barrier serves this function. Patients in the Holding Area are maintained in their rooms and wear surgical masks. Staff wear PPE in accordance with hospital guidance for interacting with patients with low or high suspicion for COVID-19 infection, which is based on whether or not they have any COVID-like symptoms. This space has a transient population as turn-around time for COVID-19 testing is between 12 and 24 h. Patients participate in therapeutic activities that are compatible with isolation requirements. After patients in the Holding Area complete COVID-19 testing, they are transferred to COVID-19 Negative or Positive units.
2.3. The COVID-19 positive unit
Patients on the COVID-19 Positive unit are assigned to single rooms and are placed on droplet and contact isolation. Staff on the unit wear full PPE which consists of gown, gloves, N95 or surgical mask, and eye protection. Therapeutic activities are conducted mainly using a telehealth platform and include 5–6 groups per day, individual sessions, family sessions, and other clinical interactions. Patients, physicians and nursing staff have access to each other with hospital provided tablet computers. Detailed telehealth procedures are described elsewhere (Cheung et al., 2020; Francois et al., preparation; Kanellopoulos et al., 2020). Patients are retested fourteen days after their original COVID-19 positive swab. If they continue to test positive, they are retested every 3 days thereafter. When a patient tests negative, a second test is administered on the subsequent day; if the second test confirms a negative result, the patent is transferred to a COVID-19 Negative unit or discharged to appropriate aftercare. In circumstances where patients become psychiatrically stable for discharge and remain COVID-19 positive, they are discharged home with appropriate aftercare in place for both their psychiatric needs and COVID-19 related care and explicit instructions for self-quarantining and symptom monitoring.
Patients on the COVID-19 Positive unit are evaluated and treated medically for their COVID-19 illness by internists and medical nurse practitioners. Their vital signs and pulse oximetry are monitored twice daily. If a patient develops decreased oxygen saturation below 94% on room air, worsening shortness of breath, chest pain, or dyspnea on exertion, they are transferred to a medical emergency room for further evaluation. Risk factors (age > 50, hypertension and cardiovascular disorders, diabetes mellitus, chronic lung and renal disease, obesity, immunosuppression) are also considered in the clinical management and decision to transfer patients to emergency medical services. Given the limited availability of supplemental oxygen and acute medical care resources at our facility, similar medical criteria are applied in consideration of the eligibility of COVID-19 positive patients for admission. Extensive procedures for COVID-19 positive psychiatric units have been described elsewhere (Cheung et al., 2020; Francois et al., preparation).
3. Patient triage
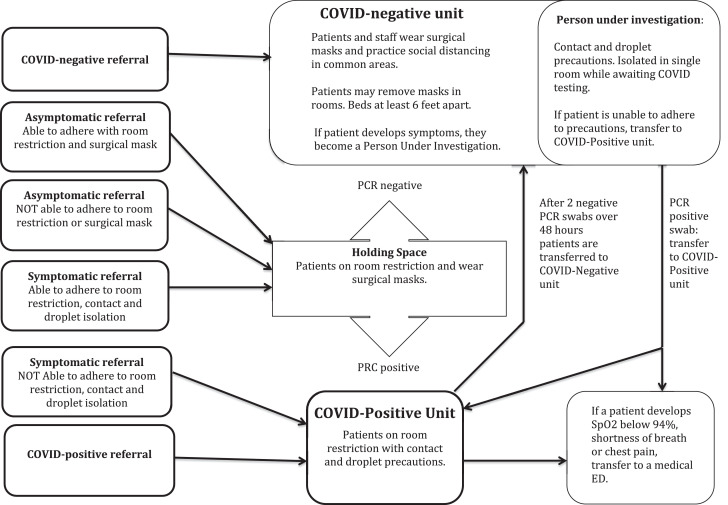
Patients with COVID-19 testing immediately prior to referral are triaged to the COVID-19 Positive or COVID-19 Negative unit (Fig. 1 ). Untested patients are triaged to the Holding Area unless they are symptomatic and their psychiatric symptoms interfere with their ability to adhere to droplet and contact isolation. In this case, they are triaged to the COVID-19 Positive unit pending test results.
Fig. 1.
Algorithm for COVID testing and patient triage in a free-standing psychiatric facility.
4. Discussion
We designed the algorithm presented here with three goals: reducing COVID-19 transmission to patients and staff in a high risk setting, preserving the mandate of creating the safest and least restrictive treatment environment for psychiatric inpatients, and conserving high-demand PPE. The triage decisions represent guidelines, and some variations may apply. For example, access to rapid point of care COVID-19 testing may facilitate and simplify the admission triage process. However, free-standing psychiatric facilities in community settings may be limited by implementation and maintenance requirements of point of care testing, creating a need for clinical triage protocols like the one we describe.
We encountered several challenges developing and implementing this algorithm. At the beginning of the pandemic, PPE and COVID-19 testing were not universally available. Subsequently, rare patients refused COVID-19 testing or had behavioral symptoms that limited adherence to social distancing or the use of surgical masks. However, the vast majority of our patients adapted to procedures described without (or only minimal) difficulty.
5. Conclusions
We present an algorithm for operational implementation of screening, testing, isolation, and treatment of COVID-19 in a free-standing psychiatric facility. A limitation of the current report is that it represents an iterative, rapid institutional response to a novel pathogen and therefore is based on expert consensus from the CDC, the hospital system's Department of Infection Control and Prevention, and the authors’ experiences in an inpatient psychiatric setting. At the time of this writing, our institution has not suffered an outbreak of COVID-19 and that vast majority of COVID-19 patients we have treated contracted the virus prior to admission. We plan to report these results in full in future work.
Although this algorithm was specifically designed for a large free-standing psychiatric facility, it can also be readily adapted to psychiatric units in general medical facilities with emergency departments and medical units or other institutional settings such as nursing homes that treat patients with behavioral symptoms and may be at significant risk of intra-institutional COVID-19 outbreaks.
Author statement
Benjamin Brody participated in early discussions and drafting of the algorithm described and led all clinical activities on a COVID-Negative unit during the months described. He wrote the original draft of the manuscript, created the accompanying figure, and the revised the manuscript.
Sharon Parish led all general medicine activities on the campus described during the months described and participated in the conceptualization of the manuscript. She wrote the sections related to general medical care and participated in the editing of the manuscript.
Dora Kanellopoulos worked on a COVID-Positive unit during the months described and participated in the conceptualization of the article. She wrote parts of the section about the COVID-Positive unit and edited the manuscript.
Mark Russ led all clinical activities on the campus during the months described and lead the effort to create the algorithm described. He also participated in the editing of the manuscript.
Disclosures
None of the authors have any financial relationships to disclose.
Declaration of Competing Interest
None of the authors report any grant support, other external funding, or other conflicts of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113244.
Appendix. Supplementary materials
References
- Shinn A.K., Viron M. Perspectives on the COVID-19 Pandemic and Individuals With Serious Mental Illness. J Clin Psychiatry. 2020 Apr 28;81(3) doi: 10.4088/JCP.20com13412. [DOI] [PubMed] [Google Scholar]
- Li L. Challenges and Priorities in Responding to COVID-19 in Inpatient Psychiatry. Psychiatr Serv. 2020 Apr 23 doi: 10.1176/appi.ps.202000166. [DOI] [PubMed] [Google Scholar]
- Fahed M., Barron G.C., Steffens D.C. and Logistical Considerations of Caring for Older Adults on Inpatient Psychiatry During the COVID-19 Pandemic. Am J Geriatr Psychiatry. 2020 May 5 doi: 10.1016/j.jagp.2020.04.027. S1064-7481(20)30328-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying S., Yang, S. and Fei, J.M. Psychiatry Hospital Management Facing COVID-19: from Medical Staff to Patients Brain Behav Immun. 2020 Apr 10;S0889-1591(20)30455-4. [DOI] [PMC free article] [PubMed]
- Woloshin S., Patel N., Kesselheim A.S. False Negative Tests for SARS-CoV-2 Infection - Challenges and Implications. N Engl J Med. 2020 Jun 5 doi: 10.1056/NEJMp2015897. [DOI] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.H. et al. for the China Medical Treatment Expert Group for COVID-19.Clinical Characteristics of Coronavirus Disease 2019. N Engl J Med. 2020 Apr 30;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- “Precautions to Prevent Transmission of Agents” Centers for Disease Control and prevention. Accessed May 23rd, 2020. https://www.cdc.gov/infectioncontrol/guidelines/isolation/precautions.html.
- Cheung E.H., Strouse T.B., Li L. Planning for a psychiatric COVID-19–positive unit. Clinical Psychiatry News. May 15, 2020 https://www.mdedge.com/psychiatry/article/222331/coronavirus-updates/planning-psychiatric-COVID-19-positive-unit Accessed May 24th, 2020. [Google Scholar]
- Francois, D. Rosenblum, R., Sanchez-Barranco, P. Kanellopoulos, D.COVID-19 Inpatient Psychiatric Unit: challenges and lessons learned. In preparation.
- Kanellopoulos, D., Bueno, C., McGlynn, L., Francois, D., Gerber, S., Rosenblum, L., Runge, M., Sanchez-Barranco, P., Alexopoulos, G.S.Implementation of Telehealth Services for Inpatient Psychiatric COVID-19 positive patients: a Blueprint for Adapting the Milieu. Submitted for publication May 28, 2020. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.