Abstract
Interprofessional education (IPE) is a prerequisite to building a collaborative practice environment and optimizing patient care. The purpose of this systematic review was to assess the impact of IPE on outcomes related to healthcare pre-licensure learners and professionals, including: changes in attitudes/perceptions; acquisition of knowledge regarding other disciplines’ roles and development of collaborative skills; and change in collaborative behavior. We searched PubMed, CINAHL, Embase, and ERIC for studies published from 2007 to 2017 in English; nineteen studies were eligible. The Joanna Briggs Institute appraisal tool was used to assess the quality of the studies. Thirteen studies used a quasi-experimental design. The studies varied in terms of setting, teaching methods, assessment measures, and quality. Seventeen of the nineteen studies (89%) that assessed change in attitudes towards other disciplines and value placed on a team-based approach for improving patient care, found statistically significant improvements. All seven of the studies that assessed change in collaborative behavior found statistically significant improvements. Among the 12 studies that assessed development of collaborative skills, there were mixed-results. Future directions include: conducting more studies among healthcare professionals, assessing the long-term impact of IPE, objectively assessing change in collaborative behavior, and assessing the impact of IPE on patient-centered outcomes.
Keywords: systematic review, interprofessional education, interprofessional collaboration, attitudes, collaboration, behavior
Introduction
The 21st century patient population is complex with multiple comorbidities requiring an interprofessional collaborative approach to optimize care. A single disciplinary approach to patient care is costly, unsafe, and ineffective and thus the creation of interprofessional teams of healthcare providers is essential to manage complex and chronic patient care needs (Institute of Medicine, 2003). Global leaders in health care, including the World Health Organization (WHO) have created new models and are calling for collaborative action. According to the WHO (2010), collaborative practice in health-care occurs when “multiple health workers from different professional backgrounds provide comprehensive services by working with patients, their families, carers and communities to deliver the highest quality of care across settings” (p.13). The Interprofessional Collaborative Practice model has been linked with improved health outcomes (infectious and noncommunicable diseases), indicators of patient safety, mortality rate reduction, and responsiveness to epidemics (WHO, 2010; Lemieux-Charles & McGuire, 2006; Naylor et al., 2004; McAlister et al., 2004; Holland et al., 2005).
To build a collaborative care environment, there is an inherent prerequisite for Interprofessional Education (IPE) to provide purposeful education for skill acquisition and insight into a collaborative practice environment. The WHO (2010) states that IPE occurs when “students from two or more professions learn about, from, and with each other to enable effective collaboration and improve health outcomes” (p.10). The role of IPE therefore is to engage future and current healthcare providers in developing the skills to work effectively together as members of a collaborative practice-ready workforce. Ideally, IPE should be viewed on a continuum and thus commence early during pre-licensure training in the university setting and extend throughout a health professional’s career (Barr et al., 2005).
Background
Despite the importance of building a collaborative practice environment and developing IPE training, to our knowledge a systematic review has not been conducted in the past five years to evaluate the effect of IPE on collaborative practice. Barr, Koppel, Reeves, Hammick, and Freeth (2005) modified Kirkpatrick’s (1996) education evaluation typology and suggested that the levels of evidence in evaluating IPE programs, include (1) learner satisfaction, (2) modification of attitudes/perceptions and the acquisition of knowledge/skills, (3) change in behavior, and (4) change in organizational practice and the benefits to patients/clients. The impact of IPE on pre-licensure healthcare learners and professionals’ attitudes, development of collaborative skills, and change in behavior are most frequently assessed via self-report surveys and interviews (Reeves et al., 2016). Earlier systematic and scoping reviews extensively described the development and delivery of IPE but largely conducted evaluation at the participant satisfaction level (i.e., Barr et al. level 1) with fewer studies reporting changes in attitudes, knowledge, skills (Barr et al. level 2), behavior (Barr et al. level 3 evidence), or organizational practice (Barr et al. level 4a) and benefits to clients and patients (Barr et al. level 4b) (Curran et al., 2015; Fox et al., 2018; Hammick, Freeth, Koppel, Reeves, & Barr, 2007; Lapkin, Levett-Jones, & Gilligan, 2013; Reeves et al., 2016; Thistlethwaite, 2012).
The systematic reviews that evaluated IPE at level two of Barr’s typology have demonstrated inconsistent findings. Three of the reviews found that pre- and post-licensure learners’ attitudes and perceptions toward interprofessional collaboration and clinical decision-making can potentially be enhanced through IPE (Barr et al. level 2) (Lapkin et al., 2013; Reeves et al., 2016; Fox et al., 2018). However, Hammick and colleagues (2007) found IPE was less effective in affecting both pre- and post-licensure learners’ attitudes towards other health and social care professional teams. IPE was found to be effective in developing knowledge and skills for collaborative working, including understanding the roles and responsibilities of other professions (Barr et al. level 2) (Hammick et al., 2007). Two reviews also assessed whether IPE was related to changes in behavior (Barr et al. level 3), organizational practice, or benefits to patients/clients (Barr et al. level 4) but due to the small number of studies having assessed these outcomes they were unable to draw definitive conclusions (Hammick et al., 2007 & Reeves et al., 2016).
Similarly, the most recently conducted Cochrane systematic reviews have focused exclusively on the effect of practice-based interprofessional collaboration interventions on interprofessional activities (Reeves et al., 2017) and the effect of IPE on healthcare outcomes (Reeves, Perrier, Goldman, Freeth, & Zwarenstein, 2013; Reeves et al., 2008; Zwarenstein et al., 2000). Reeves and colleagues (2017), examined interprofessional collaboration interventions conducted solely in the workplace, including: interprofessional meetings, interprofessional rounds, communication tools, checklists, and externally facilitated interprofessional activities such as collaborative planning and reflection activities. The authors found that healthcare professionals’ adherence to guidelines and the use of healthcare resources may be slightly improved by interprofessional collaboration interventions. However, the certainty of evidence from the included studies (n=9) was low to very low and the authors were unable to draw definitive conclusions regarding the effects of externally facilitated interprofessional activities on quality of care, continuity of care, or collaborative working. The most recent Cochrane review assessing IPE (n=15) focused on patient healthcare outcomes and patient satisfaction but was unable to adequately assess the extent to which individuals from different health care professions behave collaboratively in the delivery of care and did not include outcomes to assess impact on attitudes, knowledge, or change in behavior (Reeves et al., 2013).
Previously conducted systematic reviews on IPE have been limited to a certain type of IPE intervention (Hammick et al., 2007) or pre-licensure learner population (Fox et al., 2018 & Lapkin et al., 2013). In addition, these reviews have largely been limited to assessing the impact of IPE on attitudes and knowledge regarding interprofessional collaboration; often demonstrating conflicting findings. The ability of IPE to effectively change collaborative practice is also unclear (Reeves at al., 2016). This systematic review contributes to the field by assessing IPE interventions delivered in a variety of educational settings and across the continuum of professional development. In particular, we aimed to determine the impact on attitudes, knowledge, skills of collaboration (Barr et al. level 2) and change in collaborative practice (Barr et al. level 3). Reeves and colleagues (2016) provided a comprehensive overview of 46 studies evaluating the impact of IPE. However, the breadth of this review limited their ability to provide extensive details on the individual interventions, measures, and outcomes. The current systematic review will add additional insight and depth on the included studies and IPE interventions.
Objective
The objective of this systematic review was to assess the impact of IPE on outcomes related to healthcare pre-licensure learners and professionals, including: changes in their attitudes and perceptions (Barr et al. level 2a); acquisition of knowledge of other healthcare professionals’ roles and development of collaborative skills (Barr et al. level 2b); and change in perceived or actual collaborative behavior (Barr et al. level 3).
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs), pre-and post-test quasi-experimental studies, and trials with mixed-methods designs were considered for inclusion in this systematic review. This review was limited to these quantitative designs as the objective was to assess a change in outcomes. In previous systematic reviews, the majority of studies employed experimental or quasi-experimental designs, usually a controlled or non-controlled pre-and post-test design (Reeves et al., 2016).
Types of participants
Studies that were considered for inclusion in this systematic review included IPE interventions that were conducted among students and professionals in health and social care disciplines, including but not limited to: physicians, pharmacists, nurses, psychologists, physical therapists, occupational therapists, dieticians, and social workers. Interventions aimed at educating faculty members were not included. Both pre-licensure health and social care students and professionals were included in this review as it is important to assess the impact of IPE along the continuum of career development.
Types of interventions
For the purposes of this review, an IPE intervention is defined as when “members of more than one health or social care (or both) professions learn interactively together, for the explicit purpose of improving interprofessional collaboration or the health/well-being (or both) of patients/clients” (Reeves et al., 2013, p. 5). Interventions taking place in a classroom, online, simulation, and/or clinical setting were considered for eligibility.
Outcomes
This systematic review will include studies that assess the impact of IPE on modification of attitudes and perceptions (Barr et al. level 2a), acquisition of knowledge and skills (Barr et al. level 2b), and behavioral change (Barr et al. level 3). These outcomes were based on Barr and colleagues (2005) IPE evaluation typology. The following operational definitions of these outcomes will be used to group the included studies under the three different outcomes in the results section (Barr et al., 2005):
Modification of attitudes/perceptions: changes in attitudes or perceptions between participant groups, changes in attitudes or perceptions towards the value and/or use of team approaches to caring for a specific client group, changes in readiness for shared expertise, and/or changes in perceived need for and/or valuing of collaboration.
Acquisition of knowledge/skills: changes in knowledge and skills linked to interprofessional collaboration such as understanding the roles and responsibilities of other professions, perceived ability to work and communicate with other professions, and competence and autonomy within one’s own profession.
Behavioral change: identifies individuals perceived or actual transfer of interprofessional learning to their practice setting.
Studies must have used a validated objective measure to be considered eligible (e.g. survey or observation checklist). Studies only using qualitative methods to explore outcomes were not considered eligible for this review.
Search methods for identification of studies
With guidance from a medical librarian we searched the following electronic databases for relevant articles published between 2000 and 2017: PubMed, CINAHL, Embase, and ERIC. The final search for each database was conducted on November 9, 2017. A detailed description of the search strategy for CINAHL is shown in Table 1. The complete search strategy, which reflects the slight differences to accommodate the unique search requirements of the different databases, can be found in Appendix 1. The search generated a total of 184 abstracts: 67 from PubMed, 67 from CINAHL, 50 from Embase, and 0 from ERIC. After duplicates were removed, 147 abstracts remained.
Table 1.
Study review CINAHL search strategy.
| Step | Search or filter details | Results |
|---|---|---|
| 1 | (MH "Education, Interdisciplinary") OR ((interdisciplin* OR interprofession* ) N3 educat* ) | 5,103 |
| 2 | (MH "Collaboration") OR collaborat* | 73,003 |
| 3 | 1 AND 2 | 1,902 |
| 4 | (MH "Attitude") OR attitude* | 239,261 |
| 5 | 3 AND 4 | 459 |
| 6 | 5 AND ((MH "Clinical Trials+") OR "clinical trial") OR (clinical N4 trial* OR random* ) OR (MH "Program Evaluation")) | 67 |
Data collection and analysis
Three authors (ES, FM, and EJ) independently reviewed the 147 abstracts retrieved by the searches, so that each abstract was reviewed twice, to identify all those eligible for inclusion. Studies were eligible for inclusion if they met the following criteria:
there was an intervention where IPE occurred between at least two health and/or social care students or professionals
the intervention was delivered in either a classroom, online, simulation, and/or clinical setting
the intervention was evaluated using either a randomized controlled trial, pre- and post-test quasi-experimental, or trial with a mixed-methods design
the impact on attitudes towards IPE and other health and social care professionals, knowledge about health and social care professionals’ roles, skills of collaboration, and/or change in collaborative behavior were assessed
outcomes were assessed using validated quantitative measurement tools.
Agreement about whether a study met the inclusion criteria was reached between the two authors who reviewed it. Thus, a third reviewer was not required to resolve conflicts. Forty-four articles were identified from this abstract search as potentially meeting these criteria.
Assessment of risk and bias in included studies
ES and BH independently assessed the risk of bias for each study using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Quasi-Experimental Studies (2016), agreement was reached between the two appraisers. The JBI checklist was selected as the majority of the included studies were evaluated using a quasi-experimental design. The JBI checklist was developed following extensive peer review, and it is also a widely used tool that provides appraisers with detailed instructions on how to evaluate each criteria, making consistency between reviewers more likely. The risk of bias assessments for each study are displayed in Supplementary Table 1. During title/abstract review, studies were excluded if they did not assess outcomes pre- and post- intervention but no studies were excluded based on bias assessment during full-text review. Sources of bias were taken into consideration when evaluating the state of the science. Many of the studies included in this review are subject to selection biases, including: volunteer and nonrespondent bias. Participants who volunteer may have more positive attitudes towards IPE and collaboration, knowledge of other health and social care professionals’ roles and skills of collaboration, and be more receptive to change in collaborative behavior at baseline than the general population or non-volunteers in comparison groups. Many of these studies also suffered from non-respondent bias, in which those who completed the surveys might differ in important ways from those who did not respond. Single group or nonequivalent group designs, such as many of the studies included in this review, also introduce selection bias. Overall, the quality of the studies included in this review were judged to be low.
Data collection
Four review authors (ES, FM, EJ, and AR) extracted relevant information from a selection of included studies. The key study characteristics extracted included: study design (RCT, pre- and post-test quasi-experimental, or trial with mixed-methods); sample characteristics (sample size, represented disciplines, sampling method); description of IPE intervention (duration, number of meetings, setting, and content); retention rate; main outcome measures; and results for the main outcomes. To ensure consistency in data extraction across authors, ES reviewed all the studies and if discrepancies were found they were resolved between authors.
Data analysis
Due to the majority of studies being of quasi-experimental design, and the vast amount of heterogeneity between interventions and outcomes, a meta-analysis of the results was not possible. Thus, the results were presented in a narrative form and organized based on Barr et al.’s (2005) education evaluation typology.
Results/Findings
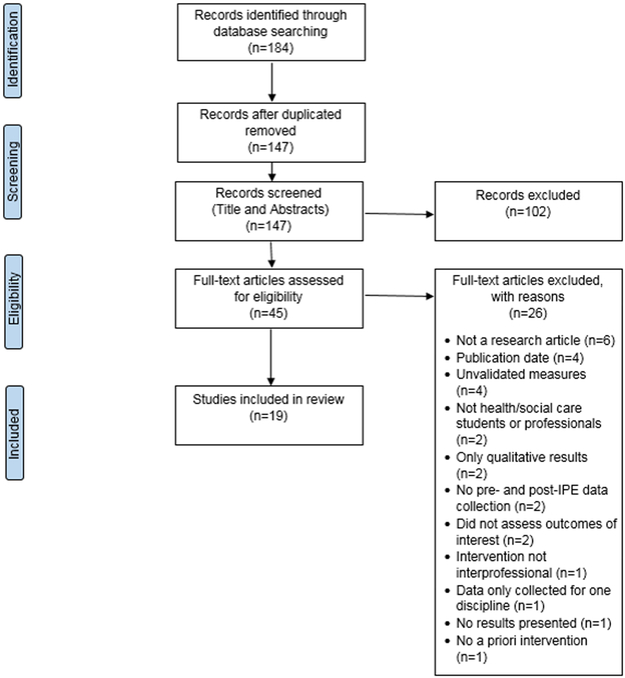
The search was further narrowed to articles published between 2007 and 2017 to reflect the current state of the science; forty articles remained for full-text review. These three reviewers then independently assessed the full-text articles to examine whether they met all of the inclusion criteria. Nineteen studies met the outlined criteria. See Figure 1 for the detailed steps taken for the selection.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses diagram depicting the flow of records.
Overview of Included Studies
A summary of the study characteristics is included in Table 2. Each individual study is summarized in Supplementary Table 2. Among the 19 studies eligible for this review, sample sizes ranged from 10 to 573 participants with six studies having samples of less than 50 participants; a power analysis was only conducted for one study (Sutherland & Moline, 2014). Retention rates, defined as both pre-and post-survey data completion, ranged from 13% to 100% (Fitzsimmons et al., 2013; Lawlis et al., 2015; Pullon et al., 2013; Sutherland & Moline, 2014).
Table 2.
Summary of Study Characteristics
| Study Characteristics | N studies (%) |
|---|---|
| Country of publication | |
| USA | 7(36.8%) |
| Canada | 5(26.3%) |
| New Zealand | 3(15.8%) |
| Australia | 2(10.5%) |
| Other | 2(10.5%) |
| Study designs | |
| Quasi-experimental w/ one group | 8(42.1%) |
| Quasi-experimental w/ two groups | 5(26.3%) |
| Mixed-methods w/ quasi-experimental quantitative arm | 5(26.3%) |
| Controlled longitudinal design | 1(5.3%) |
| Study participants | |
| Healthcare pre-licensure learners | 16(84.2%) |
| Healthcare professionals | 3(15.8%) |
IPE Interventions
The IPE interventions tested in these studies were designed to advance understanding of collaboration (n=10; Bain et al., 2014; Dacey et al., 2010; Dillon et al., 2009; DiVall et al., 2014; Eccott et al., 2012; Fernandes et al., 2015; Fitzsimmons et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012; Puskar et al., 2015) and understanding or management of a health problem (n=9; Brown et al., 2008; Cartwright et al., 2015; Darlow et al., 2015; Lawlis et al., 2015; McCaffrey et al., 2013; Pullon et al., 2013; Pullon et al., 2016; Robben et al., 2012; Sutherland & Moline, 2014). Of these nine studies, four were conducted within the context of dementia (Cartwright et al., 2015; McCaffrey et al., 2013; Lawlis et al., 2015) and elderly care (Robben et al., 2012) and two within the context of chronic disease management (Darlow et al., 2015; Pullon et al., 2013).
The interventions were conducted in a classroom, online, simulation, and/or clinical setting. Seven interventions were conducted solely in a classroom setting (Brown et al., 2008; Dacey et al. 2010, Eccott et al., 2012; Fernandes et al., 2015; McFadyen et al. 2010; Robben et al., 2012; Sutherland & Moline, 2014), two online (Cartwright et al., 2015; Puskar et al., 2015), two in simulation with debriefing (Dillon et al., 2009; Mohaupt et al., 2012), and one in a clinical setting (Lawlis et al., 2015). The other six studies combined classroom and online (Bain et al., 2014; Fitzsimmons et al., 2013), classroom and clinical (Darlow et al., 2015; McCaffrey et al., 2013; Pullon et al., 2016) and classroom, online, and clinical settings (Pullon et al., 2013). The clinical components were largely conducted as home visits or at facilities for people with dementia.
The majority of the interventions (n=14) lasted for less than 3 months (Brown et al., 2008; Cartwright et al., 2015; Dacey et al., 2010; Darlow et al., 2015; DiVall et al., 2014; Fernandes et al., 2015; McCaffrey et al., 2013; Mohaupt et al., 2012; Pullon et al., 2013; Pullon et al., 2016; Puskar et al., 2015; Lawlis et al., 2015; Robben et al, 2013; Sutherland & Moline, 2014). Of these studies, two lasted a day (DiVall et al., 2014; Mohaupt et al., 2012) and two for less than 6 hours (Puskar et al., 2015; Sutherland & Moline, 2014). Only two studies lasted for longer than three months, one for a year (Fitzsimmons et al., 2013) and one for 4 years (McFadyen et al., 2010). Three studies did not provide any information on duration of the intervention (Bain et al., 2014; Dillon et al., 2009; Eccott et al., 2012). Only one study examined the impact of the intervention over a longer follow-up period of a year (Bain et al., 2014).
Outcomes of IPE Interventions
Sixteen different scales were used across the 19 studies; however, the three most commonly used were the Readiness for Interprofessional Learning Scale (n=7), the Attitudes Towards Health Care Teams Scale (n=6), and the Interdisciplinary Education Perception Scale (n=6). Due to the heterogeneity of scales used across the reviewed studies, information regarding magnitude of improvement were not provided within the following narrative; however, this information can be found in Supplementary Table 2.
Modification of Attitudes and Perceptions (Barr et al., level 2a)
All 19 of the studies assessed changes in attitudes between participant groups, readiness for shared expertise, perceived need for and/or valuing of cooperation and collaboration, and/or changes in attitude toward the value of an interprofessional team approach to caring for patients.
Two studies reported that there were statistically significant improvements over time in pre-licensure learners and professionals’ attitudes towards other professions (Lawlis et al., 2015; Robben et al., 2012). Lawlis and colleagues (2015) also found a statistically significant improvement in perceived likelihood of meaningful learning from individuals of other disciplines. One study compared changes in attitudes between nursing and medical students and found that while nursing students already had high scores at baseline, medical students showed statistically significant improvement in viewing collaboration as important and nurses as autonomous following the IPE intervention (Dillon et al., 2009).
Five studies demonstrated statistically significant improvement in professional identity among pre-licensure learners, meaning that there was a readiness for shared expertise with other students through team-based approaches to learning as opposed to the typical discipline-based approach to learning (Darlow et al., 2015; DiVall et al., 2014; Fernandes et al., 2015; Fitzsimmons et al., 2013; McFadyen et al., 2010). In two of these studies this statistically significant improvement was larger than that seen in the comparison group (Darlow et al., 2015; McFadyen et al., 2010). McFadyen and colleagues (2010) also found that this improvement was statistically significant across professions, with occupational therapy, physical therapy, and podiatry students showing the most improvement; nursing students, were the only professional group who had not improved by year 4 of the program. One study (n=10), demonstrated borderline statistically significant improvements in professional identity among pre-licensure learners in the intervention group above that seen in the comparison group (Dacey et al., 2010). This study also found that students who were not open to shared experiences with students from other professions were less likely to be patient centered (Dacey et al., 2010).
Fourteen studies assessed change in perceived need for and/or valuing of cooperation/collaboration among pre-licensure learners and professionals from various professions (Cartwright et al., 2015; Dacey et al., 2010; Darlow et al., 2015; DiVall et al., 2014; Fernandes et al., 2015; Fitzsimmons et al., 2013; Lawlis et al., 2015; McCaffrey et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012; Pullon et al., 2013; Puskar et al., 2015; Robben et al., 2012; Sutherland & Moline, 2014). Ten of these studies showed statistically significant improvement in perceived need for and/or valuing of cooperation (Cartwright et al., 2015; Dacey et al., 2010; Darlow et al., 2015; DiVall et al., 2014; Fernandes et al., 2015; Lawlis et al., 2015; McFadyen et al., 2010; Mohaupt et al., 2012; Pullon et al., 2013; Sutherland & Moline, 2014), with three studies showing statistically significant improvement above that seen in a comparison group (Dacey et al., 2010; Darlow et al., 2015; McFadyen et al., 2010). However, only the study conducted by Darlow and colleagues (2015) was known to have comparable groups at baseline. Pre-licensure learners from all professions exhibited a more positive effect over time (McFadyen et al., 2010; Mohaupt et al., 2012); however, occupational therapy, physical therapy, and radiography students became more positive towards teamwork and cooperation as they progressed through their education. Of the four studies that did not show statistically significant improvement, one had demonstrated high perceived need and/or valuing of collaboration at baseline (Puskar et al., 2015) and three had lower scores at baseline that did not improve (Fitzsimmons et al., 2013; McCaffrey et al., 2013; Robben et al., 2012).
Five studies also demonstrated statistically significant improvement in pre-licensure learners and professionals’ perception of interprofessional teams as effective in improving patient care (Bain et al., 2014; Brown et al., 2008; Eccott et al., 2012; Pullon et al., 2013; Pullon et al., 2016) and better meeting the needs of family, caregivers, and patients above that seen in a comparison group (Pullon et al., 2016). However, in two of the studies that assessed pre-licensure learners’ attitudes, there was no improvement in viewing healthcare teams as being dependent on each other for skills and knowledge (Brown et al., 2008; Eccott et al., 2012). One study did show that pre-licensure learners’ understanding of interprofessional team work, value of their individual contribution, knowledge acquisition in interprofessional interactions, and team member role appreciation can positively impact patient care (Brown et al., 2008). These pre-licensure learners also showed improvement in valuing the importance of communication skills, confidence in working with other professionals, and the promotion of professionalism when working on interprofessional teams to improve patient care (Brown et al., 2008).
Acquisition of Knowledge and Skills (Barr et al., level 2b)
Twelve studies assessed perceived change in knowledge and skills linked to interprofessional collaboration, including: understanding roles and responsibilities of other professions, perceived ability to work and communicate with other professions, and competence and autonomy within one’s own profession (Bain et al., 2014; Cartwright et al., 2015; Darlow et al., 2015; DiVall et al., 2014; Eccott et al., 2012; Fernandes et al., 2015; Fitzsimmons et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012; Pullon et al., 2016; Puskar et al., 2015; Sutherland & Moline, 2014).
Eight of these studies reported on perceived changes regarding understanding the roles and responsibilities of other professions. Three studies showed statistically significant improvement in the understanding of roles and responsibilities of other healthcare professions among pre-licensure learners (Fernandes et al., 2015; Sutherland & Moline, 2014), with one showing greater improvement than that seen in a comparison group (Pullon et al., 2016). Four studies, one with a small sample size (n=24), found positive but statistically non-significant improvement in understanding the roles and responsibilities of other professionals (DiVall et al., 2014; Eccott et al., 2012; McFadyen et al., 2010; Mohaupt et al., 2012). One study showed no improvement among pre-licensure learners (Fitzsimmons et al., 2013). One study found statistically significant improvement in coming to view a physician-centered team structure less favorably, and while this did not remain statistically significant it remained improved one year later (Bain et al., 2014).
Five studies assessed perceived self-improvement in skills related to interprofessional collaboration and/or increased comfort in working with people from other professions (Bain et al., 2014; Cartwright et al., 2015; Darlow et al., 2015; Pullon et al., 2016; Robben et al., 2012). In a study where both the pre-and-post surveys were administered retrospectively, statistically significant perceived improvements were found in communication, collaboration, collaborative patient/family-centered approach, conflict management/resolution and team functioning among professionals, with improvements remaining statistically significant a year later (Bain et al., 2014). Five studies also found statistically significant improvements among pre-licensure learners and professionals in self-reported team skills, including: ability to communicate as well as comfort and ability to work with people from other professions (Cartwright et al., 2015; Darlow et al., 2015; Eccott et al., 2012; Pullon et al., 2016; Robben et al., 2012), with one showing greater improvement than that seen in a comparison group (Darlow et al., 2015).
Six studies found a statistically significant increase in perceived competence and autonomy among pre-licensure learners and professionals in regards to their own profession (Fernandes et al., 2015; Fitzsimmons et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012; Puskar et al., 2015; Sutherland & Moline, 2014), one of which compared results to a comparison group (McFadyen et al., 2010). This improvement did not differ significantly across pre-licensure learners from various professions (McFadyen et al., 2010; Mohaupt et al., 2012). One study found that this improvement was greater following a debriefing as opposed to just after the educational components (Puskar et al., 2015).
Behavioral Change (Barr et al., level 3)
Seven studies assessed either perceived or actual transfer of interprofessional learning to changed professional practice (Bain et al., 2014; Fernandes et al., 2015; Fitzsimmons et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012; Puskar et al., 2015; Sutherland & Moline, 2014).
Six studies demonstrated that following IPE both pre-licensure learners and professionals had statistically significant improvement in perceived actual cooperation, including whether individuals in their profession seek the advice of other professions, share resources, make efforts to understand others contributions, and work well with others (Fernandes et al., 2015; Fitzsimmons et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012; Puskar et al., 2015; Sutherland & Moline, 2014). For one study, this improvement was seen above a comparison group (McFadyen et al., 2010). This improvement in perceived cooperation was not significantly different across pre-licensure learners from the various professions (McFadyen et al., 2010; Mohaupt et al., 2012), meaning pre-licensure learners of each profession thought they had improved. In one study, improvement was greater following debriefing as opposed to just after receiving the education (Puskar et al., 2015). Only one study assessed actual improvement in team practices through observation and found a statistically significant improvement which was maintained one year later (Bain et al., 2014).
Discussion
Principal Findings
The objective of this systematic review was to assess the impact of IPE on outcomes related to healthcare pre-licensure learners and professionals, including: modifications in their attitudes and perceptions (Barr et al. level 2a); acquisition of knowledge of other healthcare professionals’ roles and development of collaborative skills (Barr et al. level 2b); and change in perceived or actual collaborative behavior (Barr et al. level 3). All of the studies assessed modifications in attitudes and perceptions (Barr et al. level 2a), 63% of the studies assessed acquisition of knowledge and skills (Barr et al. level 2b), and 37% of the studies assessed behavioral change. A variety of study designs (e.g., quasi-experimental, mixed methods, and controlled longitudinal) with a comparison group in some studies (Dacey et al., 2010; Darlow et al., 2015; McCaffrey et al., 2013; McFadyen et al., 2010; Pullon et al., 2016), a wide array of settings (e.g., classroom, online, simulation, and clinical), and generally large sample sizes were notable.
Modification of Attitudes and Perceptions (Barr et al., level 2a)
This systematic review revealed that in 17 of the 19 studies (89%) IPE was effective in improving attitudes towards pre-licensure learners and professionals of other disciplines, as well as increasing the value placed on a team-based approach for improving patient care (Barr et al. level 2a). While the overall quality of the included studies was low, the number of studies showing statistically significant improvement in attitudes and perceptions is promising. In addition, four of the five studies that compared findings across an intervention and comparison group found statistically significant improvements (Dacey et al., 2010; Darlow et al., 2015; McCaffrey et al., 2013; Pullon et al., 2016).
Acquisition of Knowledge and Skills (Barr et al., level 2b)
Results were mixed as to whether IPE is effective in improving the understanding and knowledge of roles and responsibilities of other healthcare professions with varying degrees of IPE study quality (Barr et al. level 2b). However, the three studies that compared results across groups found statistically significant improvements in the acquisition of knowledge and/or skills (Darlow et al., 2015; McFadyen et al., 2010; Pullon et al., 2016). There was a trend towards perceived improvement in collaborative skills (e.g., communication, conflict management/resolution, ability to work with others) as a result of IPE (Barr et al. levels 2b).
Behavioral Change (Barr et al., level 3)
All seven of the studies (100%) that assessed change in collaborative behavior found statistically significant improvements; however, the majority of these studies assessed change in behavior subjectively and therefore the results are subject to response bias and should be interpreted with caution (Barr et al. level 3). Only one study compared findings across two groups (McFadyen et al., 2010).
Comparison with Prior Work
The positive impact of IPE on attitudes towards students and professionals of other disciplines and a team-based approach for improving patient care was also noted in prior reviews (Fox et al., 2018; Lapkin et al., 2013). However, our findings are somewhat contradictory to Hammick and colleagues’ (2007) who found that IPE improved understanding of roles and responsibilities of other health and social care professionals. This could in part be due to differences in the quality of included studies. The current systematic review included all eligible studies regardless of quality; however, Hammick and colleagues (2007) only included high-quality studies, as determined by a five-point author team developed scale. Our mixed results might also have been due to limitations in the included IPE intervention designs (DiVall et al., 2014; Eccott et al., 2012; Fitzsimmons et al., 2013; McFadyen et al., 2010) and/or small sample size (Eccott et al., 2012). Some of the IPE intervention designs were limited by the lack of discussion surrounding the roles of other healthcare professions or because they were developed by students who may not have had a proper understanding about other disciplines.
Future Directions for IPE Research
IPE Intervention Design
Researchers and educators should consider using a rigorous IPE intervention design model (e.g., backward design) to guide curriculum/intervention development and to make sure course objectives, content, and activities/assessments are all aligned. Traditional curriculum design has course designers begin with developing the course content, often resulting in misalignment of course objectives, content, and assignments (Wiggins & McTighe, 2006). The backwards design proposes that course designers start with the desired learning goals and then derive the curriculum content to help students complete learning activities and meet the specified learning goals (Kelting-Gibson, 2005; Wiggins & McTighe, 2006; Wiggins & McTighe, 1998). Using the backwards design appears to be a stronger approach than traditional development with prelicensure teachers demonstrating increased ability to select suitable instructional goals, design coherent instruction, and assess student learning outcomes (Kelting-Gibson, 2005).
Health and Social Care Professionals Inclusion
In this systematic review, 16 of the 19 studies conducted were among pre-licensure learners. In the future, IPE should include more health and social care professionals to understand how IPE impacts organizational practice and benefits to patients/clients (Barr et al., level 4). Few previous systematic reviews have assessed the impact of IPE and interprofessional collaboration interventions among health and social care professionals in comparison to the amount conducted among pre-licensure learners (Reeves et al., 2016; Reeves at al., 2017; & Reeves et al., 2013).
Cross Professional Comparison Studies
Researchers should consider comparing findings across professions to see whether IPE has the same impact on attitudes, knowledge/skills, and behavior change regardless of profession. Only five of the studies included in this review compared findings across professions (Darlow et al., 2015; Dillon et al., 2009; McCaffrey et al., 2013; McFadyen et al., 2010; Mohaupt et al., 2012); two of which compared results across more than two professions, both of which found mixed results (McFadyen et al., 2010; Mohaupt et al., 2012).
Reduce Risk of Bias
The studies meeting the inclusion criteria for this review largely used quasi-experimental designs which are subject to concerns regarding internal validity. However, these designs are typically more practical to conduct in educational settings than RCTs. When using these designs, efforts should be made by the research teams to reduce the risk of bias by using a comparison group to which participants are assigned. Researchers should also report comparability between groups at baseline and power analyses to help readers draw more definitive conclusions.
Standardized Measurement
Sixteen different scales were used across the 19 studies. Researchers should use a widely used tool to increase homogeneity and interpretability across studies. Researchers should also consider utilizing more objective measures to assess the impact of IPE. The observation Bruyère Clinical Team Self-Assessment Scale can be used to objectively assess actual cooperation among teams (Bain et al., 2014). Objective measures will help researchers more accurately assess whether pre-licensure learners and professionals are incorporating what is taught into their practice and interactions with other health and social care professionals.
Patient-Centered Outcomes
Finally, this review was structured according to Barr et al.’s (2005) education evaluation typology. We would like to propose that patient-centered outcomes, such as patient, family, and caregiver satisfaction, be added as a level of evaluation. The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey could be used to assess whether patients are satisfied with the interprofessional care they are receiving. HCAHPS scores are publicly reported and serve as incentives for hospitals to improve their quality of care. If IPE results in more collaborative practice and subsequently improves patient satisfaction and HCAHPS scores, this may serve as an incentive for hospitals to provide IPE for professionals and further promote interprofessional teamwork.
Conclusion
Healthcare teams of the 21st century rely on the expertise of professionals from several disciplines to optimize patient care. IPE is an inherent prerequisite to building a collaborative practice environment. This systematic review demonstrated that IPE was effective in improving both pre-licensure learners and professionals’ attitudes towards other disciplines and the value placed on a team-based approach for improving patient outcomes. In addition, IPE may be effective in improving collaborative skills and changing collaborative behavior. Additional studies are needed that compare these outcomes across groups that receive the IPE and those that don’t. Future directions in IPE research include: conducting more studies among healthcare professionals, assessing the long-term impact of IPE, and objectively assessing change in collaborative behavior.
Supplementary Material
Footnotes
Declaration of Interest
The authors report no conflicts of interest.
References
- 1.Bain L, Kennedy C, Archibald D, LePage J, & Throne C (2014). A training program designed to improve interprofessional knowledge, skills and attitudes in chronic disease settings. Journal of interprofessional care, 28(5), 419–425. [DOI] [PubMed] [Google Scholar]
- 2.Barr H, Koppel I, Reeves S, Hammick M, & Freeth D (2005). Effective interprofessional education: assumption, argument and evidence. London: Blackwell. [Google Scholar]
- 3.Brown B, Warren NS, Brehm B, Breen P, Bierschbach JL, Smith R, …Van Loon RA (2008). The design and evaluation of an interprofessional elective course with a cultural competence component. Journal of allied health, 37(4), 316E–337E. [PubMed] [Google Scholar]
- 4.Cartwright J, Franklin D, Forman D, & Freegard H (2015). Promoting collaborative dementia care via online interprofessional education. Australasian journal on ageing, 34(2), 88–94. [DOI] [PubMed] [Google Scholar]
- 5.Curran V, Reid A, Reis P, Doucet S, Price S, Alcock L, & Fitzgerald S (2015). The use of information and communications technologies in the delivery of interprofessional education: A review of evaluation outcome levels. Journal of interprofessional care, 29(6), 541–550. [DOI] [PubMed] [Google Scholar]
- 6.Dacey M, Murphy JI, Anderson DC, & McCloskey WW (2010). An interprofessional service-learning course: Uniting students across educational levels and promoting patient-centered care. Journal of Nursing Education, 49(12), 696–699. [DOI] [PubMed] [Google Scholar]
- 7.Darlow B, Coleman K, McKinlay E, Donovan S, Beckingsale L, Gray B, … Pullon S (2015). The positive impact of interprofessional education: a controlled trial to evaluate a programme for health professional students. BMC medical education, 15(1), 98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dillon PM, Noble KA, & Kaplan L (2009). Simulation as a means to foster collaborative interdisciplinary education. Nursing Education Perspectives, 30(2), 87–90. [PubMed] [Google Scholar]
- 9.DiVall MV, Kolbig L, Carney M, Kirwin J, Letzeiser C, & Mohammed S (2014). Interprofessional socialization as a way to introduce collaborative competencies to first-year health science students. Journal of interprofessional care, 28(6), 576–578. [DOI] [PubMed] [Google Scholar]
- 10.Eccott L, Greig A, Hall W, Lee M, Newton C, & Wood V (2012). Evaluating students’ perceptions of an interprofessional problem-based pilot learning project. Journal of allied health, 41(4), 185–189. [PubMed] [Google Scholar]
- 11.Fernandes AR, Palombella A, Salfi J, & Wainman B (2015). Dissecting through barriers: A mixed-methods study on the effect of interprofessional education in a dissection course with healthcare professional students. Anatomical sciences education, 8(4), 305–316. [DOI] [PubMed] [Google Scholar]
- 12.Fitzsimmons A, Cisneros B, & Samore J (2014). A learner developed longitudinal interprofessional education curriculum. Journal of interprofessional care, 28(1), 66–67. [DOI] [PubMed] [Google Scholar]
- 13.Fox L, Onders R, Hermansen-Kobulnicky CJ, Nguyen TN, Myran L, Linn B, & Hornecker J (2018). Teaching interprofessional teamwork skills to health professional students: A scoping review. Journal of interprofessional care, 32(2), 127–135. [DOI] [PubMed] [Google Scholar]
- 14.Hammick M, Freeth D, Koppel I, Reeves S, & Barr H (2007). A best evidence systematic review of interprofessional education: BEME Guide no. 9. Medical teacher, 29(8), 735–751. [DOI] [PubMed] [Google Scholar]
- 15.Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, & Hay L (2005). Systematic review of multidisciplinary interventions in heart failure. Heart, 91, 899–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute of Medicine. (2003). The Future of the Public’s Health in the 21st Century. Washington, DC: National Academies Press. [Google Scholar]
- 17.Joanna Briggs Institute. (2016). The Joanna Briggs Institute Critical Appraisal tools for use in JBI systematic reviews: Checklist for quasi-experimental studies. Retrieved from http://joannabriggs.org/research/critical-appraisal-tools.html
- 18.Joyal KM, Katz C, Harder N, & Dean H (2015). Interprofessional education using simulation of an overnight inpatient ward shift. Journal of interprofessional care, 29(3), 268–270. [DOI] [PubMed] [Google Scholar]
- 19.Kelting-Gibson LM (2005). Comparison of curriculum development practices. Educational Research Quarterly, 29(1), 26. [Google Scholar]
- 20.Kirkpatrick D (1996). Great ideas revisited: Revisiting Kirkpatrick’s four-level model. Training and Development, 50(1), 54–59. [Google Scholar]
- 21.Lapkin S, Levett-Jones T, & Gilligan C (2013). A systematic review of the effectiveness of interprofessional education in health professional programs. Nurse education today, 33(2), 90–102. [DOI] [PubMed] [Google Scholar]
- 22.Lawlis T, Wicks A, Jamieson M, Haughey A, & Grealish L (2016). Interprofessional education in practice: Evaluation of a work integrated aged care program. Nurse education in practice, 17, 161–166. [DOI] [PubMed] [Google Scholar]
- 23.Lemieux-Charles L, & McGuire WL (2006). What do we know about health care team effectiveness? A review of the literature. Medical Care Research and Review, 63, 263–300. [DOI] [PubMed] [Google Scholar]
- 24.McAlister FA, Stewart S, Ferrua S, & McMurray JJ (2004). Multidisciplinary strategies for the management of heart failure patients at high risk for admission. Journal of the American College of Cardiology, 44, 810–819. [DOI] [PubMed] [Google Scholar]
- 25.McCaffrey R, Tappen RM, Lichtstein DM, & Friedland M (2013). Interprofessional education in community-based Alzheimer’s disease diagnosis and treatment. Journal of interprofessional care, 27(6), 534–536. [DOI] [PubMed] [Google Scholar]
- 26.McFadyen AK, Webster VS, Maclaren WM, & O’neill MA (2010). Interprofessional attitudes and perceptions: Results from a longitudinal controlled trial of pre-registration health and social care students in Scotland. Journal of interprofessional care, 24(5), 549–564. [DOI] [PubMed] [Google Scholar]
- 27.Mohaupt J, van Soeren M, Andrusyszyn MA, Macmillan K, Devlin-Cop S, & Reeves S (2012). Understanding interprofessional relationships by the use of contact theory. Journal of interprofessional care, 26(5), 370–375. [DOI] [PubMed] [Google Scholar]
- 28.Naylor CJ, Griffiths RD, Fernandez RS (2004). Does a multidisciplinary total parenteral nutrition team improve outcomes? A systematic review. Journal of Parenteral and Enteral Nutrition, 28, 251–258. [DOI] [PubMed] [Google Scholar]
- 29.Pullon S, McKinlay E, Beckingsale L, Perry M, Darlow B, Gray B…Morgan S (2013). Interprofessional education for physiotherapy, medical and dietetics students: a pilot programme. Journal of primary health care, 5(1), 52–58. [PubMed] [Google Scholar]
- 30.Pullon SS, Wilson C, Gallagher P, Skinner M, McKinlay E, Gray L, & McHugh P (2016). Transition to practice: can rural interprofessional education make a difference? A cohort study. BMC medical education, 16(1), 154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Puskar K, Mitchell AM, Albrecht SA, Frank LR, Kane I, Hagle H,…Talcott KS (2016). Interprofessional collaborative practice incorporating training for alcohol and drug use screening for healthcare providers in rural areas. Journal of interprofessional care, 30(4), 542–544. [DOI] [PubMed] [Google Scholar]
- 32.Reeves S, Fletcher S, Barr H, Birch I, Boet S, Davies N, McFadyen A, Rivera J, & Kitto S (2016). A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39, Medical Teacher, 38(7), 656–668. [DOI] [PubMed] [Google Scholar]
- 33.Reeves S, Pelone F, Harrison R, Goldman J, & Zwarenstein M (2017). Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, doi: 10.1002/14651858.CD000072.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reeves S, Perrier L, Goldman J, Freeth D, & Zwarenstein M (2013). Interprofessional education: effects on professional practice and healthcare outcomes (update). Cochrane Database of Systematic Reviews, (3). doi: 10.1002/14651858.CD002213.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reeves S, Zwarenstein M, Goldman J, Barr H, Freeth D, Hammick M, & Koppel I (2008). Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews, (1). doi: 10.1002/14651858.CD002213.pub2 [DOI] [PubMed] [Google Scholar]
- 36.Robben S, Perry M, van Nieuwenhuijzen L, van Achterberg T, Rikkert MO, Schers H, …Melis R (2012). Impact of interprofessional education on collaboration attitudes, skills, and behavior among primary care professionals. Journal of Continuing Education in the Health Professions, 32(3), 196–204. [DOI] [PubMed] [Google Scholar]
- 37.Sutherland SE, & Moline KA (2015). The ARCTIC workshop: an interprofessional education activity in an academic health sciences center. Journal of dental education, 79(6), 636–643. [PubMed] [Google Scholar]
- 38.Thistlethwaite J (2012). Interprofessional education: a review of context, learning and the research agenda. Medical education, 46(1), 58–70. [DOI] [PubMed] [Google Scholar]
- 39.Wiggins G, & McTighe J (2006). Understanding by design (2nd ed.). Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- 40.Wiggins G, & McTighe J (1998). Understanding by design. Upper Saddle River, NJ: Prentice Hall. [Google Scholar]
- 41.World Health Organization. (2010). Framework for Action on Interprofessional Education and Collaborative Practice. Geneva: World Health Organization. [PubMed] [Google Scholar]
- 42.Zwarenstein M, Reeves S, Barr H, Hammick M, Koppel I, & Atkins J (2001). Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews, (3). doi: 10.1002/14651858.CD002213 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.