To the Editor
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS CoV-2), was declared a global public health emergency on 30 January 2020. Emerging data suggests that COVID-19 has extrapulmonary manifestations and complications, subsequently leading to multiorgan failure and death. Common cardiovascular and renal complications reported to be associated with COVID-19 include myocardial injury, heart failure, acute kidney injury and electrolyte disturbances.1 , 2 In addition to the observation that older patients, males and those with pre-existing comorbidities such as cardiovascular disease, diabetes, chronic kidney disease and chronic liver disease are at highest risk for severe illness or death,3 , 4 COVID-19 complications have been shown to correlate with the disease severity or mortality.5 , 6 Emerging data also suggests COVID-19 contributes to adverse hepatic manifestations such as acute hepatic injury. Wang and colleagues in their recent published study to investigate characteristics and prognostic factors in 339 elderly patients with COVID-19, a high proportion of severe and critical cases were observed as well as a high fatality rate.7 Apart from cardiovascular complications such as acute cardiac injury, arrhythmia and cardiac insufficiency, 28.7% of patients were reported to have developed liver enzyme abnormalities. Coronavirus disease 2019 is still evolving; its exact clinical course, severity and complications are still not completely clear. Given the sparse data, the hepatic manifestations and complications of COVID-19 are not clearly defined. In this context, we sought to address the following questions using a systematic meta-analysis: (i) what are the hepatic manifestations and complications of COVID-19?; (ii) what is the prevalence of hepatic manifestations and incidence of hepatic complications?; and (iii) are patients with pre-existing hepatic conditions more susceptible to these complications?
The protocol for this review was registered in the PROSPERO International prospective register of systematic reviews (CRD42020190354) and the review was conducted in accordance with PRISMA and MOOSE guidelines (Supplementary Materials 1–2). Published studies reporting on hepatic complications following admission in patients hospitalised with COVID-19 and/or hepatic manifestations during admission were sought in MEDLINE, Embase, and The Cochrane library from 2019 to 15 June 2020. Details of the search strategy are reported in Supplementary Material 3. The prevalence of comorbidities (eg, pre-existing chronic liver disease), prevalence of hepatic manifestations and incidence of hepatic complications across studies with their 95% confidence intervals (CIs) were pooled using Freeman-Tukey variance stabilising double arcsine transformation and random-effects models. All statistical analyses employed STATA release MP 16 (StataCorp LP, College Station, TX, USA)
Nineteen retrospective cohort studies comprising of 15,103 patients with COVID-19 were included (Table 1 ; Supplementary Materials 4–5). Fourteen studies were based in China and five in the USA. The average age at baseline ranged from 32 to 71 years.
Table 1.
Characteristics of included studies.
| Author, year | Source of data | Country | Dates of data | Mean/median | Male% | Hospitalisation | No. of | Hepatic | NOS |
|---|---|---|---|---|---|---|---|---|---|
| of publication | collection | age (years) | (days) | patients | complications | ||||
| Aggarwal, 2020 | UnityPoint Clinic | USA | March - April 2020 | 67.0 | 75.0 | 2.0 | 16 | Acute hepatic injury | 4 |
| Arentz, 2020 | Evergreen Hospital in Kirkland, Washington | USA | Feb - March 2020 | 70.0 | 52.0 | 5.2 | 21 | Acute hepatic injury | 4 |
| Chen, 2020 | Tongji Hospital in Wuhan | China | Jan - Feb 2020 | 62.0 | 62.0 | 13.0 | 274 | Acute hepatic injury | 4 |
| Cao, 2020 | Zhongnan Hospital of Wuhan University | China | Jan - Feb 2020 | 54.0 | 52.0 | 11.0 | 102 | Acute hepatic injury; liver enzyme abnormalities | 4 |
| Du, 2020 | Hannan Hospital and Wuhan Union Hospital | China | Jan - Feb 2020 | 65.8 | 72.9 | 10.1 | 85 | Acute hepatic injury | 4 |
| Guo, 2020 | Seventh Hospital of Wuhan City | China | Jan - Feb 2020 | 58.5 | 48.7 | 16.3 | 187 | Acute hepatic injury | 5 |
| Jin, 2020 | Zhejiang province | China | Jan – Feb 2020 | 45.2 | 50.8 | NR | 651 | Acute hepatic injury | 6 |
| Liu, 2020 | Shenzhen Third People's hospital | China | Dec 2019 - Jan 2020 | 61.0 | 66.7 | 8.6 | 12 | Hepatic insufficiency | 4 |
| Phipps, 2020 | New York-Presbyterian network | USA | March – April 2020 | 65.0 | 57.0 | 6.0 | 2273 | Liver enzyme abnormalities | 6 |
| Price-Haywood, 2020 (W) | Ochsner Health in Louisiana | USA | March – April 2020 | 55.5 | 45.7 | 7.0 | 1030 | Acute hepatic injury | 6 |
| Price-Haywood, 2020 (B) | Ochsner Health in Louisiana | USA | March – April 2020 | 53.6 | 37.7 | 6.0 | 2451 | Acute hepatic injury | 6 |
| Richardson, 2020 | Hospitals in New York | USA | March - April 2020 | 63.0 | 60.3 | 4.5 | 5700 | Acute hepatic injury | 4 |
| Shi,2020 | Renmin Hospital of Wuhan University | China | Jan - Feb 2020 | 64.0 | 49.3 | NR | 416 | Hypoproteinaemia | 6 |
| Wang, 2020 | Renmin Hospital of Wuhan University | China | Jan - Feb 2020 | 71.0 | 49.0 | 28.0 | 339 | Liver enzyme abnormalities | 4 |
| Xi, 2020 | Fourth People's Hospital of Qinghai Province; Third People's Hospital of Xining | China | Jan – April 2020 | 32.0 | 67.0 | 13.5 | 18 | Acute hepatic injury | 4 |
| Yang, 2020 | Wuhan Jin Yin-tan hospital | China | Dec 2019 - Jan 2020 | 59.7 | 67.0 | 10.0 | 52 | Liver dysfunction | 4 |
| Zhang, 2020 | Huanggang Central Hospital; The Second Affiliated Hospital of Shandong First Medical University | China | Jan – Feb 2020 | 48.3 | 55.7 | 10.2 | 194 | Low albumin; elevated aminotransferases | 4 |
| Zhao, 2020 | Jingzhou Central Hospital | China | Jan – Feb 2020 | 46.0 | 53.8 | NR | 91 | Acute hepatic injury | 4 |
| Zhao, 2020b | Shouyi and East districts of Renmin Hospital of Wuhan University | China | Jan – Feb 2020 | 61.0 | 46.6 | 7.0 | 1000 | Acute hepatic injury | 4 |
| Zhou, 2020 | Jinyintan Hospital & Wuhan Pulmonary Hospital | China | Dec - Jan 2020 | 56.0 | 62.0 | 11.0 | 191 | Hypoproteinaemia | 5 |
B, blacks; NOS, Newcastle Ottawa Scale; NR, not reported; W, whites.
In pooled analysis of 10 studies, the prevalence of pre-existing chronic liver disease (95% CI) in COVID-19 patients was 1.9% (0.5–3.8) (Supplementary Material 6). The prevalence (95% CI) of pre-existing liver cirrhosis (3 studies), hepatitis B (3 studies) and hepatitis C (2 studies) was 0.4% (0.0–1.8), 0.9% (0.1–2.5) and 0.3% (0.2–0.5) respectively (Supplementary Material 7). The prevalence (95% CI) of hepatic manifestations on admission: elevated alanine aminotransferase (ALT) (9 studies), elevated aspartate aminotransferase (AST) (8 studies), low albumin (2 studies) and elevated total bilirubin (3 studies) was 26.6% (15.8–39.0), 37.2% (20.3–55.8), 45.6 (40.5–50.8) and 18.2% (10.0–28.1) respectively (Supplementary Material 8).
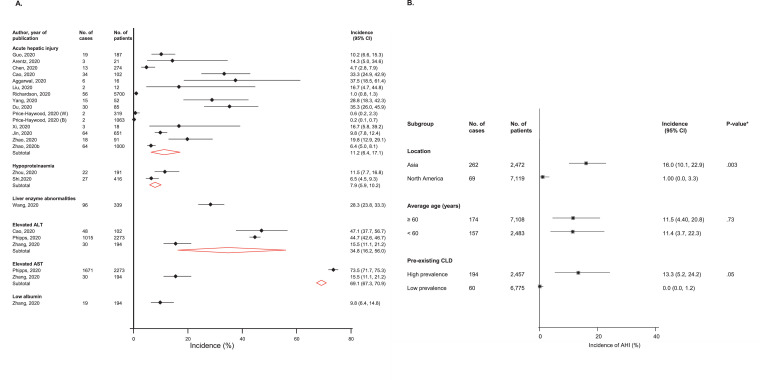
Over hospital stays ranging from 2 to 28 days, the pooled incidence was 69.1% (67.3–70.9) for elevated ALT (2 studies); 34.8% (16.2–56.0) for elevated AST; 11.2% (6.4–17.1) for acute hepatic injury (15 studies) and 7.9% (5.9–10.2) for hypoproteinaemia (n = 2 studies) (Fig. 1 A). Subgroup analyses suggested that the incidence of acute hepatic injury was higher in Chinese populations and groups with a higher prevalence of pre-existing chronic liver disease; however, the incidence of acute hepatic injury was similar in older (≥ 60 years) or younger age (< 60 years) groups (Fig. 1B).
Fig. 1.
(A) Incidence of hepatic complications in COVID-19 patients; (B) Incidence of acute hepatic injury in COVID-19 patients, by clinically relevant characteristics
AHI, acute hepatic injury; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CI, confidence interval (bars); CLD, chronic liver disease; *, p-value for meta-regression.
Based on up-to-date published evidence, the common hepatic complications of COVID-19 are liver enzyme abnormalities (particularly the aminotransferases) followed by acute hepatic injury and hypoproteinaemia. Common hepatic manifestations on admission are elevated levels of ALT, AST and total bilirubin as well as low albumin levels. In contrast to a previous study which reported that about 2–11% of patients with COVID-19 have liver comorbidities,8 the current review suggests that the prevalence estimate of pre-existing chronic liver disease may be lower at 1.9%. Though there is controversy regarding the causes of liver injury in COVID-19,8 the following mechanistic pathways have been proposed: (i) drug-induced during treatment; (i) direct injury to the liver due to COVID-19 hepatitis; (ii) COVID-19 induced myositis causing elevations in circulating levels of liver enzymes; (iii) binding of SARS CoV-2 directly to angiotensin-converting enzyme 2 (ACE2) positive rich cholangiocytes and causing liver damage; (iv) hepatic congestion due to high levels of positive end expiratory pressure during mechanical ventilation; and (v) aggravation of liver injury by SARS CoV-2 in patients with pre-existing viral hepatitis.4 The current findings suggest that patient groups with higher prevalence of pre-existing chronic liver disease have higher incidence of acute hepatic injury.
Patients with pre-existing liver dysfunction appear to have worse outcomes in COVID-19,8 which has been attributed to their immunocompromised status.8 Hepatic complications such as acute hepatic injury have also been shown to be associated with increased risk of severe COVID-19 and fatal outcomes.9 Liver injury is commonly characterised by markedly elevated levels of the aminotransferases and evidence suggests that elevated levels of these enzymes are associated with greater risk of severe disease and mortality.4 Hepatic dysfunction is associated with systemic disturbances such as activation of the coagulation and fibrinolytic cascades, depressed platelet counts, increased neutrophil counts, decreased lymphocyte counts and increased ferritin levels,10 which disrupt innate immune regulation. More intensive surveillance of markers of hepatic dysfunction is needed for patients who are admitted, to enable early and individually tailored therapeutic approaches.
Inherent limitations of this review included: (i) low methodological quality and sample sizes of included studies, which was not unexpected given the urgency to report and gain a better understanding of COVID-19; (ii) potential for selective reporting by some of the studies; (iii) definitions of acute hepatic injury were not reported by studies, hence it is unknown if this was consistent across studies; (iv) timing for assessment of hepatic markers may vary between studies, hence estimates may be biased; and (v) the potential possibility of patient overlap given that the majority of studies were conducted from China.4
Synthesis of the current literature suggests that liver enzyme abnormalities, acute hepatic injury and hypoproteinaemia are frequent hepatic complications among patients hospitalised with COVID-19. Intensive monitoring of markers of these complications and management during admission could help in the prediction of favourable outcomes. The causes of these hepatic complications need further elucidation.
Declaration of Competing Interest
None.
Acknowledgements
SKK acknowledges support from the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care. These sources had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2020.06.043.
Appendix. Supplementary materials
References
- 1.Kunutsor S.K., Laukkanen J.A. Renal complications in COVID-19: a systematic review and meta-analysis. Ann Med. 2020 doi: 10.1080/07853890.2020.1790643. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kunutsor S.K., Laukkanen J.A. Cardiovascular complications in COVID-19: a systematic review and meta-analysis. J Infect. 2020 doi: 10.1016/j.jinf.2020.05.068. PubMed PMID: 32504747. Epub 2020/06/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss P., Murdoch D.R. Clinical course and mortality risk of severe COVID-19. Lancet. 2020;395(10229):1014–1015. doi: 10.1016/S0140-6736(20)30633-4. PubMed PMID: 32197108. Pubmed Central PMCID: PMC7138151. Epub 2020/03/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kunutsor S.K., Laukkanen J.A. Markers of liver injury and clinical outcomes in COVID-19 patients: a systematic review and meta-analysis. J Infect. 2020 doi: 10.1016/j.jinf.2020.05.045. PubMed PMID: 32474033. Pubmed Central PMCID: PMC7255758. Epub 2020/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1017. PubMed PMID: 32219356. Pubmed Central PMCID: PMC7101506. Epub 2020/03/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X., Fang X., Cai Z., Wu X., Gao X., Min J. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Res. Wash D C. 2020;2020 doi: 10.34133/2020/2402961. PubMed PMID: 32377638. Pubmed Central PMCID: PMC7187729. Epub 2020/05/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L., He W., Yu X., Hu D., Bao M., Liu H. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.019. PubMed PMID: 32240670. Pubmed Central PMCID: PMC7118526. Epub 2020/04/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang C., Shi L., Wang F.S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–430. doi: 10.1016/S2468-1253(20)30057-1. PubMed PMID: 32145190. Pubmed Central PMCID: PMC7129165. Epub 2020/03/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lei F., Liu Y.M., Zhou F., Qin J.J., Zhang P., Zhu L. Longitudinal association between markers of liver injury and mortality in COVID-19 in China. Hepatology. 2020 doi: 10.1002/hep.31301. PubMed PMID: 32359177. Epub 2020/05/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. PubMed PMID: 32031570. Pubmed Central PMCID: PMC7042881. Epub 2020/02/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.