Abstract
Background
There has been much interest in environmental temperature and race as modulators of Coronavirus disease-19 (COVID-19) infection and mortality. However, in the United States race and temperature correlate with various other social determinants of health, comorbidities, and environmental influences that could be responsible for noted effects. This study investigates the independent effects of race and environmental temperature on COVID-19 incidence and mortality in United States counties.
Methods
Data on COVID-19 and risk factors in all United States counties was collected. 661 counties with at least 50 COVID-19 cases and 217 with at least 10 deaths were included in analyses. Upper and lower quartiles for cases/100,000 people and halves for deaths/100,000 people were compared with t-tests. Adjusted linear and logistic regression analyses were performed to evaluate the independent effects of race and environmental temperature.
Results
Multivariate regression analyses demonstrated Black race is a risk factor for increased COVID-19 cases (OR=1.22, 95% CI: 1.09–1.40, P=0.001) and deaths independent of comorbidities, poverty, access to health care, and other risk factors. Higher environmental temperature independently reduced caseload (OR=0.81, 95% CI: 0.71–0.91, P=0.0009), but not deaths.
Conclusions
Higher environmental temperatures correlated with reduced COVID-19 cases, but this benefit does not yet appear in mortality models. Black race was an independent risk factor for increased COVID-19 cases and deaths. Thus, many proposed mechanisms through which Black race might increase risk for COVID-19, such as socioeconomic and healthcare-related predispositions, are inadequate in explaining the full magnitude of this health disparity.
Key Indexing Terms: COVID-19, SARS-CoV-2, Coronavirus, Black Race, Environmental temperature
Introduction
Since the first case of coronavirus disease 2019 (COVID-19) in December 2019, COVID-19 has spread rapidly around the world.1 As of April 14, 2020, the Johns Hopkins University Coronavirus Resource Center has reported over 600,000 cases in the United States. Developing new therapies, identifying risk factors, and minimizing spread remain top priorities in the fight against COVID-19.
Previous studies have examined the effects of various risk factors on spread of COVID-19 including patient demographics,2 social determinants of health,3 environmental variables,4, 5, 6 housing,7 and underlying health conditions.8, 9, 10 In particular, there have been reports of an environmental temperature effect on COVID-19 cases,4, 5, 6 however the intersection of environmental temperature and socioeconomic variables has not been fully elucidated in the United States. Additionally, numerous headlines have brought race to the forefront as a potentially significant risk factor for increased COVID-19 incidence.11 For example, African Americans have accounted for all but three COVID-19 related deaths in St. Louis, Missouri and three quarters of those in Milwaukee, Wisconsin.12 However, the effects of race are often intermixed with the effects of other socioeconomic factors.
In this study, using multivariate regression analyses controlling for demographics, underlying health conditions, social determinants of health, environmental variables, and social distancing adherence, we seek to illuminate the independent effects of both race and environmental temperature on the incidence of COVID-19 cases and mortality at the US county level.
Materials and methods
COVID-19 cases and deaths data
COVID-19 confirmed case number and death number through April 14, 2020 were obtained for each US county from the Center for Systems Science and Engineering (CSSE) Coronavirus Resource Center at Johns Hopkins University. This data source contains COVID-19 case number and deaths data from all 3,143 US counties in 50 states and the District of Columbia (D.C.). Cases/100,000 people and deaths/100,000 people for each US county were calculated using CSSE and census data. Counties were excluded from the analyses if they had fewer than 50 cases or their first case occurred fewer than 3 weeks prior to the end of the study. With these constraints, 661 counties from 50 states and Washington D.C were included in case analysis. Counties were excluded from death analyses if they reported fewer than 10 deaths or the first death had occurred fewer than 2 weeks prior to the end of the study. The deaths analyses include 217 counties from 37 states and Washington D.C. (Table 1 ).
TABLE 1.
Counties per state included in COVID-19 case and death analysis.
| State | # of counties In case analysis | # of counties death analysis | State | # of counties In case analysis | # of counties death analysis |
|---|---|---|---|---|---|
| Alabama | 15 | 4 | Montana | 2 | 0 |
| Alaska | 2 | 0 | Nebraska | 3 | 0 |
| Arizona | 7 | 3 | Nevada | 2 | 2 |
| Arkansas | 8 | 1 | New Hampshire | 4 | 0 |
| California | 29 | 15 | New Jersey | 21 | 16 |
| Colorado | 17 | 7 | New Mexico | 6 | 1 |
| Connecticut | 8 | 6 | New York | 31 | 12 |
| Delaware | 3 | 2 | North Carolina | 27 | 2 |
| District of Columbia | 1 | 1 | North Dakota | 2 | 0 |
| Florida | 35 | 11 | Ohio | 27 | 10 |
| Georgia | 44 | 12 | Oklahoma | 9 | 3 |
| Hawaii | 2 | 0 | Oregon | 6 | 1 |
| Idaho | 4 | 0 | Pennsylvania | 31 | 13 |
| Illinois | 15 | 5 | Rhode Island | 4 | 0 |
| Indiana | 30 | 8 | South Carolina | 17 | 2 |
| Iowa | 8 | 1 | South Dakota | 2 | 0 |
| Kansas | 5 | 2 | Tennessee | 14 | 4 |
| Kentucky | 6 | 1 | Texas | 32 | 10 |
| Louisiana | 34 | 19 | Utah | 6 | 0 |
| Maine | 3 | 1 | Vermont | 4 | 1 |
| Maryland | 15 | 8 | Virginia | 23 | 2 |
| Massachusetts | 12 | 11 | Washington | 14 | 8 |
| Michigan | 23 | 6 | West Virginia | 4 | 0 |
| Minnesota | 6 | 1 | Wisconsin | 10 | 2 |
| Mississippi | 16 | 0 | Wyoming | 2 | 0 |
| Missouri | 10 | 3 |
Data sources for covariates
Race demographics for counties was obtained from the County Health Rankings and Roadmaps Program database. Daily environmental temperature data for counties was obtained from the National Oceanic and Atmospheric Administration. County temperature was calculated using mean temperature for a period starting 10 days before the first confirmed county case and through the most current date (April 14, 2020). Unacast social distancing data was obtained through a research agreement with the company. Data from mobile phones was used to track average changes in distance travelled within counties after the first reported COVID-19 case. Change in average distance travelled was used as an indicator of social distancing. Data for other potential risk factors used in analysis was obtained through publicly available data sources. (Table 2 ).
TABLE 2.
Publicly available data sources used in analysis.
| County data | Source |
|---|---|
| COVID-19 Cases+Deaths | Center for Systems Science and Engineering (CSSE) Coronavirus Resource Center at Johns Hopkins University. (https://coronavirus.jhu.edu/map.html) |
| COVID-19 Tests | The COVID Tracking Project (https://covidtracking.com/) |
| 2010 Population, Population Density, Housing Density | United States Census Bureau (https://www.census.gov/en.html) |
| 2018 Gross Domestic Product | Bureau of Economic Analysis County Data (https://www.bea.gov/data/by-place-county-m) |
| Social Distancing: % Change in Average Mobility and Non-Essential Visits | Unacast Social Distancing Scoreboard (https://www.unacast.com/covid19/social-distancing-scoreboard) |
| 2012-2018 Population Demographics, Health, and Social Determinants of Health Statistics | County Health Rankings and Roadmaps Program (https://www.countyhealthrankings.org/) |
| Environmental Temperature | National Oceanic and Atmospheric Administration (https://www.ncdc.noaa.gov/) |
| Underlying Health Conditions 2014-2016: Diabetes, Hypertension, Coronary Artery Disease, Obesity, Poverty, Pollution | United States Census Bureau American Factfinder United States Diabetes Surveillance System (https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html#) |
| 2014 Respiratory Mortality | Institute for Health Metrics and Evaluation (http://ghdx.healthdata.org/record/ihme-data/united-states-chronic-respiratory-disease-mortality-rates-county-1980-2014) |
| 1998-2018 Liver Mortality | Multiple Cause of Death Database (https://wonder.cdc.gov/mcd-icd10.html) |
Statistical analysis
T-tests were used to compare differences between covariates for the highest quartile and lowest quartile cases/100,000 and the top 50% versus the bottom 50% deaths/100,000. Since modeling complex phenomenon without controlling for a variety of confounding variables can lead to skewed results, sequential regression modelling was used to demonstrate the effect of race and temperature on cases and deaths/100,000. The stepwise approach to regression helps mitigate excessive confounding risk through sensitivity analysis. Logistic regression was used to compare counties in the highest quartile for cases/100,000 to those in the lowest. There were an insufficient number of counties meeting the deaths/100,000 requirements to run logistic regression, thus linear regression was used for deaths/100,000 analyses. Results of linear regression for cases per/100,000 including all 661 counties are provided for direct comparison between cases and deaths.
The sequential model had four parts. Each model included all variables from the previous models. Model 1 was a univariate analysis. Model 2 added the following county macroeconomic and COVID-19-specific variables: population density, GDP/capita, COVID-19 tests/100,000 people (state level data), COVID-19 cases/100,000 people (deaths analysis only), a marker for which State the county is in, average percent reduction in cellphone movement from day of first confirmed case to end of study, the percent of population living in overcrowded housing, and the number of days since the first confirmed COVID-19 case. Model 3 added these county demographics and environmental variables to Model 2: percent of population over 65, proportion of Black residents, percent of the population that is female, percent of population living in rural areas, the Food Environment Index (a measure of accessibility and affordability of healthy food), the rate of violent crime/100,000 people, the average environmental temperature from 10 days before the first case to the end of the study, air quality measured as the average annual ambient concentrations of atmospheric particulate matter under 2.5 micrometers (PM2.5), percent of the population considered to be in fair or poor health, and the percent of the population living in poverty. Model 4 was the full model and included medical comorbidities and access to health care variables in addition to all variables in Model 3. Specifically these new variables were: diabetes, obesity, physical inactivity, excessive drinking, and smoking were all reported as percent of the population; liver disease, hypertension, coronary heart disease, and chronic respiratory disease were reported as mortality/100,000 people; and the patient to primary care physician ratio, the percent of people sleeping fewer than seven hours/night, the percent of the population without health insurance and the percent of the population who received the flu vaccine were also included.
All statistical analyses were performed with Prism 8.0 (GraphPad Software, San Diego, CA). For all analyses, α = 0.05.
Results
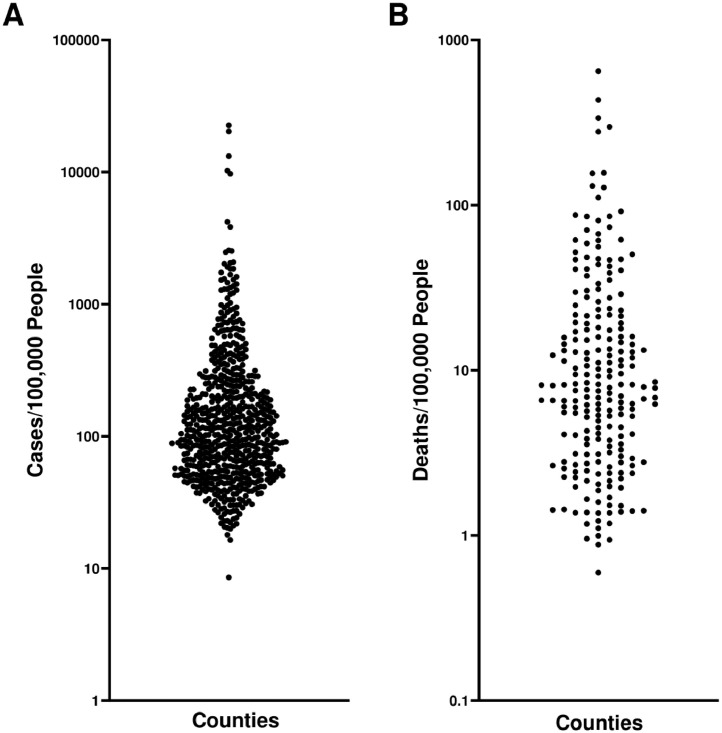
Our study contained data from 3143 US counties across all 50 states and the District of Columbia (D.C). 661 US counties (21.0%) from 50 states and D.C. were included in case analysis (Figure 1 A). 217 US counties (6.9%) from 37 states and D.C. were included in death analysis (Figure 1B).
FIGURE 1.
Distribution of COVID-19 (A) Cases/100,000 people and (B) Deaths/100,000 people for United States counties included in analyses.
There were significant differences in demographics between the two cohorts for cases/100,000 people. Some of the variables that differed between lower and upper quartiles for cases/100,000 people analysis included Gross Domestic Product (GDP)/Capita (45.97 vs. 85.59, P=0.005), percent decrease in mobility (increase in social distancing) since first COVID-19 case (42.13% vs. 38.70%, P=0.005), percent of population over age 65 (16.44% vs. 17.80%, P=0.004), percent Black (9.23% vs. 15.66%, P=<0.0001), percent of population with diabetes mellitus (9.36% vs. 10.05%, P =0.0448), coronary heart disease mortality/100,000 (89.14 vs. 96.58, P=0.0060), percent considered physically inactive (22.90% vs. 25.91%, P=<0.0001), percent who drink excessively (18.99% vs. 18.21%, P=0.0125), percent who smoke tobacco (15.54% vs. 16.72%, P=0.0001), the patient to primary care physician ratio (1,553.4 vs. 2,444.53, P=0.0002), and percent who received the flu vaccine (47.98% vs. 46.39%, P=0.0295). (Table 3 ).
TABLE 3.
Characteristics of study cohorts used in COVID-19 analysis up to April 14, 2020.
| Variable | Cases/100,000 lowest quartile (SEM) n = 165 | Cases/100,000 highest quartile (SEM) n = 165 | P Value | Deaths/100,000 lower half (SEM) n = 108 | Deaths/100,000 upper half (SEM) n = 109 | P Value |
|---|---|---|---|---|---|---|
| County Macroeconomics + Covid-19 Specific Variables | ||||||
| COVID-19 Cases/100,000 peopleb | 41.2 (0.82) | 1138.8 (212.9) | <0.001 | 119.5 (8.97) | 1321.6 (318.3) | <0.001 |
| COVID-19 Deaths/100,000 peoplea | 1.21 (0.08) | 36.35 (5.78) | <0.001 | 3.79 (0.20) | 49.48 (8.41) | <0.001 |
| COVID-19 Tests/100,000 people | 832.6 (27.5) | 1363.3 (58.1) | <0.001 | 1014.1 (56.8) | 1447.7 (68.5) | <0.001 |
| Population Density/Square Mile (2010) | 594.3 (67.9) | 1300.6 (444.3) | 0.12 | 1211.65 (167.81) | 1893.13 (668.46) | 0.32 |
| GDP/Capita (2010) | 45.97 (1.21) | 85.59 (13.98) | 0.005 | 61.40 (2.43) | 70.79 (11.82) | 0.44 |
| Social Distancing: % Decrease in Mobility After First COVID-19 Case | 42.13% (0.50%) | 38.70 (1.11%) | 0.005 | 43.97 (0.63) | 43.31 (1.08) | 0.60 |
| % Overcrowded Housing | 2.94% (0.19%) | 2.42%(0.13%) | 0.028 | 3.06% (0.21%) | 2.37% (0.14%) | 0.007 |
| # Days Since First Case | 31.56 (0.65) | 32.1 (0.57) | 0.56 | 22.14 (0.49) | 22.78 (0.57) | 0.39 |
| County Demographics + Environmental Variables | ||||||
| % Age >65 | 16.44% (0.35%) | 17.80% (0.31%) | 0.004 | 15.44% (0.38%) | 16.64% (0.33%) | 0.02 |
| % Non-Hispanic Whitea | 66.64% (1.56%) | 68.01% (1.51%) | 0.53 | 58.00% (1.75%) | 65.94% (1.73%) | 0.001 |
| % Black | 9.23% (0.72%) | 15.66% (1.29%) | <0.001 | 14.79% (1.23%) | 16.16% (1.53%) | 0.49 |
| % Hispanica | 16.37% (1.43%) | 10.57% (0.89%) | <0.001 | 17.83% (1.45%) | 11.16% (0.92%) | <0.001 |
| % Asiana | 4.50% (0.44%) | 2.96% (0.30%) | 0.004 | 6.61% (0.66%) | 4.32% (0.43%) | 0.004 |
| % Native Hawaiian/Other Pacific Islandera | 0.34% (0.089%) | 0.11%(0.0095%) | 0.004 | 0.20% (0.028%) | 0.13% (0.015%) | 0.019 |
| % American Indian & Alaska Nativea | 1.14% (0.102%) | 1.61% (0.56%) | 0.41 | 1.00% (0.11%) | 1.016% (0.26%) | 0.97 |
| % Female | 50.81% (0.072%) | 50.75% (0.14%) | 0.71 | 51.02% (0.076%) | 51.10% (0.093%) | 0.52 |
| % Rural | 17.59% (1.05%) | 36.32% (2.47%) | <0.001 | 8.07% (0.83%) | 21.90% (2.27%) | <0.001 |
| <37° Latitudea | 49.1% (3.9%) | 31.5% (3.6%) | 0.001 | 49.1%(4.8%) | 23.9% (4.1%) | <0.001 |
| Food Environment Index | 7.73 (0.054) | 7.86 (0.092) | 0.22 | 7.756 (0.077) | 7.87 (0.102) | 0.37 |
| Violent Crimes/100,000 People | 359.40 (16.57) | 341.59 (21.06) | 0.51 | 436.23 (22.13) | 361.13 (26.64) | 0.03 |
| Average Environmental Temperature From 10 Days Before First Case (°C) | 52.74(0.56) | 11.33 (0.48) | 0.80 | 11.88 (0.59) | 10.54 (0.61) | 0.09 |
| Air quality: Average Ambient PM2.5 (2014) | 9.94 (0.15) | 9.37 (0.14) | 0.005 | 10.12 (0.19) | 9.76 (0.15) | 0.146 |
| % In Fair/Poor Health | 16.38% (0.292%) | 17.33% (0.33%) | 0.03 | 16.05% (0.32%) | 16.73% (0.39%) | 0.18 |
| % Poverty | 13.29% (0.37%) | 14.91% (0.53%) | 0.012 | 13.34% (0.39%) | 14.29% (0.62%) | 0.20 |
| Medical Comorbidities + Access to Health Care | ||||||
| % Diabetes Mellitus | 9.36% (0.15%) | 10.05% (0.31%) | 0.045 | 8.73% (0.17%) | 9.49% (0.27%) | 0.018 |
| Liver Disease Mortality/100,000 People (1998-2018) | 14.77 (0.38) | 14.95 (0.49) | 0.77 | 13.48 (0.35) | 13.68 (0.35) | 0.69 |
| Hypertension Mortality/100,000 People (2014-2016) | 233.4 (6.3) | 218.7 (8.8) | 0.18 | 223.2 (7.3) | 209.3 (8.7) | 0.22 |
| Coronary Heart Disease Mortality/100,000 People (2014-2016) | 89.14 (1.75) | 96.58 (2.04) | 0.006 | 86.87 (1.89) | 97.54 (2.51) | <0.001 |
| Chronic Respiratory Disease Mortality/100,000 People (2014) | 56.32 (0.99) | 54.28 (1.29) | 0.80 | 50.53 (1.10) | 52.21 (1.37) | 0.34 |
| % Obesity in Ages 20+ (2015) | 29.42% (0.35%) | 29.90% (0.48%) | 0.42 | 27.37% (0.46%) | 29.34% (0.53%) | 0.005 |
| % Physical Inactivity | 22.90% (0.38%) | 25.91% (0.44%) | <0.001 | 21.73% (0.46%) | 25.01% (0.48%) | <0.001 |
| % Excessive Drinking | 18.99% (0.21%) | 18.21% (0,23%) | 0.01 | 19.06% (0.25%) | 18.85% (0.26) | 0.57 |
| % Smoking Tobacco | 15.54% (0.23%) | 16.72% (0.27%) | <0.001 | 14.87% (0.29%) | 16.29% (0.36%) | 0.002 |
| Patient:Primary Care Physician Ratio | 1553.39 (58.16) | 2444.53 (232.0) | <0.001 | 1284.96 (46.95) | 1729.78 (104.18) | <0.001 |
| % Uninsured | 10.07% (0.36%) | 9.25% (0.29%) | 0.08 | 9.89% (0.43%) | 8.44% (0.35%) | 0.010 |
| % Flu Vaccine | 47.98% (0.46%) | 46.39% (0.56%) | 0.03 | 47.85% (0.56%) | 47.60% (0.62%) | 0.76 |
Not included in either regression model
Only included in mortality model
Similarly, there were differences between the lower and upper half cohorts for deaths/100,000 people analyses. Some of these variables that differed included the percent of population over age 65 (15.44% vs. 16.64%, P=0.017), percent with diabetes mellitus (8.73% vs. 9.49%, P=0.018), coronary heart disease mortality/100,000 (86.87 vs. 97.54, P=0.0008), percent obese in those over age 20 (27.37% vs. 29.34%, P=0.0054), percent who smoke tobacco (14.87% vs. 16.29%, P=0.0023), the patient to primary care physician ratio (1,284.96 vs. 1,729.78, P=0.0001), and the percent without health insurance (9.89% vs. 8.44%, P=0.0099). (Table 3).
To control for possible confounding variables, sequential multivariate regression analyses were performed. For case rate logistic regression analysis, the adverse effect of percent Black remained significant with the addition of macroeconomic and COVID-19 specific variables in logistic regression (OR=1.03, 95% CI:1.01–1.06, P=<0.0001) whereas the effect of environmental temperature was still not significant (OR=0.97, 95% CI: 0.93–1.01, P=0.19). Adding county demographics and environmental factors resulted in both percent Black (OR=1.16, 95% CI: 1.08–1.24, P=<0.0001) and environmental temperature (OR=0.82, 95% CI: 0.73–0.90, P=0.0002) demonstrating significant effects on cases per/100,000. In the final model, the adverse effect of percent Black (OR=1.22, 95% CI: 1.09–1.40, P=0.001) and the protective effect of environmental temperature (OR=0.81, 95% CI: 0.71–0.91, P=0.0009) remained robust to the addition of medical comorbidities and access to health care. Similar results are seen in the linear model, although the effects of percent Black and environmental temperature do not become significant until Model 3 (Table 4 ).
TABLE 4.
Sequential multivariate modeling for COVID-19 case and death rate vs. black race and environmental temperature.
| COVID-19 cases/100,000 | Univariate analysis [95% CI] | Add macroeconomic and covid specific variables [95% CI] | Add county demographics and environmental factors [95% CI] | Add medical comorbidities and access to healthcare [95% CI] |
|---|---|---|---|---|
| Logistic | ||||
| %Black | OR=1.03 [1.02-1.06] | OR=1.03 [1.01-1.06] | OR=1.16 [1.08-1.24] | OR=1.22 [1.09-1.40] |
| p<0.001 | p=0.02 | p<0.001 | p=0.001 | |
| Environmental Temperature | OR=1.00 [0.96-1.03] | OR=0.97 [0.93-1.01] | OR=0.82 [0.73-0.90] | OR=0.81 [0.71-0.91] |
| p=0.79 | p=0.19 | p<0.001 | p<0.001 | |
| Linear | ||||
| %Black | β=-0.12 [-7.69-7.44] | β=-3.62 [-9.98-2.73] | β=12.71 [8.09-17.33] | β=11.29 [5.44-17.13] |
| p=0.97 | p=0.26 | p<0.001 | p<0.001 | |
| Environmental Temperature | β=-0.30 [-11.35-10.74] | β=-0.73 [-7.39-5.93] | β=-10.46 [-18.69 to -2.22] | β=-13.15 [-22.85 to -3.45] |
| p=0.96 | p=0.83 | p=0.01 | p=0.008 | |
| COVID-19 Deaths/100,000 | Univariate Analysis [95% CI] | Add Macroeconomic and Covid Specific Variables [95% CI] | Add County Demographics and Environmental factors [95% CI] | Add Comorbidities and Access to Healthcare [95% CI] |
| Linear | ||||
| %Black | β=-0.01 [-0.63-0.61] | β=0.20 [0.02-0.37] | β=0.57 [0.36-0.79] | β=0.35 [0.09-0.61] |
| p=0.99 | p=0.03 | p<0.001 | p=0.008 | |
| Environmental Temperature | β=0.32 [-0.52-1.15] | β=0.09 [-0.21-0.39] | β=-0.11 [-0.44-0.22] | β=-0.10 [-0.48- 0.27] |
| p=0.45 | p=0.56 | p=0.53 | p=0.59 |
Top: Logistic regression results for COVID-19 Cases per 100,000 for the lowest and highest quartiles as well as linear regression results for all 661 counties meeting the inclusion requirements. Bottom: Linear regression results for COVID-19 Deaths per 100,000 for all 217 counties included in the analyses. Odds ratios and their 95% confidence intervals were reported for logistic regressions. Regression coefficients and their 95% confidence intervals were reported for linear regressions
For death rate analysis, percent Black had a significantly positive effect on mortality after addition of macroeconomic and COVID-19 specific variables in the linear regression (β=0.20, 95% CI: 0.02–0.37, P=0.027). The effect of environmental temperature was not significant after addition of macroeconomic and COVID-19 specific variables (β=0.09, 95% CI:-0.21–0.39, P=0.557). After county demographics and environmental factors were also added, the effect of percent Black (β=0.57, 95% CI: 0.36–0.79, P=<0.0001) remained significant while environmental temperature was not significant (β=-0.11, 95% CI: -0.44–0.22, P=0.525). In the final model, after the addition of medical comorbidities and access to health care markers, the effect of percent Black (β=0.35, 95% CI: 0.09–0.61, P=0.008) was still significant and positive while the effect of environmental temperature was not significant (β=-0.10, 95% CI:-0.48 - 0.27, P=0.594) (Table 4).
Discussion
The United States has become a major epicenter of the coronavirus pandemic, now reporting the greatest number of total cases and deaths worldwide. By conducting sequential multivariate analyses of variables that span social, structural, and environmental spheres, our study aimed to more completely characterize the effects of Black race and environmental temperature on the incidence and mortality of COVID-19 in the U.S. Our results suggest that higher environmental temperatures may lead to decreased incidence, however a similar effect was not seen for mortality. Black race was an independent risk factor for increased COVID-19 cases and mortality.
Impact of race
As noted previously, Black Americans have accounted for all but three COVID-19 related deaths in St. Louis, Missouri and three quarters of those in Milwaukee, Wisconsin.12 Further, recent analyses of patients hospitalized for COVID-19 in 99 United States counties spanning 14 states have demonstrated significantly increased hospitalization rates amongst Black Americans.11 Our study corroborates and expands on these findings to suggest that Black Americans may be at significantly higher risk of COVID-19 infection and mortality nationwide.
Studies on COVID-19 incidence amongst Black Americans have pointed to the fact that, compared to the general population of the United States, Black Americans have been shown to have increased rates of smoking tobacco use and chronic medical comorbidities such as cardiovascular disease, diabetes mellitus, hypertension, obesity, and chronic respiratory disease, all of which convey increased risk of adverse COVID-19 outcomes.8, 9, 10, 11 Recent work has also cited the many inequities in structural variables, which now manifest in the disproportionate number of Black Americans suffering from poverty, environmental hazards, overcrowded housing, and decreased access to healthcare.11 However, after controlling for these factors in this study, the effect of Black race on number of COVID-19 cases and deaths persisted, indicating other modulating factors must be considered.
One potential domain includes additional sociocultural variables that have become relevant within the context of the pandemic. For example, African Americans make up a large percentage of the healthcare, transportation, government, and food supply industries, job sectors that have been deemed “essential” services in light of the SARS-CoV-2 pandemic.13 Despite the majority of Americans currently living in counties with some form of social distancing mandate, fewer than one in five Black Americans have a job with flexibility to work from home, compared with more than a third of white and Asian American workers.14 Thus, racial differences in social distancing may exist and could be contributing to increased risk of COVID-19 for Black Americans.
Another potential consideration is that non-Hispanic Black populations in the United States suffer from vitamin D deficiency at higher rates than other racial groups. In a recent comprehensive analysis of serum 25-hydroxyvitamin D (25(OH)D) levels collected from more than 26,000 adults in the United States, 71.9% of non-Hispanic Black individuals were found to suffer from vitamin D deficiency and 22.6% had vitamin D insufficiency. Of the many sociodemographic, behavioral, and clinical variables analyzed, being a racial or ethnic minority was the strongest predictor of vitamin D deficiency, with non-Hispanic Black populations suffering from vitamin D deficiency at rates 24 times more than those seen in the white population.15 Vitamin D has been suggested as a potentially mitigative factor in the COVID-19 pandemic due to its important modulatory effect on immune response.16 , 17 Furthermore, vitamin D deficiency has been implicated in numerous adverse health conditions such as acute respiratory syndromes, tuberculosis, and cardiovascular disease.18 However, no clinical evidence has shown vitamin D supplements are beneficial in prevention or treatment of COVID-19, as no randomized trials on vitamin D supplementations have been performed.19 While some registered open label trials are being performed, no results have been reported, and it is still unclear whether vitamin D is beneficial.19
Impact of environmental temperature
Environmental variables such as temperature have been studied significantly around the world, with varying results. Studies have positive correlations, negative correlations, or no correlations between rates of COVID-19 and increased temperature.4, 5, 6 Here, we demonstrate an independent effect of environmental temperature that results in reduced COVID-19 cases, but not mortality, across US counties. If warmer temperatures do, in fact, play a role in mitigating disease spread, it is reasonable to expect a potential seasonal trend in global cases. As environmental temperatures begin to warm in the Northern hemisphere during the summer months, we may begin to see a decrease in disease burden; however, we should prepare to see a resurgence in COVID-19 incidence when environmental temperatures again decrease in the fall and winter months, as has been exhibited in previous pandemics like the Spanish flu.20 Likewise, countries in the Southern hemisphere should be prepared to experience seasonal trends in the opposite direction.
The mechanism through which environmental temperature may execute its mitigative effects remains unclear, though previous studies have shown other viruses including SARS-CoV and influenza have similar associations with temperature.21, 22, 23, 24 Warmer temperatures have been associated with decreased transmission for these viruses.21, 22, 23, 24 Some suggested mechanisms include increased stability of viral particles and smaller droplets at colder climates. For droplets, colder climates are associated with lower humidity, causing smaller droplets to remain airborne for extended periods of time and increase spread.24 Lastly, while warmer temperature may or may not affect rates of COVID-19 cases and deaths, temperature alone will likely not be sufficient in halting further spread of COVID-19.25
Chronic respiratory disease and pollution
In univariate analysis, chronic respiratory disease did not significantly affect COVID-19 case and death numbers, and increased air pollution was associated with decreased COVID-19 cases. These results were unexpected given that both variables have been shown to increase risk for COVID-19.9 , 26 However, univariate analysis may be affected by confounding variables and may not represent true effects. For example, environmental temperature in this study was not significant in univariate analysis but was significant in multivariate sequential modeling. Additionally, air pollution data in this study is from 2014 and may not reflect current air pollution. Given increased social distancing, many counties with historically high air pollution levels currently have significantly decreased pollution levels, which may have decreased pollution related COVID-19 cases.27 , 28
Limitations
This study is limited by excluding counties with insufficient COVID-19 case or death data. This limitation is unavoidable and waiting for sufficient data may deter public health response. Also, the COVID-19 pandemic is still in progress and counties are at different stages. Thus, case and mortality statistics for the counties provide a snapshot of the current state, but may not, and likely will not, be reflective of the ultimate case and death tolls in these counties. Moreover, most counties are still in the early stages of accumulating deaths which axiomatically lags behind the number of cases. Since we relied heavily on publicly available sources to create our database, we used sources that may be outdated or inconsistent with the statistics during the past few months. Social distancing was measured through changes in distance travelled within US counties. While this correlates with COVID-19 cases and is an indicator of social distancing, mobility data does not capture whether people are near each other and truly social distancing. Finally, confounding effects are also possible. The stepwise approach to regression mitigates excessive confounding risk through sensitivity analysis and signifies that the findings are not error artifacts. Changing values of the linear coefficients and the logistic odds ratios indicate that Models 1 and 2 are underfitted. The consistency of Models 3 and 4 indicate that Black Race is both significant and truly associated with COVID-19 cases and deaths while Temperature is associated with COVID-19 cases, but not deaths. Ecological fallacies may be present in the model for demographic and socioeconomic variables compared to individual cases and deaths; we report as granularly as practical to account for this.
Conclusions
This study evaluated the independent effects of Black race and environmental temperature on the incidence of cases and mortality of COVID-19 at the US county level. In multivariate regression analyses that controlled for county demographics, socioeconomic factors, and medical comorbidities, counties with higher average environmental temperatures were associated with decreased COVID-19 cases, but not deaths. Black race was significantly associated with both increased cases and increased deaths. This suggests that many of the proposed mechanisms through which Black race might increase risk for COVID-19, such as socioeconomic and healthcare-related predispositions, are inadequate in explaining the full magnitude of this health disparity.
Acknowledgments
Acknowledgments
We thank Lauren Spinazze from the Unacast Group for providing us with data from their Social Distancing Scoreboard. We would also like to thank Aman M. Choudhri for his help with data acquisition.
Footnotes
The author has no financial or other conflicts of interest to disclose.
No funding sources supported this work.
References
- 1.Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48(2):155–163. doi: 10.1007/s15010-020-01401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang J, Litvinova M, Wang W. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect Dis. 2020;20(7):780–793. doi: 10.1016/S1473-3099(20)30230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhong BL, Luo W, Li HM. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Rousan N, Al-Najjar H. The correlation between the spread of COVID-19 infections and weather variables in 30 Chinese provinces and the impact of Chinese government mitigation plans. Eur Rev Med Pharmacol Sci. 2020;24(8):4565–4571. doi: 10.26355/eurrev_202004_21042. [DOI] [PubMed] [Google Scholar]
- 5.Prata DN, Rodrigues W, Bermejo PH. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ujiie M, Tsuzuki S, Ohmagari N. Effect of temperature on the infectivity of COVID-19. Int J Infect Dis. 2020;95:301–303. doi: 10.1016/j.ijid.2020.04.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5(4):e186–ee87. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 10.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England) 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yancy CW. COVID-19 and African Americans [e-pub ahead of print] Jama. 2020 doi: 10.1001/jama.2020.6548. Accessed June 25, 2020. [DOI] [PubMed] [Google Scholar]
- 12.Dorn Av, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gibbons A. How can we save black and brown lives during a pandemic? Data from past studies can point the way. Sci Mag Web. April 10, 2020 https://www.sciencemag.org/news/2020/04/how-can-we-save-black-and-brown-lives-during-pandemic-data-past-studies-can-point-way Accessed June 25, 2020. [Google Scholar]
- 14.Gould E, Shierholz H. Economic Policy Institute Website; March 19, 2020. Not everybody can work from home: black and hispanic workers are much less likely to be able to telework.https://www.epi.org/blog/black-and-hispanic-workers-are-much-less-likely-to-be-able-to-work-from-home/ Accessed April 16, 2020. [Google Scholar]
- 15.Liu X, Baylin A, Levy PD. Vitamin D deficiency and insufficiency among US adults: prevalence, predictors and clinical implications. Br J Nutr. 2018;119(8):928–936. doi: 10.1017/S0007114518000491. [DOI] [PubMed] [Google Scholar]
- 16.Braiman M. Latitude dependence of the COVID-19 mortality rate—a possible relationship to vitamin D deficiency?March 26, 2020. Available at: https://ssrn.com/abstract=3561958. Accessed June 25, 2020.
- 17.Grant WB, Lahore H, McDonnell SL. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87(4):1080s–1086s. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 19.Lee J, Van Hecke O, Roberts N. Centre for Evidence-Based Medicine Website; May 1, 2020. Vitamin D: a rapid review of the evidence for treatment or prevention in COVID-19.https://www.cebm.net/covid-19/vitamin-d-a-rapid-review-of-the-evidence-for-treatment-or-prevention-in-covid-19/ Accessed June 25, 2020. [Google Scholar]
- 20.Juzeniene A, Ma L-W, Kwitniewski M. The seasonality of pandemic and non-pandemic influenzas: the roles of solar radiation and vitamin D. Int J Infect Dis. 2010;14(12):e1099–ee105. doi: 10.1016/j.ijid.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Chan KH, Peiris JS, Lam SY. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011;2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Demongeot J, Flet-Berliac Y, Seligmann H. Temperature decreases spread parameters of the new Covid-19 case dynamics. Biology (Basel) 2020;9(5):E94. doi: 10.3390/biology9050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin K, Yee-Tak Fong D, Zhu B. Environmental factors on the SARS epidemic: air temperature, passage of time and multiplicative effect of hospital infection. Epidemiol Infect. 2006;134(2):223–230. doi: 10.1017/S0950268805005054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaakkola K, Saukkoriipi A, Jokelainen J. Decline in temperature and humidity increases the occurrence of influenza in cold climate. Environ Health. 2014;13(1):22. doi: 10.1186/1476-069X-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lipsitch M. Seasonality of SARS-CoV-2: will COVID-19 go away on its own in warmer weather? Center for Communicable Disease Dynamics Website. Available at:https://ccdd.hsph.harvard.edu/will-covid-19-go-away-on-its-own-in-warmer-weather/. Accessed June 25, 2020
- 26.Wu X, Nethery RC, Sabath BM, Exposure to air pollution and COVID-19 mortality in the United States. medRxiv 2020: 2020.04.05.20054502. [DOI] [PMC free article] [PubMed]
- 27.Dutheil F, Baker JS, Navel V. COVID-19 as a factor influencing air pollution? Environ Pollut. 2020;263 doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kann D. Los Angeles has notoriously polluted air. But right now it has some of the cleanest of any major city. CNN Website. Updated April 7, 2020. Available at: https://www.cnn.com/2020/04/07/us/los-angeles-pollution-clean-air-coronavirus-trnd/index.html. Accessed June 25, 2020