Abstract
Background
Hong Kong, a Special Administrative Region of China, recorded its first confirmed coronavirus disease 2019 (COVID-19) case on 23 January 2020. We reviewed the case epidemiology and the various public health measures implemented from January to May 2020.
Methods
The epidemiological and clinical characteristics of the cases recorded in different phases of the epidemic were described and compared, and the effectiveness of the public health measures implemented were reviewed using the changes in the daily number of confirmed cases and the interval from symptom onset to hospital admission.
Results
Between January and May 2020, 1084 confirmed COVID-19 cases were reported, about 70% of which had a history of travel during the incubation period. The case fatality ratio was 0.4%. The local epidemic progressed through four phases: (1) preparedness and imported infection from mainland China, (2) local transmission, (3) imported infection from overseas countries associated with local transmission, and (4) controlled imported infection with limited local transmission, with an eventual reduction of the daily case number and minimization of the onset-to-admission interval. Various public health measures, including enhanced surveillance, border control, and social distancing, were introduced in phases in response to the prevailing local and global situations.
Discussion
The overall containment strategy in Hong Kong led to a stabilization of the number of cases and the absence of a community-wide outbreak during the 4.5 m after the first case was reported. This strategy of containment might serve as an example for future planning of preparedness and response against novel infectious agents.
Keywords: COVID-19, Novel coronavirus, Public health intervention, Quarantine, Contact tracing, Enhanced surveillance, Hong Kong, SARS-CoV-2
Introduction
Hong Kong Special Administrative Region, with a population of 7.4 million, is a major financial and transport hub located at the southern coast of China and has intimate ties with mainland China and the rest of the world. Having experienced the severe acute respiratory syndrome (SARS) outbreak in 2003, Hong Kong closely monitored the situation of coronavirus disease 2019 (COVID-19) following the first report in Wuhan on 31 December 2019. In early January 2020, COVID-19 was included as a statutory notifiable disease. Following confirmation of the first COVID-19 case in Hong Kong on 23 January 2020, more than 1000 confirmed cases were reported in the ensuing 4 m.
Throughout the epidemic, Hong Kong adopted a containment strategy of early identification and isolation of cases, with tracing and quarantine for up to 14 d of every close contact. To enhance case detection, Hong Kong stepped up its surveillance and testing strategies at different time points, with additional community mitigation measures.
This study was performed to review the epidemiology of the confirmed COVID-19 cases reported from January to May 2020 and to assess the overall effectiveness of the various public health measures.
Methods
Case definition
A confirmed COVID-19 case was defined according to the case definition issued by the Centre for Health Protection (CHP), Department of Health (Centre for Health Protection, 2020). In brief, confirmation required the detection (e.g., by reverse transcription-polymerase chain reaction (RT-PCR)) of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in a clinical specimen.
Source of case information
For each confirmed case, relevant epidemiological and clinical data collected from CHP epidemiological investigations were extracted from the CHP electronic databases.
Case classification
Based on the presence of a history of travel during the incubation period (IP, defined as 14 d before symptom onset) and CHP epidemiological investigations, each confirmed case was classified as one of the following: (1) an imported case (travelled to a place with local COVID-19 transmission during the IP); (2) a linked local case (no history of travel during the IP, with source identified); (3) an unlinked local case (no history of travel during the IP, with no source identified); or (4) a possibly imported case (a history of travel during part of the IP).
Descriptive and analytical epidemiology
The epidemiological and clinical profiles of the confirmed cases were described and compared between different case classifications and phases of the epidemic, using appropriate statistical tests with Microsoft Excel 2013 and R version 3.6.0.
Assessment of the public health measures and their effectiveness
The evolution of the COVID-19 epidemic in Hong Kong was described using epidemic curves. The various major public health measures implemented by the government in response to the prevailing disease situation were reviewed (The Government of the Hong Kong, 2020). Their overall effectiveness was assessed by calculating the 7-day moving averages of the daily number of confirmed cases reported and the interval from symptom onset to hospital admission (onset-to-admission interval) (Ng et al., 2020). The latter gave an indication of the duration the case spent within the community while being infectious. For asymptomatic cases, the onset date was substituted by the date of collection of the first positive specimen. For imported cases, the date of arrival in Hong Kong was used if it was later than the onset date, so as to allow a realistic assessment of the public health interventions.
Results
Descriptive and analytical epidemiology (Table 1)
Table 1.
Epidemiological and clinical profiles of the 1084 confirmed COVID-19 cases reported in Hong Kong
| Imported case( n = 657) (%) |
Linked local case (n = 250) (%) |
Unlinked local case (n = 69) (%) |
Possibly imported case (n = 108) (%) |
Total(n = 1084) (%) | p-value | |
|---|---|---|---|---|---|---|
| Total | 657 (60.6%) | 250 (23.1%) | 69 (6.4%) | 108 (10%) | 1084 | |
| Age (years) | ||||||
| 0–14 | 29 (4.4%) | 9 (3.6%) | 0 (0%) | 1 (0.9%) | 39 (3.6%) | <0.00001a |
| 15–24 | 264 (40.2%) | 17 (6.8%) | 1 (1.4%) | 7 (6.5%) | 289 (26.7%) | |
| 25–44 | 181 (27.5%) | 122 (48.8%) | 35 (50.7%) | 57 (52.8%) | 395 (36.4%) | |
| 45–64 | 142 (21.6%) | 73 (29.2%) | 25 (36.2%) | 36 (33.3%) | 276 (25.5%) | |
| 65+ | 41 (6.2%) | 29 (11.6%) | 8 (11.6%) | 7 (6.5%) | 85 (7.8%) | |
| Sex | ||||||
| Male | 362 (55.1%) | 123 (49.2%) | 42 (60.9%) | 61 (56.5%) | 588 (54.2%) | 0.241a |
| Female | 295 (44.9%) | 127 (50.8%) | 27 (39.1%) | 47 (43.5%) | 496 (45.8%) | |
| Condition | ||||||
| Ever critical or serious/death | 21 (3.2%) | 14 (5.6%) | 16 (23.2%) | 2 (1.9%) | 53 (4.9%) | <0.00001a |
| Stable | 636 (96.8%) | 236 (94.4%) | 53 (76.8%) | 106 (98.1%) | 1031 (95.1%) | |
| Mode of case identification | ||||||
| Active notification by medical practitioners | 236 (35.9%) | 48 (19.2%) | 2 (2.9%) | 50 (46.3%) | 336 (31%) | <0.00001a |
| Contact tracing by CHP | 72 (11%) | 132 (52.8%) | 5 (7.2%) | 5 (4.6%) | 214 (19.7%) | |
| Enhanced laboratory surveillance in public hospitals | 6 (0.9%) | 15 (6%) | 21 (30.4%) | 7 (6.5%) | 49 (4.5%) | |
| Enhanced surveillance at emergency departments, GOPCs, and private sector | 71 (10.8%) | 55 (22%) | 41 (59.4%) | 41 (38%) | 208 (19.2%) | |
| Enhanced surveillance for returning travellers | 272 (41.4%) | 0 (0%) | 0 (0%) | 5 (4.6%) | 277 (25.6%) | |
| Average onset-to-admission interval (days) | 2.6 | 3.6 | 6.3 | 4.2 | 3.2 | <0.00001b |
| Average hospital length of stay for discharged cases (days) | 20.4 | 24.1 | 23.6 | 21.8 | 21.6 | 0.00006604b |
CHP, Centre for Health Protection; GOPC, general outpatient clinic.
Chi-square test.
Welch F-test.
Table 1
A total of 1084 confirmed cases were reported between January and May 2020, comprising 588 males and 496 females (male to female ratio, 1.19:1) who ranged in age from 40 d to 96 y (mean 37.5, median 35 y). The date of symptom onset was between 18 January and 26 May 2020. Among the 859 patients (79.2%) who reported symptoms, the five most common symptoms included cough (436, 50.8%), fever (428, 49.8%), sore throat (174, 20.3%), headache (98, 11.4%), and runny nose (97, 11.3%). The remaining 225 cases (20.8%) were asymptomatic, with the first asymptomatic case reported on 23 February 2020.
All cases were isolated in public hospitals. As at 31 May 2020, 1036 patients had been discharged, with an average length of stay of 21.6 d (range 1–94 d; median 20 d). Four deaths were reported (case fatality ratio, 0.4%): three male patients and one female patient died (age range 39–80 y), all of whom had underlying medical conditions such as diabetes or hypertension. Apart from the four fatal cases, 25 cases were ever in a critical condition and 24 cases were ever in a serious condition. Most of the cases remained in a stable condition (1031 cases).
All cases were confirmed by RT-PCR between 23 January and 31 May 2020. They were identified from active notification by medical practitioners of suspected cases fulfilling the CHP reporting criteria (n = 336, 31.0%), enhanced surveillance for returning travellers (n = 277, 25.6%), contact tracing of confirmed cases (n = 214, 19.7%), enhanced surveillance at emergency departments, general outpatient clinics (GOPCs), and in the private sector (n = 208, 19.2%), and enhanced laboratory surveillance of pneumonia cases in public hospitals (n = 49, 4.5%). The onset-to-admission interval ranged from zero to 43 d (mean 3.2 d, median 2 d). Overall, 657 were imported cases (60.6%), 250 were linked local cases (23.1%), 69 were unlinked local cases (6.4%), and 108 were possibly imported cases (10.0%). For imported and possibly imported cases, the five countries most commonly visited during the IP were the United Kingdom (n = 405), the United States (n = 88), France (n = 47), Pakistan (n = 37), and Switzerland (n = 36).
Five hundred and sixty-eight cases (52.4%) were implicated in a total of 149 epidemiologically linked clusters. The cluster size varied from two to 105 cases (median two cases). A majority involved household members and people who travelled together. Several big clusters occurred during social gatherings or settings where the participants shared food or drinks together without wearing masks.
There was no significant difference in sex distribution between the four case classification groups. Notably, more than 40% of imported cases were in the 15–24 y age group, which differed from the other three groups, in which cases in the 25–44 y and 45–64 y age groups predominated. About one-fourth of unlinked local cases had ever been in a critical or serious condition or died, which was higher than the rates in the other groups. Most imported cases were identified from enhanced surveillance of returning travellers and active notification by medical practitioners, while most unlinked local cases were identified from enhanced surveillance in hospitals, GOPCs, and the private sector. Over half of the linked local cases were identified through contact tracing by the CHP. Unlinked local cases had the longest average onset-to-admission interval (6.3 d), while imported cases had a shorter average length of hospital stay than local cases (20.4 and 21.8 d versus 24.1 and 23.6 d).
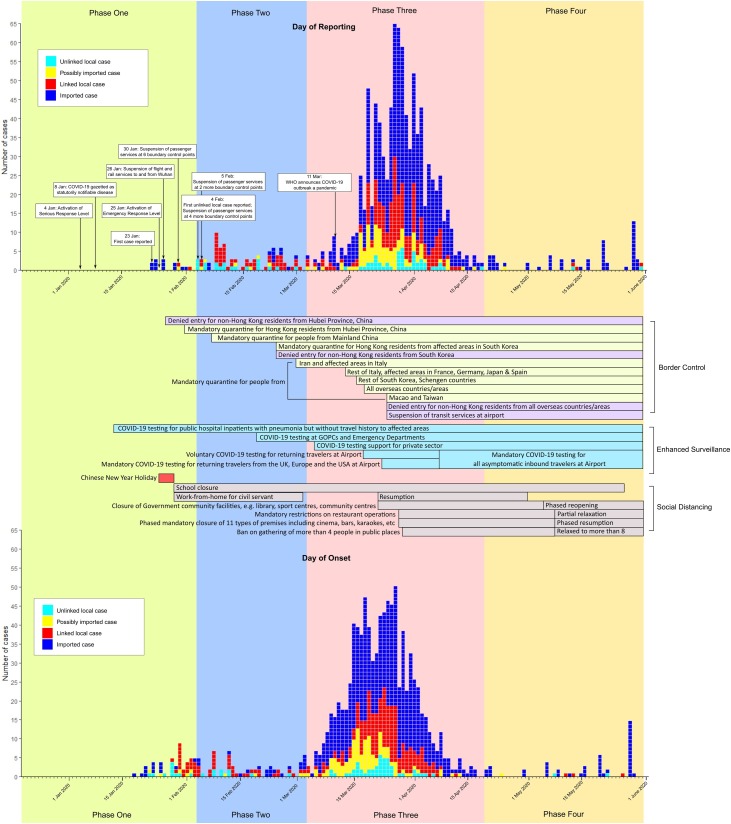
Phases of epidemic and public health measures (Figure 1 and Table 2)
Fig. 1.
Phases of the COVID-19 epidemic in Hong Kong and the corresponding public health measures by (a) date of reporting and (b) date of onset. [Au?1]
Table 2.
Key summary of cases by phases of the COVID-19 epidemic
| Phase one (31 Dec 2019 to 3 Feb 2020) |
Phase two(4 Feb to 3 Mar 2020) | Phase three(4 Mar to 19 Apr 2020) | Phase four(20 Apr to 31 May 2020) | Total | p-value | |
|---|---|---|---|---|---|---|
| Total | 15 (1.4%) | 85 (7.8%) | 925 (85.3%) | 59 (5.4%) | 1084 | |
| Case classification | ||||||
| Imported case | 12 (80%) | 11 (12.9%) | 581 (62.8%) | 53 (89.8%) | 657 (60.6%) | <0.00001a |
| Linked local case | 2 (13.3%) | 49 (57.6%) | 196 (21.2%) | 3 (5.1%) | 250 (23.1%) | |
| Unlinked local case | 0 (0%) | 19 (22.4%) | 48 (5.2%) | 2 (3.4%) | 69 (6.4%) | |
| Possibly imported case | 1 (6.7%) | 6 (7.1%) | 100 (10.8%) | 1 (1.7%) | 108 (10%) | |
| Mode of case identification | ||||||
| Active notification by medical practitioners | 10 (66.7%) | 0 (0%) | 322 (34.8%) | 4 (6.8%) | 336 (31%) | <0.00001a |
| Contact tracing by CHP | 3 (20%) | 49 (57.6%) | 157 (17%) | 5 (8.5%) | 214 (19.7%) | |
| Enhanced laboratory surveillance in public hospitals | 2 (13.3%) | 32 (37.6%) | 14 (1.5%) | 1 (1.7%) | 49 (4.5%) | |
| Enhanced surveillance at emergency departments, GOPCs, and private sector | 0 (0%) | 4 (4.7%) | 202 (21.8%) | 2 (3.4%) | 208 (19.2%) | |
| Enhanced surveillance for returning travellers | 0 (0%) | 0 (0%) | 230 (24.9%) | 47 (79.7%) | 277 (25.6%) | |
| Age (years) | ||||||
| 0–14 | 0 (0%) | 0 (0%) | 27 (2.9%) | 12 (20.3%) | 39 (3.6%) | <0.00001a |
| 15–24 | 0 (0%) | 6 (7.1%) | 274 (29.6%) | 9 (15.3%) | 289 (26.7%) | |
| 25–44 | 3 (20%) | 15 (17.6%) | 355 (38.4%) | 22 (37.3%) | 395 (36.4%) | |
| 45–64 | 6 (40%) | 36 (42.4%) | 223 (24.1%) | 11 (18.6%) | 276 (25.5%) | |
| 65+ | 6 (40%) | 28 (32.9%) | 46 (5%) | 5 (8.5%) | 85 (7.8%) | |
| Sex | ||||||
| Male | 9 (60%) | 40 (47.1%) | 502 (54.3%) | 37 (62.7%) | 588 (54.2%) | 0. 299a |
| Female | 6 (40%) | 45 (52.9%) | 423 (45.7%) | 22 (37.3%) | 496 (45.8%) | |
| Symptoms | ||||||
| Symptomatic | 15 (100%) | 80 (94.1%) | 744 (80.4%) | 20 (33.9%) | 859 (79.2%) | <0.00001a |
| Asymptomatic | 0 (0%) | 5 (5.9%) | 181 (19.6%) | 39 (66.1%) | 225 (20.8%) | |
| Average daily number of COVID-19 viral tests performed | 161 | 990 | 2283 | 2245 | 1556 | NA |
CHP, Centre for Health Protection; GOPC, general outpatient clinic; NA, not applicable.
Chi-square test
Fig. 1
Table 2
The epidemic in Hong Kong progressed through four phases, from preparedness and imported infection from mainland China, to local transmission, to imported infection from overseas countries associated with local transmission, to finally controlled imported infection with limited local transmission. The overall shape of the epidemic curve was characterized by a stable number of cases reported during the first two phases, followed by a surge in phase three and then an eventual drop in case numbers during phase four.
Phase one—preparedness and imported infection from mainland China (31 December 2019 to 3 February 2020)
Global and local case epidemiology
Cases reported during this phase were largely confined to mainland China, especially Wuhan. On 23 January 2020, Hong Kong recorded the first case who was a traveller from Wuhan intercepted at the border. Overall, 15 cases were reported in this phase, with 14 having a history of travel to mainland China (11 were from Wuhan) and one being linked to an imported case from Wuhan.
Enhanced surveillance and testing
The reporting criteria were updated from time to time based on the concurrent knowledge on COVID-19 and the evolving global situation. The clinical criteria that required the presence of both fever and respiratory symptoms were revised on 23 January 2020 to either one of the symptoms, upon the finding of afebrile presentations in a number of cases. The epidemiological criteria, at first only including a history of travel to Wuhan, were later extended to cover the entire Hubei Province.
To detect cases without a history of travel to an affected area, COVID-19 testing for all inpatients admitted to public hospitals with pneumonia without a travel history was introduced on 13 January 2020.
Border control measures
Enhanced border control measures, including surveillance targeting inbound travellers from affected areas, the suspension of passenger services at boundary control points, entry restriction, and mandatory 14-day quarantine for arriving passengers were implemented to limit the population flow to and from affected areas, initially including Wuhan and later the whole of Hubei Province.
Social distancing measures
Various social distancing measures were also promulgated by the government to reduce interpersonal contact in the community, including school suspension, cancellation of large-scale social events, and work-from-home arrangements for civil servants.
Phase two—local transmission (4 February to 3 March 2020)
Global and local case epidemiology
Meanwhile, multiple provinces in mainland China were reporting a marked increase in cases. Starting in mid-February, increases in cases were also reported globally with massive local transmission in some countries including South Korea (Korean Society of Infectious Diseases et al., 2020), Italy (Remuzzi and Remuzzi, 2020), and Iran (National Committee on COVID-19 Epidemiology, 2020).
In Hong Kong, the first unlinked local case was confirmed on 4 February, signifying entry into the next phase of the epidemic. The daily number of reported cases in this phase was between zero and 10. More than half of the cases recorded were linked local cases identified through contact tracing, with most of them belonging to clusters associated with social or religious gatherings around the Chinese New Year holidays at the end of January. Epidemiological investigations revealed that the transmission probably occurred during gatherings when the sources were pre-symptomatic or asymptomatic. Of note, the largest cluster involved nine attendees and three workers at a Buddhist temple, with further spread to seven of their close contacts. The source was suspected to be an asymptomatic carrier who had previously travelled to mainland China.
Of the imported cases, only two had a history of travel to mainland China, while the rest (nine cases) were evacuees from the Diamond Princess cruise ship, on which a massive COVID-19 outbreak occurred (Nakazawa et al., 2020).
Enhanced surveillance and testing
The reporting criteria were further revised to include a history of travel to all areas with active community transmission.
It was also noted that some cases had consulted their primary care physicians prior to admission but were not tested for COVID-19. They in general had a longer onset-to-admission interval. To increase the testing coverage and availability of testing in outpatient settings for early case detection, free COVID-19 testing was made available in GOPCs, emergency departments, and later in private medical practices. The laboratory capacity was also expanded to accommodate the increasing demand. To improve case ascertainment among asymptomatic close contacts, COVID-19 testing was also provided for them before the end of their 14-day quarantine period.
Border control measures
In response to the global situation, border control measures already in place, including mandatory quarantine, were extended to cover additional countries and areas with large-scale outbreaks. Certain groups of people, for example flight crews and cross-border truck drivers operating between mainland China and Hong Kong, were exempted from the mandatory quarantine arrangement and put under medical surveillance.
Phase three—imported infection from overseas countries associated with local transmission (4 March to 19 April 2020)
Global and local case epidemiology
While the number of cases reported in mainland China started decreasing in mid-February, large-scale outbreaks with active community transmission were occurring in many overseas countries such as the United Kingdom, the United States, France, Spain, Japan, and Germany.
Locally, the first imported case with a history of travel outside mainland China was reported on 4 March, signifying the start of another phase. A new wave of imported cases followed, first involving returning travellers of tour groups and then returnees from overseas countries, particularly students (245 cases) from the United Kingdom and the United States. In addition, there was also an increase in local cases from several large clusters involving bars, karaoke clubs, and social gatherings. The largest cluster involved 42 staff members and 30 visitors to four pubs, with four generations of transmission, affecting 103 people in total.
Together, these brought about an upsurge of cases starting in early March, reaching the peak of 65 cases reported in one day on 27 March. Subsequently, the number of reported cases gradually decreased, with the last unlinked local case in this phase being reported on 19 April.
Enhanced surveillance and testing
To allow earlier identification and isolation of imported cases, a free COVID-19 testing service was provided for returning travellers at the airport, which was first on a voluntary basis and later became compulsory. This ‘test and hold’ arrangement required them to wait at a holding centre for the test results.
The overall effort of enhanced surveillance is exemplified by the fact that it identified nearly half of the cases reported in this phase and the vastly increased number of COVID-19 tests performed daily, from 161 in phase one to 2283 in phase three.
Border control measures
The worsening global situation led to additional border control measures, including the extension of the compulsory home quarantine requirement to returnees from all overseas countries, denial of entry for non-Hong Kong residents from overseas countries, and the suspension of transit services at the airport.
Social distancing measures
The occurrence of multiple local clusters involving bars and social gatherings called for intensification of social distancing measures. Apart from the closure of additional governmental community venues, the government also introduced regulations mandating the closure of 11 types of premises including cinemas, fitness centres, karaoke clubs, and bars. A ban on gatherings of more than four people in a public place was also imposed. In addition, legal restrictions on restaurant operations were introduced to limit the mixing of patrons, with enhanced infection control measures such as temperature screening.
Phase four—controlled imported infection with limited local transmission (20 April to 31 May 2020)
Global and local case epidemiology
While the epidemic continued globally, the daily number of cases reported in Hong Kong returned to a low level during this phase, with some days reporting zero cases. Nearly 90% of cases were imported, with more than 60% being returnees from Pakistan.
Two sporadic local family clusters involving five cases without any history of travel during the IP were identified during this phase. For each cluster, extensive contact tracing and source finding were conducted. This included the use of deep throat saliva testing for all tenants in the same residential building and social and workplace contacts. The sources of both clusters could not be identified, implying the presence of low-level local transmission in the community.
Enhanced surveillance and testing
Additional measures were implemented to increase the coverage of COVID-19 testing. Private medical practitioners could directly request COVID-19 testing from the CHP laboratory and the number of specimen collection points was doubled. Workers at the airport and staff working in homes for the elderly or disabled were offered free COVID-19 testing. A majority of imported cases were identified through the ‘test and hold’ arrangement at the airport, which prevented their transmission to the community.
Border control measures
While the existing border control measures were continued, exemptions to the mandatory quarantine requirements were extended to cover additional groups of individuals with the need to travel between mainland China and Hong Kong, e.g., business owners and legal practitioners.
Social distancing measures
A number of social distancing measures were relaxed in view of the local situation. Starting from 8 May, premises previously mandated for closure were allowed to reopen in phases. Classes were resumed on 27 May. The number of persons allowed in group gatherings in public places was relaxed from four to eight, with exemptions given to religious gatherings.
Effectiveness of public health measures
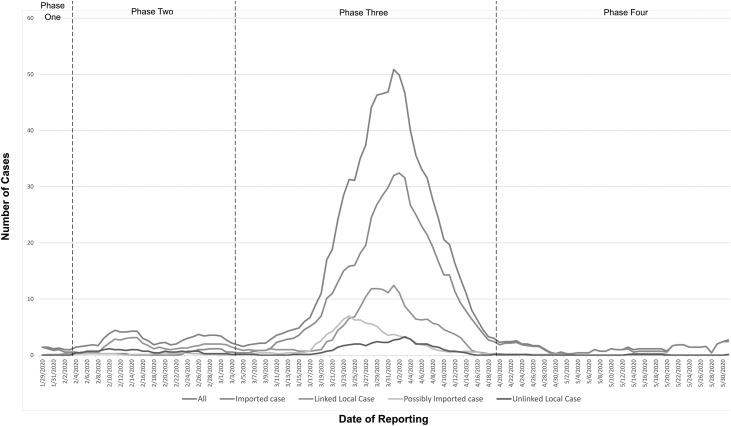
Number of cases reported (Figure 2)
Fig. 2.
Seven-day moving average of the daily number of reported cases. [Au?2]
The total number of cases reported remained at a low level throughout phase one and two. There was a small increase of linked local cases during phase two, corresponding to the local clusters associated with gatherings during the Chinese New Year holidays and an outbreak related to a Buddhist temple.
There was a surge in reported cases from the beginning of phase three. Although the main drivers of this surge were imported and possibly imported cases from overseas returnees, a marked increase in linked local cases was observed from the several large local clusters involving bars, karaoke clubs, and social gatherings. An increase in unlinked local cases was also observed, although on a smaller scale. After reaching the peak around early April, the number of cases across different case classifications experienced a gradual decrease towards phase four and remained at a low level comparable to that of phases one and two.
Interval from symptom onset to hospital admission (Figure 3)
Fig. 3.
Seven-day moving average of the onset-to-admission interval (in days) for all confirmed cases. [Au?2]
The duration of the interval from symptom onset to hospital admission showed some fluctuation from phase one, followed by a decrease towards the end of the phase two. At the start of phase three, an increase in the duration was again observed, followed by a continuous decrease in the interval towards phase four. The duration experienced some fluctuation in the later part of phase four, with the rises being attributed to the two unlinked local cases who, after symptom onset, had spent several days in the community before admission.
Discussion
Confirmed COVID-19 cases in Hong Kong had a different demographic profile compared with the global patient population reported by the World Health Organization (WHO) (World Health Organization, 2020c). In general, Hong Kong cases had a slightly higher male to female ratio (1.19:1 versus 1.03:1) and were younger (more than two-third of cases were below 45 y of age). The latter could be explained by the high proportion of imported cases being students returning from overseas.
Notably, the case cohort was characterized by a much lower case fatality ratio (0.4%) than those reported globally during the same period (6.1%) (World Health Organization, 2020d). Multiple factors, including younger case population, a robust public healthcare system, and earlier diagnosis through a high laboratory testing rate, might have contributed to this phenomenon.
In other overseas countries, the first wave of COVID-19 case importation was usually followed by widespread community transmission (Cohen and Kupferschmidt, 2020). Given its high population density and intimate connections to mainland China and the rest of the world, Hong Kong was highly vulnerable to a community-wide outbreak following importations from the start. However, a different pattern of a contained COVID-19 epidemic, characterized by a high proportion of imported cases with the absence of community-wide transmission, instead emerged.
While several studies in China and Italy have identified the positive impact of public health interventions such as lockdown and social distancing in curtailing community-wide outbreaks (Lau et al., 2020, Ji et al., 2020, Signorelli et al., 2020, Gregori et al., 2020), the present study findings suggest that the timely implementation of public health measures in response to the prevailing situations was able to establish this pattern of containment, without resorting to extreme measures such as city-wide lockdown or stay-at-home regulations. In phase one, the preparatory work for the looming epidemic laid the legal framework and logistical groundwork for the subsequent public health actions. Although travel restrictions had not been recommended by the WHO (World Health Organization, 2020e), our findings suggest that the border control measures, consisting of entry restriction and mandatory quarantine, were able to limit the number of cases imported from affected areas.
In phase two, the CHP epidemiological investigation of local cases allowed prompt identification and quarantine of contacts, some of whom eventually became cases. This, coupled with the social distancing measures, might have prevented further community spread. Despite the occurrence of several Chinese New Year-associated local clusters, the number of cases reported remained stable.
The influx of imported cases in phase three placed additional pressure on the healthcare system and resulted in an increase in the onset-to-admission interval. Nevertheless, the additional border control and enhanced surveillance measures were able to detect a large proportion of cases imported from overseas and minimized the time they spent in the community while being infectious. The several local clusters associated with bars and social gatherings were quickly contained through CHP contact tracing and only resulted in transient and limited community spread. Following the mandatory social distancing measures, no additional social gathering-associated local clusters were identified. The resultant decrease in cases was associated with a reduction in the overall onset-to-admission interval.
In phase four, the limitation of local transmission allowed the relaxation of several social distancing measures. Meanwhile, the continuation of border control measures remained necessary given the ongoing global transmission of COVID-19. Nevertheless, as the epidemic in mainland China was under control and given its close economic and social ties with Hong Kong, the mandatory quarantine requirement was relaxed for certain groups of travellers between the two localities through exemptions.
There are several limitations regarding this study. As a descriptive study, causal relationships between the public health measures and the epidemic trend could not be established. In addition, the contribution of the effect of individual measures could not be assessed.
Some cases might not have been captured by the surveillance system due to under-diagnosis of mild cases and asymptomatic individuals who never presented to the healthcare system. It is likely that asymptomatic cases with silent transmission existed before the first reporting on 22 February 2020 and these might have played a role in the transmission chain involving unlinked local cases.
Lastly, community participation and cooperation also played an important role in the successful containment of the epidemic in Hong Kong. There was already a high level of disease awareness in the community in phase one. Many private organizations adopted work-from-home arrangements and announced the postponement of public events and shutdown of venues like theme parks.
The absence of community-wide transmission might also be explained by the high prevalence of voluntary facemask-wearing in the community, which was almost universal according to a local survey (Cowling et al., 2020). We noted that all the large local clusters involved occasions where mask-wearing was either not practised or practicable, for example during meal gatherings. Although universal community mask-wearing was not unanimously recommended by the WHO (World Health Organization, 2020f) and other health authorities, our experience in Hong Kong suggested that it might limit disease transmission, especially when coupled with other public health interventions, such as personal and environmental hygiene measures (Chan and Yuen, 2020). Further studies on the effectiveness of universal masking during a pandemic are warranted.
To maintain the current success of containment amid an ever-evolving global COVID-19 pandemic, a balance will need to be struck between the protection of health and minimization of economic and social disruption. All public health measures should be evaluated continuously against the prevailing local and global situations.
Overall, the combination of public health measures taken in Hong Kong were associated with a stabilization of case numbers and absence of a community-wide COVID-19 outbreak during the 4.5 m following the reporting of the first case. The strategy of containment might serve as an example for future planning of preparedness and response against novel infectious agents.
Declarations
Funding source: This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
Approval was not required.
Conflict of interest
The authors have no conflicts of interest to disclose.
Acknowledgements
The authors would like to thank the staff members of the Centre for Health Protection for their wholehearted dedication and valuable contributions to the outbreak investigation and control of COVID-19, as well as colleagues at the Hospital Authorityfor their professional care of COVID-19 patients.
References
- Centre for Health Protection, Department of Health, Hong Kong Special Administrative Region. Communicable disease surveillance case definitions. https://cdis.chp.gov.hk/CDIS_CENO_ONLINE/ceno.html. (accessed May 1, 2020).
- Chan K.H., Yuen K.Y. COVID-19 epidemic: disentangling the re-emerging controversy about medical facemasks from an epidemiological perspective. Int J Epidemiol. 2020 doi: 10.1093/ije/dyaa044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Kupferschmidt K. Countries test tactics in’ war’ against COVID-19. Science. 2020;367(6484):1287–1288. doi: 10.1126/science.367.6484.1287. [DOI] [PubMed] [Google Scholar]
- Cowling B.J., Ali S.T., Ng T.W.Y., Tsang T.K., Li J.C.M., Fong M.W. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in hong kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. Epub 2020 Apr 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregori D., Azzolina D., Lanera C., Prosepe I., Destro N., Lorenzoni G. A first estimation of the impact of public health actions against COVID-19 in Veneto (Italy) J Epidemiol Community Health. 2020 doi: 10.1136/jech-2020-214209. pii: jech-2020-214209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji T., Chen H.L., Xu J., Wu L.N., Li J.J., Chen K. Lockdown contained the spread of 2019 novel coronavirus disease in Huangshi city, China: Early epidemiological findings. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa390. pii: ciaa390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korean Society of Infectious Diseases, Korean Society of Pediatric Infectious Diseases, Korean Society of Epidemiology, Korean Society for Antimicrobial Therapy, Korean Society for Healthcare-associated Infection Control and Prevention, Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020; 35(10): e112. [DOI] [PMC free article] [PubMed]
- Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Schubert J., Bania J. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020 doi: 10.1093/jtm/taaa037. pii: taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakazawa E., Ino H., Akabayashi A. Chronology of COVID-19 cases on the diamond princess cruise ship and ethical considerations: a report from Japan. Disaster Med Public Health Prep. 2020;24:1–8. doi: 10.1017/dmp.2020.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Committee on COVID-19 Epidemiology, Ministry of Health and Medical Education, IR Iran. Daily situation report on coronavirus disease (COVID-19) in Iran; March 23, 2020. Arch Acad Emerg Med. 2020; 8(1):e36. [PMC free article] [PubMed]
- Ng Y., Li Z., Chua Y.X., Chaw W.L., Zhao Z., Er B. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore - January 2-February 29, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(11):307–311. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. Epub 2020 Mar 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorelli C., Scognamiglio T., Odone A. COVID-19 in Italy: impact of containment measures and prevalence estimates of infection in the general population. Acta Biomed. 2020;91(3–S):175–179. doi: 10.23750/abm.v91i3-S.9511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Government of the Hong Kong Special Administrative Region. HKSAR Government Press Releases. https://www.info.gov.hk/gia/ISD_public_Calendar_en.html. (accessed May 1, 2020).
- World Health Organization. disease 2019 (COVID-19) Situation Report – 89. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200418-sitrep-89-covid-19.pdf (accessed May 1, 2020).
- World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report – 133. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200601-covid-19-sitrep-133.pdf (accessed June 10, 2020).
- World Health Organization. Updated WHO recommendations for international traffic in relation to COVID-19 outbreak. 29 February 2020. https://www.who.int/news-room/articles-detail/updated-who-recommendations-for-international-traffic-in-relation-to-covid-19-outbreak (accessed May 1, 2020).
- World Health Organization. Advice on the use of masks in the context of COVID-19. https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed June 11, 2020).