A new viral severe acute respiratory syndrome coronarovirus 2 (SARS-CoV-2), was identified in the end of 2019 in China. Since then, the disease has expanded rapidly worldwide and the World Health Organization (WHO) has characterized the disease as coronavirus disease 2019 (COVID-19) and declared it as a pandemic on March 2020.1 Although the majority of COVID-19 patients are asymptomatic or paucisymptomatic, many patients can experience respiratory failure, and quickly progress to acute respiratory distress syndrome (ARDS) requiring advanced and rescue therapies.
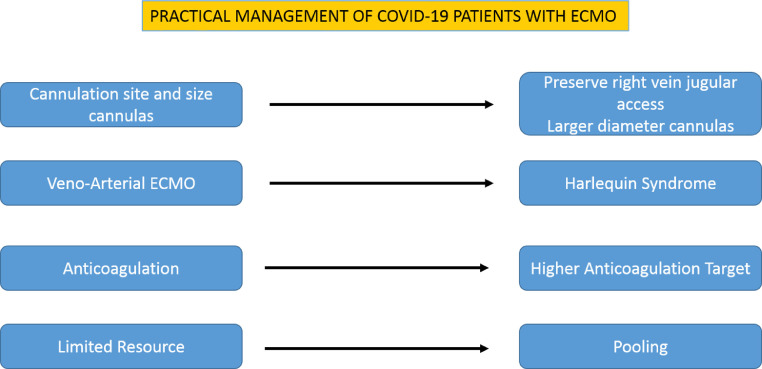
SARS-CoV-2 is associated with very high mortality and is related to the direct and indirect effects of disease and to the lack of effective therapies. The role of ExtraCorporeal Membrane Oxygenation (ECMO), as a rescue therapy in refractory hypoxemia during severe COVID-19, is currently not well defined, and only limited case series reporting a very high mortality rate are available.2 , 3 Results of the V-V ECMO therapy during influenza A (H1N1) and MERS outbreaks suggest that ECMO may be helpful in selected patients, so could it be in COVID-19 patients.4 , 5 Our experience is based on more of 50 COVID-19 patients treated with ECMO since March 2020 in our institution (Henri Mondor Hospital, a referral Ecmo center of the Paris network). Over more than 350 COVID-19 critically ill patients had managed in our ICU, we report some practical observations on the management of ECMO therapy in the severe COVID-19 cases (Fig. 1 ).
Fig. 1.
Schematic specific highlights of practical management of ECMO therapy in COVID-19 patients.
Technical considerations: cannulation site and size of cannulas
The V-V ECMO classic configuration with a double cannulation of the right internal jugular vein and the right femoral vein should be preferred; femoral-jugular configuration is the most efficient technique for respiratory support, especially in the most hypoxemic patients, and allows lower recirculation rate that femoro-femoral configuration. When the preferred cannulation is not possible, the alternative configurations of V-V ECMO support involve bilateral femoral cannulation or more rarely the use of left internal jugular vein.
So, at ICU admission, we recommend to preserve the right venous jugular access for further possible need for V-V ECMO, and to insert central venous catheter into the left internal jugular vein.
Oxygenation of the ECMO depends on the fraction of inspired oxygen (FiO2) in the gas mixture of oxygenator and principally on ECMO flow. So, V-V ECMO therapy requires a high flow rate approaching at least two thirds of patient's cardiac output, a condition that necessistates use of large cannulas. This concept is even more valid for COVID-19 patients, for whom ECMO indication is more driven by hypoxemia than hypercapnia. In addition, as obesity is a clear risk factor for severe COVID-19 pneumonia,6 and as obese patients have higher cardiac output, high flow rates are required. To ensure maximal flow and avoid hemolysis, large caliber drainage cannulas relative to the presumed needs of the patient, typically 25 to 29 French should be used. On the contrary, percutaneous double lumen bicaval cannula should be avoided for COVID-19 patients, as high blood flows cannot be achieved with this technique.
Veno-Arterial ECMO and Harlequin syndrome
In some patients with COVID-19, shock can be present, due to septic shock, cytokine storm, acute core pulmonale or specific cardiac failure with myocarditis, Tako-Tsubo syndrome or coronary thrombosis enhanced by inflammation.7 In case of cardiogenic shock, alone or associated with ARDS, veno-arterial (V-A) ECMO support can be required. Less frequently, patients treated initially with V-V ECMO for respiratory failure may subsequently develop cardiac failure, requiring secondary V-A ECMO support. For instance, in our experience, 7 patients were supported with an initial VA-ECMO: in 4 cases, the initial indication was refractory ARDS, but hypoxic cardiac arrest occurred at the moment of cannulation, in 2 cases the indication was a pulmonary embolism and in 1 case severe myocarditis. In 1 case the initial V-V ECMO was changed in veno-arterio-venous (V-AV) ECMO for a right ventricular failure. All patients who experienced hypoxic cardiac arrest and one patient with pulmonary embolism developed differential cyanosis with upper body hypoxemia and lower body hyperoxia, resulting in a Harlequin syndrome. This syndrome, also defined as north-south syndrome, is a well-known complication of peripheral V-A ECMO and in COVID-19 patients must be suspected and recognised at an early stage.
Anticoagulation levels
Observations converge toward procoagulant patterns characterized by hypercoagulability and high rate of arterial/venous thrombosis. d-dimer levels, indeed, are high in most COVID-19 patients and have been associated with worse prognosis.8 , 9 These considerations are well correlated with clinical practice with a high rate of renal-replacement catheters thrombosis, or with the observation that during cannulae insertion for ECMO implantation, clots form early in the tubbing. We revised our institutional protocols with higher targets of anticoagulation. Consequently, even though patients are already on therapeutic anticoagulant therapy, we suggest that a bolus with of 50 IU/kg unfractionated heparin should be administered, before cannulation. When a therapeutic anticoagulant therapy is not yet established, a double dose should be considered.
Anticoagulation monitoring during ECMO therapy is crucial to avoid thrombosis formation in the circuit, but at the same time to avoid haemorrhagic complications. In our experience, anti-Xa activity target should be increase to 0.5 and 0.7 IU/ml.
Perspectives
Due to the high virulence and severity of SARS-CoV-2, China, many conutries have to cope with the massive arrival of patients in ICU. The limited resources of ventilators is one of the most important resource challenge, but at the same time, the availability of ECMO devices and circuits is also a challenge in the ECMO expert centers. A pooling of resources and the coordination of the various centers at regional and local level is a crucial point in the management of patients requiring ECMO.10 This organization has allowed the distribution of resources in the expert ECMO centers, but also the coordinated mobilization of ECMO teams towards non-specialized hospitals and the transfer of patients to expert ECMO center.
Despite the immense challenge, physicians have to face in the Covid-19 pandemic setting, research on ECMO is paramount importance to identify patients who will benefit the most, and the optimal management. Results of on-going registries and interventional studies are urgently requested.
Declaration of Competing Interest
None
Acknowledgements
We wish to thank all anesthesiologist, intensive care physicians, cardiac surgeons and perfusionist team for your collaboration
References
- 1.World Health Organization (WHO). Coronavirus disease (COVID-19) outbreak (https://www.who.int). 2020.
- 2.Zeng Y., Cai Z., Xianyu Y., Yang B.X., Song T., Yan Q. Prognosis when using extracorporeal membrane oxygenation (ECMO) for critically ill COVID-19 patients in China: a retrospective case series. Crit Care. 2020 Apr 15;24(1):148. doi: 10.1186/s13054-020-2840-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henry B.M., Lippi G. Poor survival with extracorporeal membrane oxygenation in acute respiratory distress syndrome (ARDS) due to coronavirus disease 2019 (COVID-19): pooled analysis of early reports. J Crit Care. 2020 Apr 1;58:27–28. doi: 10.1016/j.jcrc.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alshahrani M.S., Sindi A., Alshamsi F. Extracorporeal membrane oxygenation for severe Middle East respiratory syndrome coronavirus. Ann Intensive Care. 2018;8:3. doi: 10.1186/s13613-017-0350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt M., Zogheib E., Rozé H., Repesse X., Lebreton G., Luyt C.E., Trouillet J.L., Bréchot N., Nieszkowska A., Dupont H., Ouattara A., Leprince P., Chastre J., Combes A. The PRESERVE mortality risk score and analysis of long-term outcomes afterextracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensiv Care Med. Oct 2013;39(10):1704–1713. doi: 10.1007/s00134-013-3037-2. 23907497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., Labreuche J., Mathieu D., Pattou F., Jourdain M., Lille Intensive Care COVID-19 and Obesity study group High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 2020 Apr 9 doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Long B., Brady W.J., Koyfman A., Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020 Apr 18 doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]; 32317203.
- 8.Ranucci M., Ballotta A., Di Dedda U., Bayshnikova E., Dei Poli M., Resta M., Falco M., Albano G., Menicanti L. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020 Apr 17 doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramanathan K., Antognini D., Combes A., Paden M., Zakhary B., Ogino M., MacLaren G., Brodie D., Shekar K. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30121-1. S2213-2600(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]