Abstract
Context
Limited access to opioids for patients with cancer has been reported as a potential unintended consequence of recent regulations restricting opioid use and prescribing practices. To our knowledge, there are a limited number of peer-reviewed studies that evaluate the perceived difficulties of the patients with cancer when filling their opioid prescription. To understand these difficulties, we surveyed patients receiving opioids in our outpatient supportive care center (SCC).
Objectives
The primary objective of this study was to evaluate cancer patients' perceptions of overall difficulties when filling their opioid prescription. Secondary objectives included determining associations between patient characteristics and difficulty and comparing difficulty between filling opioid and nonopioid prescriptions.
Methods
Patients with cancer receiving opioids that had been seen two times or more at our SCC were asked to complete a survey. The information collected included patient demographics, clinical characteristics, and patients' experiences filling their opioid prescription.
Results
The patients' median age was 60 years; 54% were female and 69% were white. Forty-four patients (32%) reported that they have experienced difficulty filling their opioid prescription. More than 25% of those 44 patients perceived difficulty from interactions with the pharmacy and/or pharmacist. Forty-six patients (33%) reported more difficulty filling their opioid prescriptions than filling their nonopioid prescriptions.
Conclusion
This study provides evidence that patients with cancer visiting our SCC perceived difficulties obtaining their opioid prescriptions. The results suggest that negative interactions with the pharmacy and/or pharmacist contribute to their perceived difficulty. Additional research is needed to further characterize the contributors of the difficulties patients with cancer face in filling their opioid prescriptions.
Key Words: Analgesics, opioid, prescriptions, cancer pain, opioid epidemic, palliative care, pain management
Key Message
Limited access to opioids for patients with cancer has been reported as a potential unintended consequence of recent regulations restricting opioid use and prescribing practices. After receiving outpatient supportive care, approximately one-third of cancer patients with an opioid prescription perceived having difficulties when filling their opioid prescription.
Introduction
Pain is one of the most frequent and burdensome symptoms among patients with cancer, with prevalence rates of 66% in patients with metastatic disease, 55% in patients during treatment, and 39% in patients after curative treatment.1 Although opioid therapy remains the first line of defense for effective management of cancer-related pain,2 the abuse and misuse of opioids continues to be a growing epidemic in the U.S.3 Subsequently, the Centers for Disease Control and Prevention, released guidelines for physicians to safely prescribe opioids to patients.4 Although these guidelines exclude patients undergoing active cancer treatment or palliative care, recent reports show that an unintended consequence of the systemic and regulatory changes has been limited access to opioids for patients with cancer.5, 6, 7, 8 In a survey conducted by Public Opinion Strategies on behalf of the American Cancer Society Cancer Action Network and the Patient Quality of Life Coalition, cancer patients, survivors, and others with serious illnesses reported having experienced increased difficulties receiving their opioid prescription from 2016 to 2018.9 This limited access to opioids adversely impacts the management of cancer-related pain, as at least one-third of patients with cancer reported that they did not receive adequate medication for the intensity of their pain.10, 11, 12 The under-treatment of cancer pain is associated with other psychosocial and physical symptoms that negatively affect clinical outcomes and the patient's quality of life.9 , 13
Barriers that prevent adequate pain management for patients with cancer have been previously described, including regulatory requirements, racial and socioeconomic disparities, societal attitudes toward pain management (i.e., opioid stigma),14 and parenteral opioid shortages.15, 16, 17 The availability of opioids has been further impacted by the reduction in opioid prescription patterns among oncologists. One study reported a significant decreasing annual trend of opioid use in patients with advanced cancer who received inpatient palliative care (morphine equivalent daily dose of 150 mg/day in 2008 to 83 mg/day in 2014).18 Another study showed that the amount of opioids prescribed to patients with cancer before referral to an outpatient palliative care clinic decreased to 40 mg/day in 2015 from 78 mg/day in 2010.19 Moreover, anecdotal patient reports to our clinic describing difficulties in filling opioid prescriptions make us suspicious that this may be a widespread problem.
Although the impact of the opioid epidemic and the recent regulatory changes on cancer patients' access to their opioid medications has been described,15 , 16 , 18 , 19 there are a limited number of peer-reviewed studies that have evaluated cancer patients' perceived difficulties when filling their opioid prescriptions. Based on the previous limited literature, we hypothesized that after receiving outpatient supportive care, cancer patients perceive difficulties when filling their opioid prescription. Therefore, this pilot study was conducted to determine cancer patients' perceived difficulties when filling their opioid prescription after receiving outpatient supportive care. To understand these difficulties, we conducted a patient survey with questions about the patient's experiences in filling their opioid prescriptions. The patients also answered questions about their experiences filling prescriptions for their other regular (nonopioid) medications. Knowledge and understanding of these perceived difficulties will shed light on the contributors of these issues and allow for implementation of strategies to overcome the difficulties to ensure that patients with cancer are not negatively impacted when obtaining their legitimate opioid prescriptions.
Methods
This survey study was approved by the Institutional Review Board at The University of Texas MD Anderson Cancer Center. Patients were eligible to participate if they were at least of 18 years, had a cancer diagnosis, were receiving opioids prescribed by the MD Anderson supportive care center (SCC), had visited the SCC two previous times for the purpose of opioid pain management, and were able to understand, read, write, and speak English. The survey consisted of 24 questions relating to patients' perceptions of the problems that they encountered when filling their prescriptions for opioids. To our knowledge, there are no validated measurements to use for evaluation of patients' difficulties filling opioid prescriptions. The survey was developed based on a previous study conducted by Public Opinion Strategies on behalf of the American Cancer Society Cancer Action Network and the Patient Quality of Life Coalition,9 and questions used in the survey were refined by input from experts in the field at MD Anderson SCC. The survey was assessed for readability and was pilot-tested on volunteers to ensure that it took less than 10 minutes to complete. Five minutes was the average time to complete the survey. Before administration of the survey, patients' demographic and clinical information were collected, including scores on the Cut-down, Annoyed, Guilty, and Eye-opener questionnaire, opioid prescription history, and cancer diagnosis.
Our primary objective was to evaluate cancer patients' perceptions of overall difficulties when filling their opioid prescription. Overall difficulty was determined by a yes and/or no question on the survey. Our secondary objectives were to determine if associations existed between patient characteristics and patient difficulty filling opioid prescriptions, and to evaluate the patients' perceived difficulties when filling opioid vs. nonopioid prescriptions.
Statistical Analysis
Summary statistics were used to describe the demographic and clinical characteristics of the study population. The association between patients' perception about difficulty filling opioids and their characteristics was evaluated by Wilcoxon rank sum test and Chi-squared (Fisher's exact) test for continuous and categorical variables, respectively. Estimates of odds ratio along with 95% CI were calculated by fitting univariate logistic models.
Results
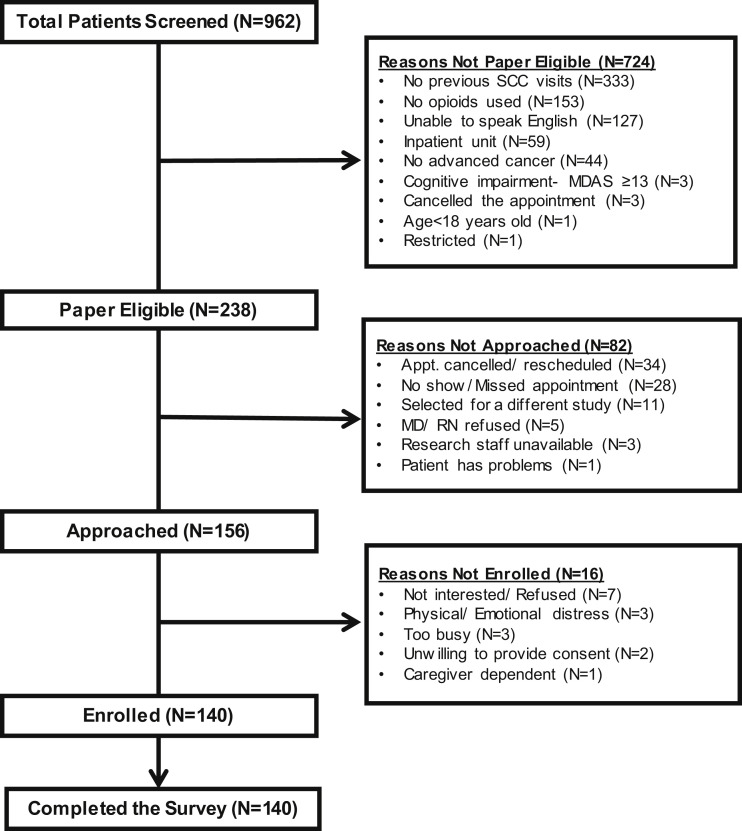
A total of 962 patients with advanced cancer presenting to the MD Anderson SCC were screened between April and September 2019. Of the 238 patients who were eligible, 156 patients were approached and 140 patients completed the survey (Fig. 1 ). The reasons for not approaching 82 of the 238 eligible patients are listed in Fig. 1. One patient who completed the survey only received prescriptions via mail order, so that patient's responses were removed from the analysis. Table 1 lists the demographic and clinical characteristics of 139 patients who completed the survey. The median age (interquartile range) was 60 (20, 90) years, and 55% of the patients were female.
Fig. 1.
Consolidated Standards of Reporting Trials diagram of patients' flow throughout the study. SCC = supportive care center; MDAS = Memorial Delirium Assessment Scale; MD = medical doctor; RN = registered nurse.
Table 1.
Patient Characteristics
| Variable | Total, n (%) | Overall, Has the Patient Had Difficulties When Filling Their Opioid Prescription? n (%)a |
|
|---|---|---|---|
| Yes | No | ||
| All patients | 139 (100) | 44 (32) | 95 (68) |
| Median age (range) | 60 (20, 90) | 59 (20, 81) | 62 (30, 90) |
| Female sex | 76 (55) | 25 (57) | 51 (54) |
| Race/ethnicity | |||
| White | 96 (69) | 33 (75) | 63 (66) |
| African American | 28 (20) | 7 (16) | 21 (22) |
| Hispanic | 13 (10) | 2 (4.5) | 11 (12) |
| Asian/Pacific Islander | 2 (1) | 2 (4.5) | 0 |
| Marital status | |||
| Married/significant other | 92 (66) | 25 (57) | 67 (71) |
| Single | 18 (13) | 8 (18) | 10 (11) |
| Divorced | 16 (12) | 7 (16) | 9 (9) |
| Widowed/separated | 13 (9) | 4 (9) | 9 (9) |
| Highest level of education completed | |||
| Less than high school/tech school | 12 (9) | 4 (9) | 8 (8) |
| High school/tech school | 30 (22) | 6 (14) | 24 (25) |
| Incomplete college or junior college | 38 (27) | 12 (27) | 26 (27) |
| Complete college | 39 (28) | 16 (36) | 23 (24) |
| Incomplete masters/doctoral degree | 3 (2) | 0 | 3 (3) |
| Complete masters/doctoral degree | 17 (12) | 6 (14) | 11 (12) |
| Annual household income | |||
| <$40,000 | 38 (28) | 13 (30) | 25 (27) |
| $40,000–$80,000 | 33 (24) | 11 (24) | 22 (23) |
| >$80,000 | 36 (26) | 13 (30) | 23 (24) |
| Prefer not to say | 31 (22) | 7 (16) | 25 (26) |
| Cancer diagnosis | |||
| Breast | 21 (15) | 9 (21) | 12 (13) |
| Gastrointestinal | 23 (17) | 8 (18) | 15 (16) |
| Head and neck | 18 (13) | 6 (14) | 12 (13) |
| Genitourinary | 20 (14) | 5 (11) | 15 (16) |
| Gynecologic | 13 (9) | 5 (11) | 8 (8) |
| Thoracic | 23 (17) | 5 (11) | 18 (19) |
| Sarcoma | 9 (7) | 3 (7) | 6 (6) |
| Otherb | 12 (8) | 3 (7) | 9 (9) |
| Current cancer stage | |||
| Locally advanced | 38 (27) | 10 (23) | 28 (30) |
| Metastatic | 101 (73) | 34 (77) | 67 (70) |
| CAGE-AID positive | 22 (16) | 8 (18) | 14 (15) |
| First given opioids (months) | |||
| Less than three | 11 (8) | 5 (11) | 6 (6) |
| Three to six | 22 (16) | 5 (11) | 17 (18) |
| Six to 12 | 42 (30) | 12 (27) | 30 (32) |
| >12 | 64 (46) | 22 (50) | 42 (44) |
| Median MEDD (IQR) | 120 (80, 185) | 151 (82, 242) | 120 (80, 180) |
CAGE-AID = Cut Down, Annoyed, Guilty, Eye-opener Adapted to Include Drugs questionnaire; MEDD = morphine equivalent daily dose; IQR = interquartile range.
Number and percentage of individuals reported are those who answered always/very often/sometimes to the stated variable.
Other diagnoses include skin, lymphoma, myeloma, and leukemia.
Table 2 reports the perceived experiences of patients when filling their opioid prescription. Overall, 44 patients (32%) reported that they have experienced difficulty filling their opioid prescription. Of those 44 patients, 12 (27%) said that the pharmacist(s) remembers them each time, which is significantly lower than the 55% of patients (53 of 96) who have not experienced difficulty and also said that the pharmacist remembers them (P < 0.005). Table 3 reports the attitudes and beliefs of patients according to difficulty filling their opioid prescription. Those who reported difficulty filling their opioid prescription were more likely to feel emotional distress when going to the pharmacy (12 of 44 [27%] vs. 3 of 95 [3%]; P < 0.001), that the difficulty was caused by the pharmacy and/or pharmacist (12 of 44 [27%] vs. 1 of 95 [1%]; P < 0.001), and that the pharmacist makes them feel ashamed (6 of 44 [14%] vs. 0 of 95 [0%]; P < 0.001).
Table 2.
Perceived Difficulties Experienced by Patients When Filling Opioid Prescriptions
| Variable | Total, n (%)a | Overall, Has the Patient Had Difficulties When Filling Their Opioid Prescription? n (%)a |
P | |
|---|---|---|---|---|
| Yes | No | |||
| All patients | 139 (100) | 44 (32) | 95 (68) | |
| Do you regularly receive your opioid prescription from the same pharmacist(s)?b | 115 (83) | 33 (75) | 82 (85) | 0.072 |
| Does the pharmacist seem to remember you each time you visit the pharmacy?b | 65 (48) | 12 (27) | 53 (55) | 0.005 |
| How often have you been unable to get your opioid prescription? | 5 (4) | 4 (9) | 1 (1) | 0.035 |
| How often have you been unable to get your opioid prescription because the pharmacy did not have the particular drug in stock? | 7 (5) | 4 (9) | 3 (3) | 0.207 |
| How often have you been unable to get your opioid prescription because your insurance would not cover it? | 2 (1) | 2 (5) | 0 (0) | 0.098 |
| How often has a pharmacist asked you about why you needed your opioid prescription? | 4 (3) | 3 (7) | 1 (1) | 0.094 |
| How often has your insurance company limited you to only one pharmacy to go to for filling your opioid prescription? | 3 (2) | 0 (0) | 3 (3) | 0.551 |
| How often has your insurance company reduced the number of times you can refill your opioid prescription? | 3 (20 | 3 (7) | 0 (0) | 0.031 |
| How often has your insurance company reduced the number of pills in your opioid prescription? | 3 (2) | 3 (7) | 0 (0) | 0.032 |
| How often has the pharmacist given you only part of your opioid prescription (e.g., for seven days instead of the 30 days for which the prescription was written)? | 3 (2) | 3 (7) | 0 (0) | 0.030 |
| How often have you paid a high copay (more than $50) for your opioid prescription? | 10 (7) | 4 (9) | 6 (63) | 0.726 |
Number and percentage of individuals reported are those who answered always/very often/sometimes to the stated variable.
Number and percentage of individuals reported are those who answered yes to the stated variable.
Table 3.
Attitudes and Beliefs of Patients Who Report Difficulty Filling Their Opioid Prescription
| Variable | Total, n (%)a | Overall, Has Patient Had Difficulties When Filling Their Opioid Prescription? n (%)a |
P | |
|---|---|---|---|---|
| Yes | No | |||
| All patients | 139 (100) | 44 (32) | 95 (68) | |
| I feel financial distress when filling my opioid prescription | 18 (13) | 6 (14) | 12 (13) | 1.00 |
| I feel that the pharmacy/pharmacist makes the process of filling my opioid prescription difficult | 13 (9) | 12 (27) | 1 (1) | <0.001 |
| I feel emotional distress when I go to the pharmacy to fill my opioid prescription | 15 (11) | 12 (27) | 3 (3) | <0.001 |
| The pharmacist makes me feel ashamed for having an opioid prescription | 6 (4) | 6 (14) | 0 (0) | <0.001 |
| I feel more comfortable filling my opioid prescription at a pharmacy in a different neighborhood than where I live | 11 (8) | 5 (11) | 6 (6) | 0.324 |
| Overall, it is more difficult to fill my opioid prescription than to fill my other nonopioid prescription medicine(s) | 46 (33) | 30 (68) | 16 (17) | <0.001 |
| I feel more financial distress when filling my opioid prescription than when filling my other nonopioid prescription medicine(s) | 19 (14) | 11 (25) | 8 (8) | 0.015 |
| I feel that the pharmacy/pharmacist makes the process more complicated when I fill my opioid prescription than when I fill my other nonopioid prescription medicine(s) | 20 (14) | 17 (39) | 3 (3) | <0.001 |
| I feel more emotional distress at the pharmacy when I pick up my opioid prescription than when I pick up my other nonopioid prescription medicine(s) | 9 (7) | 7 (16) | 2 (2) | 0.005 |
| The pharmacist treats me differently when I pick up my opioid prescription than when I pick up my other nonopioid prescription medicine(s) | 7 (5) | 5 (11) | 2 (2) | 0.033 |
Number and percentage of individuals reported are those who strongly agree/agree with the stated variable.
Difficulty filling opioid prescriptions as compared with nonopioid prescriptions was reported more frequently among the 44 patients who perceived overall difficulty filling their opioid prescription (30 of 44 [68%] vs. 16 of 95 [17%]; P < 0.001). We asked patients to report the most common reason they had difficulty filling their opioid prescription vs. their nonopioid prescription. Consistent with patients with difficulty indicating the pharmacist as the reason for their difficulty, 17 of 44 patients (39%) also identified the pharmacy and/or pharmacist as the most common reason. The other most common reasons for difficulty filling their opioid vs. nonopioid prescriptions included financial distress (11 patients; 25%) and emotional distress (7 patients; 16%) when picking up their opioid prescription. The mean morphine equivalent daily dose was statistically significantly greater in patients who reported more difficulty filling their opioid prescription than their nonopioid prescription (217 mg/day vs. 137 mg/day; P < 0.001). There was no association between reported difficulty and the patients' demographic characteristics.
Discussion
The results of this pilot study show that patients with cancer who are on opioid therapy to manage their pain have perceived having difficulties when filling their opioid prescriptions. Importantly, patients who reported difficulties were able to identify barriers related to psychological difficulties and the pharmacist's attitude toward them. The findings also show that patients perceived that it was more difficult to fill opioid prescriptions compared with nonopioid prescriptions. Overall, these results provide preliminary data on cancer patients' perceptions of the difficulties encountered when trying to get their opioid prescription after visiting an outpatient SCC.
Our results are similar to another study conducted in adult cancer outpatients at a supportive care clinic that reports opioid stigma was endorsed by 59 of 97 (61%) patients who were prescribed opioids.20 When queried about specific aspects of opioid stigma that they experienced, 21 of 97 (22%) patients identified trouble filling prescriptions and 14 of 97 (14%) patients reported difficulty getting prescriptions.20 Our findings further suggest that the reason for difficulty in obtaining opioid prescriptions stems from emotional distress, most likely experienced from the interaction of the patient with the pharmacist when picking up their medication. Unlike other studies that report socioeconomic21 and racial22, 23, 24 disparities as a barrier to opioid access in general patient populations, this study did not show an association between patients' racial demographics and difficulty obtaining opioids. One reason for this could be that most patients who completed the survey were white (69%). However, a large percentage of the patients who reported difficulty were white (75%), suggesting that limited opioid access may affect people across various racial groups. More research is needed to fully characterize the patient demographics associated with difficulty getting opioid prescriptions in the adult cancer population.
We were surprised to find that patients did not perceive having logistical difficulty, such as restrictions from the insurance company, when filling their opioid prescription. Although these challenges have been reported previously by others, it is possible that by the time this study was carried out, the opioid access difficulties originating from prior authorizations of insurance companies had been mostly resolved. Another possible explanation is that many patients might not understand that the barrier might stem from insurance issues and therefore ascribe their difficulty to the pharmacy and/or pharmacist. Nonetheless, it is possible that the current coronavirus disease 2019 (COVID-19) pandemic may cause new logistical difficulties, as the medical product chains are impacted by shortages in medications and patients across diagnoses are facing increasing difficulties seeking medical care;25 this makes it even more crucial that patients with cancer have access to their opioid prescriptions.
Some limitations of this study include its small sample size and the lack of a validated tool to assess patients' perceptions of the difficulties encountered when filling their opioid prescription. Although patients' demographic and clinical information was obtained, the geographic location of the pharmacy where the patient had difficulties was not collected because of concerns over patient privacy and zip code as potentially identifying information; thus, we were unable to assess if certain geographic regions were associated with difficulty filling opioid prescriptions. Because reports suggest that geographic factors could play a role in opioid access for patients,26 future studies overcoming privacy concerns around patient geography could prove extremely insightful. Another limitation is that the results might not be generalizable to patients receiving cancer care at other institutions and hospitals because this study was carried out at a single institution: a comprehensive cancer center with its own outpatient pharmacy. Moreover, the patients in this study were seen twice by our supportive care clinicians, who take extra care to ensure that patients have access to opioids for their pain by prescribing opioids that are less expensive. This scenario could be different in other clinics where financial concerns are not considered or in clinics that are not as experienced with strategies to overcome access barriers as in the SCC, suggesting that patients' financial distress could be underrepresented. Finally, our results may not be generalizable to the overall U.S. cancer patient population, as the opioid epidemic has been characterized as less severe in Texas compared with other regions of the country.27
Despite the limitations of the study, these findings suggest that negative interactions with pharmacists contribute to cancer patients' perceived difficulties when obtaining their legitimate opioid medications. These interactions that inflict shame and emotional distress on the patient with cancer can lead to negative outcomes via avoidance of pharmacies and health care providers, poor adherence to pain medication, and undertreatment of pain.20 These findings further suggest opportunities to educate pharmacists on the experience of patients and their potential distress when filling their legitimate opioid prescriptions, along with educational opportunities to provide to patients in terms of their safe use of opioids and their rights when filling prescriptions. A study in our SCC showed that education focused on opioid safety for patients with advanced cancer led to improved patient-reported safe opioid storage, usage, and disposal.28 Providing this type of opioid management education for patients at the time of prescribing (by the physician) and at the time of dispensing (by the pharmacist) could reduce the patient's emotional distress by alleviating their concerns about using opioids as well as decreasing potential complications around filling the prescription from the pharmacist. Evaluating the use of educational material for patients and pharmacists when receiving and filling an opioid prescription would therefore be a rich avenue of future research.
The tantalizing results of this study suggest that additional research could uncover other contributors of perceived difficulty to accessing opioids in the context of the cancer patient population. To accomplish this effort, studies should be carried out to investigate the types of pharmacies where these difficulties are taking place (i.e., community pharmacies vs. hospital pharmacies). Importantly, additional studies are needed to determine the sociodemographic and clinical characteristics of patients who perceive difficulties when filling their opioid prescriptions.
Conclusions
Evidence from this study shows that patients with cancer perceived difficulties when filling their opioid prescriptions, and the results suggest that negative interactions with the pharmacy and/or pharmacist contribute to their perceived difficulty. To ensure that patients with cancer can access their legitimate opioid prescriptions without negative impacts, including shame and emotional distress, further research efforts are needed to fully characterize these difficulties and to implement strategies that address their origins.
Disclosures and Acknowledgments
This research was supported in part by a National Institutes of Health Cancer Center support grant (P30CA016672) for the Biostatistics Resource Group and a National Institutes of Health Clinical and Translational Science Award (1UL1TR003167-01). The authors are grateful to all respondents who completed the surveys. The authors also thank Aimee Anderson, PhD, for her editorial assistance and Nwabunie Nwana for her assistance with the survey. The authors declare no conflicts of interest.
References
- 1.van den Beuken-van Everdingen M.H., Hochstenbach L.M., Joosten E.A., Tjan-Heijnen V.C., Janssen D.J. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51:1070–1090.e9. doi: 10.1016/j.jpainsymman.2015.12.340. [DOI] [PubMed] [Google Scholar]
- 2.Koyyalagunta D., Bruera E., Solanki D.R. A systematic review of randomized trials on the effectiveness of opioids for cancer pain. Pain Physician. 2012;15:ES39–ES58. [PubMed] [Google Scholar]
- 3.Scholl L., Seth P., Kariisa M., Wilson N., Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67:1419–1427. doi: 10.15585/mmwr.mm675152e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dowell D., Haegerich T.M., Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315:1624–1645. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Page R., Blanchard E. Opioids and cancer pain: patients' needs and access challenges. J Oncol Pract. 2019;15:229–231. doi: 10.1200/JOP.19.00081. [DOI] [PubMed] [Google Scholar]
- 6.Cooper A.F. Opioids and cancer pain: patient needs and challenges to treatment from the perspective of a survivor and patient advocate. J Oncol Pract. 2019;15:226–228. doi: 10.1200/JOP.19.00079. [DOI] [PubMed] [Google Scholar]
- 7.Paice J.A. A delicate balance: risks vs benefits of opioids in cancer pain. Pain. 2020;161:459–460. doi: 10.1097/j.pain.0000000000001773. [DOI] [PubMed] [Google Scholar]
- 8.Paice J.A. Under pressure: the tension between access and abuse of opioids in cancer pain management. J Oncol Pract. 2017;13:595–596. doi: 10.1200/JOP.2017.026120. [DOI] [PubMed] [Google Scholar]
- 9.American Cancer Society Cancer Action Network and the Patient Quality of Life Coalition New data: some measures meant to address opioid abuse are having adverse impact on access to legitimate pain care for patients. 2018. https://www.fightcancer.org/releases/new-data-some-measures-meant-address-opioid-abuse-are-having-adverse-impact-access Available from.
- 10.Deandrea S., Montanari M., Moja L., Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19:1985–1991. doi: 10.1093/annonc/mdn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greco M.T., Roberto A., Corli O. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32:4149–4154. doi: 10.1200/JCO.2014.56.0383. [DOI] [PubMed] [Google Scholar]
- 12.Paice J.A., Von Roenn J.H. Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol. 2014;32:1721–1726. doi: 10.1200/JCO.2013.52.5196. [DOI] [PubMed] [Google Scholar]
- 13.Zaza C., Baine N. Cancer pain and psychosocial factors: a critical review of the literature. J Pain Symptom Manage. 2002;24:526–542. doi: 10.1016/s0885-3924(02)00497-9. [DOI] [PubMed] [Google Scholar]
- 14.Scarborough B.M., Smith C.B. Optimal pain management for patients with cancer in the modern era. CA Cancer J Clin. 2018;68:182–196. doi: 10.3322/caac.21453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hollingsworth H., Herndon C. The parenteral opioid shortage: causes and solutions. J Opioid Manag. 2018;14:81–82. doi: 10.5055/jom.2018.0434. [DOI] [PubMed] [Google Scholar]
- 16.Bruera E. Parenteral opioid shortage—treating pain during the opioid-overdose epidemic. N Engl J Med. 2018;379:601–603. doi: 10.1056/NEJMp1807117. [DOI] [PubMed] [Google Scholar]
- 17.Paice J.A. Cancer pain management and the opioid crisis in America: how to preserve hard-earned gains in improving the quality of cancer pain management. Cancer. 2018;124:2491–2497. doi: 10.1002/cncr.31303. [DOI] [PubMed] [Google Scholar]
- 18.Yennurajalingam S., Lu Z., Reddy S.K. Patterns of opioid prescription, use, and costs among patients with advanced cancer and inpatient palliative care between 2008 and 2014. J Oncol Pract. 2019;15:e74–e83. doi: 10.1200/JOP.18.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haider A., Zhukovsky D.S., Meng Y.C. Opioid prescription trends among patients with cancer referred to outpatient palliative care over a 6-year period. J Oncol Pract. 2017;13:e972–e981. doi: 10.1200/JOP.2017.024901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bulls H.W., Hoogland A.I., Craig D. Cancer and opioids: patient experiences with stigma (COPES)—a pilot study. J Pain Symptom Manage. 2019;57:816–819. doi: 10.1016/j.jpainsymman.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joynt M., Train M.K., Robbins B.W. The impact of neighborhood socioeconomic status and race on the prescribing of opioids in emergency departments throughout the United States. J Gen Intern Med. 2013;28:1604–1610. doi: 10.1007/s11606-013-2516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cintron A., Morrison R.S. Pain and ethnicity in the United States: a systematic review. J Palliat Med. 2006;9:1454–1473. doi: 10.1089/jpm.2006.9.1454. [DOI] [PubMed] [Google Scholar]
- 23.Anderson K.O., Mendoza T.R., Valero V. Minority cancer patients and their providers: pain management attitudes and practice. Cancer. 2000;88:1929–1938. [PubMed] [Google Scholar]
- 24.Dickason R.M., Chauhan V., Mor A. Racial differences in opiate administration for pain relief at an academic emergency department. West J Emerg Med. 2015;16:372–380. doi: 10.5811/westjem.2015.3.23893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hahn S.M. U.S. Food and Drug Administration. Coronavirus (COVID-19) supply chain update. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-supply-chain-update Available from.
- 26.Jefferson K., Quest T., Yeager K.A. Factors associated with black cancer patients' ability to obtain their opioid prescriptions at the pharmacy. J Palliat Med. 2019;22:1143–1148. doi: 10.1089/jpm.2018.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson N., Kariisa M., Seth P., Smith H., Davis N.L. Drug and opioid-involved overdose deaths—United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69:290–297. doi: 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de la Cruz M., Reddy A., Balankari V. The impact of an educational program on patient practices for safe use, storage, and disposal of opioids at a comprehensive cancer center. Oncologist. 2017;22:115–121. doi: 10.1634/theoncologist.2016-0266. [DOI] [PMC free article] [PubMed] [Google Scholar]