Abstract
Gastrointestinal manifestations of COVID-19 are rare and have primarily been limited to diarrhea or vomiting. Intussusception is the most common cause of bowel obstruction in infants, with up to 30% of pediatric intussusception cases having a preceding viral illness. We present the rare case of intussusception in a SARS-CoV-2 positive infant. This is the first documented case of survival in a SARS-CoV-2 positive patient presenting with intussusception as the primary manifestation. As our knowledge of this disease evolves, surgeons need to remain suspicious for possible gastrointestinal manifestations of COVID-19.
Keywords: COVID-19, Intussusception, Pediatric
1. Introduction
The COVID-19 pandemic has brought the world to a standstill, causing the loss of countless lives and wreaking financial havoc. It was first reported as a cluster of patients with severe pneumonia symptoms, linked to a seafood market in Wuhan, China. Caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), it has spread to, as of 29th May 2020, 215 countries or territories and has resulted in 5.7 million infected and over 350,000 deaths [1]. Symptoms range widely from mild, including fever, dry cough, dyspnea, myalgia, vomiting and diarrhea, to potentially fatal respiratory distress Respiratory symptoms are the most common.
Children tend to be less likely to be COVID-19 positive and are usually afflicted with milder symptoms [2]. Among 44,762 laboratory confirmed cases from China, only 416 (1%) and 549 (1%) were from age groups <10 and 10–19 years [3]. Similar statistics have emerged from the USA. Out of 22,060 COVID-19 related hospitalizations between March 1st and March 16th, 2020, only 68 (0.003%) and 91 (0.004%) fell in the 0–4 and 5–17 years age groups. The cumulative rate per 100,000 was thus 3.5 and 1.7 in 0–4 and 5-17 year-olds [4]. Furthermore, presence of symptoms was less frequent in children compared to adults, along with a shorter course of illness, as suggested by the fact that the median duration of fever was 3 days in children, compared to 10 days in adults [5]. Children with severe symptoms usually tend to have underlying medical conditions or comorbidities, with some children exhibiting an insidious onset of respiratory symptoms, only being revealed after CT scans were conducted. A case series from the UK documented 8 COVID-19 patients presenting with fever, abdominal pain and diarrhea with a working diagnosis of systemic sepsis secondary to suspected appendicitis [6]. This highlights the possible gastrointestinal complications that are possible with SARS-CoV-2 infection. Another case series of 5 pediatric patients presenting with non-respiratory symptoms was conducted in Wuhan, China. Of note, Case 1 in that series was of a 10-month-old female with intussusception who tested positive for SARS-CoV-2 [7].
Intussusception is the most common cause of bowel obstruction in infants, most commonly occurring between the ages of 4 and 10 months [8]. Viral illnesses are known to cause intussusception. Its incidence ranges between 0.24 and 2.4 per 1000 live births, while the mortality rate is 2.1 per 1 million live births in the US. However, case fatality rates are much higher in Africa (9.4%) [9].
We present the unusual case of a patient with intussusception who was subsequently diagnosed to be SARS-CoV-2 positive.
2. Case presentation
A 4 months, 25 days old baby boy presented to the emergency room at Aga Khan University Hospital (AKUH), Karachi, Pakistan, with a two-day history of acute onset, intermittent, severe, crampy abdominal pain, accompanied by inconsolable crying and drawing up of the legs towards the abdomen and reluctance to feed. Each episode occurred at an interval of 20–30 minutes and lasted for 15–20 minutes. With the passage of time, the episodes became more prolonged and severe. He had developed 2 episodes of per rectal bleeding in the preceding 24 hours which was fresh but also mixed with mucoid stool (currant jelly). He was taken to a family physician and then spent 12 hours at a government hospital being treated for gastroenteritis. There was no fever, vomiting, or diarrhea.
The child was otherwise healthy, vaccinated according to the Extended Program for Immunization (EPI) protocol, and had no significant past surgical history. However, he had recovered from an upper respiratory tract infection (URTI) with symptoms of fever, cough and rhinorrhea 1 week prior to the development of his current gastrointestinal symptoms, for which he was seen in a polyclinic by a family physician and prescribed antipyretics and supportive management.
On physical examination in the emergency room, he appeared to be a pale, irritable child. His heart rate was 136 beats per minute, he was afebrile, with an oxygen saturation of 98% and a sausage shaped lump palpable in the right upper abdomen. The rest of his systemic examination including the respiratory system and ENT was unremarkable.
2.1. Investigations
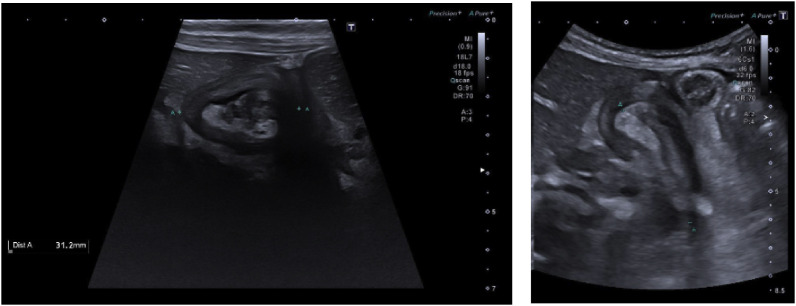
The child was found to have hypochromic microcytic anemia (Hb: 9.2 g/dL) along with a total leucocyte count of 9.9 × 109/L (raised monocytes 12.1%). Ultrasound abdomen confirmed intussusception (Fig. 1 ).
Fig. 1.
There is evidence of telescoping of bowel within the bowel loop in right upper quadrant of abdomen in the subhepatic region giving doughnut sign. Appearances are suggestive of intussusception.
2.2. Management
The patient was resuscitated in the emergency room. Broad spectrum intravenous antibiotics were administered (listed in Table 1 ) and pneumatic reduction of intussuscepted bowel (ileocolic intussusception) was performed under fluoroscopic guidance in the radiology suite after insufflation of air at 100 mm Hg for 3 minutes under two attempts. Free flow of air was observed in the large and small bowel, representing a successful reduction of intussusception. No immediate post procedure complication was noted.
Table 1.
Comparison of our patient with the patient reported by Cai et al.
| Moazzam et al. | Cai et al. | |
|---|---|---|
| Underlying disease | Intussusception | Intussusception |
| Gender | Male | Female |
| Age | 4 months, 25 days | 10 months |
| Exposure history | None | None |
| First clinical manifestation | Acute, intermittent, crampy abdominal pain, inconsolable crying, per rectal bleeding (currant jelly stool) | Paroxysmal crying, vomiting, currant jelly-like stool |
| Fever | Afebrile | Febrile (Maximum temperature = 39.8 °C) |
| Days from onset of symptoms to admission | 2 | 1.25 |
| Complications | None | Shock; MODS (liver, kidney, myocardium, DIC, acute respiratory failure |
| Treatment | ||
| Surgical | Pneumatic Reduction | Pneumatic Reduction |
| Medical |
|
|
| Length of stay (days) | 2.5 | 36 |
| Outcome | In good health one-week post-discharge | Death |
The patient was then admitted for further observation. Due to the ongoing pandemic and positive history of URTI one week prior, he was screened for SARS-CoV-2 (COVID-19) using a nasal swab (qualitative PCR) which was positive (Report as per CAP guidelines on 23rd March 2020). The child had no Covid-19 contact history.
He then underwent a chest x-ray (Fig. 2 ) which was normal, and his blood work included:
-
•
CRP:3.7 (0–10 mg/dL),
-
•
Ferritin:162.9 (22–322 ng/mL),
-
•
D-Dimer:3.8 (<0.5 mg/L FEU).
Fig. 2.
Chest radiograph AP supine projection; No evidence of any active cardiac or pulmonary disease noted.
The patient did not receive any treatment for COVID-19 as he was asymptomatic, however, the parents were advised to follow isolation protocols and return immediately upon the development of symptoms. The patient's recovery was uneventful, and his diet was established in 24 hours. He was discharged in a stable condition after a total hospital stay of 60 hours. Throughout the hospital course, he did not develop any respiratory symptoms or signs of sepsis and was recovering and in good health 1-week post-discharge.
3. Discussion
According to our literature review, this is only the second such instance of a SARS-CoV-2 positive patient presenting to a healthcare center with intussusception as the primary manifestation, and the first documented case in which the patient survived. The only other documented case was in Wuhan, China. In that particular case, the patient was a 10-month-old female who presented with fever, restlessness, vomiting and currant jelly-like stool for 30 hours. However, there were no respiratory symptoms or exposure to COVID-19. After successful diagnostic air enema, the child developed a high fever, became drowsy and developed intermittent convulsions. Signs of multiorgan failure (liver, kidney and myocardium), along with disseminated intravascular coagulation also developed. The patient subsequently tested positive for SARS-CoV-2 twice in throat swab samples. Furthermore, necrosis of the proximal ileum was discovered with subsequent resection. On day 36, the patient died due to multiorgan failure [7]. A comparison of the two documented SARS-CoV-2 positive patients who developed intussusception has been detailed in Table 1.
Although gastrointestinal symptoms have been documented in COVID-19, they are rare and have primarily been limited to diarrhea or vomiting. A review of 452 patients in 23 studies revealed that diarrhea (6.6%) and vomiting (5.8%) were far less than common than fever (43.1%) or cough (43.4%) [10]. Overall, symptoms in the pediatric population were shown to be milder in the pediatric population in a case series of 2135 patients in China. When the symptoms were classified as asymptomatic, mild, moderate, severe or critical, the distribution was 4.4%, 51.0%, 38.7%, 5.3% and 0.6% respectively. However, in children less than 1 year of age, the proportion of patients with severe or critical illness was markedly higher at 8.8% and 1.9%. As a result, it concluded that although children generally developed milder symptoms, infants in particular were vulnerable to severe or critical illness [[11], [12], [13]]. Furthermore, infants had higher hospitalization rates (15%–62%) compared to older children (1–17 years) (4.1%–14%) and adults. Multiple mechanisms for the milder symptoms have been proposed. The SARS-CoV-2 virus downregulates ACE2 expression thus impairing angiotensin-2 metabolism, which promotes lung injury. High levels of ACE-2 are present in children, thus they may be protective against severe illness [5,14,15]. Furthermore, it has been proposed that countries with routine BCG vaccination have lower COVID-19 mortality and morbidity rates [16]. As aging occurs, the regenerative capacity of lungs gradually decreases, thus the lungs in children are better placed to recover from COVID-19 [17]. Conversely, an inadequate adaptive immunity response due to an immature immune system could account for the poorer prognosis in infants compared to young children.
Viral shedding in COVID-19 patients primarily occurs through nasal secretions, however, a feco-oral route of transmission has also been postulated. This is supported by a study which found that 8 out of 10 COVID-19 positive children had positive rectal swabs, even after their nasopharyngeal swabs had turned negative [18].
Intussusception may be caused by anatomical causes, associated diseases and pertinent to this case, viral infections. However, only 10% of patients have an identifiable cause of the intussusception, with the vast majority being idiopathic. Infections can cause mesenteric lymphadenopathy and hypertrophy of Peyer patches, which can act as a lead point for the intussusceptum. Approximately 30% of pediatric intussusception cases have a preceding viral illness. Adenovirus and Rotavirus, along with some parasites, have been identified as agents which can cause intussusception [19]. A study from 1990 showed that rotavirus had a seasonal peak temperate climates while being present throughout the year in the tropics [20]. However, a subsequent large-scale review demonstrated that country income level was more predictive of the likelihood of having seasonal disease [21]. Poliovirus, enterovirus, parechovirus and norovirus have also been found in the stool specimens of affected patients [22]. After the viral illness, children tend to present with acute onset colicky abdominal pain, excessive irritability, vomiting and a “currant jelly” stool due to the presence of blood and mucus. This course is intermittent, in that the child may return to a normal level of activity in between bouts of symptoms.
Our case also followed a similar pattern, with a viral URTI illness preceding the onset of intussusceptive symptoms. This raises suspicion of SARS-CoV-2 directly affecting the gastrointestinal tract, leading to mesenteric adenitis and resulting in intussusception. This would be the first such reported incidence of intussusception as a manifestation of SARS-CoV-2 infection, with no respiratory symptoms. It is plausible that the respiratory symptoms that the child had one week prior were in fact due to SARS-CoV-2 and the intussusception episode was a delayed complication instead of a primary manifestation. Another explanation for this could be that the child had contracted an upper respiratory tract infection (URTI) of undocumented etiology and thus developed intussusception, subsequently contracting SARS-CoV-2 during the course of his visit to the government hospital whilst seeking treatment for his URTI. Furthermore, contracting SARS-CoV-2 during his stay at our hospital is highly unlikely, given that he was tested only 13 hours after admission and the child did not develop any respiratory symptoms during his hospital stay or in the week after discharge.
Testing rates in the pediatric population are much lower compared to adults and elderly globally. The WHO, CDC and numerous government health agencies emphasize fever and respiratory symptoms in the testing criteria for suspected cases [23]. Since both of these are present in less than 50% of pediatric cases [10], it raises substantial concern for underestimation of pediatric cases of COVID-19. As a result, testing rates globally must be enhanced to gauge the true disease burden and to gain a better understanding of the associated complications.
4. Conclusion
We report, to the best of our knowledge, the first documented instance of survival in a case of intussusception in a SARS-CoV-2 positive pediatric patient. Owing to the dearth of literature on this subject, further studies need to be conducted on the gastrointestinal complications associated with COVID-19. Since the knowledge of this virus is still evolving, surgeons need to remain suspicious for possible gastrointestinal manifestations of SARS-CoV-2.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient. No additional intervention was performed on the patient for the purpose of reporting. Department Head approval was obtained for publishing this report.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Funding
No funding or grant support.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.World Health Organization. WHO Coronavirus disease (COVID-19) dashboard. Covid-19 dashboard 2020:1–1. Accessed on 29th May 2020.
- 2.Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr Int J Paediatr. 2020:1–8. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. J Am Med Assoc. 2020;323:1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Coronavirus disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/covid-data/pdf/covidview-05-22-2020.pdf Available at: Accessed on 29th May 2020.
- 5.Dhochak N., Singhal T., Kabra S.K., Lodha R. Pathophysiology of COVID-19: why children fare better than adults? Indian J Pediatr. 2020;416 doi: 10.1007/s12098-020-03322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tullie L., Ford K., Bisharat M., Watson T., Thakkar H., Mullassery D. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. Lancet Child Adolesc Heal. 2020;7:19–20. doi: 10.1016/S2352-4642(20)30165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai X., Ma Y., Li S., Chen Y., Rong Z., Li W. Clinical characteristics of 5 COVID-19 cases with non-respiratory symptoms as the first manifestation in children. Front Pediatr. 2020;8:1–9. doi: 10.3389/fped.2020.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang J., Jiang B., Parashar U., Nguyen T., Bines J., Patel M.M. Childhood intussusception: a literature review. PloS One. 2013;8:1–14. doi: 10.1371/journal.pone.0068482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gluckman S., Karpelowsky J., Webster A.C., Mcgee R.G. Management for intussusception in children. Cochrane Database Syst Rev. 2017;2017 doi: 10.1002/14651858.CD006476.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cui X., Zhang T., Zheng J., Zhang J., Si P., Xu Y. Children with coronavirus disease 2019 (COVID‐19): a review of demographic, clinical, laboratory and imaging features in 2,597 pediatric patients. J Med Virol. 2020;2019 doi: 10.1002/jmv.26023. 0–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 12.Lu X., Zhang L., Du H. SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [n.d] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tezer H., Bedir Demirdağ T. Novel coronavirus disease (Covid-19) in children. Turk J Med Sci. 2020;50:592–603. doi: 10.3906/SAG-2004-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ong J.S.M., Tosoni A., Kim Y.J., Kissoon N., Murthy S. Coronavirus disease 2019 in critically ill children: a narrative review of the literature. Pediatr Crit Care Med. 2020:1–5. doi: 10.1097/PCC.0000000000002376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hossny E., El-Owaidy R. COVID-19 in children: current data and future perspectives. Egypt J Pediatr Allergy Immunol. 2020;18:3–9. doi: 10.21608/ejpa.2020.81765. [DOI] [Google Scholar]
- 16.Miller A., Reandelar M.J., Fasciglione K., Roumenova V., Li Y., Otazu G.H. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiolog- ical study. medRxiv. 2020 doi: 10.1101/2020.03.24.20042. doi: 10.1101/2020.03.24.20042. n.d. [DOI] [Google Scholar]
- 17.Navarro S., Driscoll B. Regeneration of the aging lung: a mini-review. Gerontology. 2017;63:270–280. doi: 10.1159/000451081. [DOI] [PubMed] [Google Scholar]
- 18.Xu Y., Li X., Zhu B., Liang H., Fang C., Gong Y. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsicovetere Priscilla, Jd P.A.-C., Joga Ivatury S., Mha M.D., White Brent, MD, Stefan D., Holubar, MD M Intestinal intussusception: etiology, diagnosis, and treatment. Clin Colon Rectal Surg. 2017;30 doi: 10.1055/s-0036-1593429. 003–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cook S.M., Glass R.I., LeBaron C.W., Ho M.S. Global seasonality of rotavirus infections. Bull World Health Organ. 1990;68:171–177. [PMC free article] [PubMed] [Google Scholar]
- 21.Patel M.M., Pitzer V.E., Alonso W.J. Global seasonality of rotavirus disease. Pediatr Infect Dis J. 2013;32(4) doi: 10.1097/INF.0b013e31827d3b68. e134‐e147, n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee Y.W., Yang S.I., Kim J.M., Kim J.Y. Clinical features and role of viral isolates from stool samples of intussuception in children. Pediatr Gastroenterol Hepatol Nutr. 2013;16:162–170. doi: 10.5223/pghn.2013.16.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tiago H. de Souzaa, MD, PhD; José A. Nadala, MD Ms, Roberto J. N. Nogueiraa, b, MD, PhD; Ricardo M. Pereiraa, MD, PhD; Marcelo B. Brandãoa, MD P. Clinical manifestations of children with COVID-19: a systematic review 2020. [DOI] [PMC free article] [PubMed]