Abstract
The world is facing one of its worst public health crises in modern history. Coronavirus 2019 (COVID-19) has shown how fragile our global preparedness for infectious diseases is. The world is a small-connected globe with short travel time between its remote parts. COVID-19 has spread globally and swiftly with major impacts on health, economy, and quality of life of communities. At this point in the time, April 9, 2020, >1,500,000 patients have been infected and >88,000 patients have died worldwide within the last 3 months. The status is evolving and the costly lessons learned over time are increasing. These lessons are global as this virus is. They involve different domains of health sciences including virology, public health, clinical, critical care, and disaster management. This review addresses our current knowledge of COVID-19 pandemic from the basic virology and transmission, through prevention, infection control, clinical management, and finally disaster management including the recovery period. This review has a multidisciplinary approach, which is needed at this time. After this difficult period passes, we have to carry the lessons we learned for the future so that we can be better prepared. One thing that has clearly emerged from this ongoing crisis is that infectious diseases have no borders and we have to work together, using the one world, one health approach, if we are to minimize the enormous impact such pandemics can cause.
Keywords: Coronavirus, coronavirus 2019, critical care, disaster, emergency, epidemiology, infection control, prevention
Introduction
Emerging and re-emerging viral diseases are not new. Indeed, in the last 30 years alone, we have seen dozens of outbreaks. Notable examples include the outbreak of H5N1 bird flu in 1997, severe acute respiratory syndrome (SARS) in 2002, the H1N1 swine flu pandemic in 2009, Middle East respiratory syndrome (MERS) in 2012, Ebola virus in 2014, and then the Zika virus in 2015.[1,2] Thus, if emerging and re-emerging viral infections are a common occurrence, why do we feel so threatened when a new viral disease emerges? History tells us that some of these new viral diseases, specifically those spread via the respiratory route, can have devastating impact on human health and healthcare systems. Take the example of the 1918 influenza pandemic, famously known as the “Spanish flu.” It is estimated that this outbreak killed between 17 and 50 million people worldwide.[3,4] Although the case mortality rate with this virus was estimated to be only 3%–5%, the virus was highly infectious and infected more than a third of the world population.[3] Then, we had the 1957 Asian flu, followed 10 years later by the 1968 Hong Kong flu, each of which caused more than a million deaths.[5] With this track record, it is not surprising that there is so much public concern surrounding the novel coronavirus outbreak.
The Initial Outbreak
The current pandemic coronavirus disease (coronavirus 2019 [COVID-19]) was first reported to the WHO by the Chinese authorities on December 31, 2019.[6] The initial cluster of cases was linked to a wholesale food market where both live and dead animals were sold. These types of markets are common in many parts of China, and on several occasions, they have been identified as sources of transmission of zoonotic viruses.[7] In the current outbreak, patients presented with symptoms of lower respiratory tract infection, but laboratory tests for all common causes returned negative, except for real-time reverse transcription polymerase chain reaction (RT-PCR) assay targeting a conserved region of the RNA-dependent RNA polymerase gene of coronaviruses (CoV). This enzyme is essential for the replication of these viruses. Subsequent primary cell culture, electron microscopy, and genomic sequencing studies identified the causative agent of COVID-19 to be a new member of the β-coronavirus family.[6]
The Coronavirus 2019 Virus
CoVs are a large family of enveloped RNA viruses that infect a variety of wild and domestic animals, including bats, birds, cats, and camels. The COVID-19 virus has 88% genome identity to a bat-derived coronavirus from which it is believed to have evolved[8] and 79% homology to SARS-CoV-1, but only about 50% similar to MERS-CoV.[9] Based on its close similarity to SARS-CoV-1, the International Committee on Taxonomy of Viruses named the new virus SARS-CoV-2.
The human coronavirus family consists of seven members which infect humans. Four of these (229E, OC43, NL63, and HKU1) typically infect the upper respiratory tract and cause common cold. By contrast, SARS-CoV-1 and MERS-CoV can frequently cause infection of the lower respiratory tract, leading to severe disease.[10,11] The main mode of transmission of CoV is via respiratory droplets or by direct/indirect contact with contaminated secretions [Table 1]. The virus particles can remain infectious on inanimate objects from hours to several days.[12] Like other CoV, the primary cellular target of COVID-19 virus is cells of the respiratory tract. Infection is mediated by the binding of the viral envelop spike protein with the cell surface receptor, angiotensin-converting enzyme 2.[9] Interestingly, this is the same receptor that SARS-CoV uses for its entry into its target cells. Although SARS-CoV-2 is of animal origin, the virus has clearly adapted to its new human host. A recent study analyzing the viral genome of over 100 cases indicated that the virus has mutated from the original S to the new L stain.[13] The later strain was suggested to be more aggressive. Although this report has yet to be verified, it is not surprising, since RNA viruses tend to be less stable and typically have a much higher mutation rate compared to DNA viruses. Whether the mutations leading to the evolution of the two stains are associated with differing disease severity is not known. In spite of the unprecedented speed with which new data are being published, much still remains regarding the biology, pathogenesis, and the treatment strategies for this new virus.
Table 1.
Comparison of some of the features of severe acute respiratory syndrome-coronavirus disease-1, Middle East respiratory syndrome-coronaviruses, and severe acute respiratory syndrome-CoV-2 (As of 9th April 2020)
| SARS-CoV-1 | MERS-CoV | SARS-CoV-2* | |
|---|---|---|---|
| Year/place of initial outbreak | 2002/China | 2012/KSA | 2019/China |
| Suspected natural host | Bats | Bats | Bats |
| Intermediate host | Civet cats? | Camels | ? |
| Number of cases (period) | 8096 (November 02-July-03) | 2499 (July-12-December-19) | 1,521,809 (January-20-April 9) |
| CMR (%) | 9.6 | 35 | 4.1 |
| Mode of transmission | Droplets, direct/indirect | Droplets, direct/indirect | Droplets, direct/indirect |
| Incubation period, days (range) | 2-7 (2-21) | 2-7 (2-14) | 2-7 (2-14) |
| Super spreaders | Yes | Yes | Yes |
| Reproduction number (R0) | 3.0 | 0.3-0.8 | 1.4-6.5 |
| Genome size (kb) | 29.7 | 30.1 | 29.8 |
| Main cellular target | Respiratory epithelium | Respiratory epithelium | Respiratory epithelium |
| Cell receptor | ACE2 | CD26/DPP4 | ACE2 |
SARS: Severe acute respiratory syndrome, MERS: Middle East respiratory syndrome, COV: Coronaviruses, CMR: Case mortality rate, ACE2: Angiotensin-converting enzyme 2
Coronavirus 2019 Pandemic
Coronavirus 2019 infection has spread swiftly starting from china through the whole globe. The WHO declared the outbreak of COVID-19 as a public health emergency of international concern and issued temporary recommendations under the International Health Regulations.[14] In March 11, 2020, the WHO has declared COVID-19 as pandemic.[15] However, in March 13, 2020, it announced that “Europe has now become the epicenter of the pandemic.”[16] By April 9, 2020, >1,500,000 patients were infected and >88,000 patients died. Figure 1 shows COVID-19 cases worldwide, up to March 23, 2020 [Figure 1]. The early stages of the COVID-19 outbreak in China focused mainly on the clinical management, with minimum emphasis on the public health interventions which should aim at understanding the spectrum, severity, components (symptomatic and asymptomatic), and transmission of the virus.[17]
Figure 1.
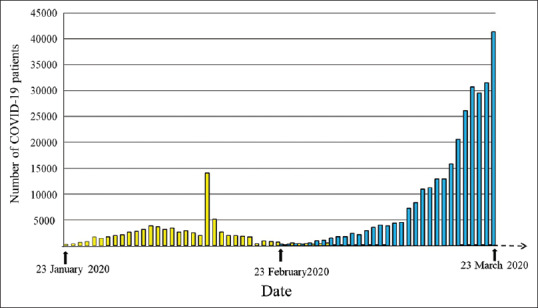
Daily number of coronavirus 2019 patients in china (yellow bars) and rest of the world (blue bars) during the period of January 23, 2020, till March 23, 2020, crude data were extracted from https://www.worldometers. info/coronavirus/(accessed on 24th March 2020)
Control and Preventive Measures
Asymptomatic carriers are the potential source for COVID-19 infection. The infection can be transmitted during an incubation period in which the symptoms can be short and nonspecific including fever, cough, and difficulty in breathing.[18] The incubation period is between 2 and 14 days.[19] COVID-19 can be transmitted via droplets and fomites through unprotected person-to-person close contact (within about 2 m). This virus can spread through respiratory droplets when an infected person coughs or sneezes.[14] A fecal–oral transmission was suggested in children having COVID-19 in whom RT-PCR rectal swabs were positive after having negative RT-PCR results of the nasopharyngeal swabs indicating gastrointestinal tract viral shedding.[20]
Because there is no cure for the COVID-19, and a vaccine has not yet been developed, supportive care and prevention of complications are the main pillars of current management. Therefore, emphasis should be on control and prevention of the disease spread within the community, especially for those who are most vulnerable. Members of a community should limit exposure by avoiding large public gatherings and close contacts. Furthermore, they should practice good hygiene by washing their hands for a minimum of 20 s, covering their mouth and nose when sneezing and coughing, and disinfecting surface areas. Those who are at high risk (with comorbidities or immune suppression) are advised to isolate themselves at home.[18] Health-care providers should strictly follow the infection control measures in their health-care settings. They should regularly and properly wash their hands when moving between patients and should use proper personal protective equipment (PPE) when managing infected patients. Furthermore, early laboratory confirmation of infected cases, their isolation and quarantine, and contact tracing is pivotal for infection control. The public health professional's role is to identify close contact of symptomatic patient as early as possible for isolation and treatment as well as prompt referral to health-care facilities for laboratory proper diagnostic tests. The high-risk contact person is defined as “a person who has close contact with a symptomatic person living in the same household,” whereas a low-risk casual contact is defined as “a person staying in a closed environment for <15 min or at a distance of >2 m.”[18]
Clinical Presentation
In a study with >44 thousand patients from China having COVID-19, majority have mild illness (81%). Severe, critical cases, and death were in 14%, 5%, and 2.3%, respectively. The overall case-fatality rate (CFR) from different parts of the world ranged between 0.25% and 3.0%.[21,22] Infection affects men more than women. Almost 90% of the patients have an age between 30 and 79 years. Patients older than 80 years have a CFR of 14.8%, whereas those having an age of 70–79 years have a CFR of 8%.[21] Severe COVID-19 is more common in those having comorbidities such as diabetes, cardiac disease, hypertension, and chronic obstructive airway disease. The most common clinical features include fever, cough, shortness of breath, and myalgia. A small subset of patients had gastrointestinal complaints such as nausea and diarrhea.[23] Various hematologic abnormalities were reported in patients with COVID-19, including lymphocytopenia (83.2%), thrombocytopenia (36.2%), and leukopenia (33.7%). These findings were more prominent in severe cases.[23] Cytokines (interleukin 2 [IL-2], IL-10, and tumor necrosis factor-alpha) were reported to be higher in the plasma of intensive care unit (ICU) patients who are infected with COVID-19, suggesting a picture of cytokine storm.[24] Predictors of death in COVID-19 patients included old age, comorbidities, secondary infections, and elevated blood inflammatory markers.[25]
Pregnant women seem to have a similar clinical course to nonpregnant women. It is unlikely to have a mother fetal transmission route based on negative neonatal throat swabs and samples from amniotic fluid, placenta, cord blood, and breast milk.[26,27,28] All children including neonates and infants are susceptible to COVID-19, which is usually milder than adults. More than 90% are asymptomatic or have mild or moderate disease.[29] Common pediatric clinical presentations include cough (48.5%), pharyngeal erythema (46.2%), and fever (41.5%). Hypoxia was present only in 2.3% of patients (oxygen saturation below 92%). Mechanical ventilation is rarely needed in children.[30]
Diagnosis
The diagnosis of COVID-19 depends on the history of exposure, the clinical presentation, imaging, and the RT-PCR results, which are the gold standard for diagnosis.[31] RT-PCR has certain limitations. It may be initially negative for a period of 3–8 days before turning into positive.[32,33] Patients can be infectious during this period. Furthermore, it depends on the availability. Clinicians have to make important decisions when this test is not available.
Blood investigations that can be of help include an elevated CRP, lymphocytopenia, and normal or low white blood cell count.[34] Those patients who have a history of exposure without fever and have normal lymphocytes and CRP can be advised to go home and self-isolate themselves.[34]
Computed tomography (CT) scan has turned out to be very useful as a scanning tool detecting the early sign of COVID infection.[34] The two main radiological signs in COVID-19 include the ground-glass opacity (GGO) and consolidations.[32,35] These lesions are located mainly at the subpleural region at the periphery of the lung. GGO is an area of increased attenuation with hazy margin and does not affect the vascular or bronchial margin [Figure 2]. Consolidation which is an area of opacification can be within the GGO, can surround the GCO (reversed halo sign), or can be alone [Figure 3]. Han et al.[35] have shown in a study of 108 patients of COVID-19 disease that 60% had GGO, 41% had consolidation besides the GGO, vascular dilation was present in 80%, and the bronchogram sign was present in 48%. These findings are very sensitive as only 5 (3%) out of 167 patients who had these radiological findings turned out to be negative.[33] Similarly, the most common radiological finding in children having COVID-19 pneumonia is the bilateral ground-glass opacities.[30]
Figure 2.
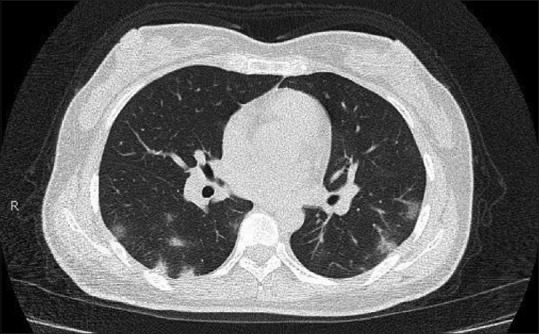
Axial noncontrast image of a computed tomography of the chest performed 5 days after the onset of symptoms shows patchy, peripheral predominantly nodular areas of consolidation and ground-glass opacities. Zhang W, Shi H. Evolving COVID-19 Pneumonia. Radiology Case Collection doi: 10.1148/ cases. 20201558. Published online March 17, 2020. ©Radiological Society of North America (Reproduced with permission from the Radiological Society of North America)
Figure 3.
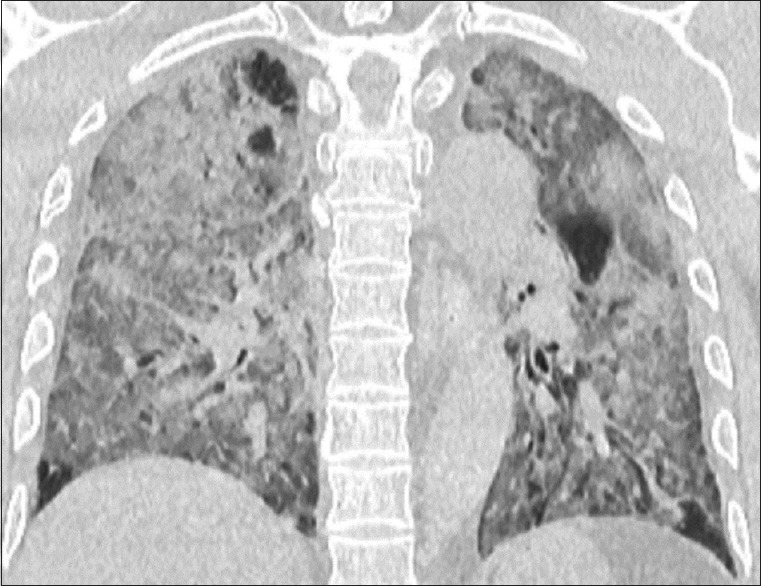
Coronal reformatted noncontrast CT images show diffuse ground-glass opacities and consolidation with areas of secondary lobular sparing. Gui S, Pan F, Yang L. Severe Coronavirus Disease 2019 (COVID-19). Radiology Case Collection doi: 10.1148/cases. 20201281. Published online February 20, 2020. ©Radiological Society of North America (Reproduced with permission from the Radiological Society of North America)
Critical Care Management
Management of COVID-19 critically ill patients is an important challenging part of the response to this pandemic. Critical care physicians have to coordinate different medical teams, contain the infection, treat the patients, and protect themselves and their staff. Out of 710 patients with COVD-19 treated in China, 52 (7.3%) were critically ill of whom 32 (61.5%) died. The main reasons to admit patients to the ICU are severe respiratory failure and shock, which require immediate respiratory and circulatory support.[36] The condition may deteriorate and patients may develop sepsis, renal failure, and disseminated intravascular coagulation.
There are numerous challenges faced while performing these duties including early recognition of critically ill patients who need ICU admission (like old patients and those with comorbidities), using early alerting scores, utilizing available biomarkers to predict severity and outcome of patients, and defining priorities between multiple contagious critically ill patients. Furthermore, critical care physicians have to manage shortages of resources including Personal Protective Equipments (PPEs), ventilators, and drugs. Finally, they have to communicate with families, breaking bad news if needed, dealing with their own stress, and caring for their own families.[37,38]
Critical care physicians should decide the appropriate mode of respiratory support. Endotracheal intubation is preferably done with video-guided laryngoscopy. Managing the patient in a prone position (12–16 h daily) is useful. It is advised to have low tidal volume (4–8 ml/ kg of body weight) and a high Positive End Expiratory Pressure (PEEP) targeting a plateau pressure of <30 cm H2O.[39]
Crystalloids are the preferred fluids to resuscitate shock taking care not to over-resuscitate due to their harmful effects on the lungs. The response to resuscitation should be monitored by clinical parameters, serum lactate, and fluid response. If the targeted mean arterial blood pressure could not be achieved, norepinephrine, followed by vasopressin if needed, is indicated. Dobutamine can be added when there is cardiac dysfunction.[39]
There is no effective treatment for COVID-19. Despite that, empirical antibiotics and antiviral treatment are commonly used.[40] The recent guidelines suggest using empirical antibiotics in all ventilated patients.[39] Nevertheless, we think that antibiotics are not indicated for treating COVID-19 pneumonia unless there is a community-acquired superimposed bacterial pneumonia or hospital-acquired ventilator-associated pneumonia. It is essential to obtain cultures and procalcitonin results prior to initiating empirical therapy because it may help differentiating between bacterial and viral infections.
Recent published guidelines[39] have concluded that there is no proven benefit for the antiviral treatment and suggested a weak recommendation against the use of lopinavir and ritonavir. The same guidelines found that that there is insufficient evidence to recommend the routine use of chloroquine or hydroxychloroquine. Nevertheless, chloroquine may reduce the viral replication.[41] A recent systematic review has concluded that the use of chloroquine can be supported by preclinical data, safety of the drug, and expert opinion. However, this should be done within urgent clinical trials that adhere to ethical standards.[42] A recent nonrandomized clinical trial was performed in twenty COVID-19 patients who received 600 mg of hydroxychloroquine daily with azithromycin added depending on the clinical presentation. The authors suggested that azithromycin reduced the virus load after 6 days.[43] Nevertheless, the group is heterogeneous, having a small number and and the control group was non randomized. Routine use of systemic corticosteroids for respiratory failure in COVID-19 patients is not recommended. However, it may be considered in severe septic patients with ARDS. In that case, corticosteroids should be used in low doses and for a short period.[39] The literature is growing exponentially, the evidence is changing, and the recommendations may change when this review is published. The readers have to continuously update themselves with this evolving disease.
Disaster Management
A disaster is defined as “a situation in which available resources are insufficient for immediate need of medical care.”[44] At present, the COVID-19 status varies in different countries. Nevertheless, in some countries, the number of serious cases is beyond what the health system can accommodate to keep the desired level of health care. This is a disaster by definition in which decisions to prioritize using resources to save as much patients as possible are taken. Low priority is given for those patients having low chance of survival.
There are four phases of disaster management: (1) preparedness that includes planning, building the infrastructure for response, preparing required resources, and training; (2) mitigation by reducing the severity of the disaster and its impact; (3) response during the emergency, which includes command, communication, coordination, triage, decontamination, transport, and treatment; and finally (4) recovery which is meant to restore the community function back to be normal.[45] We describe these phases in the current COVID-19 pandemic.
Preparedness
There should be early effective surveillance and response systems that detect and respond to infectious threats.[46] Early warning is pivotal for a proper response. International timely data sharing and collaboration between governments on infectious pandemics is essential for its control.[47,48] There is a latent period before a sharp dissemination of the infection occurs. It is clear from the COVID-19 pandemic that the response was slow despite early alarming warnings. As a result, a large number of patients were infected. The genetic sequencing of COVID-19 was quickly processed in China. It was shared with the WHO within 8 days of its isolation so that diagnostic RT-PCR tests could be developed. Nevertheless, it took a full month to declare COVID-19 to be the cause of the infectious break.[47,48] Inadequate initial epidemiological risk assessment and concentrating mainly on the clinical management delayed international appreciation of the seriousness of the infection.[47] It was only when COVID-19 spread globally that the WHO categorized it as a pandemic. Two days later, it declared that “Europe has now become the epicenter of the pandemic.”[15,16] Continuous training of staff on how to deal with highly infectious patients and supporting them with proper laboratory structure or alternatively assure quick access to it is important for a successful preparedness plan.[48]
Mitigation
Every effort should be done to reduce the rate of spread during the infectious period. The aim of this stage is to flatten the curve of the number of infected patients and spread it overtime so as not to overcome the capacity of the health-care system. In case this is not achieved, there will be a large number of serious patients within a short period of time that cannot be managed within the health-care system. Flattening the curve will give a chance to treat the same number of patients over a longer time. It is clear that the outcome of a health-care system will depend on its resilience and capacity [Figure 4].
Figure 4.
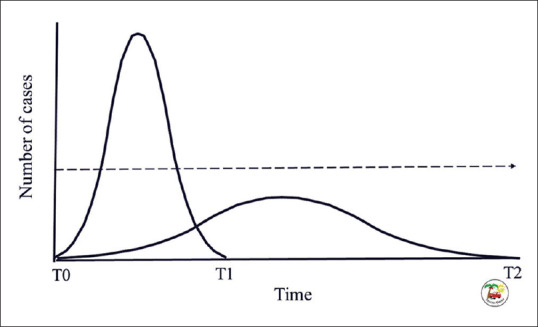
An illustration demonstrating the principle of mitigation. The left curve represents the natural curve of an epidemic. The curve starts at time 0 (T0) and ends at time 1 (T1). The dashed line represents the health care capacity. The number of infected patients is much more than the system capacity. By reducing the progress of infection, the natural curve will flattened. The modified curve will start at time 0 (T0) and end at time 2 (T2). The aim is to reduce its peak to be less than the health care capacity. The same patients are treated over a longer period of time trying to give the desired health care standard (Illustrated by Professor Fikri Abu-Zidan)
Response
It is essential to have an effective command system using an emergency management plan to organize the hospital activities during highly contagious infection disasters. This will evaluate the resources, decide priorities to supply, and coordinate activities.[49] Protection of health-care providers need PPE for those caring for suspected or confirmed COVID-19 patients. These include N95 masks, impermeable gowns to fluids (AAMI level 3), disposable gloves, and face shields or eye goggles.[50]
Triage is an important component of managing infectious disasters. Plans should be tailored depending on the local circumstances although this should have been preplanned. The principles are the same, which depend on separating the infected patients from the noninfected ones. It is advised to triage the suspected infected patients outside the hospital or in designated areas so as not to mix them with ordinary hospital patients. Zhang et al. triaged their patients through establishing adult fever clinics depending on the clinical findings, body temperature, CRP, and lymphopenia followed by chest CT scan or RT-PCR if needed.[34] Cao et al. set an online clinic, giving free consultation to reduce the influx to the emergency room. Nonemergency patients were advised to stay at home. Patients were triaged to high risk, low risk, or normal cases. Each had their treatment track to separate each group from the other.[49] The details of the management of COVID-19 were discussed in the previous sections.
Media has a major component in spreading accurate scientific information, giving proper advice for the population, and helping the health-care sector in their important function. The community should work in harmony to overcome this everyone threatening crisis.
Recovery
This stage has not globally been reached. The pandemic COVID-19 is not yet over. It may leave serious effects on economy, politics, and mental health. The recovery phase will depend on numerous factors, including mutation and adaptation of the virus, number of infected patients, the age and the immunity status of the population, severity of the disease, current response of the countries, enforcement of self-isolation and quarantine, travel restrictions, health-care reserve, and finally the economic status of the country. It is not known how the infection would progress if travel restrictions were removed. The recovery stage may be lengthy before countries return to their previous functional status.
The ability of a health-care system to recover quickly from a disaster depends on its resilience which is defined as the capacity of a health-care system and its population to prepare, respond, maintain its function, reflect on lessons learned during a crisis, and being able to reorganize its functions.[51] COVID-19 has clearly demonstrated that majority of countries has limited resilience for infectious pandemics. It is only by learning from current lessons that we can prevent and mitigate future infectious disasters.
Conclusions
COVID-19 virus has shown how fragile our global preparedness for infectious diseases is. COVID-19 pandemic has spread globally and swiftly with major impacts on health, economy, and quality of life of communities. The status is evolving and the costly global lessons learned over time are increasing. Emerging and re-emerging infections with pandemic potential will certainly happen. It would be naïve to think otherwise. The challenge is how best to prepare for such an event. After this difficult period passes, we will need to reassess our strategies in controlling and preventing such pandemics and learn from our experiences. We all need to unite and work as one world, one health approach if we are to successfully tackle such outbreaks.
Footnotes
Funding
None declared.
Conflicts of interest
None declared.
References
- 1.Morens DM, Folkers GK, Fauci AS. The challenge of emerging and re-emerging infectious diseases. Nature. 2004;430:242–9. doi: 10.1038/nature02759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gao GF. From “A”IV to “Z”IKV: Attacks from emerging and re-emerging pathogens. Cell. 2018;172:1157–9. doi: 10.1016/j.cell.2018.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taubenberger JK, Morens DM. 1918 Influenza: The mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spreeuwenberg P, Kroneman M, Paget J. Reassessing the global mortality burden of the 1918 influenza pandemic. Am J Epidemiol. 2018;187:2561–7. doi: 10.1093/aje/kwy191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viboud C, Simonsen L, Fuentes R, Flores J, Miller MA, Chowell G. Global mortality impact of the 1957-1959 influenza pandemic. J Infect Dis. 2016;213:738–45. doi: 10.1093/infdis/jiv534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. Anovel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao GF. Influenza and the live poultry trade. Science. 2014;344:235. doi: 10.1126/science.1254664. [DOI] [PubMed] [Google Scholar]
- 8.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. Apneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–3. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–74. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan G. A novel coronavirus capable of lethal human infections: An emerging picture. Virol J. 2013;10:66. doi: 10.1186/1743-422X-10-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raoult D, Zumla A, Locatelli F, Ippolito G, Kroemer G. Coronavirus infections: Epidemiological, clinical and immunological features and hypotheses. Cell Stress. 2020. [Last accessed on 2020 Mar 14]. doi: 1015698/cst202004216 [Epub ahead of print] Available from: https://wwwncbinlmnihgov/pmc/articles/PMC7064018/ [DOI] [PMC free article] [PubMed]
- 12.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. doi: 10.1056/NEJMc2004973. doi: 101056/NEJMc2004973 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang X, Wu C, Li X, Song Y, Yao X, Wu X. On the origin and continuing evolution of SARS-CoV-2 NWAA036 National Science Review. 2020. [Last Accessed on 2020 Apr 08]. Available from: https://academicoupcom/nsr/advance-article/doi/101093/nsr/nwaa036/5775463 . [DOI] [PMC free article] [PubMed]
- 14.World Health Organization. Novel Coronavirus (2019-nCoV) -Situation Report-10. [Last accessed on 2020 Mar 10]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200130-sitrep-10-ncovpdf?sfvrsn=d0b2e480_2 .
- 15.World Health Organization. World Health Organization; 2020. Mar 11, [Last accessed on 2020 Mar 16]. WHO Director-General's opening remarks at the media briefing on COVID-19. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19--11-march-2020 . [Google Scholar]
- 16.BBC. Coronavirus: Europe Now Epicentre of the Pandemic, Says WHO. 16th. 2020. Mar, [Last accessed on 2020 Mar 16]. Available from: https://wwwbbccom/news/world-europe-51876784 .
- 17.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 – Studies needed. N Engl J Med. 2020;382:1194–6. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 18.European Centre for Disease Prevention and Control. Communicable Disease Threat Report European Centre for Disease Prevention and Control; Week 10, 1-7 March, 2020. [Last accessed on 2020 Mar 17]. Available from: https://wwwecdceuropaeu/sites/default/files/documents/communicable-disease-threats-report-7%20Mar-2020-PUBLICpdf .
- 19.Patel A, Jernigan DB 2019-nCoV CDC Response Team. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak – United States, December 31, 2019-February 4, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:140–6. doi: 10.15585/mmwr.mm6905e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jallon JM, Risler Y, Iwatsubo M. Beef liver L-glutamate dehydrogenase mechanism: Presteady state study of the catalytic reduction of 2.oxoglutarate by NADPH. Biochem Biophys Res Commun. 1975;67:1527–36. doi: 10.1016/0006-291x(75)90200-4. [DOI] [PubMed] [Google Scholar]
- 21.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 Cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. doi: 101001/jama20202648 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Wilson N, Kvalsvig A, Barnard LT, Baker MG. Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2606.200320. doi: 103201/eid2606200320 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX. China medical treatment expert group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. doi: 101056/NEJMoa2002032 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. doi: 101007/s00134-020-05991-x [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020;395:809–15. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen S, Huang B, Luo DJ, Li X, Yang F, Zhao Y, et al. Pregnant women with new coronavirus infection: A clinical characteristics and placental pathological analysis of three cases. Zhonghua Bing Li Xue Za Zhi. 2020;49:E005. doi: 10.3760/cma.j.cn112151-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 28.Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H. Infants born to mothers with a new Coronavirus (COVID-19) Front Pediatr. 2020. [Last accessed on 2020 Mar 19]. doi: 103389/fped202000104. Available from: https://wwwfrontiersinorg/articles/103389/fped 202000104/full . [DOI] [PMC free article] [PubMed]
- 29.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 pii: e20200702 doi: 101542/peds2020-0702 [Epub ahead of print] [Google Scholar]
- 30.Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J. SARS-CoV-2 infection in children. N Engl J Med. 2020 doi: 10.1056/NEJMc2005073. doi:101056/NEJMc2005073 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, Lu GM, et al. Coronavirus disease 2019 (COVID-19): A perspective from China. Radiology. 2020:200490. doi: 10.1148/radiol.2020200490. doi:10.1148/radiol.2020 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Y, Xia L. Coronavirus disease 2019 (COVID-19): Role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.22954. doi:10.2214/AJR.20.22954. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 33.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019-nCoV pneumonia: Relationship to negative RT-PCR testing. Radiology. 2020:200343. doi: 10.1148/radiol.2020200343. doi: 10.1148/radiol.2020 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang J, Zhou L, Yang Y, Peng W, Wang W, Chen X. Therapeutic and triage strategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir Med. 2020;8:e11–e12. doi: 10.1016/S2213-2600(20)30071-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Han R, Huang L, Jiang H, Dong J, Peng H, Zhang D. Early clinical and CT manifestations of coronavirus disease 2019 (COVID-19) pneumonia. AJR Am J Roentgenol. 2020:1–6. doi: 10.2214/AJR.20.22961. doi: 10.2214/AJR.20.22961. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 36.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. pii:S2213-2600(20)30079-5 doi: 101016/S2213-2600(20)30079-5 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murthy S, Gomersall CD, Fowler RA. Care for critically Ill patients with COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.3633. doi: 101001/jama20203633 [Epub ahead of print] PubMed PMID: 32159735. [DOI] [PubMed] [Google Scholar]
- 38.Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05979-7. doi: 101007/s00134-020-05979-7 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Society of Critical Care Medicine. [Last accessed on 2020 Mar 21]. Available from: https://wwwsccmorg/getattachment/Disaster/SSC-COVID19-Critical-Care-Guidelinespdf . [DOI] [PMC free article] [PubMed]
- 40.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gao J, Tian Z, Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. 2020;14:72–3. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 42.Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020 doi: 10.1016/j.jcrc.2020.03.005. pii: S0883-9441(20)30390-7 doi: 101016/jjcrc202003005 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020:105949. doi: 10.1016/j.ijantimicag.2020.105949. doi:10.1016/j.ijantimicag.2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lennquist S. Major incidents: Definitions and demands on the health-care system. Medical Responses to Major Incidents and Disasters A Practical Guide for Medical Staff. In: Lennquist S, editor. 1st ed. London: Springer; 2012. pp. 1–7. [Google Scholar]
- 45.Briggs SM, editor. 2nd ed. USA: Cine-Med Publishing, Inc, CT; 2014. Mass casualty incident management In: Advanced Disaster Medical Response Manual for Providers; pp. 1–7. [Google Scholar]
- 46.Infectious diseases and microbiological threats. Medical Responses to Major Incidents and Disasters A Practical Guide for Medical Staff. In: Wahl M, Lennquist S, editors. 1st ed. London: Springer; 2012. pp. 293–303. [Google Scholar]
- 47.Peeri NC, Shrestha N, Rahman MS, Zaki R, Tan Z, Bibi The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? Int J Epidemiol. 2020 doi: 10.1093/ije/dyaa033. pii: dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith N, Fraser M. Straining the system: Novel coronavirus (COVID-19) and preparedness for concomitant disasters. Am J Public Health. 2020:e1–e2. doi: 10.2105/AJPH.2020.305618. doi: 10.2105/AJPH.2020.305618. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cao Y, Li Q, Chen J, Guo X, Miao C, Yang H, et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med. 2020 doi: 10.1111/acem.13951. doi: 101111/acem13951 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cheng VC, Wong SC, Chen JH, Yip CC, Chuang VW, Tsang OT, et al. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020:1–6. doi: 10.1017/ice.2020.58. doi: 10.1017/ice.2020.58. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nuzzo JB, Meyer D, Snyder M, Ravi SJ, Lapascu A, Souleles J, et al. What makes health systems resilient against infectious disease outbreaks and natural hazards?. Results from a scoping review. BMC Public Health. 2019;19:1310. doi: 10.1186/s12889-019-7707-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


