Abstract
Child maltreatment is a robust risk factor for suicidal ideation and behaviors during adolescence. Elevations in internalizing and externalizing symptomology have been identified as two distinct developmental pathways linking child maltreatment and adolescent risk for suicide. However, recent research suggests that the co-occurrence of internalizing and externalizing symptomology may form a distinct etiological pathway for adolescent risk behaviors. Using the Longitudinal Studies on Child Abuse and Neglect (LONGSCAN) sample (N = 1,314), the present study employed a person-centered approach to identify patterns of concurrent change in internalizing and externalizing psychopathology over five time points from early childhood to adolescence in relation to previous experiences of child maltreatment and subsequent suicidal ideation and behaviors. Results indicated four distinct bivariate externalizing and internalizing growth trajectories. Group membership in a heightened comorbid internalizing and externalizing symptom trajectory mediated the association between childhood abuse and adolescent suicidal ideation and suicidal behaviors. These findings suggest that the concurrent development of externalizing and internalizing symptoms in childhood and adolescence may constitute a unique developmental trajectory that confers risk for suicide-related outcomes.
Keywords: adolescence, child maltreatment, comorbidity, growth-mixture modeling, suicidal ideation and behavior
Introduction
Epidemiological data indicate that suicide rates among adolescents in the United States are steadily increasing (Curtin, Warner, & Hedegaard, 2016). Suicide is now the second leading cause of death among adolescents, and approximately seven percent of youth attempt suicide each year (Kann et al., 2016). Accumulating evidence underscores the central role of child maltreatment as a potent risk factor for youths’ suicidal ideation (Gomez et al., 2017; Miller, Esposito-Smythers, Weismoore, & Renshaw, 2013) and suicide attempts (Hadland et al., 2015; Johnson et al., 2002; Miller, Esposito-Smythers, Weismoore, & Renshaw, 2013). Child maltreatment is a severe form of childhood adversity, which has been shown to increase the risk for suicide attempts by as much as five- to sevenfold (Johnson et al., 2002). Further, studies show that at least one in four maltreated youth report a history of suicidal ideation, planning, or attempts (Collishaw et al., 2007; Coohey, Dirks-Bihun, Renner, & Baller, 2014; Taussig, Harpin, & Maguire, 2014). More than three million children are investigated for alleged maltreatment each year in the United States (US Department of Health & Human Services Administration for Children and Families Administration on Children Youth and Families Children’s Bureau, 2018), placing these youth at an increased risk for suicide-related outcomes (Collishaw et al., 2007).
Despite the robust documentation on the link between child maltreatment and suicidal ideation and behaviors, there is relatively scant knowledge on the developmental mechanisms underlying this association. Several studies have identified internalizing and externalizing psychopathology as two separate mechanisms in the association between child maltreatment and suicidal ideation and behaviors in adolescence (e.g., Miller, Adams, Esposito-Smythers, Thompson, & Proctor, 2014; Rytilä-Manninen, Haravuori, Fröjd, Marttunen, & Lindberg, 2018; Wanner, Vitaro, Tremblay, & Turecki, 2012). However, emerging research suggests that some youth exhibit both internalizing and externalizing symptoms and that these concurrent symptom elevations are stable over time (Willner, Gatzke-Kopp, & Bray, 2016). Despite the documented presence of comorbidity in internalizing and externalizing symptomology, it remains to be determined whether such comorbidity is linked to increased risk for suicidal ideation and behaviors in adolescence. Thus, the current study seeks to test the role of comorbid change in internalizing and externalizing psychopathology in the developmental pathway between childhood adversity and adolescent suicidal ideation, planning, and attempts.
Child Maltreatment and Externalizing and Internalizing Symptomology
Prior empirical work and theoretical models implicate child maltreatment as a significant risk factor for the development of internalizing and externalizing psychopathology (e.g., Li & Godinet, 2014; Oshri, Rogosch, Burnette, & Cicchetti, 2011; Wilson, Samuelson, Staudenmeyer, & Widom, 2015). The absence of stable, safe, and nurturing care during childhood ushers in vulnerabilities in child development that increase the likelihood for compromised socioemotional outcomes in adolescence, including heightened internalizing and externalizing symptom trajectories (Cicchetti & Rogosch, 2002). Within the organizational framework of child development, the context of child maltreatment is considered a pathogenic environment that challenges children’s ability to attain stage-salient developmental tasks (Cicchetti & Banny, 2014). The disruption of socioemotional stage-salient tasks, such as the development of emotion regulation (Cummings, Schermerhorn, Davies, Goeke-Morey, & Cummings, 2006), may cascade into future psychopathology that includes internalizing and externalizing behaviors.
Copious evidence underscores the effect of child maltreatment on youths’ internalizing and externalizing symptoms and disorders (Bolger & Patterson, 2001; English et al., 2005; Li & Godinet, 2014; Oshri et al., 2011). There are some limitations in this literature, however, including the need for more research on the influence of maltreatment type in relation to internalizing and externalizing problems. The maltreatment literature classifies maltreatment into four primary types, including physical abuse, sexual abuse, neglect, and emotional abuse (English & LONGSCAN Investigators, 1997). Although these types significantly covary with one another, there is evidence that each of these types may be differentially associated with psychopathology across the lifespan (Moran, Vuchinich, & Hall, 2004; Oshri, Sutton, Clay-Warner, & Miller, 2015). For example, in a study that utilized caseworker records of maltreatment, preadolescents who experienced physical abuse were at an increased risk for externalizing, while those who experienced physical neglect were at an increased risk for internalizing problems (Petrenko, Friend, Garrido, Taussig, & Culhane, 2012). Much of the empirical work in this area has utilized a single measure of maltreatment, however, so more research is needed to uncover the unique influence of maltreatment types on the development of youth internalizing and externalizing symptoms.
There are also limitations in the literature on child maltreatment and adolescent externalizing and internalizing problems, which relate to research design and modeling strategies. Although a growing body of research has utilized longitudinal designs to investigate child maltreatment and adolescent psychopathology, much of this work has examined psychopathology at a single point in adolescence (e.g., Mills et al., 2013; Moylan et al., 2010). However, youth psychopathology is often not stable and instead fluctuates over time. Researchers have accounted for this by utilizing longitudinal designs and techniques such as cross-lagged panel modeling and growth curve models to examine how maltreatment predicts changes in internalizing and externalizing symptoms across childhood and adolescence (Kim-Spoon, Cicchetti, & Rogosch, 2013; Rogosch, Oshri, & Cicchetti, 2010; Thompson, English, & White, 2016). Notably, recent studies have utilized pattern-based analytical strategies (also referred to as person-centered approaches) to investigate the influence of early adversity on patterns of change in internalizing and externalizing symptoms during adolescence (Lauterbach & Armour, 2015; Proctor, Skriner, Roesch, & Litrownik, 2010). However, these studies have been limited by modeling the effect of maltreatment on changes in internalizing and externalizing problems separately. Thus, research is missing on the influence of maltreatment, including specific types of maltreatment, on concurrent trajectories of internalizing and externalizing symptoms across childhood and adolescence.
Internalizing and Externalizing Symptoms and Suicide Risk: The Comorbidity Hypothesis
There is strong evidence that supports internalizing and externalizing symptomologies as two distinct developmental pathways to suicide risk in adolescence and young adulthood (Brezo et al., 2008; Kerr, Reinke, & Eddy, 2013). Indeed, internalizing psychopathology (e.g., depressive and anxious symptoms) and externalizing psychopathology (e.g., aggression and disruptiveness) have each been documented as separate predictors of suicide attempts (e.g., Verona, Sachs-Ericsson, & Joiner, 2004; Wanner, Vitaro, Tremblay, & Turecki, 2012). For example, in a recent longitudinal study, trajectories of anxiousness (i.e., internalizing behaviors) and disruptiveness (i.e., externalizing behaviors) served as mediators in the link between self-reported childhood adversity and suicide attempts (Wanner et al., 2012). However, despite the extant literature on internalizing and externalizing symptom pathways to suicidal ideation and behaviors (Kerr et al., 2013; Verona et al., 2004), less attention has been given to the common co-occurrence of these symptoms and the risk for suicide.
Recent empirical research and theory suggest that elevated internalizing and externalizing symptoms constitute a distinct subclass of psychopathology (Willner et al., 2016) that may be triggered by adverse childhood experiences such as maltreatment (Dvir, Ford, Hill, & Frazier, 2014). Youth who exhibit such comorbid internalizing and externalizing problems over time may have a particularly heightened risk for suicidal ideation and behaviors. The integrated motivational-volitional theory of suicide suggests that both internalizing-related factors (e.g., thwarted belongingness, feelings of burdensomeness) and externalizing-related factors (e.g., impulsiveness) exacerbate the pathway towards suicidal ideation, intent, and behaviors (O’Connor, 2011). Thus, a comorbid pattern of internalizing and externalizing psychopathology is a third plausible developmental pathway between child maltreatment and the development of suicidal ideation and behaviors in adolescence. However, thus far no longitudinal research has examined internalizing and externalizing pathways concurrently to evaluate the comorbid symptom trajectory as a distinct pathway to suicidal ideation and behaviors or as a mediator in the association between child maltreatment and adolescent suicide risk.
The Present Study
There are several methodological challenges inherent in testing the hypothesis that comorbid symptom trajectories underlie the relation between child maltreatment and suicidal ideation and behaviors. These challenges include the need (a) to utilize multi-wave longitudinal data in order to examine change in internalizing and externalizing problems over time; (b) to simultaneously model patterns of internalizing and externalizing symptomology in order to investigate whether a comorbid trajectory is evident; and (c) to investigate nonlinear change in internalizing and externalizing symptoms. The present study sought to address these challenges by utilizing a person-centered methodological approach (i.e., bivariate growth mixture modeling), using five waves of multi-reporter longitudinal data. This person-centered modeling approach can be used to identify distinct clinical subgroups of symptomology within the sample, and to test whether there were individuals within the sample who exhibited concurrent elevations in internalizing and externalizing symptoms over time.
We hypothesized that more severe child maltreatment experiences would predict symptom trajectories characterized by higher levels of internalizing and/or externalizing psychopathology. Further, youth with stable-high or increasing internalizing and/ or externalizing behavior trajectories were expected to be at a greater risk for suicidal ideation, suicidal planning, and suicide attempts in adolescence. More specifically, we hypothesized that there would be a class of youth who exhibit concurrent elevations in internalizing and externalizing psychopathology and that membership in this distinct comorbid trajectory group would be predicted by child maltreatment and predictive of suicidal ideation and behaviors in adolescence.
Different types of maltreatment (physical and sexual abuse, emotional abuse, and neglect) have been shown to have differential effects on psychopathology, although findings in this area have been inconsistent (Manly, Kim, Rogosch, & Cicchetti, 2001; Moran et al., 2004; Oshri et al., 2015). Thus, the present study also attempted to discern the influence of maltreatment types on psychopathology and suicide risk. Additionally, we examined moderation by sex due to epidemiological data showing that adolescent girls report higher rates of suicidal ideation and behaviors (Kann et al., 2016). Similar studies have found that sex moderates the role of psychiatric symptomology (Brezo et al., 2008; Wanner et al., 2012) in predicting suicidal ideation and behaviors. These research objectives regarding the roles of maltreatment types and sex in the examined models were exploratory, and no directional hypotheses were made. Last, we controlled for variables that are associated with risk for psychopathology and suicidal ideation and behaviors, including income, transitions to foster families, and race.
Methods
Sample
The sample was obtained from the Longitudinal Studies on Child Abuse and Neglect (LONGSCAN) consortium of studies (N = 1,354; 51.48% female). The racial and ethnic makeup of the LONGSCAN sample is diverse, with 53.3% of the children identifying as African American, 26.2% as Caucasian, 7.2% as Hispanic, 11.9% as biracial or multiracial, and 1.5% as other. The data collection of the LONGSCAN study was conducted at five regional sites throughout the United States, and it included data from youth, caretakers, teachers, and child welfare specialists. The eligibility criteria for each data collection site was unique. For example, at the East site, families were selected for the study if they met criteria for being low-income or otherwise at risk (e.g., having a parent with HIV or having inadequate growth in their first two years), while at the Northwest site, families were selected for the study after being reported to Child Protective Services for suspected maltreatment (Larrabee & Lewis, 2014). The total sample at the time of recruitment included 65.3% of maltreated youth and 35.7% of nonmaltreated youth and their families. LONGSCAN researchers began collecting data when the children were approximately age 4 (Mage = 4.56, SD = 0.70) and revisited youth every two years until the final age-18 assessment (Mage = 18.51, SD = 0.62). Informed consent and assent was obtained from all individual participants included in the study (Runyan et al., 2014). In the present study, data from six waves were used: Time 1 (Mage = 6.42, SDage = 0.52); Time 2 (Mage = 8.27, SDage = 0.52); Time 3 (Mage = 9.83, SDage = 0.55); Time 4 (Mage = 12.37, SDage = 0.44); Time 5 (Mage =14.35, SDage = 0.45); and Time 6 (Mage = 16.32, SDage = 0.44).
Measures
Child maltreatment
Trained LONGSCAN researchers reviewed Child Protective Services records to code data on child maltreatment in accordance with the Modified Maltreatment Classification System (MMCS; English & LONGSCAN Investigators, 1997). The MMCS is a modification of the Maltreatment Classification System (MCS; Barnett, Manly, & Cicchetti, 1993), and it includes detailed codes for maltreatment characteristics such as time, subtype, and severity (Runyan et al., 1998). Four maltreatment subtypes were assessed: physical abuse, sexual abuse, emotional abuse, and neglect. For the present study, the severity of maltreatment for each type of maltreatment was coded on a continuum, with “1” representing less severe cases of abuse or neglect and “5” representing the most severe cases of abuse or neglect. Youth with no record of maltreatment were given a score of “0.” The maximum severity of each maltreatment type from birth to T1 (Mage = 6.42) and from T1 until T6 (Mage = 16.32) were utilized for the present analysis.
Behavior problems
Internalizing and externalizing symptomologies were assessed using the Child Behavior Checklist (CBCL; Achenbach, 1991). Primary caretakers reported on their child’s behavior problems approximately every two years from T1 (Mage = 6.42) to T5 (Mage =14.35). The internalizing scale consisted of a sum score of items on the subscales that measured withdrawn behaviors, anxious/depressive symptomology, and somatic symptoms. The externalizing scale consisted of a sum score of items on the subscales that measured aggressive behavior and delinquent behavior. Scores ranged from 0 to 62 for internalizing and from 0 to 66 for externalizing, with higher scores representing more severe behavior problems. Raw scores were utilized in the analysis as opposed to t-scores, as suggested for longitudinal growth models (Seltzer, Frank, & Byrk, 1994). The internal reliability coefficients were satisfactory for the internalizing problem scale (αT1 = .83, αT2 = .87, αT3 = .89, αT4 = .89, and αT5 = .89) and for the externalizing problem scale (αT1 = .91, αT2 = .92, αT3 = .93, αT4 = .92, and αT5 = .93).
Suicidal ideation and behaviors
Youth self-reported the presence of suicidal ideation and behaviors at the age-16 time point with the project-developed Adolescent Health Status and Service Utilization measure (Knight, Smith, Martin, Lewis, & LONGSCAN Investigators, 1998). For the present study, three dichotomous items were utilized: a variable indicating the presence of suicidal ideation (“During the last 12 months, did you ever seriously consider attempting suicide?”); a variable indicating the presence of a suicide plan (“During the last 12 months, did you make a plan about how you would attempt suicide?”); and a variable indicating if the youth had attempted suicide at least once in the past year. At the age-16 time point, 5.60% of youth reported that they had attempted suicide at least once in the past year, 8.85% reported seriously considering suicide, and 5.48% reported that they had made a suicide plan in the past year.
Covariates
Control variables included foster care placements, race, family income, and gender. Race was coded dichotomously as 0 = Caucasian and 1 = African American. At the age-6, age-8, and age-10 visits, the primary maternal caregiver reported on the number of times the child moved to foster care (including placements in group homes or shelters) in the past year. A sum score was created out of these variables. Family SES risk was measured using a cumulative score that included both objective and subjective indicators of socioeconomic status (Diemer, Mistry, Wadsworth, López, & Reimers, 2013). A score of 1 was given for the following four risk factors: caretakers having on average less than high school education, use of government financial assistance, income between $15,000 and $19,999 or less per year, and a response of either “somewhat bothered” or “bothered a great deal” to a question regarding worries about having money for basic necessities. Scores on this cumulative measure of socioeconomic disadvantage ranged from zero (not socioeconomically disadvantaged) to four (very socioeconomically disadvantaged), with a mean score of 1.95 (SD = 1.32). Lastly, gender was coded as 1 = male and 2 = female.
Analytic Plan
All analyses were performed using Mplus version 7.4 (Muthén & Muthén, 2017). In order to examine the general trends in growth of internalizing and externalizing problems in late childhood to adolescence, a bivariate (e.g., parallel process) growth model was conducted using internalizing and externalizing problems at age 6, 8, 10, 12, and 14. Time points were fixed to 0, 1, 2, 3, and 4, as there was an equidistant time span of two years between each time point. Internalizing and externalizing problems at each time point were allowed to covary. Linear and quadratic bivariate growth curves were both tested to determine the best growth curve solution.
To account for heterogeneity of growth trajectories in the sample, a growth mixture modeling approach was utilized. This allowed for the examination of distinct classes of internalizing and externalizing trajectories. Class solutions were examined for two through five classes and were compared using various fit indices. Entropy was evaluated in order to determine how accurate classifications were for each class solution; values close to 1.0 were considered to have good entropy (Wickrama, Lee, O’Neal, & Lorenz, 2016). In addition, information criterion statistics such as the Bayesian information criterion (BIC) and the Akaike information criterion (AIC) were used, with lower values indicating a better class solution. Furthermore, a Lo-Mendell-Rubin (VLMR) likelihood ratio test was utilized to test the class solution (k) against the null hypothesis class solution (k-1). Prior empirical work, theory, and interpretability were also considered when choosing the best class solution, as recommended by Wickrama and colleagues (2016).
Predictors and outcomes of the distinct classes were examined using Lanza’s three-step approach (Lanza, Tan, & Bray, 2013). The three-step approach allows for the examination of covariates (e.g., predictors and outcomes) of latent growth classes without altering the original properties of the class solutions (Wickrama et al., 2016). The continuous predictors of the categorical class solutions were tested by using a multinomial regression framework. Several predictors were tested. First, we examined the influence of control variables on internalizing and externalizing trajectories. We then examined the influence of child maltreatment severity (by type) from birth to age 6 on internalizing and externalizing trajectories. Additionally, we examined the influence of a common maltreatment factor, which was derived from a latent factor of the four maltreatment types from birth to age 6. The moderating role of gender was explored by examining the influence of interaction terms (Maltreatment type × Gender) on internalizing and externalizing trajectories. Last, we tested whether the class solutions would significantly predict suicide-related outcomes by conducting chi-square tests of significance to compare probabilities of suicide-related outcomes across classes.
Following, a series of multiple mediation tests were run using the conditional probability of class membership as a mediator and suicidal ideation, suicidal planning, and suicide attempts as outcomes. We chose to utilize the severity of different maltreatment types (i.e., physical abuse, sexual abuse, emotional abuse, and neglect) from birth through age 6 as independent variables to preserve the temporal ordering in the mediational model. In each model, we also included the severity of maltreatment that occurred between ages 6 and 16 as a competing mediator, as it is possible that proximal maltreatment experiences also predict suicide-related behaviors at age 16. Control variables included SES risk, race, gender, and foster care status. Nonsignificant covariates were trimmed from the final model. Mediation was tested using the product of coefficients method via Mplus, with a weighted least square mean and variance adjusted (WLSMV) estimator to account for the categorical outcome variables. To reduce the inflated Type I error rate that is expected when testing multiple hypotheses, we utilized the False Discovery Rate (FDR) procedure for our multiple tests of mediation, as recommended for multiplicity control in SEM designs (Cribbie, 2007).
Results
Descriptive Statistics and Correlations
Descriptive statistics and bivariate correlations are shown in Table 1. Variables that represented severity of physical and sexual abuse between birth and age 6 were transformed by taking the natural logarithm, due to high positive skewness (>2.00). The percentage of missing data ranged from 0% to 41%. At the age-16 time point, child interviews were conducted with 59% of the original sample. Thus, the majority of missing data were due to attrition. Little’s MCAR test was significant, χ2 = 1710.26, p < .001, suggesting that data was not missing completely at random (MCAR). Thus, a correlation analysis was subsequently utilized to determine if missingness on modeled variables were related to observed data. Analyses were consistent with the assumption of data missing at random (MAR; Schafer & Graham, 2002). There was evidence that missing data were related to observed study variables. For example, data missingness on suicidal ideation at age 16 was related to the number of times of attempted suicide at age 16. Thus, data analyses were conducted using the full information maximum likelihood method (Enders & Bandalos, 2001). Full information maximum likelihood has been recommended for models with MAR data, as it has been shown to result in less biased parameter estimates than those generated by other methods of handling missing data, such as listwise deletion.
Table 1.
Correlation analysis and descriptive statistics of study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Physical Abuse | - | |||||||||||||||||||||
| 2. Sexual Abuse | .23** | - | ||||||||||||||||||||
| 3. Neglect | .33** | .21** | - | |||||||||||||||||||
| 4. Emotional Abuse | .36** | .22** | .37** | - | ||||||||||||||||||
| 5. Maltreatment factor | .73** | .46** | .70** | .78** | - | |||||||||||||||||
| 6. Internalizing (Age 6) | .05 | .09** | .07* | .08** | .10** | - | ||||||||||||||||
| 7. Internalizing (Age 8) | .07* | .17** | .08* | .04 | .11** | .57** | - | |||||||||||||||
| 8. Internalizing (Age 10) | .12** | .15** | .10** | .08* | .15** | .49** | .58** | - | ||||||||||||||
| 9. Internalizing (Age 12) | .09** | .11** | .06 | .08** | .12** | .48** | .54** | .65** | - | |||||||||||||
| 10. Internalizing (Age 14) | .15** | .11** | .14** | .12** | .19** | .41** | .46** | .53** | .65** | - | ||||||||||||
| 11. Externalizing (Age 6) | .11** | .10** | .15** | .13** | .18** | .60** | .41** | .37** | .40** | .36** | - | |||||||||||
| 12. Externalizing (Age 8) | .12** | .13** | .15** | .08** | .17** | .40** | .62** | .43** | .44** | .42** | .69** | - | ||||||||||
| 13. Externalizing (Age 10) | .15** | .12** | .16** | .10** | .19** | .34** | .41** | .66** | .48** | .44** | .58** | .68** | - | |||||||||
| 14. Externalizing (Age 12) | .14** | .07* | .13** | .11** | .17** | .34** | .38** | .45** | .65** | .54** | .56** | .63** | .70** | - | ||||||||
| 15. Externalizing (Age 14) | .17** | .09** | .15** | .12** | .19** | .29** | .33** | .39** | .48** | .70** | .50** | .54** | .60** | .73** | - | |||||||
| 16. Suicidal Ideation | .02 | .08* | .01 | .05 | .05 | .01** | .11** | .13** | .18** | .18** | .12** | .13** | .12** | .17** | .12** | - | ||||||
| 17. Suicidal Plan | .09* | .12** | .01 | .04 | .08* | .08* | .10** | .13** | .17** | .21** | .08* | .12** | .09* | .14** | .10* | .64** | - | |||||
| 18. Suicidal Attempts | .03 | .08** | .01 | .03 | .05 | .11** | .13** | .18** | .21** | .25** | .10** | .14** | .14** | .15** | .16** | .68** | .58** | - | ||||
| 19. Family SES Risk | .03 | −.08** | .00 | .03 | .01 | .07* | .06 | −.04 | .01 | .01 | .06* | .06 | .01 | .08* | .07 | .01 | .00 | −.03 | - | |||
| 20. Race | −.26** | −.19** | −.19** | −.19** | −.29** | −.10** | −.13** | −.13** | −.15** | −.14** | −.08** | −.12** | −.07* | −.11** | −.09** | −.07* | −.08* | −.08* | .20** | - | ||
| 21. Gender | −.03 | .14** | −.01 | .01 | .02 | .05 | .00 | −.03 | .00 | .08* | −.08** | −.11** | −.17** | −.13** | −.04 | .13** | .14** | .11** | −.04 | .03 | - | |
| 22. Foster care placement | .13** | .12** | .12** | .04 | .14** | .11** | .10** | .06 | .09** | .16** | .10** | .13** | .84** | .06 | .09** | .04 | .08* | .07 | −.05 | −.08** | −.01 | - |
| Mean | 0.12 | 0.07 | 2.68 | 1.03 | 0.80 | 6.38 | 6.92 | 6.52 | 7.54 | 7.53 | 13.14 | 12.40 | 11.40 | 12.02 | 11.90 | 0.09 | 0.05 | 0.06 | 1.97 | 0.53 | 1.52 | 0.04 |
| Percent (%)a | 14.77 | 6.20 | 41.43 | 17.43 | 8.85 | 5.48 | 5.60 | 53.25 | 51.48 | |||||||||||||
| SD | 0.23 | 0.20 | 3.27 | 1.97 | 0.95 | 5.68 | 6.41 | 6.73 | 6.87 | 7.21 | 8.95 | 9.15 | 9.45 | 9.68 | 10.27 | 0.28 | 0.23 | 0.43 | 1.30 | 0.50 | 0.50 | 0.30 |
Note: Maltreatment variables represent the maximum severity of abuse from birth to age 6. Race was coded dichotomously with 0 = Caucasian and 1 = African American. Gender was coded as 0 = male and 1 = female.
For dichotomous variables, the percentage of participates who indicated “yes” is shown. For maltreatment variables, the percentage of participants who experienced each type of abuse is indicated. For race and gender, the percentage of participants who identified respectively as African American or female is shown.
p < .05,
p < .01.
Unconditional Bivariate Growth Curve Model
A bivariate growth curve was tested to inspect the average initial point (intercept), growth trajectories (slope), and variance of internalizing and externalizing symptomology over five points from ages 6 to 14. The model with quadratic terms fit the data significantly better than the model without quadratic terms, Δχ2 = 104.82, p < .001, so quadratic terms were included in all subsequent models. The final unconditional bivariate growth curve model had excellent fit, CFI = .99; SRMR = .02; χ2/df = 1.85. See Figure 1 for a depiction of the average growth trends for internalizing and externalizing symptomology between ages 6 and 14. After the analysis was conducted, in order to interpret the clinical significance of these average growth curves, mean raw scores of internalizing and externalizing at each time point were converted to T scores. The average scores for internalizing or externalizing symptomology in the total sample were not clinically significant (See Supplemental Figure 1). Internalizing symptomology had a significant intercept, B = 6.42; 95% CI [1.17, 1.43], and nonsignificant slope, B = .23; 95% CI [−.03, .18], and quadratic growth term, B = .63; 95% CI [−.09, .14]. Externalizing symptomology had a significant intercept, B = 13.13; 95% CI [1.49, 1.72], slope, B = −1.06; 95% CI [−.35, −.15], and quadratic growth term, B = .20; 95% CI [.10, .32]. Notably, the variance of the slope and intercept for both internalizing and externalizing symptomology was significant (p < .001). These variances indicated that there was a potential for significant variability in symptom intercepts and growth trajectories within the LONGSCAN sample. Therefore, a growth mixture model was subsequently utilized to examine whether there were unobserved subgroups of youth with diverging symptom growth trajectories.
Figure 1.
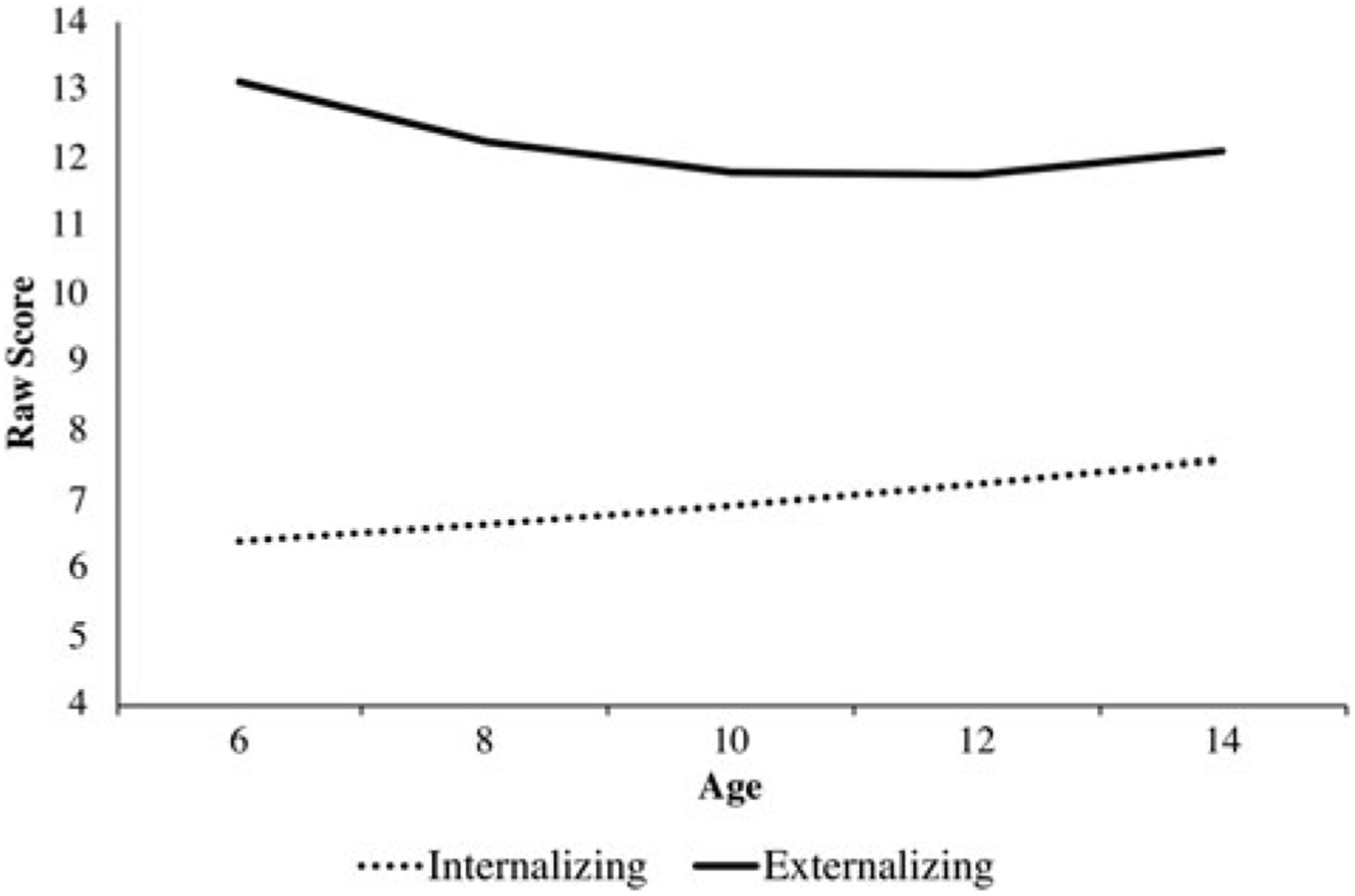
Bivariate growth curve with quadratic terms.
Class Solutions
In order to determine the most optimal class solution, the quadratic growth model was run with two through five classes. Fit indices and theoretical interpretability of each model was compared. The class solutions and fit indices are presented in Table 2. The four-class solution was statistically and theoretically the optimal solution, based on the lower AIC and BIC and higher entropy score than the three-class solution.1 Furthermore, although the five-class solution exhibited good statistical fit criteria in terms of entropy, AIC, and BIC, there existed two classes with less than 3% of the sample, which were deemed to be statistically unrepresentative and to have limited generalizability (Wickrama et al., 2016). Thus, we chose the four-class solution. The four trajectories were named based on the pattern of change of internalizing and externalizing symptoms over time: the high comorbidity class (6.43% of sample); the high externalizing class (7.96% of sample); the moderate and decreasing class (3.37% of sample); and the low symptomology class (82.25% of sample). See Figure 2 for a graphic displaying the growth curve for each of these classes and Table 3 for the intercept and growth curve characteristics of each class. In Figure 2, we have displayed the four classes according to their mean T-score at each time point to facilitate interpretation. T-scores greater than 63 are considered to be clinically significant (Achenbach, 1991).
Table 2.
Fit statistics across the growth mixture class solutions (N = 1,307)
| SC N (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Classes | AIC | BIC | Adj BIC | Entropy | VLMR (p) | C1 | C2 | C3 | C4 | C5 |
| 2 | 65643.792 | 65897.391 | 65741.741 | .913 | 235.011 (.234) | 1214 (93%) | 93 (7%) | |||
| 3 | 65406.623 | 65696.450 | 65518.565 | .874 | −76.479 (.108) | 112 (9%) | 106 (8%) | 1089 (83%) | ||
| 4 | 65246.560 | 65572.616 | 65372.494 | .886 | 89.780 (.298) | 1075 (82%) | 104 (8%) | 84 (6%) | 44 (3%) | |
| 5 | 65130.657 | 65492.941 | 65270.584 | .888 | −34.602 (.139) | 111 (8%) | 1033 (79%) | 34 (3%) | 12 (1%) | 106 (8%) |
Note: AIC = Akaike information criterion; BIC = Bayesian information criteria; VLMR = Vuong-Lo-Mendell-Rubin Likelihood ratio test; SC = smallest class size. Lower values of AIC and BIC and higher values of entropy and probabilities indicate better model fit. Chosen class is shown in bold.
Figure 2.
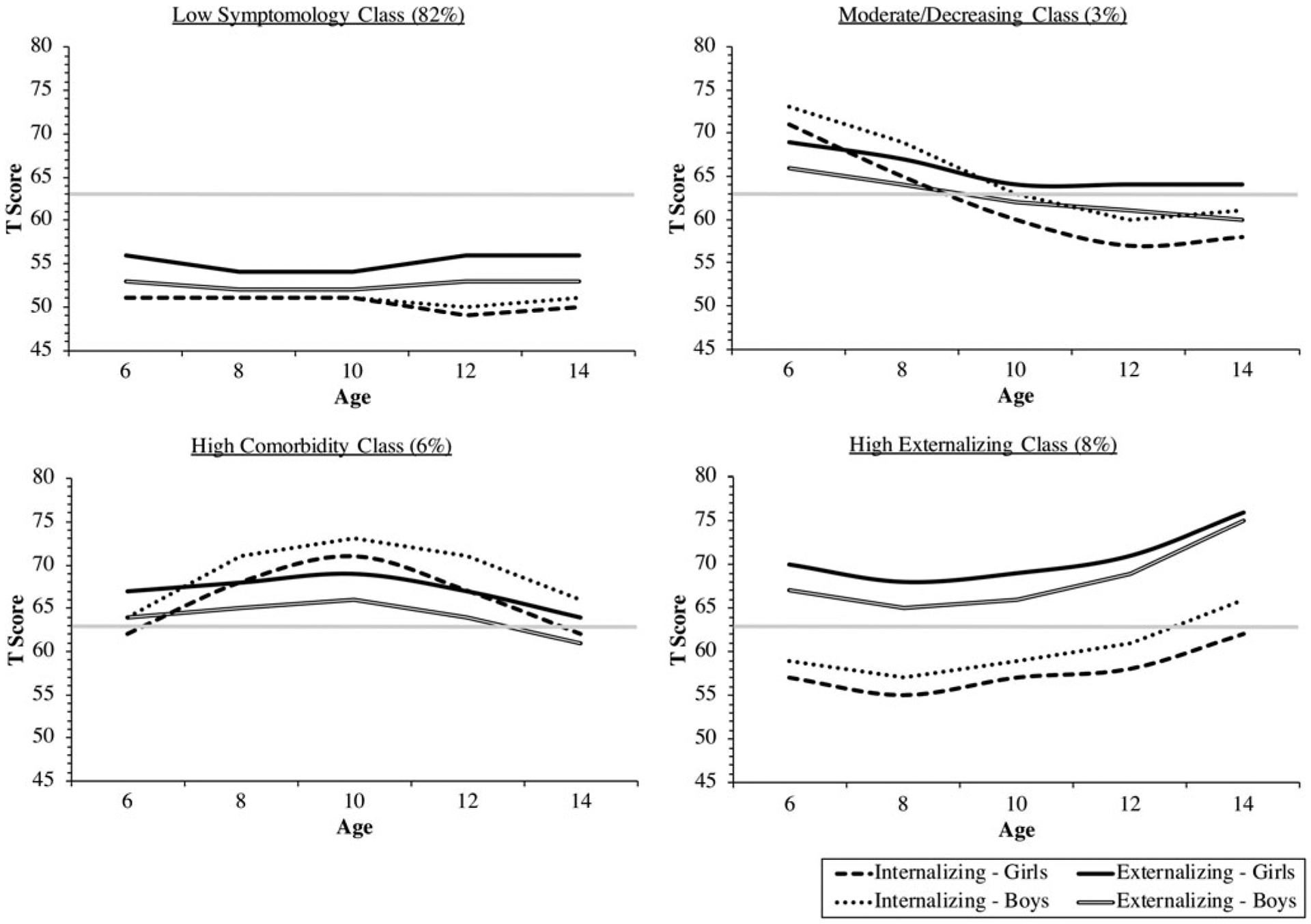
Four-class bivariate growth curve solution. On each graph, the gray line represents the clinical cut off score. T scores greater than 63 are considered to be clinically significant.
Table 3.
Growth factor parameter estimates for four-class unconditional model (N = 1,307)
| Internalizing Problems Est.(SE) | Externalizing Problems Est.(SE) | ||||||
|---|---|---|---|---|---|---|---|
| Trajectories | n (%) | Intercept | Slope | Quadratic | Intercept | Slope | Quadratic |
| High Comorbidity | 84 (6.43%) | 12.93 (1.36)*** | 8.01 (1.36)*** | −1.79 (1.92)*** | 19.93 (1.93)*** | 2.25 (1.36) | −0.73 (0.31)* |
| High Externalizing | 104 (7.96%) | 8.72 (0.85)*** | −1.69 (0.96) | 0.88 (0.23)*** | 22.70 (1.55)*** | −3.92 (1.63)* | 1.77 (0.45)*** |
| Moderate/Decreasing | 44 (3.37%) | 21.95 (2.38)*** | −7.09 (1.96)*** | 1.14 (0.54)* | 22.22 (2.53)*** | −2.70 (2.14) | 0.28 (0.52) |
| Low Symptomology | 1075 (82.25%) | 4.93 (0.22)*** | 0.07 (0.29) | 0.04 (0.06) | 11.11 (0.31)*** | −1.01 (0.27)*** | 0.12 (0.07) |
Note: Est. = estimate; SE = standard error.
p < .05;
p < .01;
p < .001.
Predictors
See Table 4 for the results of the multinomial regression analysis. Overall, adolescents who experienced more severe physical abuse were more likely to belong to the high comorbidity class compared with the moderate/decreasing class, OR = 7.03, p < .05; 95% CI [1.15, 42.91], and adolescents who experienced more severe sexual abuse were more likely to belong to the high comorbidity class compared with the low symptomology group, OR =3.06, p < .05; 95% CI [1.06, 8.84]. Adolescents who identified as African-American were less likely to belong to the comorbidity class as compared with the high externalizing class, OR = 0.33, p < .05; 95% CI [0.14, 0.82], and the low symptomology class, OR = 0.36, p < .01; 95% CI [0.18, 0.73]. Additionally, the Gender by Sexual Abuse interaction term significantly predicted membership in the high comorbidity group compared with the low symptomology group, OR = 1.79, p < 01; 95% CI [1.08, 2.99], indicating that the influence of sexual abuse on class membership in the high comorbidity symptom profile was moderated by gender. Specifically, girls who had experiences of sexual abuse were 1.8 times more likely than boys to exhibit higher levels of comorbid psychopathology rather than low levels of psychopathology.
Table 4.
Multinomial logistic regression ORs and CIs for predictors (N = 1,307)
| High comorbidity vs. | High comorbidity vs. | High comorbidity vs. | High EXT vs. | High EXT vs. | Mod/Dec vs. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High EXT (c) | Mod/Dec (c) | Low (c) | Mod/Dec (c) | Low (c) | Low (c) | |||||||
| Model Predictors | Logit (OR) | 95%CI | Logit (OR) | 95%Cl | Logit (OR) | 95%Cl | Logit (OR) | 95%Cl | Logit (OR) | 95%CI | Logit (OR) | 95%CI |
| Control | ||||||||||||
| SES Risk | 0.11 (1.11) | [0.76, 1.63] | 0.08 (1.08) | [0.70, 1.67] | 0.16 (1.17) | [0.90, 1.53] | −0.03 (0.98) | [0.63, 1.50] | 0.05 (1.06) | [0.79, 1.41] | 0.08 (1.08) | [0.77, 1.51] |
| Race | −1.10 (0.33) | [0.14, 0.82]* | −0.27 (0.77) | [0.24, 2.43] | −1.01 (0.36) | [0.18, 0.73] ** | 0.83 (2.30) | [0.77, 6.88] | 0.09 (1.09) | [0.58, 2.04] | −0.75 (0.47) | [0.19, 1.19] |
| Gender | 0.37 (1.44) | [0.59, 3.51] | 0.10 (1.10) | [0.36, 3.35] | 0.00 (1.00) | [0.50, 2.00] | −0.27 (0.76) | [0.27, 2.17] | −0.36 (0.70) | [0.38, 1.29] | −0.09 (0.91) | [0.38, 2.18] |
| Foster care placements | −0.39 (0.68) | [0.43, 1.06] | −0.16 (0.85) | [0.43, 1.69] | −0.37 (0.69) | [0.48, 0.99] | 0.23 (1.26) | [0.65, 2.45] | 0.35 (1.42) | [1.04, 1.95] * | 0.12 (1.13) | [0.63, 2.02] |
| Maltreatment type | ||||||||||||
| Physical abuse | 0.10 (1.11) | [0.3, 4.13] | 1.95 (7.03) | [1.15, 42.91]* | 0.96 (2.61) | [0.97, 7.03] | 1.85 (6.33) | [1.05, 38.14] * | 0.86 (2.35) | [0.83, 6.63] | −0.99 (0.37) | [0.08, 1.78] |
| Sexual abuse | 0.17 (1.19) | [0.31, 4.53] | 0.20 (1.22) | [0.22, 6.85] | 1.12 (3.06) | [1.06, 8.84] * | 0.03 (1.03) | [0.20, 5.33] | 0.95 (2.58) | [0.92, 7.23] | 0.92 (2.51) | [0.60, 10.50] |
| Emotional | 0.01 (1.01) | [0.84, 1.22] | −0.11 (0.90) | [0.72, 1.12] | 0.00 (1.00) | [0.86, 1.16] | −0.12 (0.89) | [0.72, 1.09] | −0.01 (0.99) | [0.86, 1.13] | 0.11 (1.12) | [0.94, 1.33] |
| Neglect | −0.06 (0.94) | [0.85, 1.04] | −0.08 (0.92) | [0.81, 1.05] | 0.02 (1.02) | [0.94, 1.10] | −0.01 (0.99) | [0.87, 1.11] | 0.08 (1.08) | [1.01, 1.16] * | 0.09 (1.1) | [0.99, 1.22] |
| Maltreatment factor | −0.05 (0.95) | [0.63, 1.44] | 0.44 (1.56) | [0.86, 2.81] | 0.43 (1.53) | [1.11, 2.11]* | 0.49 (1.63) | [0.92, 2.90] | 0.47 (1.60) | [1.18, 2.19]** | −0.02 (0.98) | [0.59, 1.65] |
| Moderation by gender | ||||||||||||
| Physical abuse × gender | −0.31 (0.73) | [0.38, 1.39] | 0.41 (1.50) | [0.60, 3.77] | 0.02 (1.02) | [0.60, 1.74] | 0.72 (2.05) | [0.90, 4.65] | 0.33 (1.39) | [0.91, 2.12] | −0.39 (0.68) | [0.33, 1.41] |
| Sexual abuse × gender | 0.45 (1.57) | [0.81, 3.04] | 0.39 (1.47) | [0.58, 3.73] | 0.59 (1.79) | [1.08, 2.99] * | −0.06 (0.94) | [0.36, 2.42] | 0.14 (1.14) | [0.67, 1.95] | 0.20 (1.22) | [0.54, 2.73] |
| Emotional × gender | 0.17 (1.19) | [0.63, 2.23] | −0.24 (0.79) | [0.36, 1.70] | 0.09 (1.10) | [0.67, 1.81] | −0.41 (0.66) | [0.33, 1.33] | −0.08 (0.92) | [0.60, 1.43] | 0.33 (1.4) | [0.79, 2.47] |
| Neglect × gender | −0.49 (0.61) | [0.37, 1.00] | −0.20 (0.82) | [0.48, 1.42] | −0.05 (0.95) | [0.64, 1.43] | 0.29 (1.34) | [0.84, 2.13] | 0.44 (1.55) | [1.13, 2.14] ** | 0.15 (1.16) | [0.81, 1.66] |
Note: High EXT = high externalizing; Mod/Dec = moderate/decreasing; Low = low symptomology. Gender is coded as 1 = male and 2= female; Race was coded as 0 = Caucasian and 1 = African American. Classes marked as (c) serve as the comparison group. OR = odds ratio; SE = standard error; CI = confidence interval; Emotional = emotional abuse.
p < .05;
p < .01;
p < .001.
Adolescents who experienced more severe physical abuse were significantly more likely to be in the high externalizing group rather than the moderate/decreasing group, OR = 6.33, p < .05; 95% CI [1.05, 38.14]. Further, adolescents who had more foster care placements and who experienced more severe neglect were significantly more likely to belong to the high externalizing group as compared with the low symptomology group, OR =1.42, p < .05; 95% CI [1.04, 1.95]; OR = 1.08, p < .05; 95% CI [1.01, 1.16], respectively. Girls who experienced neglect were significantly more likely to belong to the high externalizing group over the low symptomology group, OR = 1.55, p < .01; 95% CI [1.13, 2.14].
Outcomes
See Table 5 for the results comparing classes of externalizing and internalizing symptom trajectories in relation to suicide-related outcomes. The high comorbidity class had a significantly higher probability of suicidal ideation, presence of a suicide plan, and suicide attempt in the past year compared with the low symptomology class, χ2 (1) = 5.62, p < .05; χ2 (1) = 4.46, p < .05; and χ2(1) = 4.90, p < .05, respectively. Adolescents in the high comorbidity class had a 23% probability of suicidal ideation, a 16% probability of having a suicide plan, and a 17% probability of having at least one suicide attempt in the previous year.
Table 5.
Probabilities and χ2 differences for continuous outcomes (N = 1,307)
| High comorbid vs. | High comorbid vs. | High comorbid vs. | High EXT vs. | High EXT vs. | Mod/Dec vs. | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| High EXT | Mod/Dec | Low | Mod/Dec | Low | Low | |||||||||||||
| Outcomes | P1 | P2 | χ2 | P1 | P2 | χ2 | P1 | P2 | χ2 | P1 | P2 | χ2 | P1 | P2 | χ2 | P1 | P2 | χ2 |
| Suicidal ideation | .23 | .14 | 1.00 | .23 | .12 | 1.19 | .23 | .07 | 5.62* | .14 | .12 | 0.09 | .14 | .07 | 1.74 | .12 | .07 | 0.48 |
| Suicide Plan | .16 | .08 | 1.37 | .16 | .11 | 0.36 | .16 | .04 | 4.46* | .08 | .11 | 0.20 | .08 | .04 | 0.74 | .11 | .04 | 1.62 |
| Suicide Attempt | .17 | .07 | 1.87 | .17 | .12 | 0.35 | .17 | .04 | 4.90* | .07 | .12 | 0.39 | .07 | .04 | 0.58 | .12 | .04 | 1.65 |
Note: High EXT = high externalizing; Mod/Dec = moderate/decreasing; Low = low symptomology. P1 is the probability of the group on the top line, and P2 is the probability of the group on the second line.
Tests of Mediation
See Table 6 for results from the tests of mediation. There were several significant indirect effects (See Figure 3). We accounted for multiple comparisons by using the FDR procedure, and all findings retained their significance. The probability of belonging to the high comorbidity class mediated the association between severity of sexual abuse from birth to age 6 and suicidal ideation, α*β = .06, SE = .03, p < .05; 95% CI [.01, .11], suicidal planning, α*β = .06, SE = .03, p < .05; 95% CI [.00, .11], and suicide attempts at age 16, α*β = .07, SE = .03, p < .05; 96% CI [.01, .12]. The indirect effects between physical abuse from birth to age 6 and suicide-related outcomes were marginally significant. Figure 3 depicts the three models with a significant indirect effect through the high comorbidity class.
Table 6.
Tests of indirect effects between childhood maltreatment types and suicidal ideation and behaviors
| Suicide Attempts | α*β | SE | p | 95% CI |
|---|---|---|---|---|
| Model 1 | ||||
| PA (Birth-6) → Comorbidity → Attempts | .043 | .023 | .056a | [−.001, .088] |
| PA (Birth-6) → PA (6–16) → Attempts | .125 | .058 | .031* | [.012, .238] |
| Model 2 | ||||
| SA (Birth-6) → Comorbidity → Attempts | .067 | .028 | .015* | [.013, .122] |
| SA (Birth-6) → SA (6–16) → Attempts | .101 | .043 | .018* | [.018, .185] |
| Model 3 | ||||
| EM (Birth-6) → Comorbidity → Attempts | .012 | .015 | .425 | [−.017, .041] |
| EM (Birth-6) → EM (6–16) → Attempts | .078 | .042 | .064a | [−.005, .160] |
| Model 4 | ||||
| Neglect (Birth-6) → Comorbidity → Attempts | .010 | .013 | .444 | [−.015, .034] |
| Neglect (Birth-6) → Neglect (6–16) → Attempts | −.029 | .053 | .587 | [−.134, .076] |
| Suicidal Ideation | ||||
| Model 5 | ||||
| PA (Birth-6) → Comorbidity → SI | .040 | .021 | .059a | [−.002, .081] |
| PA (Birth-6) → PA (6–16) → SI | .072 | .053 | .175 | [−.032, .176] |
| Model 6 | ||||
| SA (Birth-6) → Comorbidity → SI | .061 | .026 | .019* | [.010, .112] |
| SA (Birth-6) → SA (6–16) → SI | .081 | .040 | .029* | [.009, .168] |
| Model 7 | ||||
| EM (Birth-6) → Comorbidity → SI | .011 | .013 | .426 | [−.015, .037] |
| EM (Birth-6) → EM (6–16) → SI | .084 | .036 | .020* | [.013, .154] |
| Model 8 | ||||
| Neglect (Birth-6) → Comorbidity → SI | .009 | .011 | .443 | [−.014, .031] |
| Neglect (Birth-6) → Neglect (6–16) → SI | .053 | .039 | .178 | [−.024, .130] |
| Suicide Plan | ||||
| Model 9 | ||||
| PA (Birth-6) → Comorbidity → Plan | .038 | .021 | .073a | [−.004, .080] |
| PA (Birth-6) → PA (6–16) → Plan | .140 | .053 | .008** | [.037, .244] |
| Model 10 | ||||
| SA (Birth-6) → Comorbidity → Plan | .059 | .028 | .035* | [.004, .113] |
| SA (Birth-6) → SA (6–16) → Plan | .117 | .044 | .007** | [.031, .203] |
| Model 11 | ||||
| EM (Birth-6) → Comorbidity → Plan | .011 | .013 | .430 | [−.016, .037] |
| EM (Birth-6) → EM (6–16) → Plan | .141 | .042 | .001** | [.059, .224] |
| Model 12 | ||||
| Neglect (Birth-6) → Comorbidity → Plan | .009 | .012 | .446 | [−.014, .028] |
| Neglect (Birth-6) → Neglect (6–16) → Plan | .073 | .044 | .099 a | [−.014, .159] |
Figure 3.
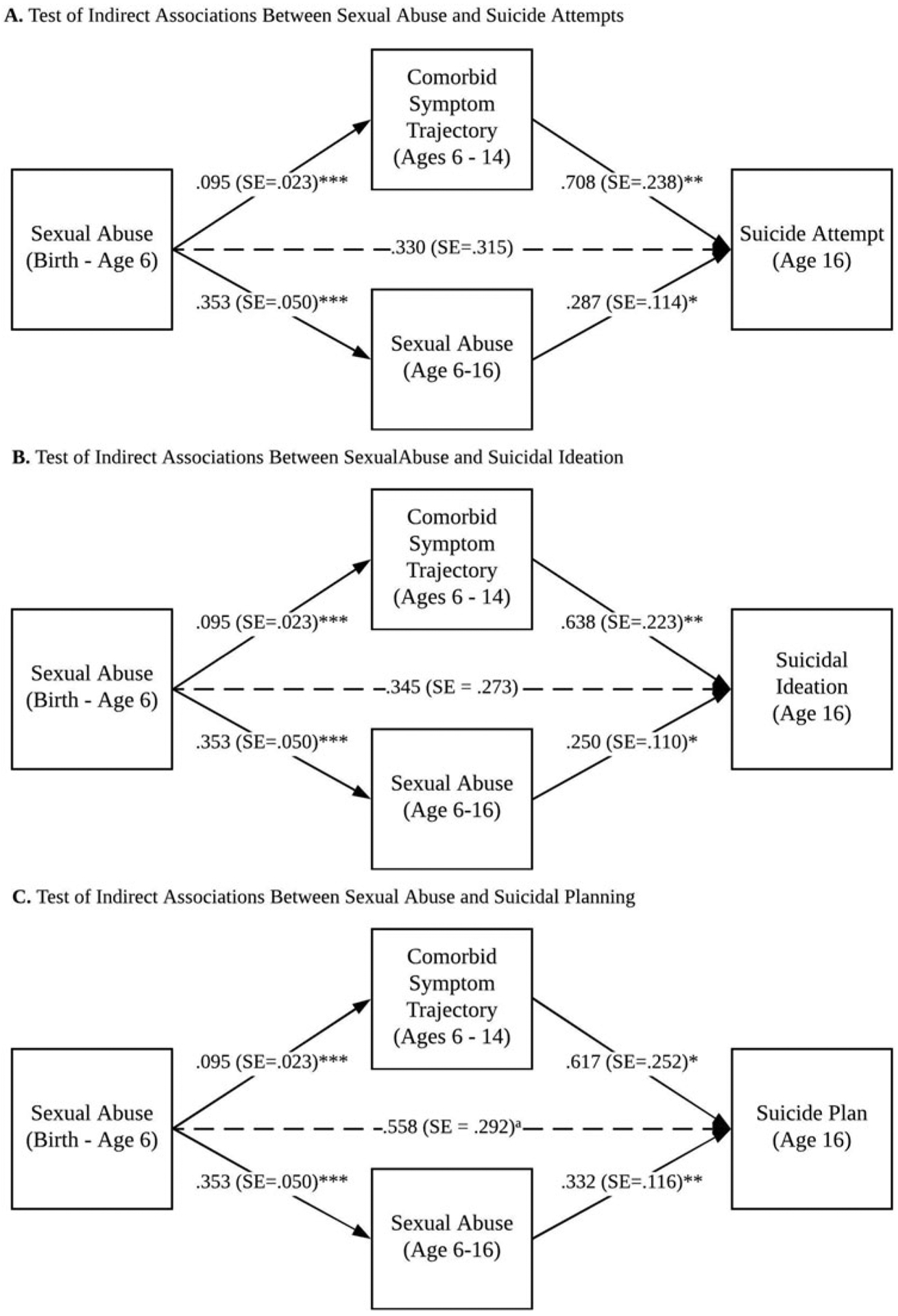
Tests of mediation. Unstandardized parameter estimates are shown in figure. ap < .10, *p < .05, **p < .01, ***p < .001.
There were also several significant indirect effects between child maltreatment from birth to age 6 and suicide-related outcomes via late childhood and adolescent maltreatment. Physical abuse from age 6 to 16 mediated the association between physical abuse from birth to age 6 and suicide attempts, α*β = .13, SE = .06, p < .05; 95% CI [.01, .24], as well as suicide planning, α*β = .14, SE = .05, p < .01; 95% CI [.04, .24]. Sexual abuse from age 6 to 16 mediated the association between early childhood sexual abuse and suicide attempts, α*β = .10, SE = .04, p < .05; 95% CI [.02, .19], suicidal ideation, α*β = .08, SE = .04, p < .05; 95% CI [.01, .17], and suicidal planning, α*β = .12, SE = .04, p < .01; 95% CI [.03, .20]. Additionally, late childhood and adolescent emotional abuse mediated the association between early childhood emotional abuse and suicidal ideation, α*β = .08, SE = .04, p < .05; 95% CI [.01, .15], and suicidal planning, α*β = .14, SE = .04, p < .01; 95% CI [.06, .22].
Discussion
Internalizing and externalizing behavior problems are two major developmental pathways that underlie the link between child maltreatment and suicidal ideation and behaviors in adolescence (Rytilä-Manninen et al., 2018; Wanner et al., 2012). However, to date, these two mechanisms have largely been modeled as independent processes. Using a person-centered analytical strategy (i.e., bivariate growth mixture modeling), we examined the presence of multiple trajectories of internalizing and externalizing symptoms within the sample. The analysis revealed four separate trajectories of psychopathology from middle childhood through adolescence. Notably, the analyses revealed that approximately6.4% of the sample belonged to a class of youth with concurrent elevations in both externalizing and internalizing problems over time, referred to as the high comorbidity class. Further, we hypothesized that child maltreatment would predict heterogeneous trajectories of internalizing and externalizing symptomology. In support of our hypothesis, child maltreatment severity and types differentially predicted membership in internalizing and externalizing symptom trajectories. Analyses revealed that several measures of child maltreatment significantly predicted group membership in the high comorbidity class. Youth who were more severely sexually abused were approximately three times more likely to be in the high comorbidity class than the low symptomology class, and youth who were more severely physically abused were approximately seven times more likely to be in the high comorbidity class than the moderate and decreasing class. We also hypothesized that individuals who followed symptom trajectories characterized by high comorbidity would be more at risk for suicidal ideation, suicidal planning, and suicide attempts in adolescence. Our findings supported this hypothesis, as youth in the high comorbidity class were significantly more at risk for suicide-related outcomes compared with youth in the low symptomology class. Last, corroborating our hypothesis, mediation analyses showed that membership in the high comorbidity symptom trajectory mediated the association between sexual abuse and three suicide-related outcomes in adolescence.
The findings of the current study suggest that comorbid elevations in internalizing and externalizing symptoms may serve as a distinct developmental trajectory that mediates the association between child maltreatment and adolescent suicidal ideation and behaviors. Specifically, in the current study, sexual and physical abuse were more likely to lead to concurrent elevations in internalizing and externalizing symptoms. There are several developmental mechanisms that may be implicated in the association between physical and sexual abuse and comorbid internalizing and externalizing psychopathology. Early-life child abuse is a significant threat to development that may disrupt a child’s attainment of self-regulation skills, resulting in heightened reactivity and emotion dysregulation (Dvir et al., 2014). Indeed, recent research suggests that early experiences such as maltreatment can alter neurocognitive development and, accordingly, influence how youth respond to emotional stimuli (for a review, see Pollak, 2008). Maltreatment has also been linked with poor impulse control in adolescence (e.g., Arens, Gaher, & Simons, 2012; Oshri, Kogan, et al., 2018), which is characteristic of youth with externalizing disorders. The combination of heightened emotion dysregulation and poor impulse control may exacerbate vulnerability for risky behaviors like suicidal ideation and behaviors during adolescence. Adolescent youth are often faced with stressors that stem from pubertal changes, identity development, and peer contexts. When faced with these acute stressors, adolescents with poor emotion regulation and poor impulse control may be more likely to exhibit negative emotionality and to act upon this negative emotionality by engaging in suicidal ideation and behaviors.
Another notable finding was that the majority of youth in the LONGSCAN sample belonged to the low symptomology class (N = 1,074, 82.2%). These youth, who displayed low levels of psychopathology despite experiences of early life adversity, can be said to follow a resilient developmental pathway. Resilience is typically defined as a developmental process wherein the individual pursues positive adaptation after significant adversity, such as child maltreatment (Luthar, Cicchetti, & Becker, 2000). In the present study, the majority of the sample consisted of youth who were maltreated or who were recruited into the study due to different risk factors (e.g., being in poverty or having a parent with HIV). Thus, the high percentage of youth who belonged to the low symptomology class may have been able to overcome these adversities and maintain psychological health throughout childhood and adolescence. Other empirical studies have similarly found that large percentages of at-risk youth are often able to follow resilient trajectories and avoid significant psychopathology (Collishaw et al., 2007; Masten, 2014; Oshri, Duprey, Kogan, Carlson, & Liu, 2018; Rutter, Kreppner, & O’Connor, 2001).
The present study considered the influence of maltreatment timing (broadly defined as early childhood versus late childhood and adolescence) in the pathway to suicidal ideation and behaviors in adolescence. Maltreatment is often a chronic experience, and early childhood experiences of child abuse may lead to revictimization during later childhood and adolescence (Hindley, 2006). Indeed, our mediation models showed that child maltreatment measured from birth to age 6 significantly predicted maltreatment measured from ages 6 to 16. We found evidence that proximal experiences of sexual abuse and emotional abuse (ages 6–16 years) and comorbid internalizing/externalizing symptomology predicted suicidal ideation and behaviors in adolescence. Further, after adding late childhood and adolescent maltreatment to the mediation models, the direct association between early childhood maltreatment and suicide-related outcomes was no longer present, indicating the importance of considering the role of more immediate maltreatment experiences in the emergence of adolescent suicidal ideation and behaviors. However, the present study did not examine the role of maltreatment at more specific timeframes in childhood (e.g., infancy) in the prediction of internalizing and externalizing symptom trajectories and suicidal ideation and behaviors during adolescence. This is a possible direction for future research, as there is some evidence that maltreatment during different developmental stages can have specific effects on socioemotional outcomes (Dunn, McLaughlin, Slopen, Rosand, & Smoller, 2013; Manly et al., 2001). For example, it is possible that physical abuse or neglect that occurs in infancy, when the child is developing an attachment relationship with their primary caregiver, can have substantial negative effects on socioemotional development.
The results of this study should be considered in light of several limitations. First, there are limitations regarding the maltreatment measures that we utilized. Although we utilized an objective record-based measure of maltreatment, it is likely that not all cases of maltreatment were reported to Child Protective Services. Future studies should also utilize self-report measures of child maltreatment. Additionally, the majority of youth who experience maltreatment will experience multiple types of abuse and neglect (Warmingham, Handley, Rogosch, Manly, & Cicchetti, 2019). Thus, measuring subtypes of maltreatment independently may not accurately capture the experience of child maltreatment. Second, a four-class solution was chosen based on a number of theoretical and statistical criteria. However, some scholars have argued that class solutions in a growth mixture modeling framework are often arbitrary (Hoeksma & Kelderman, 2006). Additionally, the moderate-decreasing class consisted of a small subsample of youth (3.37% of our total sample), which may limit the generalizability of our findings. However, other studies have found similar four-class patterns of internalizing and externalizing symptomology in samples of youth and adolescents, increasing our confidence in the replicability of these results (Lauterbach & Armour, 2015; Wanner et al., 2012). Third, due to the nature of this study as a secondary data analysis, we were limited to utilizing the measures and time points that exist in the LONGSCAN dataset. For example, we utilized three items in which youth at the age-16 time point self-reported their suicide-related symptomology in the past year, which was predicted by symptom trajectories that ended at the age-14 time point. As suicide is often an acute crisis, it is possible that the predictors of suicide would be different if measured in a more proximal period. It would be ideal for future studies to use intensive longitudinal designs, such as daily diary methods, to consider the relation between comorbid psychopathology and suicidal ideation and behaviors in adolescence. Furthermore, the study would be strengthened by utilizing a more detailed inventory for youth to report on their suicidal ideation and behaviors. Additionally, we chose to focus on suicide-related outcomes at the age-16 time point, rather than the age-18 time point, due to the large amount of missing data at the latter time point. Future studies would be strengthened by considering the change in suicidal ideation and behaviors over time across adolescence, instead of at a single time point. Further, due to limitations of the dataset, we utilized parent-reported data on child internalizing and externalizing psychopathology. Youth reports of their psychopathology are typically considered to be more valid than parent-reported data (Waters, Stewart-Brown, & Fitzpatrick, 2003). Last, due to the longitudinal nature of the data set, there was much missing data on the suicide-related outcome measures. This may have limited the power of the growth mixture modeling analysis.
Despite these limitations, this study provides novel evidence regarding the developmental associations between child maltreatment and suicidal ideation and behaviors in adolescence. The LONGSCAN sample and study design are particularly well suited for our research objectives in the present study. First, the LONGSCAN study is longitudinal, containing data on both internalizing and externalizing problems from childhood to adolescence. Second, the sample includes maltreated youth and also nonmaltreated youth who are at risk for reasons other than maltreatment. This allows for the ability to disentangle the outcomes associated with child maltreatment versus other childhood adversities, such as poverty, which we controlled for in our analysis. Thirdly, the LONGSCAN sample includes data on maltreatment from Child Protective Services (CPS) records that were coded by trained researchers, which reduces the bias inherent in self-report measures of maltreatment. This detailed coding of CPS records allowed for the examination of different characteristics of child maltreatment, such as type and timing, and their influence on youth outcomes.
In sum, the present study provides evidence that heightened comorbid internalizing and externalizing symptomology may serve as a developmental pathway between child maltreatment and adolescent suicidal ideation and behaviors. These findings enhance the current research literature on the associations between adverse childhood experiences and suicidal ideation and behaviors and have implications for suicide prevention and clinical practice. In particular, adolescent suicide prevention efforts may benefit from targeting youth who exhibit comorbid internalizing and externalizing psychopathology. Additionally, the findings highlight the importance of primary prevention of child maltreatment, in order to avoid deleterious outcomes such as high levels of behavior problems and suicidal ideation and behaviors during adolescence.
Supplementary Material
Acknowledgments.
The data used in this publication were made available by the National Data Archive on Child Abuse and Neglect, Cornell University, Ithaca, NY, and they have been used with permission. Data from Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) Assessments 0-12 were originally collected by Desmond K. Runyan, Howard Dubowitz, Diana J. English, Jonathan Kotch, Alan Litrownik, Richard Thompson, and Terri Lewis & The LONGSCAN Investigator Group.
Financial Support. Funding for the project was provided by the Office on Child Abuse and Neglect (OCAN), Children’s Bureau, Administration for Children and Families, Department of Health and Human Services (The National Center on Child Abuse and Neglect [NCCAN]), under the Office of Human Services funded this consortium of studies during the early years of data collection from 04/01/1991 until NCCAN became part of OCAN in 1998. The collector of the original data, the funder, NDACAN, Cornell University and their agents or employees bear no responsibility for the analyses or interpretations presented here. Additional support for this work was provided through Award K01DA045219 (PI: Assaf Oshri) by the National Institute on Drug Abuse.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0954579419000919
In the three-class solution, 8.6% of the sample belonged to a class characterized by low and increasing internalizing symptoms (intercept = 8.58***, slope = −.99, quadratic slope = .71**) and moderate, increasing externalizing symptoms (intercept = 21.57***, slope = −3.67**, quadratic slope = 1.69***); 8.1% of the sample was characterized by moderate and stable internalizing symptoms (intercept = 17.57***, slope = 2.21**, quadratic slope = −.73*) and moderate, decreasing externalizing symptoms (intercept = 21.63***, slope = .33, quadratic slope = −.45); 83.3% of the sample was characterized by low stable internalizing symptoms (intercept = 5.01***, slope = .09, quadratic slope = .03) and low decreasing externalizing symptoms (intercept = 11.24***, slope = −1.00***, quadratic slope = .11).
References
- Achenbach TM (1991). Manual for Child Behavior Checklist/ 4–18 and 1991 Profile. Burlington, VT: University of Vermont, Dept. of Psychiatry. [Google Scholar]
- Arens AM, Gaher RM, & Simons JS (2012). Child maltreatment and deliberate self-harm among college students: Testing mediation and moderation models for impulsivity. American Journal of Orthopsychiatry, 82, 328–337. 10.1111/j.1939-0025.2012.01165.x [DOI] [PubMed] [Google Scholar]
- Barnett D, Manly JT, & Cicchetti D (1993). Defining child maltreatment: The interface between policy and research. Child Abuse, Child Development, and Social Policy, 8, 7–73. [Google Scholar]
- Bolger KE, & Patterson CJ (2001). Pathways from child maltreatment to internalizing problems: Perceptions of control as mediators and moderators. Development and Psychopathology, 13, 913–940. 10.1001/archgenpsychiatry.2011.1385.Common [DOI] [PubMed] [Google Scholar]
- Brezo J, Barker ED, Paris J, Hébert M, Vitaro F, Tremblay RE, & Turecki G (2008). Childhood trajectories of anxiousness and disruptiveness as predictors of suicide attempts. Archives of Pediatrics & Adolescent Medicine, 162, 1015–1021. 10.1001/archpedi.162.11.1015 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Banny A (2014). A Developmental Psychopathology Perspective on Child Maltreatment In Lewis M& Rudolph KD(Eds.), Handbook of Developmental Psychopathology (pp. 723–741). Boston, MA: Springer US; 10.1007/978-1-4614-9608-3_37 [DOI] [Google Scholar]
- Cicchetti D, & Rogosch F. a. (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70, 6–20. 10.1037/0022-006X.70.1.6 [DOI] [PubMed] [Google Scholar]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, & Maughan B (2007). Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect, 31, 211–229. [DOI] [PubMed] [Google Scholar]
- Coohey C, Dirks-Bihun A, Renner LM, & Baller R (2014). Strain, depressed mood and suicidal thoughts among maltreated adolescents in the United States. Child Abuse & Neglect, 38, 1171–9. 10.1016/j.chiabu.2014.04.008 [DOI] [PubMed] [Google Scholar]
- Cribbie RA (2007). Multiplicity control in structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal, 14, 98–112. 10.1080/10705510709336738 [DOI] [Google Scholar]
- Cummings EM, Schermerhorn AC, Davies PT, Goeke-Morey MC, & Cummings JS (2006). Interparental discord and child adjustment: Prospective investigations of emotional security as an explanatory mechanism. Child Development, 77132–152. 10.1111/j.1467-8624.2006.00861.x [DOI] [PubMed] [Google Scholar]
- Curtin SC, Warner M, & Hedegaard H (2016). Increase in suicide in the United States, 1999–2014. NCHS data brief , no. 241 Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Diemer MA, Mistry RS, Wadsworth ME, López I, & Reimers F (2013). Best practices in conceptualizing and measuring social class in psychological research. Analyses of Social Issues and Public Policy, 13(1), 77–113. 10.1111/asap.2013.13.issue-1 [DOI] [Google Scholar]
- Dunn EC, McLaughlin KA, Slopen N, Rosand J, & Smoller JW (2013). Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: Results from the national longitudinal study of adolescent health. Depression and Anxiety, 30, 955–964. 10.1002/da.22102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvir Y, Ford JD, Hill M, & Frazier JA (2014). Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harvard Review of Psychiatry, 22, 149–161. 10.1097/HRP.0000000000000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling: A Multidisciplinary Journal, 8, 430–457. 10.1207/s15328007sem0803_5 [DOI] [Google Scholar]
- English DJ, & LONGSCAN Investigators. (1997). Modified maltreatment classification system (MMCS). For More Information Visit the LONGSCAN Website at http://www.iprc.unc.edu/Longscan. [Google Scholar]
- English DJ, Upadhyaya MP, Litrownik AJ, Marshall JM, Runyan DK, Graham JC, & Dubowitz H (2005). Maltreatment’s wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse & Neglect, 29, 597–619. 10.1016/j.chiabu.2004.12.008 [DOI] [PubMed] [Google Scholar]
- Gomez SH, Tse J, Wang Y, Turner B, Millner AJ, Nock MK, & Dunn EC (2017). Are there sensitive periods when child maltreatment substantially elevates suicide risk? Results from a nationally representative sample of adolescents. Depression and Anxiety, 34, 734–741. 10.1002/da.22650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadland SE, Wood E, Dong H, Marshall BDL, Kerr T, Montaner JS, & DeBeck K (2015). Suicide attempts and childhood maltreatment among street youth: A prospective cohort study. Pediatrics, 136, 440–449. 10.1542/peds.2015-1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindley N (2006). Risk factors for recurrence of maltreatment: A systematic review. Archives of Disease in Childhood, 91, 744–752. 10.1136/adc.2005.085639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeksma JB, & Kelderman H (2006). On growth curves and mixture models. Infant and Child Development, 15, 627–634. [Google Scholar]
- Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, & Brook JS (2002). Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Arch Gen Psychiatry, 59, 741–749. 10.1001/archpsyc.59.8.741 [DOI] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Hawkins J, … Zaza S (2016). Youth Risk Behavior Surveillance United States, 2015. MMWR. Surveillance Summaries, 65, 1–174. 10.15585/mmwr.ss6506a1 [DOI] [PubMed] [Google Scholar]
- Kerr DCR, Reinke WM, & Eddy JM (2013). Trajectories of depressive symptoms and externalizing behaviors across adolescence: Associations with histories of suicide attempt and ideation in early adulthood. Suicide and Life-Threatening Behavior, 43, 50–66. 10.1111/j.1943-278X.2012.00127.x [DOI] [PubMed] [Google Scholar]
- Kim-Spoon J, Cicchetti D, & Rogosch FA (2013). A longitudinal study of emotion regulation, emotion lability-negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Development, 84, 512–527. 10.1111/j.1467-8624.2012.01857.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight ED, Smith JB, Martin L, Lewis T, & LONGSCAN Investigators. (1998). Measures for Assessment of Functioning and Outcomes in Longitudinal Research on Child Abuse Volume 3: Early Adolescence (Ages 12–14). Accessible at the LONGSCAN web site (http://www.iprc.unc.edu/longscan/).
- Lanza ST, Tan X, & Bray BC (2013). Latent class analysis with distal outcomes: A flexible model-based approach. Structural Equation Modeling: A Multidisciplinary Journal, 20, 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larrabee H, & Lewis T (2014). Longitudinal studies of child abuse and neglect (LONGSCAN) Assessments 0–18: User’s Guide. Ithaca, NY: National Data Archive on Child Abuse and Neglect, Cornell University. [Google Scholar]
- Lauterbach D, & Armour C (2015). Symptom trajectories among child survivors of maltreatment: Findings from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN). Journal of Abnormal Child Psychology, 44(2), 369–379. 10.1007/s10802-015-9998-6 [DOI] [PubMed] [Google Scholar]
- Li F, & Godinet MT (2014). The impact of repeated maltreatment on behavioral trajectories from early childhood to early adolescence. Children and Youth Services Review, 36, 22–29. 10.1016/j.childyouth.2013.10.014 [DOI] [Google Scholar]
- Luthar S, Cicchetti D, & Becker B (2000). The construct of resilience: A critial evaluation and guidelines for future work. Child Development, 71, 543–562. 10.1016/j.pestbp.2011.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology, 13, 759–782. [PubMed] [Google Scholar]
- Masten AS (2014). Ordinary magic: Resilience in development. New York, NY, US: Guilford Press. [Google Scholar]
- Miller AB, Adams LM, Esposito-Smythers C, Thompson R, & Proctor LJ (2014). Parents and friendships: A longitudinal examination of interpersonal mediators of the relationship between child maltreatment and suicidal ideation. Psychiatry Research, 220, 998–1006. 10.1016/j.psychres.2014.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, Esposito-Smythers C, Weismoore JT, & Renshaw KD (2013). The relation between child maltreatment and adolescent suicidal behavior: A systematic review and critical examination of the literature. Clinical Child and Family Psychology Review, 16, 146–72. 10.1007/s10567-013-0131-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R, Scott J, Alati R, O’Callaghan M, Najman JM, & Strathearn L (2013). Child maltreatment and adolescent mental health problems in a large birth cohort. Child Abuse & Neglect, 37, 292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran PB, Vuchinich S, & Hall NK (2004). Associations between types of maltreatment and substance use during adolescence. Child Abuse & Neglect, 28, 565–574. 10.1016/j.chiabu.2003.12.002 [DOI] [PubMed] [Google Scholar]
- Moylan CA, Herrenkohl TI, Sousa C, Tajima EA, Herrenkohl RC, & Russo MJ (2010). The effects of child abuse and exposure to domestic violence on adolescent internalizing and externalizing behavior problems. Journal of Family Violence, 25, 53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus User’s Guide (8th Ed.). LosAngeles, CA: Muthén & Muthén. [Google Scholar]
- O’Connor RC (2011). The integrated motivational-volitional model of suicidal behavior. Crisis, 32, 295–298. 10.1027/0227-5910/a000120 [DOI] [PubMed] [Google Scholar]
- Oshri A, Duprey EB, Kogan SM, Carlson MW, & Liu S (2018). Growth patterns of future orientation among maltreated youth: A prospective examination of the emergence of resilience. Developmental Psychology, 54(8), 1456–1471. 10.1037/dev0000528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Kogan SM, Kwon JA, Wickrama KAS, Vanderbroek L, Palmer AA, & Mackillop J (2018). Impulsivity as a mechanism linking child abuse and neglect with substance use in adolescence and adulthood. Development and Psychopathology, 30, 417–435. 10.1017/S0954579417000943 [DOI] [PubMed] [Google Scholar]
- Oshri A, Rogosch FA, Burnette ML, & Cicchetti D (2011). Developmental pathways to adolescent cannabis abuse and dependence: Child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychology of Addictive Behaviors, 25, 634–644. 10.1037/a0023151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Sutton TE, Clay-Warner J, & Miller JD (2015). Child maltreatment types and risk behaviors: Associations with attachment style and emotion regulation dimensions. Personality and Individual Differences, 73, 127–133. 10.1016/j.paid.2014.09.015 [DOI] [Google Scholar]
- Petrenko CLM, Friend A, Garrido EF, Taussig HN, & Culhane SE (2012). Does subtype matter? Assessing the effects of maltreatment on functioning in preadolescent youth in out-of-home care. Child Abuse and Neglect, 36, 633–644. 10.1016/j.chiabu.2012.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD (2008). Mechanisms linking early experience and the emergence of emotions: Illustrations from the study of maltreated children. Current Directions in Psychological Science, 17, 370–375. 10.1111/j.1467-8721.2008.00608.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor LJ, Skriner LC, Roesch S, & Litrownik AJ (2010). Trajectories of behavioral adjustment following early placement in foster care: Predicting stability and change over 8 years. Journal of the American Academy of Child & Adolescent Psychiatry, 49, 464–473. 10.1016/j.jaac.2010.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, & Cicchetti D (2010). From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology, 22, 883–897. 10.1017/S0954579410000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runyan DK, Curtis PA, Hunter WM, Black MM, Kotch JB, Bangdiwala S, … Landsverk J (1998). LONGSCAN: A consortium for longitudinal studies of maltreatment and the life course of children. Aggression and Violent Behavior, 3, 275–285. 10.1016/S13591789(96)00027-4 [DOI] [Google Scholar]
- Runyan D, Dubowitz H, English DJ, Kotch JB, Litrownik A, Thompson R, & The LONGSCAN Investigator Group (2014). Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) Assessments 0–18 [Dataset]. Available from National Data Archive on Child Abuse and Neglect Web site, http://www.ndacan.cornell.edu [Google Scholar]
- Rutter ML, Kreppner JM, & O’Connor TG (2001). Specificity and heterogeneity in children’s responses to profound institutional privation. British Journal of Psychiatry, 179, 97–103. 10.1192/bjp.179.2.97 [DOI] [PubMed] [Google Scholar]
- Rytilä-Manninen M, Haravuori H, Fröjd S, Marttunen M, & Lindberg N (2018). Mediators between adverse childhood experiences and suicidality. Child Abuse and Neglect, 77, 99–109. 10.1016/j.chiabu.2017.12.007 [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. 10.1037//1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Seltzer MH, Frank KA, & Byrk AS (1994). The metric matters: The sensitivity of conclusions about growth in student achievement to choice of metric. Educational Evaluation and Policy Analysis, 16, 41–49. [Google Scholar]
- Taussig HN, Harpin SB, & Maguire SA (2014). Suicidality among preadolescent maltreated children in foster care. Child Maltreatment, 19, 17–26. 10.1177/1077559514525503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R, English DJ, & White CR (2016). Maltreatment history as persistent risk: An extension of Li and Godinet (2014). Children and Youth Services Review, 64, 117–121. 10.1016/j.childyouth.2016.03.003 [DOI] [Google Scholar]
- US Department of Health & Human Services Administration for Children and Families Administration on Children Youth and Families Children’s Bureau. (2018). Child Maltreatment 2016. Retrieved from https://www.acf.hhs.gov/sites/default/files/cb/cm2016.pdf [Google Scholar]
- Verona E, Sachs-Ericsson N, & Joiner TE (2004). Suicide attempts associated with externalizing psychopathology in an epidemiological sample. American Journal of Psychiatry, 161, 444–451. 10.1176/appi.ajp.161.3.444 [DOI] [PubMed] [Google Scholar]
- Wanner B, Vitaro F, Tremblay RE, & Turecki G (2012). Childhood trajectories of anxiousness and disruptiveness explain the association between early-life adversity and attempted suicide. Psychological Medicine, 42, 2373–2382. 10.1017/S0033291712000438 [DOI] [PubMed] [Google Scholar]
- Warmingham JM, Handley ED, Rogosch FA, Manly JT, & Cicchetti D (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse & Neglect, 87, 28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters E, Stewart-Brown S, & Fitzpatrick R (2003). Agreement between adolescent self-report and parent reports of health and well-being: Results of an epidemiological study. Child: Care, Health and Development, 29, 501–509. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Lee TK, O’Neal CW, & Lorenz FO (2016). Multivariate applications series Higher-order growth curves and mixture modeling with Mplus: A practical guide. New York, NY, US: Routledge/Taylor & Francis Group; 10.4324/9781315642741 [DOI] [Google Scholar]
- Willner CJ, Gatzke-Kopp LM, & Bray BC (2016). The dynamics of internalizing and externalizing comorbidity across the early school years. Development and Psychopathology, 28, 1033–1052. 10.1017/S0954579416000687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson HW, Samuelson SL, Staudenmeyer AH, & Widom CS (2015). Trajectories of psychopathology and risky behaviors associated with childhood abuse and neglect in low-income urban African American girls. Child Abuse & Neglect, 45, 108–121. 10.1016/j.chiabu.2015.02.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


