Abstract
Objectives:
The aim of this in vitro study was to test the effect of different composite modulation protocols (pre-heating, light-curing time and oligomer addition) for bulk filling techniques on resin polymerization stress, intra-pulpal temperature change and degree of conversion.
Methods:
Class I cavities (4 mm depth × 5 mm diameter) were prepared in 48 extracted third molars and divided in 6 groups. Restorations were completed with a single increment, according to the following groups: 1) Filtek Z250XT (room temperature – activated for 20 s); 2) Filtek Z250XT (at room temperature – activated for 40 s); 3) Filtek Z250XT (pre-heated at 68°C – activated for 20 s); 4) Filtek Z250XT (pre-heated at 68°C – activated for 40 s); 5) Filtek BulkFill (at room temperature – activated for 20 s); 6) Filtek Z250XT (modified by the addition of a thio-urethane oligomer at room temperature – activated for 40 s). Acoustic emission test was used as a real-time polymerization stress (PS) assessment. The intra-pulpal temperature change was recorded with a thermocouple and bottom/top degree of conversion (DC) measured by Raman spectroscopy. Data were analyzed with one-way ANOVA/Tukey’s test (α=5%).
Results:
Pre-heating the resin composite did not influence the intra-pulpal temperature (p=0.077). The thio-urethane-containing composite exhibited significantly less PS, due to a lower number of acoustic events. Groups with pre-heated composites did not result in significantly different PS. Filtek BulkFill and the thio-urethane experimental composite presented significantly higher DC.
Significance:
Resin composite pre-heating was not able to reduce polymerization stress in direct restorations. However, thio-urethane addition to a resin composite could reduce the polymerization stress while improving the DC.
Keywords: Dental restoration, Polymerization stress, Pre-heating, Composite resins, Thio-urethane additives
1. Introduction
Dental resin composites are widely used for adhesive restorative procedures, more so nowadays due to the significant improvement in their physical and mechanical properties compared to the early materials [1]. However, volumetric shrinkage is still an inherent drawback of the polymerization of the resin matrix [1,2]. The decrease in free volume around monomers during the polymerization reaction causes macroscopic shrinkage of the material [1,2]. In this way, volumetric shrinkage induces stress at the surface to which the resin composite is being adapted [1]. Although volumetric shrinkage is related to polymerization stress, other factors including elastic modulus, gelation point and final conversion can also influence polymerization stress [2–4]. The effect of the polymerization stress generated during placement of direct restorations can lead to microleakage, cuspal deflection, cuspal fractures, and marginal defects [5–9]. Therefore, reducing polymerization stress through multiple protocols and techniques during composite resin placement or new material development is a constant research aim.
Pre-heating of composite resins has been shown to modify some of the material properties. At higher temperatures resin viscosity is reduced and higher conversion can be achieved [10, 11]. In addition, monomer mobility is increased, which favors propagation and termination events, leading to higher polymerization rate [12]. Some other practical strategies might include alternative curing protocols, such as increasing light exposure time [13]. As a result of higher conversion or extended curing time, an unfavorable increase in polymerization stress or intrapulpar temperature could be expected [14]. Despite this, significant stress relaxation was observed when a resin composite is heated to 60°C [15]. Stress relaxation during conversion is possible due to viscous flow or chain relaxation [16]. Moreover, as conversion increases, better mechanical properties are also expected [17]. Therefore, there is a possibility that pre-heated resin composites could be used in bulk placement with reduced polymerization stress.
The continuous search for a material that is simply and rapidly placed with reduced polymerization shrinkage has led to the development of bulk-fill composite resins: a range of materials with several changes in the chemistry and concentration of monomers, addition of new photoinitiators, modified inorganic content and increased translucency, which allowed those materials to be placed and photo-polymerized in a single layer of 4–5 mm thickness [3, 13].
Another composite modulation protocol includes thio-urethane additives in dental resins, with the aim of reducing polymerization stress and increasing toughness in crosslinked materials. Thio-urethanes are oligomers with pending thiols from the backbone, through which they are able to establish covalent interactions with a methacrylate matrix [18]. The multiple thiol functionalities pendant from the oligomer undergo chain-transfer events with the methacrylate, creating crosslinks while at the same time leading to delayed network formation. This delayed gelation/vitrification, in turn, leads to increased final conversion and viscous flow, ultimately leading to lower stress [19]. Indeed, studies testing experimental and commercial composites modified with thio-urethanes have reported significant stress reduction combined with increased degree of conversion and mechanical properties [18, 20–22]. A recent study also suggested filler functionalization with thio-urethane, which could be an alternative for improving mechanical properties, conversion and reducing polymerization stress [23]. Although several studies reported important properties improvement with these new additives, no studies have tested them as bulk-fill materials against commercially available materials. If thio-urethane modified composites present similar or higher stress reduction than commercial bulk-fill composites, a new class of low-stress materials with even higher mechanical properties could be achieved. Testing a thio-urethane modified composite against a commercial bulk-fill composite in high C-factor (Class I and II) cavities should help clarify if this mechanism of stress reduction works better than the ones available on the market.
Therefore, the aim of this in vitro study was to evaluate the effect of different modulation protocols (i.e. using a pre-heated resin and a thio-urethane modified version of this material) for bulk techniques on resin polymerization stress, intra-pulpal temperature change and degree of conversion. A conventional resin composite was used at room temperature and pre-heated at 68°C and compared to a high viscosity bulk-fill resin composite. The tested hypotheses were: 1) pre-heating would reduce the polymerization stress and increase the degree of conversion; 2) there is no difference on the polymerization stress reduction between a thio-urethane modified resin composite and a bulk-fill resin composite.
2. Materials and methods
2.1. Thio-urethane synthesis and filler silanization
A thio-urethane was synthetized for this study by combining 4,4-methylene bis(cyclohexyl isocyanate), trimethylol-tris-3-mercaptopropionate and 3-(Triethoxysilyl) propyl isocyanate (2:1:1 mol ratio) in 60 ml of methylene chloride at room temperature. Triethylamine was used to catalyze the reaction and oligomers were purified by precipitation in hexane. All chemicals were purchased from Sigma Aldrich (Madison, WI, USA). A rotary evaporator (R-100, Buchi Corporation, New Castle, DE, USA) was used for solvent removal. Solvent evaporation was done at 32°C for 2:30 h. Formation of thio-urethane bonds and absence of starting materials was verified by H-NMR and mid-IR spectroscopy as previously described [20].
A glass filler was silanized with the synthetized thio-urethane. The silanization process was performed in an ethanol/distilled water solution (80%/ 20%). Glacial acetic acid was added to adjust the pH to 4.5. After this, 2 wt% of the oligomer was added to the ethanol/water silanizing solution together with 0.7 μm unsilanized barium-aluminium-borosilicate-glass filler (GM27884 – Schott AG, Landshut - Germany). The solution was kept under mechanical agitation for 24 hours, filtered and dried for 4 days in an oven at 37°C. A thio-urethane-silanized filler was obtained for the experimental resin composite.
2.2. Thio-urethane-modified composite
One commercial resin composite (Z250XT, 3M ESPE, St Paul, MN, USA) was used as the base for thiourethane addition. Considering that this composite has an organic content of 18 wt%, the oligomer was added in relation to the mass of resin matrix. Previous studies have reported good properties improvement with the addition of 20 wt% of thio-urethane in relation to the resin matrix weight [18], so that concentration was selected for this study. Since adding the thio-urethane leads to an overall decrease of the filler loading, additional filler silanized with the thio-urethane was incorporated so that the final material presented 82 wt% filler loading, to achieve similar loading to the original commercial material.
2.3. Cavity preparation
Forty-eight freshly extracted human third molars were used in this study. Teeth were stored refrigerated in 0.5% chloramine-T solution before use. All teeth were extracted due to therapeutic reasons and the protocols used were approved by the local ethics committee review board (46562215.6.0000.5347).
Roots were removed using a low-speed diamond saw by performing a cut 3 mm below the cement-enamel junction. Pulpal tissue was gently removed with a dentin excavator to clear the pulpal chamber. After this, a small hole was made with a round diamond bur next to the cement-enamel junction to create a lateral access to the pulpal chamber. Occlusal 4-mm deep class I cavities (C-factor=5) were prepared with a large round end taper diamond bur (#3131 – KG Sorensen, Cotia, SP, Brazil). A 5-mm diameter round template was placed over the center of the occlusal surfaces to establish the conformation of the cavity preparation. Cavities were manually prepared with a high-speed handpiece using water spray refrigeration and the dimensions were checked with a probe during the preparation. Teeth were numbered from 1 to 48 and randomly assigned by drawing to one of the 6 experimental groups.
2.4. Polymerization stress (PS)
Before the restoration procedure samples were attached to a WDI differential acoustic emission sensor from Physical Acoustics Corporation (PAC) (Figure 1) in order to determine the polymerization stress of the composites. Root surfaces were attached to the sensors with cyanoacrylate adhesive. Three channels from a PAC Disp 16C acoustic emission system were used to record acoustic events generated by PS. Each channel was connected to a different acoustic sensor of the same model and pre-amplified with a 60dB gain. Sensor 1 and 2 were used as guard sensors to detect false calls: the first from a sensor with a free surface and the second received the signal from a sensor with a non-testing tooth. Sensor 3 received the signal from the sensor where the testing tooth was attached. After the test, signals recorded from second and third sensors were used to compare and remove false signals from the environment. A threshold of 32dB was used for all the channels. The number of acoustics events (AE) and their respective amplitudes were recorded from the start of light curing until 20 minutes after. The resulting signals were filtered and reported as total AE and AE higher than 60 dB (AE>60 dB).
Figure 1.
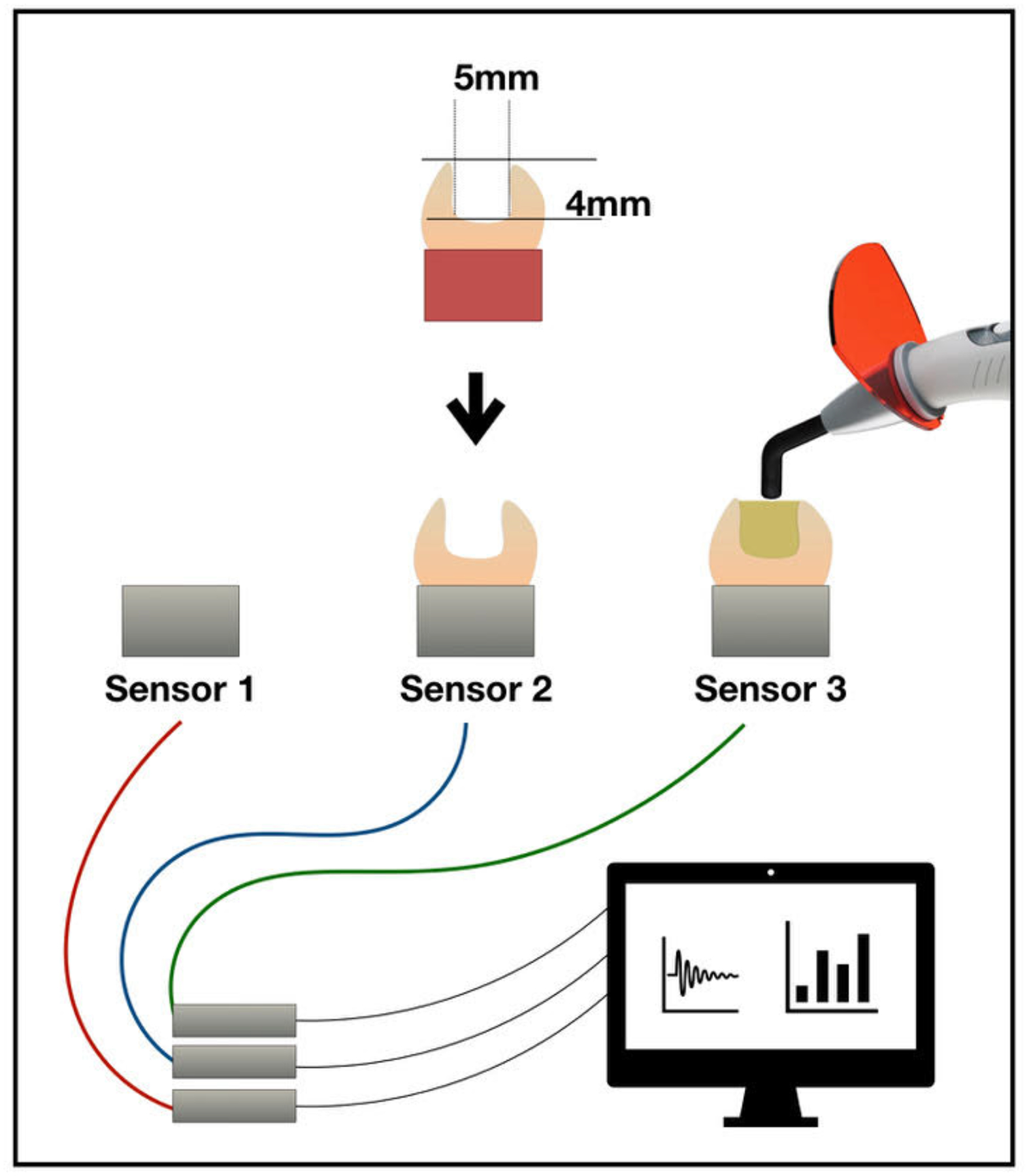
Schematic diagram of the Acoustic Emission test set-up with two guard and one test sensors. The three tests (sensor alone, sensor with empty tooth on top, and the complete assembly – in the Figure from left to right) were conducted simultaneously to avoid the recording of false call signals.
2.5. Intra-pulpal temperature
The remaining dentin thickness at the pulpal floor was measured with a caliper at 3 different spots. A mean remaining dentin thickness was calculated for each tooth and group to avoid different test conditions. The pulpal chambers were filled with thermal conducting paste (Implastec Eletrochemistry, Votorantim, SP, Brazil). A K type thermocouple sensor connected to a CPM-45 thermometer (Contemp, São Caetano do Sul, SP, Brazil) was inserted inside the pulpal chamber through the lateral hole near the cement-enamel junction. Tests were conducted in a controlled temperature room with constant baseline temperatures. Temperature changes (Δt) were recorded between the start of light curing and the maximum temperature reached. Temperature changes during adhesive activation were also recorded.
2.6. Restorative procedures
After being attached to the AE sensor, teeth were restored according to the different experimental groups. Description of the materials used are detailed in Table 1. A universal adhesive (SingleBond Universal, 3M ESPE, St Paul, MN, USA) was used in self-etch mode in dentin and in selective etch mode in enamel, for 30 seconds (Scotchbond Universal Etchant, 3M ESPE, St Paul, MN, USA). Enamel was washed with water spray for 30 seconds and cavities were dried with cotton pellets. The adhesive was applied for 20 seconds with active scrubbing. Solvent evaporation was performed with 10 seconds of gentle air. A LED curing light (Emitter, Schuster, RS, Brazil) was used for 10 seconds, at 1mm from the cavosuperficial border. Light irradiance was checked with a radiometer (LM-1, Woodpecker, Guilin, China) throughout the study. Constant light irradiance at the tip of the instrument (1300 mW/cm2) was observed during all the experiment. Two composite materials (Filtek Z250XT and Filtek BulkFill, 3M ESPE, St Paul, MN, USA) were divided into 6 experimental groups. Cavities were bulk filled according to the following groups:
Filtek Z250XT at room temperature – Activated for 20 seconds
Filtek Z250XT at room temperature – Activated for 40 seconds
Filtek Z250XT at 68°C – Activated for 20 seconds
Filtek Z250XT at 68°C – Activated for 40 seconds
Filtek BulkFill at room temperature – Activated for 20 seconds (according to manufacturer instructions)
Filtek Z250XT w/ thio-urethane at room temperature – Activated for 40 seconds
Table 1.
Materials under investigation (information as disclosed by the manufacturer).
| Product | Type | Manufacturer | Composition |
|---|---|---|---|
| Scotchbond Universal Etchant | Phosphoric acid etching gel | 3M ESPE | 32% by weight phosphoric acid, water, poly (vinyl alcohol) |
| SingleBond Universal | Universal adhesive | 3M ESPE | HEMA; Bis-GMA; Dimethacrylate resins; ethanol; silane treated silica; water; 2-propenoic acid; 2-Methyl-; reaction products with 1,10-decanediol and phosphorous oxide; copolymer of acrylic and itaconic acid; CQ; 2,6-di-tert-butyl-P-cresol |
| Filtek Z250XT (also known as Filtek Supreme Ultra and Filtek Supreme XTE) |
Nano filled conventional composite resin | 3M ESPE | Bis-GMA, UDMA,TEGDMA, Bis-EMA, silanated silica, silanated zirconia, photoinitiators |
| Filtek BulkFill Restorative | High-viscosity nano filled bulk-fill composite resin | 3M ESPE | AFM, AUDMA, UDMA, DDDMA, Ytterbium trifluoride, nonaggregated silica, nonaggregated zirconia, zirconia/silica clusters |
Abbreviations: HEMA (2-hydroxyethyl methacrylate); bis-GMA (bisphenol-A glycidyldimethacrylate); CQ (camphorquinone); AFM (addition fragmentation monomer); AUDMA (aromatic urethane dimethacrylate); bis-EMA (Ethoxylated bisphenol-A dimethacrylate); DDDMA (1, 12-Dodecanediol dimethacrylate); TEGDMA (Triethyleneglycol dimethacrylate); UDMA (urethane dimethacrylate).
For groups with pre-heated material, compules were loaded with resin composite and placed inside a composite heating device (Calset, AdDent, Danbury, CT, USA) set to 68°C for at least 5 minutes to stabilize the compule temperature inside the device. A Centrix syringe was used to deliver the resin composite inside the cavity in a single increment. Time was controlled so that each restoration had to start the light activation at 1 minute after removing the compule from the heating device. This was done to standardize the amount of heat loss for every group, which has been estimated to be around 10 °C/min [24].
2.7. Degree of conversion
After being restored, teeth were sectioned in 1 mm slices with a low-speed diamond saw under water irrigation. Slices were analyzed with micro-Raman spectroscopy (Senterra, Bruker Optik GmbH, Ettlingen, Germany). An initial spectrum was collected for each unpolymerized resin composite to identify and compare the reaction peaks by a 100-mW diode laser with 785-nm wavelength. Five samples from each group were analyzed to calculate the degree of conversion. Only central slices from restorations were used to standardize for light exposure. One reading 50 μm from the top surface and one from the bottom surface of the restoration were recorded. The aromatic peak, observed at 1,610 cm−1, was used as the reference peak and the vinyl peak, observed at 1,640 cm−1, as the reaction peak. The degree of conversion was calculated using the ratio between the reaction and internal reference peak areas as the ratio of polymerized to unpolymerized resin composite. The DC was calculated according to the formula:
2.8. Statistical analysis
The IBM SPSS Statistics for Windows (Version 20.0. IBMCorp., Armonk, NY, USA) was used to perform all the statistical analysis. Data from polymerization stress and degree of conversion evaluations were tested for normal distribution (Anderson-Darling test) and equal variances (Bartlett and Levene tests), and analyzed with one-way ANOVA and Tukey’s test (α=5%). T-tests compared Filtek Bulk Fill and Z250 XT TU at the two different light exposure times (α=5%) and degree of conversion top and bottom results. For intra-pulpal temperature, one-way ANOVA and Tukey post-hoc tests were used (α=0.05).
3. Results
3.1. Intra-pulpal temperature
Table 2 shows remaining dentin thickness on the pulpal floor and intra-pulpal temperature change during the restorative procedures. Pulpal dentin thickness was similar for all groups (p=0.834). Pre-heating the resin composite did not influence the intra-pulpal temperature change when groups subjected to the same light exposure time are considered (p=0.077). Z250XT 68°C 40s presented significantly higher temperature change, with no statistical difference to the other two groups activated for 40s. There was no statistical difference on temperature changes between adhesive polymerization and restorations light-cured for 20 seconds (1.9±0.6 °C). Thio-urethane-containing and bulk-fill composites presented the same intra-pulpal temperature change.
Table 2.
Remaining pulpal dentin thickness and intra-pulpal temperature variations during restorative procedures. Values followed by the same superscript on the same column are statistically similar (α=5%).
| Pulpal dentin thickness | Δt °C (total) | |
|---|---|---|
| Adhesive only* | 1.9 (0.6) B | |
| Z250XT 20s | 1.7 (0.6) A | 1.7 (0.5) B |
| Z250XT 40s | 1.7 (0.6) A | 2.4 (1.2) A,B |
| Z250XT 68° 20s | 1.9 (0.7) A | 1.7 (0.3) B |
| Z250XT 68° 40s | 1.7 (0.6) A | 3.2 (0.7) A |
| Filtek BulkFill 20s | 1.8 (0.7) A | 1.4 (0.1) B |
| Z250XT TU 40s | 2.0 (0.7) A | 2.5 (0.9) A,B |
average of all cavities used in this study (prior to resin composite insertion).
3.2. Polymerization stress (PS)
Acoustic emission results are presented in Table 3. The experimental composite containing thio-urethane exhibited significantly less total AE and AE>60 dB compared with the groups exposed for 40 s. For total AE, Filtek BulkFill presented significantly more events than all groups. Pre-heat treatment and exposure time did not influence the polymerization stress nor the AE>60 db when only the non-modified Z250 XT groups are considered (p>0.05). Thio-urethane-containing and bulk-fill composites showed no statistical difference on PS. Figure 2 shows the cumulative number of AE over time for all samples of each group. An acceleration on the cumulative number of AE was observed for pre-heated groups. However, this pattern was not observed neither when the thio-urethane experimental composite nor increased light-curing exposure time were evaluated. On the other hand, acceleration on the cumulative number of AE was observed for the bulk-fill resin composite.
Table 3.
Mean and standard deviation for total Acoustic Events (AE) and for AE greater than 60 dB from start of light curing until 20 minutes after. Values followed by the same superscript on the same column are statistically similar (α=5%).
| AE total | AE>60 dB | |
|---|---|---|
| Z250XT 20s | 42.4 (19.3) AB | 4.6 (4.2) AB |
| Z250XT 40s | 56.5 (16.4) A | 5.4 (2.1) A |
| Z250XT 68° 20s | 49.9 (27.1) AB | 4.1 (3.9) AB |
| Z250XT 68° 40s | 63.5 (32.9) A | 5.9 (3.6) A |
| Filtek BulkFill 20s | 214.1 (127.2) * | 3.5 (3.2) AB |
| Z250XT TU 40s | 26.3 (15.4) B | 1.4 (1.4) B |
The value for Filtek BulkFill at 20 s was excluded from the analysis of the total AE events since it was much higher than any of the other mean values.
Figure 2.
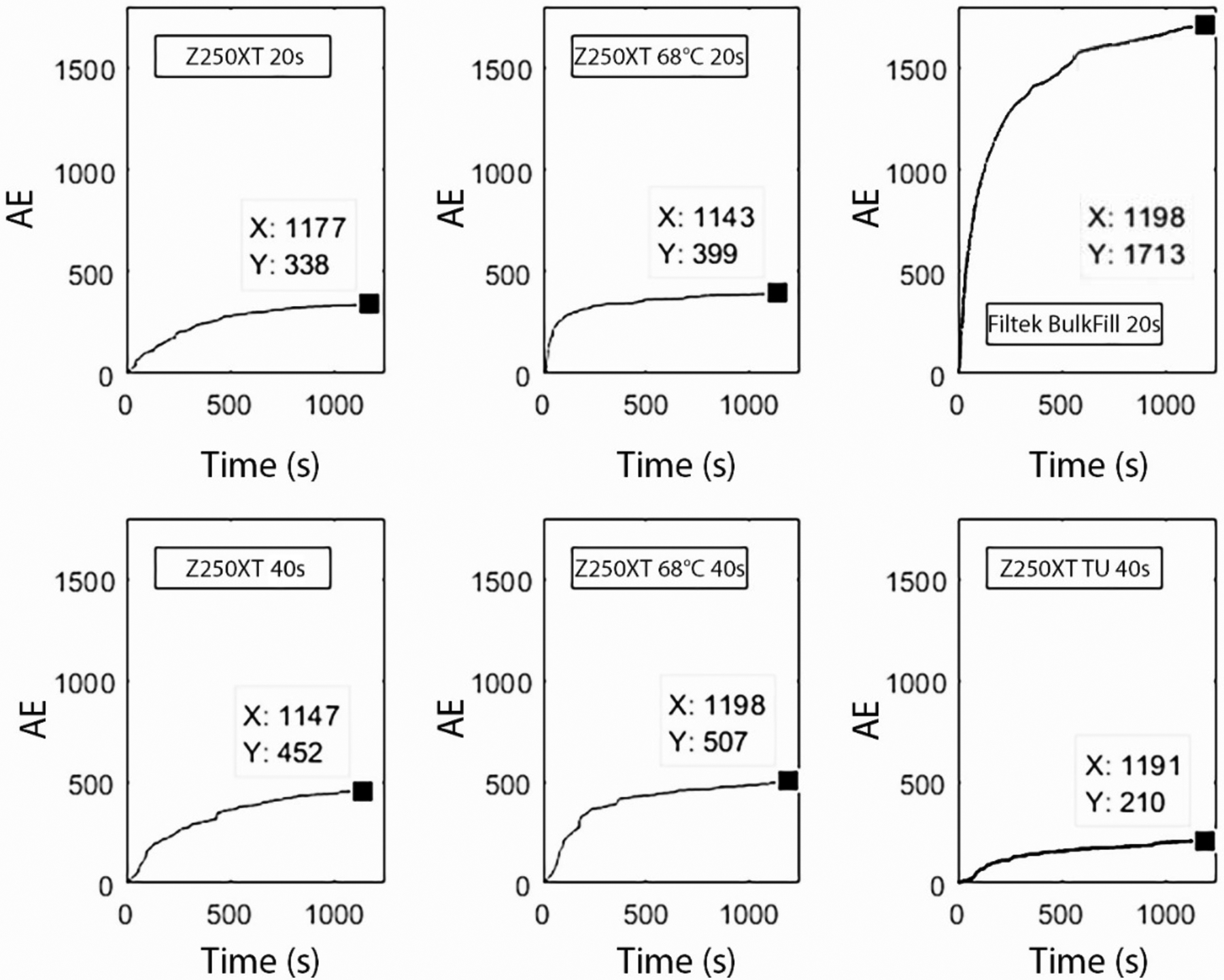
Cumulative number of total Acoustic Events (AE) for all specimens for each of the groups tested.
3.3. Degree of conversion
Table 4 shows the degree of conversion results. Filtek BulkFill and the thio-urethane experimental composite presented significantly higher conversion than other groups, at top and bottom (p<0.05). T-tests show that all groups presented lower degree of conversion at the bottom, except for Filtek BulkFill. Bottom to top ratios are all above 0.8.
Table 4.
Degree of conversion (%) measured by Raman spectroscopy and bottom to top ratio. Values followed by the same superscript on the same column are statistically similar (α=5%). T-tests compared the conversion at the top and bottom for each material – the asterisk denotes statistical difference (α=5%).
| Degree of conversion (%) | Bottom/top ratio | ||
|---|---|---|---|
| Top | Bottom | ||
| Z250XT 20s | 67.3 (2.7) B | 57.2 (2.5) B* | 0.85 |
| Z250XT 40s | 68.5 (1.0) B | 61.5 (2.3) B* | 0.89 |
| Z250XT 68° 20s | 67.2 (2.7) B | 62.2 (8.8) B* | 0.92 |
| Z250XT 68° 40s | 69.8 (2.6) B | 61.3 (6.3) B* | 0.88 |
| Filtek BulkFill 20s | 76.3 (2.9) A | 79.0 (2.4) A | 1.03 |
| Z250XT TU 40s | 78.0 (3.3) A | 73.6 (1.2) A* | 0.93 |
4. Discussion
Different bulk-fill techniques were tested with pre-heated resin composites and a thio-urethane-modified material in this in vitro study. Resin composite pre-heating did not affect the intra-pulpal temperature change. Also, pre-heating did not affect the polymerization stress and degree of conversion of the high C-factor bulk-filled restorations. Therefore, the first hypothesis was rejected. The thio-urethane modified resin composite presented significant stress reduction according to the acoustic emission test. Thus, the second hypothesis was also rejected.
In this study the intra-pulpal temperature change for pre-heated resin composites was not statistically different to that exhibited by room temperature materials when light-cured for the same time. Temperature change was only significantly higher when longer light-curing times were used. This result corroborates another study where 40 seconds of light exposure induced significantly higher intra-pulpal temperatures than 20 seconds [24]. According to Daronch et al. [25], the temperature of the resin composite is not expected to affect the intra-pulpal temperature before or after light-curing [26]. Several studies have shown that light exposure is responsible for considerable intra-pulpal temperature change and some of the factors associated with increased temperatures changes are light energy, time of exposure and light source [27–30]. Significant temperature changes with the addition of thio-urethanes to experimental composites was not expected. Although thio-urethanes are responsible for different reaction kinetics during polymerization, significant temperature changes should not be observed together with a light delay on composite vitrification.
Intra-pulpal temperature change with extended light-curing time (40 seconds) ranged between 2.4 and 3.2°C. Although temperature increase was statistically higher for this light-curing time, this temperature change may not be clinically unsafe. The best-known temperature threshold correlated with pulpal injury is 5.5°C, in which 15% of pulps evolved to necrosis. This threshold was reported in a study performed in monkeys [31], where the temperature changes were induced with a soldering iron at 275 °C, which does not translate the temperature changes occurring in dental procedures. Another study performed in humans with different methods has reported no symptomatic or histological pulp injury with temperature increases ranging from 8.9 to 14.7°C [32]. Thus, all temperature changes observed in this study were minor by comparison and could be considered safe to the pulpal tissue.
Acoustic emission has been used for estimating in vitro real time polymerization stress caused by resin composites in direct restorations. Previous studies showed that reducing the polymerization stress of composites resulted in less debonding, as evidenced by fewer AE events [33–35]. In general, this is a widely used non-destructive test capable of detecting structural defects such as crack formation and propagation, deformation, sliding, and fracture [36]. Few acoustic emission studies observing the effect of resin composite polymerization stress are present in the literature. Therefore, an AE may not be explained merely by resin composite debonding; other factors including stress relaxation inside the material could be responsible for generating an AE. A free shrinking resin composite placed over an acoustic emission sensor was already reported with no detectable AE, however this is the only report in the literature from only one specific material [34]. Also, the number of acoustic events alone may not be enough to explain the effects of polymerization stress on resin-tooth interfaces. For example, one AE with longer duration or higher amplitude may represent a more important structural defect than a number of AE with shorter durations and lower amplitudes. These parameters must be considered carefully, and consider the differences with sensor response/test setup, when analyzing acoustic emission results in further studies to avoid inaccurate interpretation of results for some materials.
In the present study, when overall AE were considered, the bulk-fill resin composite exhibited almost 4 times more AE than the conventional material. This result was not expected, as Filtek BulkFill has consistently shown lower polymerization stress than a conventional microhybrid resin in in vitro studies [37]. Furthermore, the same materials presented not statistically significant numbers of AE in an acoustic emission study [38]. One important fact that must be noticed regarding these results is the difference between the total number of AE captured by different studies. The same previous study reports mean AE ranging from 6.0 to 12.6 for different bulk-fill and conventional resin composites [38]. Other studies present even lower average AE [33, 39]. Acoustic emission is a very sensitive test that is even able to locate the AE source, so direct comparison of results from different test equipment and sample mounting configurations are difficult to achieve.
The resonant sensors used [33, 38, 39] have a high response in a limited frequency range, but a poor response for frequencies higher than 300kHz. In this study, a wide band WDI (relatively flat response between 100k-1MHz) sensor was used in order to avoid this limitation. To counterbalance the lower amplitude response, a less susceptible to noise sensor with a high level of amplification (60dB) was used. These sensors were then mounted directly on the tooth [34, 35]. In this configuration, the weak acoustic events were not subjected to possible interference from the edges of the glass slide and only went through one interface (tooth/sensor). This explains why the number of AE was high. When filtering only AE>60 dB the number of AE observed was similar to the results reported by other studies. The difference between these results and the literature might be explained by different test conditions, such as detection levels and test setup.
Results from AE>60 dB showed slightly fewer AE for BulkFill in comparison to Z250XT pre-heated or at room temperature, although not statistically different. This result could be expected and corroborates the results from a previous study, which used the microhybrid resin Z250 [38]. Light curing-time and pre-heating did not significantly affect total AE and AE>60 dB. On the other hand, the thio-urethane modified resin composite exhibited statistically lower results for both total AE and AE>60 dB. Experimental thio-urethane composites have been reported with considering low polymerization stress [21, 22, 40] and according to our results this technology seems to be a more effective low-stress additive compared to a commercial bulk-fill resin composite.
As for the effect of pre-heating the composite, cumulative AE graph shows that the stress evolved more rapidly for the pre-heated materials. Pre-heating of the resin composite has the potential to increase the final degree of conversion by favoring radical mobility and increasing the conversion before network formation (and diffusional limitations imposed by gelation/vitrification) is fully established [41], which would have at least in part explained the higher stress observed. However, pre-heating did not increase conversion in this study, which agrees with previous reports in the literature [42]. One explanation for the increased stress is the increased resin composite temperature at the time of light-curing, which would lead to greater thermal contraction upon cooling.
The light-curing device used in this study was a high-intensity LED. Light irradiance was monitored with a radiometer (~1,300 mW/cm2) and kept stable over the course of the experiments. Although conventional resin composite increments of 4 mm depth are not indicated, the conventional resin composite used presented adequate degree of conversion at the bottom of the restoration. Bottom/top degree of conversion ratios were high for all experimental groups and close to the recommended ratio (0.9) [43]. The bulk-fill and the thio-urethane experimental composite presented significantly higher conversion than the nanohybrid resin, irrespective its pre-heating or different light-curing time. Interestingly, the bulk-fill resin composite presented a bottom/top ratio greater than 1.0, though the conversion at the top and bottom were statistically similar. This apparently counter-intuitive result could potentially be explained by oxygen inhibition at the top surface, which decreases conversion. The top of the restorations was not polished before curing measurements were taken, and the depth of penetration of the RAMAN spectrometer used was 0.5–2 μm [44], well within the estimated thickness of the oxygen inhibited layer [45]. It is also likely that this ratio is an artifact of the conversion measurements – little to no attenuation of light was likely achieved, as is the intention with the formulation of bulk-fill materials, which is corroborated by the fact that the conversion at the bottom was only slightly lower than at the top, which caused the ratio to be within the standard error of the experiment. In any case, this result shows that a high-intensity curing-light may be able to cure deep resin increments. However, light attenuation is an important issue that must be considered and resin composites with different shades or opacities can present lower light transmission [46].
Experimental resin composites with the addition of thio-urethanes have been reported with higher degree of conversion, lower polymerization stress and improved mechanical properties [21, 22, 40]. Filler functionalization is a new approach for adding thio-urethanes to dental resin composites. This alternative requires less thio-urethane addition to the composite with similar properties improvement [23]. Therefore, in this study functionalized filler was added to a commercial resin composite to test it against a commercial low stress resin composite. Our results suggest that this new technology may provide more effective stress reduction, with the same or better conversion in depth in commercial materials. The experimental resin composite modified with the thio-urethane presented significant higher degree of conversion compared to the unmodified material irrespective of light-curing time or pre-heating. Also, the lowest number of AE (total and >60 dB) was observed with the thio-urethane composite. The benefits of incorporating thio-urethanes to dental composites seem to be a promising advance, especially for bulk-fill resin composites.
5. Conclusion
Pre-heating of a conventional resin composite was not be able to reduce its polymerization stress or improve degree of conversion. The addition of thio-urethane was able to improve the degree of conversion and decrease polymerization stress. However, the thio-urethane modified resin did not reduce the polymerization stress nor improved the degree of conversion when compared to a bulk-fill resin composite.
Highlights.
Pre-heating does not reduce polymerization stress of resin composite restorations
Thio-urethane addition increases resin composite degree of conversion
Thio-urethane addition reduces resin composite polymerization stress
Acknowledgements
The authors acknowledge funding from NIH-NIDCR (R15-DE023211, U01-DE023756 to CSP).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
References
- [1].Soares CJ, Faria ES, Rodrigues MP, Vilela ABF, Pfeifer CS, Tantbirojn D, et al. Polymerization shrinkage stress of composite resins and resin cements - What do we need to know? Braz Oral Res 2017; 31:e62 DOI: 10.1590/1807-3107BOR-2017.vol31.0062 [DOI] [PubMed] [Google Scholar]
- [2].Davidson CL, de Gee AJ. Relaxation of polymerization contraction stresses by flow in dental composites. J Dent Res 1984; 63:146–8. DOI: 10.1177/00220345840630021001 [DOI] [PubMed] [Google Scholar]
- [3].Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the SDR technology. Dent Mater 2011; 27:348–55. DOI: 10.1016/j.dental.2010.11.014 [DOI] [PubMed] [Google Scholar]
- [4].Weinmann W, Thalacker C, Guggenberger R. Siloranes in dental composites. Dent Mater 2005; 21:68–74. DOI: 10.1016/j.dental.2004.10.007 [DOI] [PubMed] [Google Scholar]
- [5].Ferracane JL. Buonocore Lecture. Placing dental composites - a stressful experience. Oper Dent 2008; 33:247–57. DOI: 10.2341/07-BL2 [DOI] [PubMed] [Google Scholar]
- [6].Ferracane JL, Mitchem JC. Relationship between composite contraction stress and leakage in Class V cavities. Am J Dent 2003; 16:239–43. [PubMed] [Google Scholar]
- [7].Irie M, Suzuki K, Watts DC. Marginal gap formation of light-activated restorative materials: effects of immediate setting shrinkage and bond strength. Dent Mater 2002; 18:203–10. [DOI] [PubMed] [Google Scholar]
- [8].Prager M, Pierce M, Atria PJ, Sampaio C, Caceres E, Wolff M, et al. Assessment of cuspal deflection and volumetric shrinkage of different bulk fill composites using non-contact phase microscopy and micro-computed tomography. Dent Mater J 2018; 37:393–9. DOI: 10.4012/dmj.2017-136 [DOI] [PubMed] [Google Scholar]
- [9].Singhal S, Gurtu A, Singhal A, Bansal R, Mohan S. Effect of different composite restorations on the cuspal deflection of premolars restored with different insertion techniques - an in vitro study. J Clin Diag Res 2017; 11:ZC67–70. DOI: 10.7860/JCDR/2017/20159.10440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Daronch M, Rueggeberg FA, De Goes MF. Monomer conversion of pre-heated composite. J Dent Res 2005; 84: 663–7. DOI: 10.1177/154405910508400716 [DOI] [PubMed] [Google Scholar]
- [11].Lee JH, Um CM, Lee IB. Rheological properties of resin composites according to variations in monomer and filler composition. Dent Mater 2006; 22:515–26. DOI: 10.1016/j.dental.2005.05.008 [DOI] [PubMed] [Google Scholar]
- [12].Trujillo M, Newman SM, Stansbury JW. Use of near-IR to monitor the influence of external heating on dental composite photopolymerization. Dent Mater 2004; 20:766–77. DOI: 10.1016/j.dental.2004.02.003 [DOI] [PubMed] [Google Scholar]
- [13].Zorzin J, Maier E, Harre S, Fey T, Belli R, Lohbauer U, Petschelt A, Taschner M. Bulk-fill resin composites: polymerization properties and extended light curing. Dent Mater 2015;31:293–301. DOI: 10.1016/j.dental.2014.12.010 [DOI] [PubMed] [Google Scholar]
- [14].Braga RR, Ferracane JL. Contraction stress related to degree of conversion and reaction kinetics. J Dent Res 2002;81: 114–8. [PubMed] [Google Scholar]
- [15].Calheiros FC, Daronch M, Rueggeberg FA, Braga RR. Effect of temperature on composite polymerization stress and degree of conversion. Dent Mater 2014; 30:613–8. DOI: 10.1016/j.dental.2014.02.024 [DOI] [PubMed] [Google Scholar]
- [16].Lu H, Stansbury JW, Bowman CN. Impact of curing protocol on conversion and shrinkage stress. J Dent Res 2005; 84: 822–6. DOI: 10.1177/154405910508400908 [DOI] [PubMed] [Google Scholar]
- [17].Nada K, El-Mowafy O. Effect of precuring warming on mechanical properties of restorative composites. Int J Dent 2011; 2011:536212 DOI: 10.1155/2011/536212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bacchi A, Dobson A, Ferracane JL, Consani R, Pfeifer CS. Thio-urethanes improve properties of dual-cured composite cements. J Dent Res 2014; 93:1320–5. DOI: 10.1177/0022034514551768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Pfeifer CS, Wilson ND, Shelton ZR, Stansbury JW. Delayed gelation through chain-transfer reactions: mechanism for stress reduction in methacrylate networks. Polymer 2011; 52:3295–303. DOI: 10.1016/j.polymer.2011.05.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bacchi A, Consani RL, Martim GC, Pfeifer CS. Thio-urethane oligomers improve the properties of light-cured resin cements. Dent Mater 2015; 31:565–74. DOI: 10.1016/j.dental.2015.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Bacchi A, Nelson M, Pfeifer CS. Characterization of methacrylate-based composites containing thio-urethane oligomers. Dent Mater 2016; 32:233–9. DOI: 10.1016/j.dental.2015.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bacchi A, Pfeifer CS. Rheological and mechanical properties and interfacial stress development of composite cements modified with thio-urethane oligomers. Dent Mater 2016; 32:978–86. DOI: 10.1016/j.dental.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Faria-E-Silva AL, Dos Santos A, Girotto EM, Pfeifer CS. Impact of thiourethane filler surface functionalization on composite properties. J Appl Polym Sci 2019; 5;136(25). PII: 47687. [PMC free article] [PubMed] [Google Scholar]
- [24].Rajesh Ebenezar AV, Anilkumar R, Indira R, Ramachandran S, Srinivasan MR. Comparison of temperature rise in the pulp chamber with different light curing units: An in-vitro study. J Cons Dent 2010; 13:132–5. DOI: 10.4103/0972-0707.71644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Daronch M, Rueggeberg FA, Moss L, de Goes MF. Clinically relevant issues related to preheating composites. J Esthet Res Dent 2006; 18:340–50; discussion 51. DOI: 10.1111/j.1708-8240.2006.00046.x [DOI] [PubMed] [Google Scholar]
- [26].Daronch M, Rueggeberg FA, Hall G, De Goes MF. Effect of composite temperature on in vitro intrapulpal temperature rise. Dent Mater 2007; 23:1283–8. DOI: 10.1016/j.dental.2006.11.024 [DOI] [PubMed] [Google Scholar]
- [27].Armellin E, Bovesecchi G, Coppa P, Pasquantonio G, Cerroni L. LED Curing lights and temperature changes in different tooth sites. BioMed Res Int 2016; 2016:1894672 DOI: 10.1155/2016/1894672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hannig M, Bott B. In-vitro pulp chamber temperature rise during composite resin polymerization with various light-curing sources. Dent Mater 1999; 15:275–81. [DOI] [PubMed] [Google Scholar]
- [29].Leprince J, Devaux J, Mullier T, Vreven J, Leloup G. Pulpal-temperature rise and polymerization efficiency of LED curing lights. Oper Dent 2010; 35:220–30. DOI: 10.2341/09-203-L [DOI] [PubMed] [Google Scholar]
- [30].Yazici AR, Muftu A, Kugel G, Perry RD. Comparison of temperature changes in the pulp chamber induced by various light curing units, in vitro. Oper Dent 2006; 31:261–5. DOI: 10.2341/05-26 [DOI] [PubMed] [Google Scholar]
- [31].Zach L, Cohen G. Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 1965; 19:515–30. [DOI] [PubMed] [Google Scholar]
- [32].Baldissara P, Catapano S, Scotti R. Clinical and histological evaluation of thermal injury thresholds in human teeth: a preliminary study. J Oral Rehab 1997; 24:791–801. [DOI] [PubMed] [Google Scholar]
- [33].Cho NY, Ferracane JL, Lee IB. Acoustic emission analysis of tooth-composite interfacial debonding. J Dent Res 2013; 92:76–81. DOI: 10.1177/0022034512465757 [DOI] [PubMed] [Google Scholar]
- [34].Li H, Li J, Yun X, Liu X, Fok AS. Non-destructive examination of interfacial debonding using acoustic emission. Dent Mater 2011; 27:964–71. DOI: 10.1016/j.dental.2011.06.002 [DOI] [PubMed] [Google Scholar]
- [35].Liu X, Li H, Li J, Lu P, Fok AS. An acoustic emission study on interfacial debonding in composite restorations. Dent Mater 2011; 27:934–41. DOI: 10.1016/j.dental.2011.05.008 [DOI] [PubMed] [Google Scholar]
- [36].Ohtsu M, Enoki M, Mizutani Y, Shigeishi M. Principles of the acoustic emission (AE) method and signal processing In: Society for Non-Destructive Inspection TJ, editor. Practical Acoustic Emission Testing. Tokyo: Springer Japan; 2016. p. 5–34. [Google Scholar]
- [37].Guo Y, Landis FA, Wang Z, Bai D, Jiang L, Chiang MY. Polymerization stress evolution of a bulk-fill flowable composite under different compliances. Dent Mater 2016; 32:578–86. DOI: 10.1016/j.dental.2016.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kim RJ, Kim YJ, Choi NS, Lee IB. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent 2015; 43:430–9. DOI: 10.1016/j.jdent.2015.02.002 [DOI] [PubMed] [Google Scholar]
- [39].Kim RJ, Choi NS, Ferracane J, Lee IB. Acoustic emission analysis of the effect of simulated pulpal pressure and cavity type on the tooth-composite interfacial de-bonding. Dent Mater 2014; 30:876–83. DOI: 10.1016/j.dental.2014.05.027 [DOI] [PubMed] [Google Scholar]
- [40].Bacchi A, Yih JA, Platta J, Knight J, Pfeifer CS. Shrinkage/stress reduction and mechanical properties improvement in restorative composites formulated with thio-urethane oligomers. J Mech Behav Biomed Mater 2018; 78:235–40. DOI: 10.1016/j.jmbbm.2017.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Daronch M, Rueggeberg FA, De Goes MF, Giudici R. Polymerization kinetics of pre-heated composite. J Dent Res 2006; 85:38–43. DOI: 10.1177/154405910608500106 [DOI] [PubMed] [Google Scholar]
- [42].Froes-Salgado NR, Silva LM, Kawano Y, Francci C, Reis A, Loguercio AD. Composite pre-heating: effects on marginal adaptation, degree of conversion and mechanical properties. Dent Mater 2010; 26:908–14. DOI: 10.1016/j.dental.2010.03.023 [DOI] [PubMed] [Google Scholar]
- [43].Bouschlicher MR, Rueggeberg FA, Wilson BM. Correlation of bottom-to-top surface microhardness and conversion ratios for a variety of resin composite compositions. Oper Dent 2004; 29:698–704. [PubMed] [Google Scholar]
- [44].Tran W, Tisinger LG, Lavalle LE, Sommer AJ. Analysis of thin-film polymers using attenuated total internal reflection-Raman microspectroscopy. Appl Spec 2015; 69:230–8. DOI: 10.1366/13-07024 [DOI] [PubMed] [Google Scholar]
- [45].Kim JS, Choi YH, Cho BH, Son HH, Lee IB, Um CM, et al. Effect of light-cure time of adhesive resin on the thickness of the oxygen-inhibited layer and the microtensile bond strength to dentin. J Biomed Mater Res - Part B Appl Biomater 2006; 78:115–23. DOI: 10.1002/jbm.b.30463 [DOI] [PubMed] [Google Scholar]
- [46].Arikawa H, Fujii K, Kanie T, Inoue K. Light transmittance characteristics of light-cured composite resins. Dent Mater 1998; 14:405–11. [DOI] [PubMed] [Google Scholar]


