Abstract
Background
The Severe Acute Respiratory Syndrome Coronavirus 2 pandemic has exposed surgeons to hazardous working conditions, imposing the need for personal protective equipment (PPE) use during surgery. The use of such equipment may affect their non-technical skills, augment fatigue, and affect performance. This study aimed to assess the surgeons’ perceptions of the impact of wearing PPE during emergency surgery throughout the pandemic.
Methods
An international cooperation group conducted an anonymous online survey among surgeons from over 30 countries, to assess perceptions about the impact of PPE use on non-technical skills, overall comfort, decision making, and surgical performance during emergency surgery on COVID-19 patients.
Results
Responses to the survey (134) were received from surgeons based on 26 countries. The vast majority (72%) were males. More than half of the respondents (54%) felt that their surgical performance was hampered with PPE. Visual impairment was reported by 63%, whereas 54% had communication impediments. Less than half (48%) felt protected with the use of PPE, and the same proportion perceived that the use of such equipment influenced their decision making. Decreased overall comfort was cited by 66%, and 82% experienced increased surgical fatigue.
Conclusions
Surgeons perceived impediment for both visibility and communication, and other non-technical skills while using PPE on emergency surgery in COVID-19 patients. Their perceived lack of protection and comfort and increased fatigue may have inhibited their optimal surgical performance. More attention should be placed in the design of more user-friendly equipment, given the possibility of a second wave of the pandemic.
Introduction
Several cases of pneumonia of unknown etiology were diagnosed in the city of Wuhan, China, on December 31, 2019 [1]. One week later, the causative agent was identified and termed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). This new disease, transmitted by human-to-human contact and airborne droplet routes, was named COVID-19 by the World Health Organization (WHO) [2]. The SARS-CoV-2 spread rapidly worldwide. In the following weeks, despite the containment measures adopted in China, the WHO declared the outbreak a public health emergency of international concern, and only five weeks after that announcement, it was declared a pandemic [3, 4]. Its fast-global spread and the lack of specific treatment led to an increase of infections among the general public and healthcare workers (HCW), forcing measures of social distancing for the public, and the use of PPE by HCW. In February 2020, the WHO issued interim guidance for PPE use, including gloves, medical masks, goggles or a face shield, and gown, as well as N95/FFP2 or equivalent respirators, for those performing aerosol-generating procedures [5]. The level of exposure to the virus varies by HCWs specific role. Surgeons in close contact with COVID-19 patients' body fluids perform procedures that increase their risks and exposure [6, 7]. They require proper donning and doffing of airborne PPE for optimal safety during surgical procedures. The influence of these measures on surgical performance and execution of non-technical skills during the pandemic should be of interest. Non-technical skills have been identified as essential to the safety and efficiency of surgical practice [8]. These non-technical skills are communication, situational awareness, decision making, and fatigue control, all essential when performing emergency surgery [9]. The use of PPE during emergency surgery raised concerns about their impact on surgical performance, sense of protection, the fulfillment of non-technical skills, overall comfort, and surgical fatigue. The purpose of this study was to assess surgeons' perceptions of how PPE's use influenced these skills and his/her sense of surgical performance, safety, and decision making during emergency surgery throughout a determined period of the COVID-19 pandemic.
Methods
An International Cooperation Group of PPE and Emergency Surgery was created in Spain during the COVID-19 outbreak, with surgeons from Brazil, Chile, and Portugal. The group designed a 67-question survey based on the current literature and personal experience of PPE use during the COVID-19 pandemic. The question sheet was created using the SurveyMonkey platform and issued it internationally as an anonymous online survey that ran from April 1st through the 15th, 2020. A non-probability sampling method was applied, consisting of a convenience sample of 680 surgeons from over 30 countries, categorized into four regions: Europe, America, Asia, and Africa. One hundred forty received direct email invitations, among them were international faculty members of the Definitive Surgical Trauma Care program of the International Association for Trauma Surgery and Intensive Care, as well as Trauma Surgeons of the American College of Surgeons. Additionally, 540 members of the Trauma and Emergency Surgery Chapter of the Spanish Surgical Association, were contacted and emailed a survey URL: https://es.surveymonkey.com/r/85CJG8N, also posted on social media (WhatsApp, Twitter, and LinkedIn). The vast majority of the participating surgeons specialized in general, trauma, and acute care surgery. The survey collected demographic data (age, gender, working position, and country of clinical practice) along with the surgeons’ self-impressions with PPE use and the sense of protection, visual impairment, communication with the surgical team, situational awareness, decision-making process, overall comfort, surgical performance, and surgical fatigue during the COVID-19 pandemic. The questions were formulated so that respondents could agree or disagree with the specified statement. Frequencies and percentages were calculated for the collected data.
Results
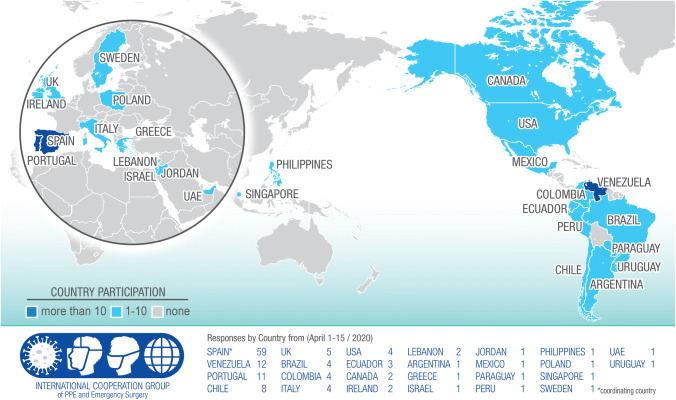
The response rate to the 680 invitations issued was of 20% (N = 134), comprised by 97 (72%) males and 37 females; almost two-thirds (64%) aged between 31 and 50, formed by 125 surgical specialists and nine surgical trainees, answering from 26 countries (12 from America, eight from Europe, four from the Middle East, and two from Asia). The vast majority answered from Spain (59), Venezuela (12), Portugal (11), and Chile (8), while the rest did it from countries with five or fewer participants (Fig. 1).
Fig. 1.
Distribution of participating countries with the number of participants per country
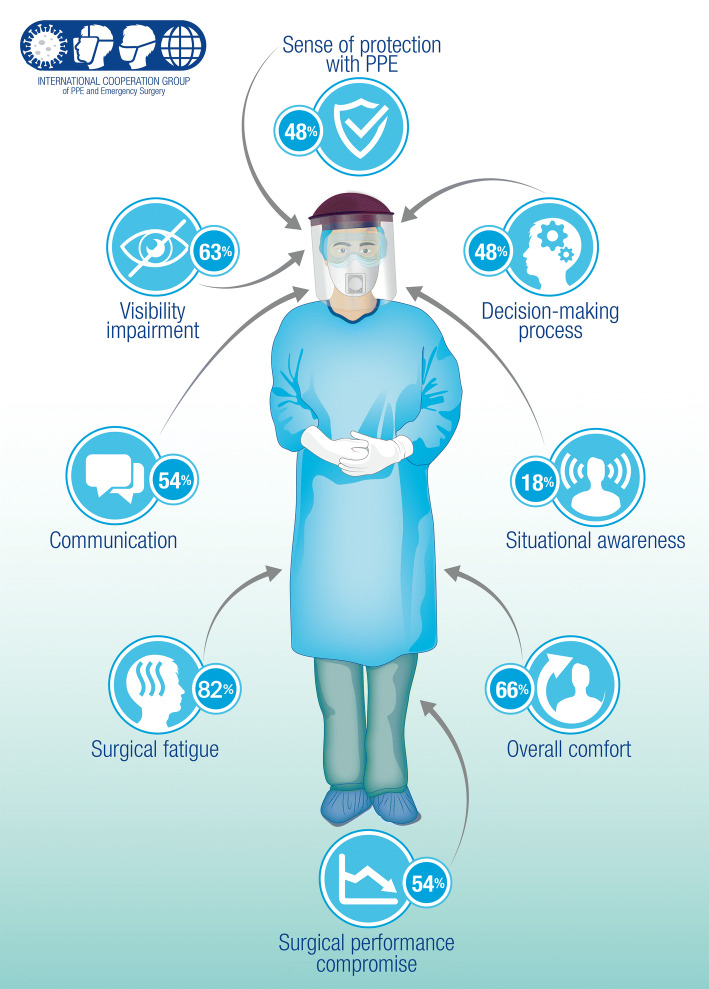
Most of the responses (76%) were received through the provided web link, just over one-fifth answered the direct email invitation (21.4%), and a minority did it through social media (1%). By the time the survey was closed, over three quarters (77%) of the studied population had admitted confirmed COVID-19 patients in their hospitals and over half (57%) had performed at least one surgery on suspected or verified cases. Concerning the surgical approach in emergency surgery, 58 (43%) had performed open surgery, and 35 (26%) conducted laparoscopic procedures. Regarding PPE selection, 83% reported double and 7% triple gloving; for eye protection, 31% used goggles, 30% facemask, 30% used both, and 9% a surgical face shield. Over half of the respondents (54%) said that they felt their surgical performance during the outbreak was compromised by PPE use and only 51% of those who answered mentioned they did feel protected with it. When questioned whether the use of PPE affected non-technical skills, over half (54%) manifested communication issues, almost two-thirds (63%) experienced visual interference, and less than one-fifth (18%) reported situational awareness concerns. Two-thirds (66%) expressed a decrease in overall comfort, a significant majority (82%) an increase in surgical fatigue, and when queried whether using PPE influenced their decision-making process, almost half (48%) answered affirmatively (Fig. 2).
Fig. 2.
Iconographic representation of PPE impact on surgeon’s working conditions
Discussion
In this study, we analyzed the impact of PPE use on non-technical skills and surgical performance while performing emergency surgery during the COVID-19 pandemic. Current PPE use recommendations for HCWs and OR staff consist of protection for droplet, contact, and airborne routes [10]. They include the use of N95/FFP3 respirators, eye protection, face shield or powered-air-purifying-respirators (PAPR), gloves, surgical gown, and shoe covers [5]. Most of the current literature regarding PPE focus on donning and doffing techniques [11–14]. However, few contemplate how the use of PPE impacts the surgeon's performance, the sensation of being protected, non-technical skills execution, sense of well-being, and ultimately, influence on surgical decision making [15]. It would be naive to think that working for extended periods while wearing this protective equipment does not influence the surgeon's comfort and performance.
Our survey attempted to analyze the global situation of the emergency surgery working conditions during the COVID-19 pandemic. However, the geographical distribution of responses gave us data that could convey more to a regional view, because almost two-thirds (63%) were from European countries. This response pattern could be influenced by the spike in new cases reported mainly in Europe during the period the survey was issued. Spanish-based surgeons' high participation level (44%) might have been influenced by the number of invitations issued by the Spanish Surgical Association to its members.
The answers received revealed that 77% of the respondents had COVID-19 patients admitted in their hospitals, and over half had performed emergency surgery in COVID-19 patients. The results show that their perceptions about the impact of PPE use of surgical performance were not a priori opinion, but the result of having experienced it. When comparing the open vs. laparoscopic approach used in emergency surgeries, a higher number of open procedures were reported (43% vs. 26%), and these differences contrasted with the results incline the authors to consider that the PPE use had a more significant impact on the surgeon while performing an open approach. One key result of our study is that more than half of the respondents asserted that PPE uses affected their surgical performance, which seems to be supported by their reports about reduced comfort, communications difficulties, and impaired visibility. Additionally, the double and even triple gloving, the use of face masks, and goggles can hamper psychomotor skill and performance of manual tasks, especially in prolonged emergency settings. Visibility impairment, mostly due to goggle fogging, was reported by almost two-thirds (63%). Contrary to our finding, Loibner M et al. did not find an impact on performance even though they reported limited dexterity and visibility when evaluating limiting factors while wearing PPE in a healthcare environment; however, this study was performed with ventilated suits and under experimental conditions [15]. The lack of confidence in the protection provided by PPE could be explained by unprecedented pandemic working conditions, the pressure to reuse equipment due to shortages, and even to the limited training caused by the pandemic itself [16]. Proper use of PPE depends not only on availability but also on training and comfort [17, 18].
We also found that PPE use under the analyzed circumstances does affect surgical non-technical skills, such as verbal communication, situational awareness, and decision making. Responses had evidenced that the first of them was affected by two pieces of such equipment: respirators and face shields. N95/ FFP2 respirators muffled the voice, and plexiglass face shields isolated the face disrupting voice projection, forcing surgeons to speak louder to colleagues and OR staff while performing surgery. Additionally, face shields and goggles generate glare and, when goggles are used along with respirators, those become foggy, obstructing visibility. Finally, an aspect of utmost importance for successful performance in emergency surgery is to exercise both psychomotor and cognitive skills, which involve a complex decision analysis [19]. Adequate judgment in surgical practice has been established as the capacity to make accurate decisions with the available information [20]. PPE use and the adverse working conditions generated during the pandemic seem to have caused increased fatigue during surgical procedures, influencing surgical judgment.
The answers received point to the assumption that the sum of these factors had a toll on overall comfort and surgical fatigue. The use of N95/FFP2 or equivalent respirators during extended periods cause physical discomfort, and some face shields can also generate pressure in the forehead, causing additional discomfort in prolonged surgeries. The use of this equipment in the surgeons’ working environment generates biomechanical stress, resulting in surgical fatigue and exhaustion. Engelmann et al. suggest taking short intermittent breaks to help maintain excellent performance, lower error rates, and increase the surgeon’s well-being [21]. Unfortunately, the working conditions during pandemic outbreaks make this strategy hard to follow. Research on PPE during infectious disease outbreaks had focused mainly on safety issues, but our study highlights areas for future research. We feel there is an increasing need to develop upgraded PPE designs, making them more comfortable, reusable, and sustainable. Improved comfort would enhance surgical performance, OR staff well-being, and a sense of confidence using PPE in times of pandemics.
It is important to note that our study had several limitations. First, the assessment method relied on perceptions prone to bias, because remembrance is subjective. Second, the study was international, and we are aware of the differences in working conditions and equipment available in each country. Third, the sampling method recruited a higher number of European responders, so that results may rule out global generalizations. Even with these limitations, we believe that our study highlights the problematic working conditions for surgeons using PPE during the COVID-19 pandemic and that they may be useful for orienting efforts to be made toward the improvement of PPE comfort level availability for future pandemics. In summary, we found that the use of personal protective equipment alters both visual and communication abilities during emergency surgery. Emergency surgery using this equipment was found to convey toward surgical discomfort and increased fatigue, affecting the decision-making process and surgical performance.
Acknowledgements
We would like to acknowledge all the members of the International Cooperation Group on PPE and Emergency Surgery: Juan Pablo Ramos, MD (Surgery Department, Sótero del Río Healthcare Complex, Santiago, Chile), Elena Rangelova, MD (Upper Abdominal Surgery Department, Sahlgrenska University Hospital, Gothenurg, Sweden). We also acknowledge Mercedes Muñoz, information specialist, for her assistance performing the literature search, Carlos Yánez Sr., Ph.D. for his revision, and Ilaria Bondi for her contribution with the medical illustrations.
Abbreviations
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- PPE
Personal protective equipment
- COVID-19
Coronavirus Disease 2019
- WHO
World Health Organization
- HCW
Healthcare worker
- OR
Operating room
- PAPR
Powered-air-purifying-respirator
- SARS
Severe Acute Respiratory Syndrome SARS
Author contributions
All authors meet authorship criteria for this manuscript as described below. The communication was conceived by CY. The literature search was performed by CY, AG, JA, and JLB. The manuscript draft was written by CY and HA. Critical revision was done by AG, JA, MR, PO, SDS, HA, LP, and JLB. All authors reviewed and approved the final manuscript.
Funding
No funding or grant support was received for this manuscript.
Compliance with ethical standards
Conflict of interest
Carlos Yánez, Antonio Güemes, Jose Aranda, Marcelo Ribeiro, Pablo Ottolino, Salomone Di Saverio, Henrique Alexandrino, Luca Ponchietti, and Jun Luís Blas have no conflict of interest in this manuscript.
Ethical standards
This article does not contain any experimental studies involving human or animal participants performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Carlos Yánez Benítez, Email: carlosyb1@gmail.com, Email: cjyanezb@salud.aragon.es.
Antonio Güemes, Email: aguemes@unizar.es.
José Aranda, Email: jose.aranda.narvaez@gmail.com.
Marcelo Ribeiro, Email: drmribeiro@gmail.com.
Pablo Ottolino, Email: ottolinopablo@gmail.com.
Salomone Di Saverio, Email: salomone.disaverio@gmail.com.
Henrique Alexandrino, Email: halexandrino123@gmail.com.
Luca Ponchietti, Email: lponchietti@salud.aragon.es.
Juan L. Blas, Email: julublas@gmail.com
References
- 1.Lu H, Stratton CW, Tang Y. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization, WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020, (2020) https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020
- 3.World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 30 January 2020. https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 4.World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/ who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11- march-2020
- 5.World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). Interim guidance 27 February 2020 https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf
- 6.Zhang W, Du RH, Zheng XS, et al. Molecular and serological investigation of 2019- nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9(1):386–389. doi: 10.1080/22221751.2020.1729071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forrester JD, Nassar AK, Maggio PM, et al. Precautions for operating room team members during the COVID-19 pandemic. J Am Coll Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yule S, Paterson-Brown S. Surgeons’ non-technical skills. Surg Clin North Am. 2012;92(1):37–50. doi: 10.1016/j.suc.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 9.Hull L, Sevdalis N. Advances in teaching and assessing nontechnical skills. Surg Clin North Am. 2015;95(4):869–884. doi: 10.1016/j.suc.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Elster E, Chung K, Potter BK. Response to COVID-19 by the surgical community. Surgery. 2020 doi: 10.1016/j.surg.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verbeek JH, Ijaz S, Mischke C, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2016 doi: 10.1002/14651858.CD011621.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suen LKP, Guo YP, Tong DWK, et al. Self-contamination during doffing of personal protective equipment by healthcare workers to prevent Ebola transmission. Antimicrob Resist Infect Control. 2018;7:157. doi: 10.1186/s13756-018-0433-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tomas ME, Kundrapu S, Thota P, et al. Contamination of health care personnel during removal of personal protective equipment. JAMA Intern Med. 2015;175(12):1904–1910. doi: 10.1001/jamainternmed.2015.4535. [DOI] [PubMed] [Google Scholar]
- 14.Zellmer C, Van Hoof S, Safdar N. Variation in health care worker removal of personal protective equipment. Am J Infect Control. 2015;43(7):750–751. doi: 10.1016/j.ajic.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loibner M, Hagauer S, Schwantzer G, Berghold A, Zatloukal K. Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomized study. PLoS ONE. 2019;14(1):e0210775. doi: 10.1371/journal.pone.0210775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang J, Zhou M, Liu F. Reasons for healthcare workers infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105(1):100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sim SW, Moey KSP, Tan NC. The use of face masks to prevent respiratory infection: a literature review in the context of the Health Belief Model. Singapore Med J. 2014;55:160–167. doi: 10.11622/smedj.2014037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chughtai AA, Seale H, Dung TC, et al. Compliance with the use of medical and cloth masks among healthcare workers in Vietnam. Ann Occup Hyg. 2016;60:619–630. doi: 10.1093/annhyg/mew008. [DOI] [PubMed] [Google Scholar]
- 19.Satava R, Gallagher AG, Pellegrini CA. Surgical competence and surgical proficiency: definitions, taxonomy, and metrics. J Am Coll Surg. 2003;196(6):933–937. doi: 10.1016/S1072-7515(03)00237-0. [DOI] [PubMed] [Google Scholar]
- 20.Clarke JR. Decision making in surgical practice. World J Surg. 1989;13(3):245–251. doi: 10.1007/BF01659029. [DOI] [PubMed] [Google Scholar]
- 21.Engelmann C, Ure B. Effects of intraoperative breaks on mental and somatic operator fatigue: a randomized clinical trial. Surg Endosc. 2012;25(12):1245–1250. doi: 10.1007/s00464-010-1350-1. [DOI] [PubMed] [Google Scholar]