Abstract
Background:
The incidence of various open shoulder procedures has changed over time. Additionally, various fellowships provide overlapping training in open shoulder surgery. There is a lack of information regarding the relationship between surgeon training and open shoulder procedure type and incidence in early career orthopedic surgeons.
Methods:
The American Board of Orthopaedic Surgery (ABOS) Part-II database was queried from 2002–2016 for reported open shoulder procedures. Procedures were categorized as follows: arthroplasty, revision arthroplasty, open instability, trauma, and open rotator cuff. We evaluated procedure trends as well as their relationship to surgeon fellowship categorized by Sports, Shoulder/Elbow, Hand, Trauma, and ‘Other’ fellowship as well as no fellowship training. We additionally evaluated complication data as it related to procedure, fellowship category, and volume.
Results:
Over the 2002–2016 study period, there were increasing cases of arthroplasty, revision arthroplasty, and trauma (P < .001). There were decreasing cases in open instability and open rotator cuff (P < .001). Those with Sports training reported the largest overall share of open shoulder cases. Those with Shoulder/Elbow training reported an increasing overall share of arthroplasty cases and higher per candidate case numbers. The percentage of early career orthopedic surgeons reporting five or more arthroplasty cases was highest among Shoulder/Elbow candidates (P < .001). Across all procedures, those without fellowship training were least likely to report a complication (OR, 0.76; 95% CI, 0.67– 0.86; P < .001). Shoulder/Elbow candidates were least likely to report an arthroplasty complication (OR 0.84, P = .03) as was any surgeon reporting five or more arthroplasty cases (OR, 0.81; 95% CI, 0.70–0.94; P= .006).
Conclusion:
The type and incidence of open shoulder surgery procedures continues to change. Among early career surgeons, those with more specific shoulder training are now performing the majority of arthroplasty related procedures and early career volume inversely correlates with complications.
Keywords: ABOS, fellowship, training, complications, shoulder, open, trends
Level of Evidence: Epidemiology Study, Large Database Analysis
As the field of orthopedics has evolved, there have been significant changes in the type and incidence of various surgical procedures. In the field of shoulder surgery, trends in the type and incidence of certain procedures continue to change as some open procedures have largely been replaced by arthroscopic or minimally invasive procedures while other open procedures such as arthroplasty are increasingly utilized. Simultaneously, the ever-increasing sub-specialization within orthopedics has changed the practice patterns of early career orthopedic surgeons performing open shoulder cases. 14 Though orthopedic surgeons with various subspecialty training perform open shoulder cases, the most significant overlap is likely between those with Sports training and those with Shoulder/Elbow training. Further analysis of open shoulder cases as it relates to fellowship training will be useful for guiding graduating residents’ expectations as well as providing orthopedic fellowships with useful information to further optimize and tailor fellowship training. Finally, this information can add more to the growing conversation correlating surgeon volume, surgeon training, and outcomes. 7,15,25,26
The purpose of this study is to evaluate trends in open shoulder procedures among early career orthopedic surgeons and to evaluate the relationship of case type and incidence to surgeon fellowship training.
We first hypothesized that there are increasing case numbers of shoulder arthroplasty and decreasing numbers of open rotator cuff surgery and open instability surgery. Secondly, we hypothesized that an increasing share of open shoulder cases are being done by orthopedic surgeons with more specific shoulder fellowship training.
We review the American Board of Orthopaedic Surgeons (ABOS) Part-II database for evaluation of these trends. After passing written Part-I board examination, candidates eligible for full board certification submit all cases during a six-month period within their first two years of active practice. This candidate-reported data is maintained by the ABOS and consists of the Current Procedural Terminology (CPT) code, International Classification of Diseases (ICD) code, year of procedure performed, patient age/sex, surgeon’s fellowship training (when applicable), and surgeon reported complications.
Methods and Materials:
Institutional review board (IRB) approval was obtained and a research proposal was submitted to the American Board of Orthopaedic Surgeons (ABOS). We queried the database initially from 2002– 2016 by CPT codes related to open shoulder procedures. We have provided general procedure trends for open shoulder cases for this time period. For specific analysis with regard to fellowship training we evaluated surgical cases performed from 2009– 2016 as there was no specific designation for Shoulder/Elbow fellowship prior to 2009 and therefore a large number of procedures fell into the “no fellowship category”. This study will thus primarily focus on the 2009–2016 data. We specifically identified common CPT codes representing “open” shoulder procedures and placed them into the following five categories: arthroplasty, revision arthroplasty, open instability, trauma, and open rotator cuff repair (Table 1). When two or more “open” shoulder CPT codes were reported in a case, we grouped based on the primary procedure code.
Table 1.
Five procedure categories with associated CPT (Current Procedural Terminology) (American Medical Association, Chicago, IL, USA) codes used for case identification.
| ARTHROPLASTY |
| 23470 Arthroplasty, glenohumeral joint; hemiarthroplasty |
| 23472 Arthroplasty, glenohumeral joint; total shoulder (glenoid and proximal humeral replacement) |
| REVISION ARTHROPLASTY |
| 23473 Revision of total shoulder arthroplasty, including allograft when performed; humeral or glenoid component |
| 23474 Revision of total shoulder arthroplasty, including allograft when performed; humeral and glenoid component |
| 23470, 23472 + one of the following ** |
| **23334 Removal of prosthesis, includes humeral or glenoid component |
| **23335 Removal of prosthesis, humeral and glenoid components (eg, total shoulder) |
| **20680 Removal of implant; deep (eg, buried wire, pin, screw, metal band, nail, rod or plate) |
| OPEN INSTABILITY |
| Soft Tissue Procedures |
| 23450 Capsulorrhaphy, anterior; Putti-Platt procedure or Magnuson type operation |
| 23455 Capsulorrhaphy, anterior; with labral repair (eg, Bankart procedure) |
| 23465 Capsulorrhaphy, glenohumeral joint, posterior |
| 23466 Capsulorrhaphy, glenohumeral joint, any type multi-directional instability |
| Bone Augmentation Procedures |
| 23460 Capsulorrhaphy, anterior, any type; with bone block |
| 23462 Capsulorrhaphy, anterior, any type; with coracoid process transfer |
| TRAUMA |
| 23485 Osteotomy, clavicle, with or without internal fixation |
| 23515 Open treatment of clavicular fracture, with or without internal or external fixation |
| 23550 Open treatment of acromioclavicular dislocation, acute or chronic |
| 23552 Open treatment of acromioclavicular dislocation, acute or chronic; with fascial graft |
| 23585 Open treatment of scapular fracture (body, glenoid or acromion), includes internal fixation when performed |
| 23615 Open treatment of proximal humeral (surgical or anatomical neck) fracture |
| 23616 Open treatment of proximal humeral fracture; with proximal humeral prosthetic replacement |
| 23630 Open treatment of greater humeral tuberosity fracture, includes internal fixation when performed |
| 23660 Open treatment of acute shoulder dislocation |
| 23670 Open treatment of shoulder dislocation, with fracture of greater humeral tuberosity |
| OPEN ROTATOR CUFF |
| 23410 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; acute |
| 23412 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; chronic |
| 23420 Reconstruction of complete shoulder (rotator) cuff avulsion, chronic (includes acromioplasty) |
Fellowship training of candidates were grouped into the following training categories: Sports, Shoulder/Elbow, Hand, Trauma, Other, and no fellowship. For those reporting two or more fellowships, we grouped into the fellowship category seemingly most specific to shoulder training (Shoulder/Elbow > Sports > Hand > Trauma > Other). For the category of “open rotator cuff’, any case that also contained an arthroscopic code was excluded. The specific revision arthroplasty codes were not widely used before 2013, thus arthroplasty codes plus hardware removal codes were additionally used to define revision arthroplasty cases prior to this. We report the number of candidates that reported at least one open shoulder procedure but have also included the number of candidates from fellowship categories taking boards that respective year for reference (Table 2). The percentages of procedures in this study are based on number of orthopedic surgeons reporting at least one open shoulder case. Additionally, the “cases per year” as reported in this study represent all cases collected over the six-month board collection period.
Table 2.
Number of candidates reporting a minimum of one open shoulder case and number of candidates ( ) from respective fellowship taking ABOS Part II same year**
| Fellowship | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | TOTAL |
|---|---|---|---|---|---|---|---|---|---|
| Shoulder/Elbow | 20(22) | 20(23) | 24(29) | 29(34) | 30(36) | 38(38) | 32(39) | 30(40) | 223(276) |
| Sports | 160(185) | 179(204) | 174(199) | 151(180) | 166(194) | 173(198) | 181(199) | 141(167) | 1325(1526) |
| Hand | 50(90) | 46 (74) | 50(102) | 43(89) | 68 (115) | 58(108) | 58(108) | 71(134) | 444(820) |
| Trauma | 37(41) | 35(41) | 53(57) | 63(73) | 59(79) | 63(73) | 50(59) | 61(68) | 421(491) |
| Other* | 62(225) | 65(219) | 63(236) | 68(234) | 68(269) | 69(254) | 69(248) | 64(284) | 528(1969) |
| None | 82(122) | 77(97) | 71(101) | 64(83) | 70(90) | 56(75) | 67(86) | 48(70) | 535(724) |
Other category includes Foot/Ankle, Adult Reconstruction, Spine, Pediatrics, and Oncology
Candidates categorized into group most specific for shoulder training if reported two or more fellowships (Shoulder/Elbow > Sports > Hand > Trauma > Other)
Finally, we evaluated surgeon reported complications as it related to procedure type and fellowship training across all procedure categories. For arthroplasty, we also assessed complication rates respective to surgeon volume.
Statistical methods:
Testing for proportion differences was performed using the chi-square test and, where appropriate, the chi-square test for trend in proportions. Odds ratios (OR) for complications were estimated using a logistic regression model. Changes in the average number of procedures per surgical candidate over time were assessed using a Poisson regression model including year as a categorical covariate. Statistical analysis was done in SAS version 9.4 and R version 3.6.0.
Results:
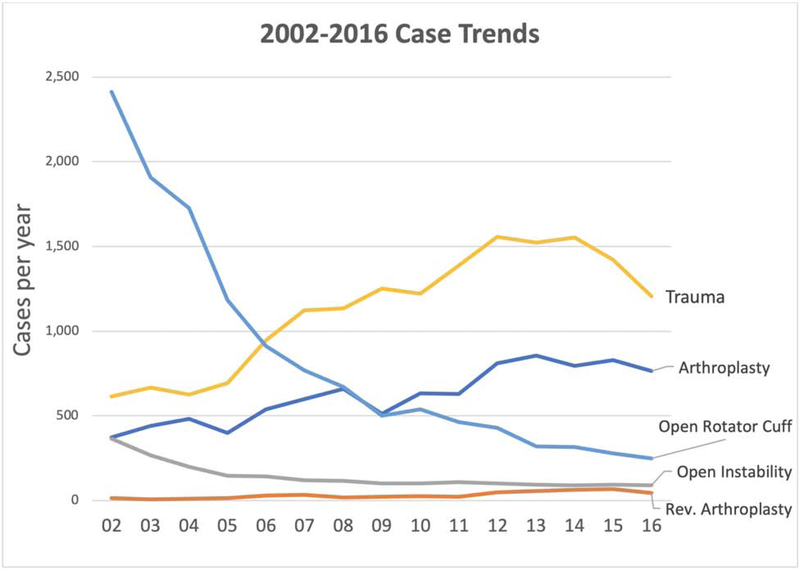
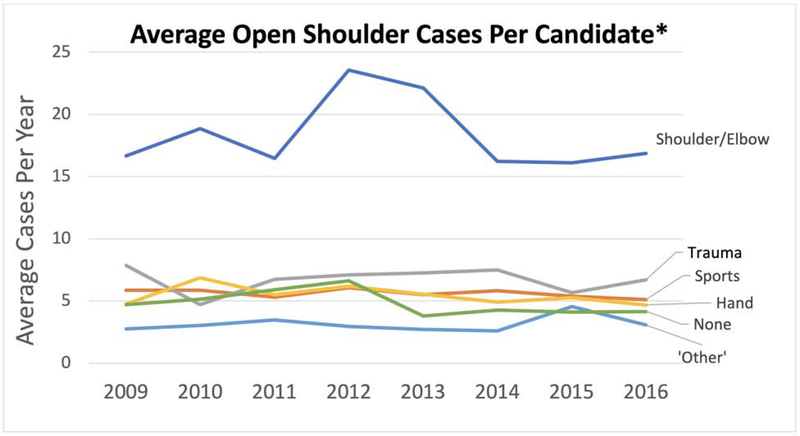
From 2002 to 2016 we identified 41,497 total open shoulder cases and these procedure trends are reported in Figure 1. From our period of primary interest 2009–2016 we identified 21,166 cases from 3,467 candidates. Post-residency fellowship training was undertaken in 2,941 (84.6%) of the candidates who reported at least one open shoulder case. The number of candidates reporting at least one open shoulder case is reported in Table 2. From 2002–2016 there were significant increases in arthroplasty (P < .001) and revision arthroplasty (P < .001) and decreases in open instability (P < .001), trauma (P < .001), and open rotator cuff (P < .001). The only trend differences in the focused 2009–2016 period were no significant change in trauma cases (P=.088) nor open instability cases (P =.085) (Figure 1). The trends in average number of open shoulder cases reported per candidate by fellowship trainings is shown in Figure 2. Over the study period there was an increase in proportion of cases reported by Shoulder/Elbow (P < .001), Hand (P = .003), Trauma (P < .001), and ‘Other’ (P =.003) candidates as well as a decrease in the number of cases reported by Sports (P < .001) candidates and those without fellowship (P < .001).
Figure 1.
Case trends from 2002–2016 for general procedure categories for open shoulder surgery among early career orthopedic surgeons.
Figure 2.
Average number of open shoulder cases reported during the 2009–2016 study period by fellowship type.
*Per candidate average is among those reporting at least one open shoulder procedure.
Arthroplasty:
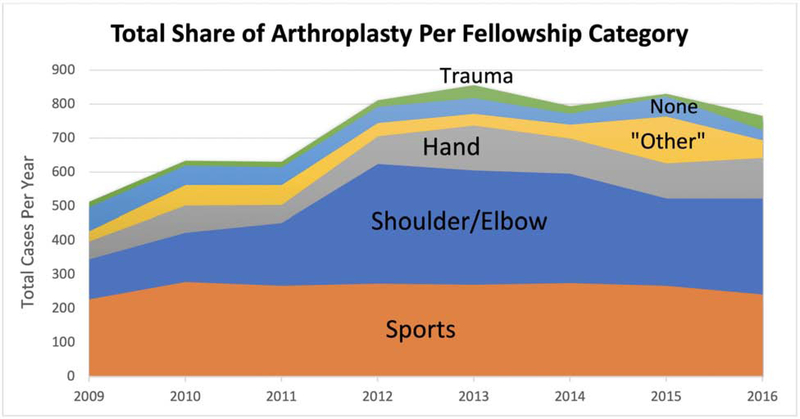
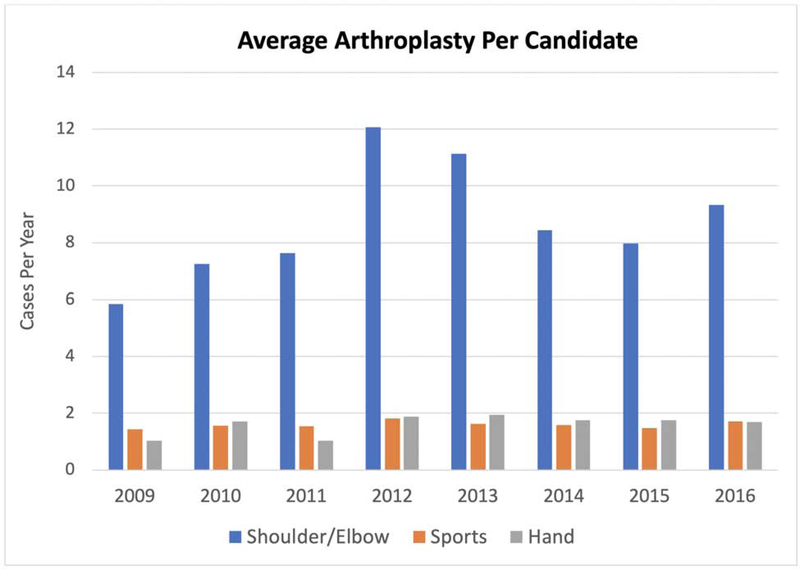
A total of 5,832 shoulder arthroplasty cases were reported from 2009–2016 with a yearly mean of 729 (range 531–895) and this increased across years (P= <.001). The trends in overall share of arthroplasty procedures from each fellowship category is reported in Figure 3. Across all years combined, those with Sports fellowship training reported the largest overall share of the arthroplasty procedures (36%) followed by those with Shoulder/Elbow training (34%). The per candidate arthroplasty numbers were highest across all years for Shoulder/Elbow candidates and increased across the study period (P < .001) (Figure 4). The following are the percentages of candidates from each fellowship reporting five or more arthroplasty cases: Shoulder/Elbow 66% (Range 55–78), Sports 11% (Range 9–14), Hand 10% (Range 6–15), ‘Other’ 4% (Range 0–6), Trauma 1.2% (Range 0–3), and no fellowship 11% (Range 9–14).
Figure 3.
Total share of arthroplasty procedure by fellowship type. Those with Sports training reported the largest share at the beginning of the study period and those with Shoulder/Elbow training reported the largest share at the end of the study period.
Figure 4.
Average arthroplasty cases per candidate from the three fellowship categories reporting the highest share or arthroplasty cases (Shoulder/Elbow, Sports, and Hand). Shoulder/Elbow reported the highest per candidate across all years (P <.001) and increases were seen in both Shoulder/Elbow and Hand per candidate averages (P <.001) but no change in Sports (P= .173). These mean case numbers are for candidates reporting at least one case, not across the entire group of fellowship candidates.
Revision Arthroplasty:
A total of 350 revision arthroplasty cases were identified during the 2009–2016 study period. There was an overall increase in revision arthroplasty during the time period with 21 cases identified in 2006 and more than doubling to 45 cases reported in 2016 (mean 43.75, range 21–67) (P < .001). The majority share of revision arthroplasty cases was reported from those with Shoulder/Elbow training (49.4%) and those with Sports fellowship training (28.2%). The remainder of cases were reported by those with Hand training (10.2%) and those with no fellowship training, Trauma training, and ‘Other’ fellowship training (12% combined).
Open Instability:
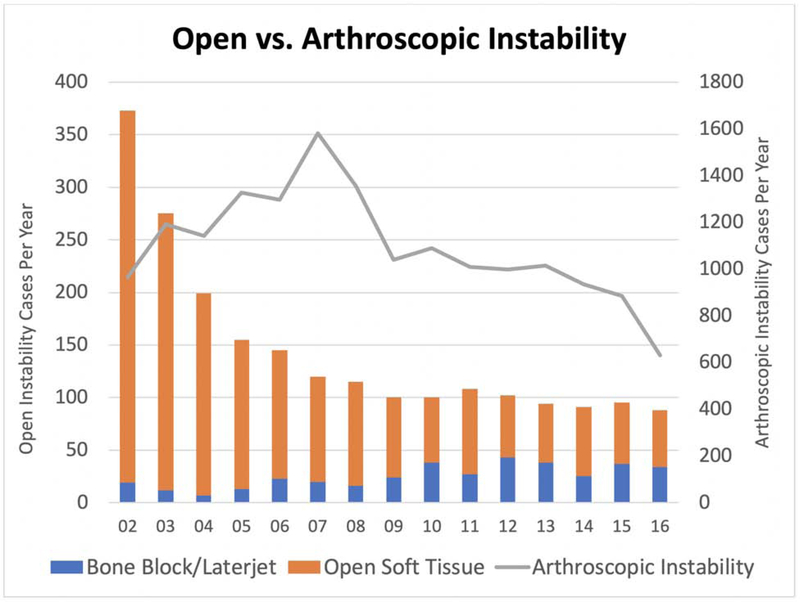
The entire data set from 2002–2016 was used to evaluate broad trends between arthroscopic instability and open instability procedures. There was a decrease in both open and arthroscopic instability cases reported (P<.001). From 2002–2016, within open instability there was a decrease in open soft tissue procedures (P<.001) and increase in bone block/Laterjet procedures (P<.001). During the focused study period from 2009–2016, 778 cases were identified as open instability surgeries but there were no significant changes across this time period in overall case numbers or between subcategories of soft tissue or bone block/ Laterjet procedures (P= .064) (Figure 5). For open soft tissue only procedures, Sports trained candidates the highest share (45.5%) of cases followed by those with no fellowship training (31.05%). Of all open shoulder categories, this was the highest share of cases reported by those with no fellowship training. For bone block/ Laterjet procedures, Sports trained candidates report a 50% share and Shoulder/Elbow reported a 35.3% share of the procedures. On a per candidate basis, Shoulder/Elbow candidates were four times more likely than the next highest (Sports) to report a bone block/ Laterjet procedure (P <.001).
Figure 5.
Trends from 2002–2016 comparing open versus arthroscopic instability surgery. The open instability category is further stratified by bone block/Laterjet and open soft tissue procedures.
Trauma:
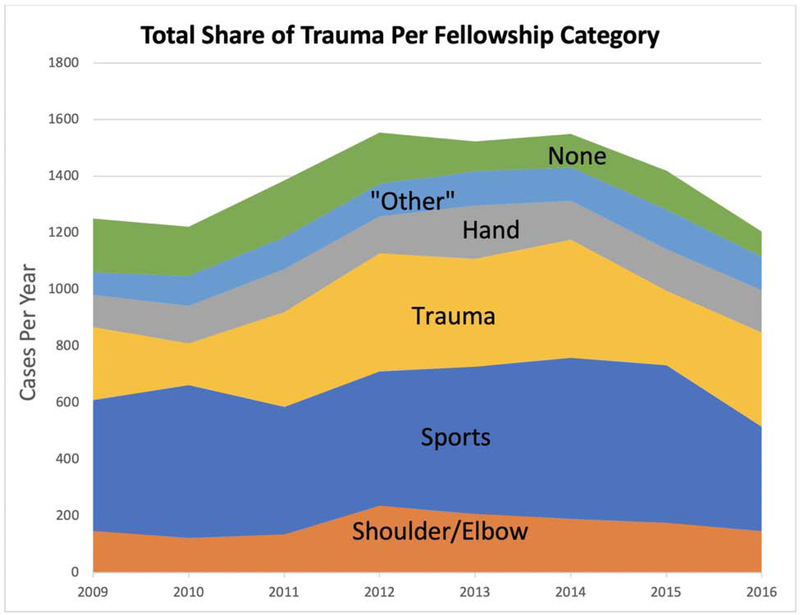
A total of 11,115 open shoulder trauma cases were identified during the 2009–2016 study period. From 2002–2016 there was a significant increase in trauma cases (P < .001) but no significant change from 2009–2016 (P = .088). The most commonly reported procedures were open treatment of clavicular fracture with 5,682 cases and open treatment of proximal humeral fracture with 3,950 cases. From the total shoulder trauma volume, Sports candidates reported 35.5% (3946) of cases, Trauma candidates reported 22.9% (2550) of cases, Shoulder/Elbow candidates reported 12.2% (1360) of cases, and the remaining 29.3% of cases were fairly evenly distributed between Hand candidates (1150), ‘Other’ candidates (908), and those with no fellowship training (1201) (Figure 6). On a per candidate basis, Shoulder/Elbow performed an average of 6.1 cases, Trauma performed 6.1 cases, Sports performed 3, and Hand performed 2.6 cases. Over the time period there was an increase in number of cases performed by those with fellowship training in Trauma (258 to 333, P < .001) and ‘Other’ (81 to 117, P = .005) categories and a decrease in Trauma cases reported by those with no fellowship (189 to 89, P < .001) and Sports fellowship (461 to 370, P = .011). On subgroup analysis of cases types, there was a sharp decline in CPT 23616 (hemiarthroplasty for fracture) from 137 cases reported to 28 cases reported. There were no significant trends in subgroups including open treatment proximal humerus fracture, open treatment clavicle fracture, and acromioclavicular reconstruction.
Figure 6.
Total share of open shoulder trauma by fellowship category.
Rotator Cuff:
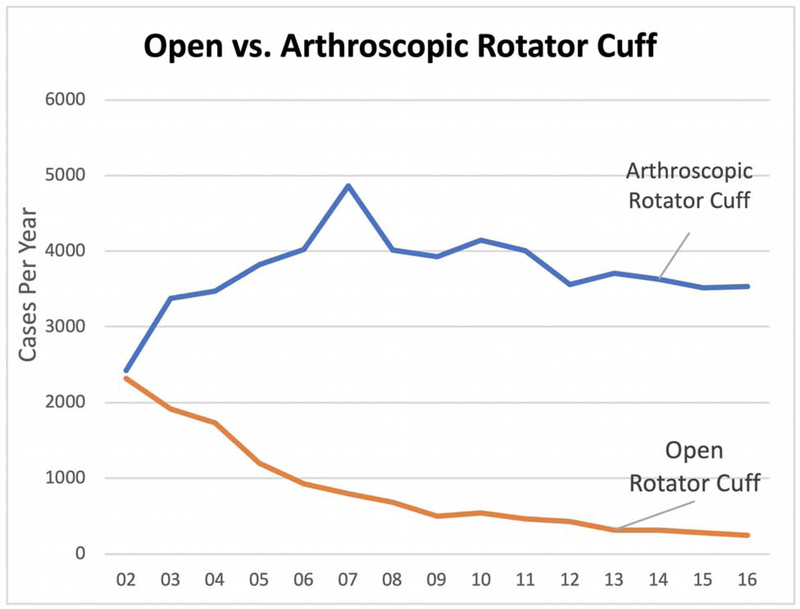
From 2002–2016 there was a significant decrease in open rotator cuff repair and an increase in arthroscopic rotator cuff repair (Figure 7). During the focused 2009–2016 study period, a total of 3,091 open rotator cuff repairs and a total of 29,318 arthroscopic rotator cuff repairs were reported. The number of open rotator cuff repairs steadily decreased from 500 cases in 2009 to 246 cases in 2016. From the total open rotator cuff case volume, Sports candidates reported 31.5% (975), those with no fellowship reported 26.9% (833), Shoulder/Elbow candidates reported 16% (495), Hand candidates reported 14.2% (440), ‘Other fellowships’ reported 7.89% (244), and Trauma candidates reported 3.4% (104) of cases. The per candidate numbers of open rotator cuff repairs decreased across all fellowship categories except those with no fellowship training (P < .001). The decreases were most significant in ‘Other’ fellowship category (72.1% decrease) and Shoulder/Elbow candidates (64.6% decrease).
Figure 7.
Trends from 2002–2016 comparing open versus arthroscopic rotator cuff procedures.
Complications:
For the 21,166 cases reported across the data set, a total of 3,293 surgical complications, 137 anesthetic complications, and 1233 medical complications were reported. The revision arthroplasty category had the highest complication rate (33%) followed by Trauma (16.7%) and arthroplasty (15%) categories. For all procedures combined, the fellowship category most unlikely to report a surgical complication was “no fellowship” (odds ratio [OR], 0.76; 95% confidence interval [CI], 0.67–0.86; P <.001) and the most likely to report a surgical complication was Trauma (OR, 1.15; 95% CI, 1.03– 1.28; P = .01). In the arthroplasty category, Trauma (OR, 1.8; 95% CI, 1.27– 2.60; P < .001) and Sports (OR, 1.17; 95% CI, 1.01– 1.28; P= .04) candidates were most likely to report a complication and Shoulder/Elbow candidates (OR, 0.84; 95% CI, 0.72– 0.99; P = .03) were least likely to report a complication. Additionally, in the arthroplasty category, those reporting five or more arthroplasty cases were less likely to report a complication than those with less than five cases (OR, 0.81; 95% CI, 0.70– 0.94; P= .006). In the open instability category, Shoulder/Elbow candidates were most likely to report a complication (OR, 2.16; 95% CI, 1.30– 3.60; P = .003). In the trauma category, Trauma candidates were least likely to report a complication (OR, 0.88; 95% CI, 0.78– 0.99; P = .04) and all other fellowships without statistical significance. Finally, in open rotator cuff, Trauma candidates were most likely to report a complication (OR, 2.19; 95% CI, 1.36– 3.52; P < .001). See Table 3 for complete data.
Table 3.
Odds ratio (with p-values) for reporting complications with respect to procedure category and fellowship. OR < 1.0 indicate lower likelihood to report complications and >1.0 indicate higher reporting of complications.
| Shoulder/Elbow | Sports | Hand | Trauma | Other | None | |
|---|---|---|---|---|---|---|
| Arthroplasty | 0.84 (0.03) | 1.17 (0.04) | 0.98 (0.84) | 1.8 (<0.001) | 0.97 (0.81) | 0.77 (0.09) |
| Open Instability | 2.16 (<0.003) | 0.87 (0.56) | 0.63 (0.41) | 2.97 (0.21) | 0.95 (0.94) | 0.46 (0.38) |
| Trauma | 1.06 (0.46) | 1.07 (0.2) | 1.08 (0.34) | 0.88 (0.04) | 0.97 (0.75) | 0.95 (0.52) |
| Open Rotator Cuff | 1.67 (<0.001) | 1.09 (0.47) | 1.18 (0.28) | 2.19 (<0.001) | 0.32 (<0.001) | 0.63 (<0.001) |
Discussion:
The first aim of this study was to evaluate the overall trends of open shoulder surgery performed by early career orthopedic surgeons over a fifteen-year period (2002–2016). Over this time period we saw increasing numbers of arthroplasty, revision arthroplasty, and trauma. There was a simultaneous and somewhat predictable decrease in open rotator cuff surgery and open instability surgery which correlates to known trends. 8,10,18,28 Specifically in the categories of arthroplasty and revision arthroplasty we saw early career orthopedic surgeons reporting increasing numbers of cases which mirrors national trends. 9 The second and primary aim of the study was to specifically evaluate trends in these procedures as they relate to fellowship training over an eight-year period (2009–2016).
In the arthroplasty category, there was a significant trend for those with more specific shoulder training performing a larger share of cases. The reason for the small decline in share of arthroplasty being performed by Shoulder/Elbow candidates after 2013 is not entirely clear but could be related to a simultaneous increase in cases done by Hand candidates. Despite the increase in arthroplasty cases reported by Hand candidates, it should be noted that approximately half of Hand candidates report any open shoulder cases and even less report arthroplasty cases. Horst et al reported that over a ten year period (2003–2013) the percentage of early career cases that fall within a candidate’s subspecialty fellowship training had risen to 81% and continues to increase. 14 The trends seen in shoulder arthroplasty are similar as surgeons with more specific shoulder training are performing an increasing share of these cases.
The reported cases of revision arthroplasty increased across the study period as would be an expected sequela of simultaneously increasing numbers of primary arthroplasty. Among all arthroplasty cases, revision cases accounted for 8.6% of cases which is similar to reported numbers. 16 There were relatively few cases in the revision category, but the majority of these cases are being performed by those with more specific shoulder training. Based on trends in this study, revision shoulder arthroplasty will continue to increase and those with more specific shoulder training will perform the majority of these cases.
In the open instability category we report increasing arthroscopic instability and decreasing open instability treatment over the longer (2002– 2016) period which has been previously reported. 4 Of all procedure categories, those with no fellowship training reported their largest share of procedures in the open soft tissue instability category. The reason for this is uncertain though certainly could be related to lack of further arthroscopic training in this area. Open soft tissue instability cases have steadily decreased from 2002–2016 while bone augmentation cases have increased. This increase is potentially attributable to increased attention to bone loss in instability surgery as well as the advent and increasing use of procedures such distal tibia allograft augmentation for glenoid bone loss. 3,20,24
In the open shoulder trauma category, there was no significant change in overall procedure volume over the 2009–2016 study period. The decrease seen in hemiarthroplasty for fracture is likely attributable to the increasing use of reverse shoulder arthroplasty (RSA) over hemiarthroplasty for fracture over this same time period. 11,23 This trend was most dramatic in those with Shoulder/Elbow training and it is plausible that surgeons with more specific shoulder training are more responsive to evidence-based changes favoring RSA over hemiarthroplasty for older patients or those not amenable to fixation. 5 The predictive factors for which candidates chose to participate in and/or have access to shoulder fracture care has yet to be defined though there are relatively high number of reported cases across all fellowship categories as well as in those without fellowship training.
The final category of open rotator cuff surgery saw significant declines in case numbers across all fellowship categories which correlates to well-known trends in this area. 2,8,10 Those with any fellowship training reported the greatest decreases in these cases when compared to those without fellowship training. In a similar finding, Amirtharaj et al reported that those without fellowship training were 35% more likely to report an open distal clavicle excision versus arthroscopic compared to those with Sports fellowship training. 1 Both such trends could be related to lack of further arthroscopic training potentially received in fellowship. Of note, some continued use of open rotator cuff repair coding could be related to the treatment of subscapularis tears which is routinely done in both open and arthroscopic fashions. 6 Nonetheless, it can be assumed that the open repair of rotator cuffs will continue to decrease, especially in early career, fellowship-trained orthopedic surgeons.
Across all procedures combined, those without fellowship training were least likely to report a surgical complication. This group also reported a higher proportion of “low risk” procedures such as instability and rotator cuff. These low rates of complications for those without fellowship training did not bear out in higher risk categories such as arthroplasty and trauma. Lower complications were reported in the arthroplasty category by those with Shoulder/Elbow training, a similar trend to what has been reported by fellowship-trained hip and knee surgeons in the field of hip and knee arthroplasty. 19 Fellowship type aside, among all candidates reporting arthroplasty cases, we found that those reporting at least five cases reported lower complication rates. Hasan et al first reported at that time in 2003 that less than 3% of orthopedic surgeons performing shoulder arthroplasty were doing at least ten arthroplasties a year. 13 Since that time, there has been much published correlating surgeon volume to patient outcomes not only in shoulder arthroplasty but across other fields of orthopedics. 7,12,17,19,21,25,26
Finally, as increasing numbers of residents continue to pursue post-graduate training through subspecialty fellowships, similar trends can be expected in the practice patterns of early career orthopedic surgeons. This information is useful for both future fellowship applicants seeking exposure to open shoulder surgery as well as for those seeking to tailor fellowship training to meet population needs. Though much remains unknown in this area, this study further elucidates the relationship between fellowship training and early career practice patterns.
The primary limitation of this study is the potential variability in coding practices. We are also limited by the six-month period of case collection in early career surgeons which might not accurately represent widespread trends and case distribution among later career surgeons. Furthermore, complication reporting is certainly limited by surgeon bias though to what degree this is affected by specialty training is unknown. Finally, the direct relationship and impact of cases done in fellowship with respect to early practice patterns needs further research.
Conclusion:
In the field of open shoulder surgery, we see changing trends with increasing numbers of shoulder arthroplasty and revision shoulder arthroplasty with decreasing numbers of open instability and open rotator cuff. Additionally, arthroplasty related procedures are being increasingly performed by those with Shoulder/Elbow fellowship training. Finally, decreased arthroplasty complications were reported in early career surgeons reporting higher case numbers in this category.
Acknowledgments
Funding
The statistical support for this research was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR002489. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH
IRB: This study was deemed to be IRB except after review by the board given the nature of the study and entirely deidentified database.
Footnotes
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Daniel P. Carpenter, Department of Orthopaedics, Washington University, Saint Louis, Missouri, USA.
Shawn D. Feinstein, Department of Orthopaedics, University of North Carolina School of Medicine, Chapel Hill, North Carolina, USA.
Eric D. Van Buren, Department of Biostatistics, University of North Carolina, Chapel Hill, North Carolina, USA.
Feng-Chang Lin, Department of Biostatistics, University of North Carolina, Chapel Hill, North Carolina, USA.
Annunziato N. Amendola, Department of Orthopaedics Duke University Medical Center, Durham, North Carolina, USA.
Robert A. Creighton, Department of Orthopaedics, University of North Carolina, Chapel Hill, North Carolina, USA.
Ganesh V. Kamath, Department of Orthopaedics, University of North Carolina, Chapel Hill, North Carolina, USA.
References:
- 1.Amirtharaj MJ, Wang D, McGraw MH, Camp CL, Degen RA, Dines DM, et al. Trends in the Surgical Management of Acromioclavicular Joint Arthritis Among Board-Eligible US Orthopaedic Surgeons. Arthroscopy 2018;34(6):1799–1805. doi: 10.1016/j.arthro.2018.01.024 [DOI] [PubMed] [Google Scholar]
- 2.Austin DC, Torchia MT, Lurie JD, Jevsevar DS, Bell J-E. Mapping the Diffusion of Technology in Orthopaedic Surgery: Understanding the Spread of Arthroscopic Rotator Cuff Repair in the United States. Clin Orthop Relat Res. 2019; Ahead of Print. doi: 10.1097/corr.0000000000000860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic bankart repair. J Bone Joint Surg AM. 2006;88(8):1755–63. doi: 10.2106/JBJS.E.00817 [DOI] [PubMed] [Google Scholar]
- 4.Bonazza NA, Liu G, Leslie DL, Dhawan A. Trends in Surgical Management of Shoulder Instability. Ortho J Sport Med. 2012;5(6):1–7. doi: 10.1177/2325967117712476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyle MJ, Youn SM, Frampton CMA, Ball CM. Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. J Shoulder Elbow Surg. 2013;22(1):32–7. doi: 10.1016/j.jse.2012.03.006 [DOI] [PubMed] [Google Scholar]
- 6.Carr A, Cooper C, Campbell M, Rees J, Moser J, Beard D, et al. Effectiveness of open and arthroscopic rotator cuff repair (UKUFF): a randomised controlled trial. Bone Joint J. 2017;99(1):107–15. doi: 10.1302/0301-620X.99B1.BJJ-2016-0424.R1 [DOI] [PubMed] [Google Scholar]
- 7.Clark JC, Simon P, Clark RE, Christmas KN, Allert JW, Streit JJ, et al. The influence of patient- and surgeon-specific factors on operative duration and early postoperative outcomes in shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(6):1011–16. doi: 10.1016/j.jse.2016.10.025450-6671 [DOI] [PubMed] [Google Scholar]
- 8.Colvin AC, Harrison AK, Flatow EL, Egorova N, Moskowitz A. National trends in rotator cuff repair. J Bone Joint Surg AM. 2012;94(3):227–33. doi: 10.2106/JBJS.J.00739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Day JS, Paxton ES, Lau E, Gordon VA, Abboud JA, Williams GR. Use of reverse total shoulder arthroplasty in the Medicare population. J Shoulder Elbow Surg. 2015;24(5):766–72. doi: 10.1016/j.jse.2014.12.023 [DOI] [PubMed] [Google Scholar]
- 10.Day MA, Westermann RW, Bedard NA, Glass NA, Wolf BR. Trends Associated with Open Versus Arthroscopic Rotator Cuff Repair. HSS J. 2019;15(2): 133–36. doi: 10.1007/s11420-018-9628-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dillon MT, Prentice HA, Burfeind WE, Chan PH, Navarro RA. The increasing role of reverse total shoulder arthroplasty in the treatment of proximal humerus fractures. Injury. 2019;50(3):676–80. doi: 10.1016/j.injury.2019.01.034 [DOI] [PubMed] [Google Scholar]
- 12.Hammond JW, Queale WS, Kim TK, McFarland EG. Surgeon Experience and Clinical and Economic Outcomes for Shoulder Arthroplasty. J Bone Joint Surg Am. 2003;85(12):2318–24. doi: 10.2106/00004623-200312000-00008 [DOI] [PubMed] [Google Scholar]
- 13.Hasan SS, Leith JM, Smith KL, Matsen FA. The distribution of shoulder replacement among surgeons and hospitals is significantly different than that of hip or knee replacement. J Shoulder Elbow Surg. 2003. March;12(2):164–69. doi: 10.1067/mse.2003.23 [DOI] [PubMed] [Google Scholar]
- 14.Horst PK, Choo K, Bharucha N, Vail TP. Graduates of Orthopaedic Residency Training Are Increasingly Subspecialized. J Bone Joint Surg Am. 2015;97:869–75. doi: 10.2106/JBJS.N.00995 [DOI] [PubMed] [Google Scholar]
- 15.Jain N, Pietrobon R, Hocker S, Guller U, Shanker A, Higgins LD. The Relationship Between Surgeon and Hospital Volume and Outcomes for Shoulder Arthroplasty. J Bone Joint Surg Am. 2004;86(3):496–505 10.2106/00004623-200403000-00006 [DOI] [PubMed] [Google Scholar]
- 16.Jain NB, Yamaguchi K. The contribution of reverse shoulder arthroplasty to utilization of primary shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(12):1905–12. doi: 10.1016/j.jse.2014.06.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mathen S, Nosrati N, Merrell G. Decreased Rate of Complications in Carpal Tunnel Release with Hand Fellowship Training. J Hand Microsurg. 2018. April 20;10(1):26–28. doi: 10.1055/s-0037-1618913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM. Surgical Trends in Bankart Repair: An Analysis of Data From the American Board of Orthopaedic Surgery Certification Examination. Am J Sports Med. 2011;39(9):1865–69. doi: 10.1177/0363546511406869 [DOI] [PubMed] [Google Scholar]
- 19.Pour AE, Bradbury TL, Horst PK, Harrast JJ, Erens GA, Roberson JR. Trends in Primary and Revision Hip Arthroplasty Among Orthopedic Surgeons Who Take the American Board of Orthopedics Part II Examination. J Arthroplasty. 2019;31(7):1417–21. doi: 10.1016/j.arth.2015.12.045 [DOI] [PubMed] [Google Scholar]
- 20.Provencher MT, Ghodadra N, LeClere L, Solomon DJ, Romeo AA. Anatomic Osteochondral Glenoid Reconstruction for Recurrent Glenohumeral Instability With Glenoid Deficiency Using a Distal Tibia Allograft. Arthroscopy. 2009;25(4):446–52. doi: 10.1016/j.arthro.2008.10.017 [DOI] [PubMed] [Google Scholar]
- 21.Ramkumar PN, Haeberle HS, Iannotti JP, Ricchetti ET. The Volume-Value Relationship in Shoulder Arthroplasty. Orthop Clinc North Am. 2018;49(4):519–25. doi: 10.1016/j.ocl.2018.05.012 [DOI] [PubMed] [Google Scholar]
- 22.Ruddell JH, Eltorai AEM, Depasse JM, Kuris EO, Gil JA, Cho DK, et al. Trends in the Orthopaedic Surgery Subspecialty Fellowship Match. J Bone Joint Surg Am. 2018;100(e139):1–9. doi: 10.5435/JAAOSGlobal-D-18-00080. eCollection 2018 Dec. [DOI] [PubMed] [Google Scholar]
- 23.Schairer WW, Nwachukwu BU, Lyman S, Craig E V., Gulotta LV. Reverse shoulder arthroplasty versus hemiarthroplasty for treatment of proximal humerus fractures. J Shoulder Elbow Surg. 2015;24(10):1560–66. doi: 10.1016/j.jse.2015.03.018 [DOI] [PubMed] [Google Scholar]
- 24.Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Shaha SH, et al. Redefining “critical” bone loss in shoulder instability. Am J Sports Med. 2015;43(7):1719–25. doi: 10.1177/0363546515578250 [DOI] [PubMed] [Google Scholar]
- 25.Singh A, Yian EH, Dillon MT, Takayanagi M, Burke MF, Navarro RA. The effect of surgeon and hospital volume on shoulder arthroplasty perioperative quality metrics. J Shoulder Elbow Surg. 2014;23(8):1187–94. doi: 10.1016/j.jse.2013.11.017 [DOI] [PubMed] [Google Scholar]
- 26.Weinheimer KT, Smuin DM, Dhawan A. Patient Outcomes as a Function of Shoulder Surgeon Volume: A Systematic Review. Arthroscopy. 2017;33(7):1273–81. doi: 10.1016/j.arthro.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 27.Wera GD, Eisinger S, Oreluk H, Cannada LK. Trends in the Orthopaedic Surgery Fellowship Match 2013 to 2017. J Am Acad Orthop Surg Glob Res Rev. 2018;2(12):e080. doi: 10.5435/JAAOSGlobal-D-18-00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zmistowski B, Padegimas EM, Howley M, Abboud J, Williams GJ, Namdari S. Trends and Variability in the Use of Total Shoulder Arthroplasty for Medicare Patients. J Am Acad Orthop Surg. 2018;26(4):133–41. doi: 10.5435/JAAOS-D-16-0072 [DOI] [PubMed] [Google Scholar]