Dear Editor,
A recent study in this journal reported the environmental contamination of severe acute respiratory syndrome 2 (SARS-CoV-2) in healthcare premises.1 Indeed, the health care workers (HCW) are highly exposed to SARS-CoV-2 infection and several recommendations have been made to protect them.2, 3, 4 Here, we aimed to describe characteristics of HCW infected with SARS-CoV-2 and the spectrum of initial symptoms in order to identity new cases as early as possible.
This longitudinal study included all HCW managed by the occupational health department of the Pitié-Salpêtrière University Hospital, Paris, France, for suspected infection with SARS-CoV-2 from March 13th to April 3rd, 2020. Included participants were symptomatic and tested Positive for SARS-CoV-2 RNA by RT-PCR in nasopharyngeal specimens. The following characteristics were recorded by physicians of the occupational health department: age, profession described as medical HCW (physicians and pharmacists), non-medical HCW (nurses, assistant-nurses, psychologist, physiotherapist, laboratory technician) and others (personal from administrative, maintenance and restoration services), department of work described as clinical (including medicine, surgical and intensive care unit [ICU]) and non-clinical (including laboratory, pharmacy, administrative, maintenance and restoration) departments, days since onset of symptoms and clinical features.
Continuous variables were expressed as the median and interquartile range [IQR] and discrete variables were expressed as numbers and percentages. Non-parametric Wilcoxon test was used to compare between-group differences and a logistic regression investigated potential prognostic factors of the presence of 3 or more symptoms.
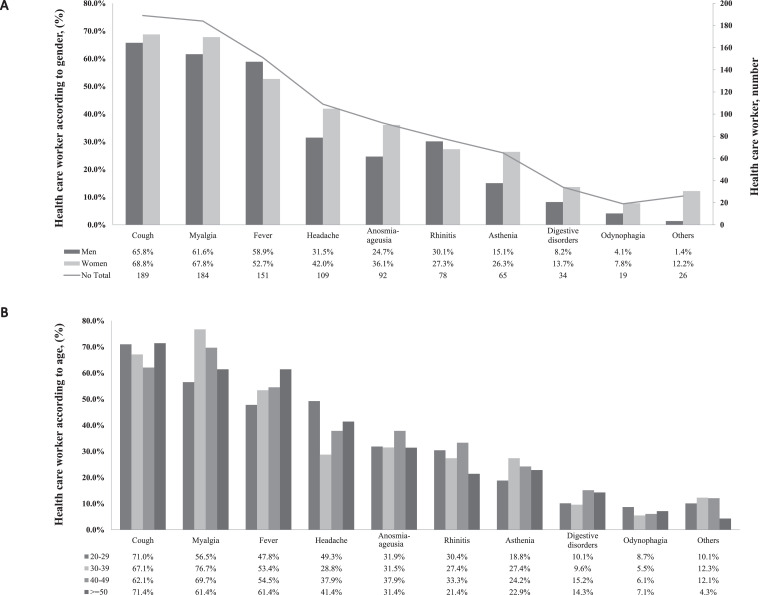
During the inclusion period, 310 HCW were tested positive for SARS-CoV-2 infection and 278 were included in this study. Median [IQR] age was 39 [30–50] years and 74% (n = 205) were women. The majority was non-medical HCW (n = 185, 67%), including 75 (27%) nurses and 70 (25%) assistant nurses. Most of HCW (n = 226, 82%) performed direct medical care in medicine (n = 137), surgical (n = 57), and ICU (n = 32) departments; the remainder included HCW from laboratory, pharmacy, administrative, maintenance and restoration services. Participants reported in median 3 [2–4] different symptoms and a median of 2 [1–4] days between the onset of symptoms and consultation (Table 1 ). The most common initial symptoms were cough (n = 189, 68%), myalgia (n = 184, 66%) and fever (n = 151, 54%) and overall, 90% (n = 251) reported at least one of the aforementioned symptoms. Headache, anosmia/ageusia and digestive disorders were found in 39%, 33% and 12% of cases, respectively (Fig. 1 A). Twenty (7%) patients reported dyspnea, of which a majority of women (n = 19). None had a severe form of coronavirus disease 2019 (Covid-19).
Table 1.
Characteristics of the 278 symptomatic health care workers tested positive for SARS-CoV-2 infection in the Pitié-Salpêtrière University Hospital from March 13th to April 3rd, 2020, according to gender and department.
| Total n = 278 |
Men n = 73 |
Women n = 205 |
p | Clinical HCW n = 226 |
Non-clinical HCW n = 51 |
p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | N | N | value | N | N | value | ||||||
| Age, n, median [IQR] | 278 | 39 [30–50] | 73 | 41 [30–52] | 205 | 38 [29–48] | 0.21 | 226 | 37 [29–48] | 51 | 46 [36–53] | 0.0001 |
| Gender, n (%) | 278 | 73 | 205 | 226 | 51 | |||||||
| Men | 73 (26) | 73 (100) | 0 (0) | – | 53 (24) | 20 (39) | 0.033 | |||||
| Women | 205 (74) | 0 (0) | 205 (100) | 173 (76) | 31 (61) | |||||||
| Health care worker, n (%)* | 277 | 73 | 204 | 226 | 51 | < 0.0001 | ||||||
| Medical | 52 (19) | 20 (27) | 32 (16) | 0.0002 | 40 (18) | 12 (24) | ||||||
| Non-medical | 179 (65) | 34 (47) | 145 (71) | 161 (71) | 18 (35) | |||||||
| Medical student | 17 (6) | 6 (8) | 11 (5) | 15 (7) | 2 (4) | |||||||
| Non-medical student | 6 (2) | 0 (0) | 6 (3) | 6 (3) | 0 (0) | |||||||
| Others | 23 (8) | 13 (18) | 10 (5) | 4 (1) | 19 (37) | |||||||
| Health care department, n (%)⁎⁎ | 277 | 73 | 204 | 225 | 51 | – | ||||||
| Clinical | 226 (82) | 53 (73) | 173 (85) | 0.03 | 226 (100) | 0 (0) | ||||||
| Non-clinical | 51 (18) | 20 (27) | 31 (15) | 0 (0) | 51 (100) | |||||||
| Symptoms, median [IQR] | 278 | 3 [2–4] | 73 | 3 [2–4] | 205 | 3 [3–4] | 0.0026 | 226 | 3 [3–4] | 51 | 3 [2–5] | 0.67 |
| Days between onset of symptoms and consultation, median [IQR] | 256 | 2 [1–4] | 68 | 2 [1–4] | 188 | 3 [1–4] | 0.088 | 209 | 2 [1–4] | 46 | 3 [2–4] | 0.35 |
n: number; IQR: interquartile; HCW: Health care worker; ICU: intensive care unit; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2.
medical HCW includes physicians and pharmacists, non-medical HCW includes nurses, assistant-nurses, psychologist, physiotherapist, laboratory technician and others HCW includes personal from administrative, maintenance and restoration services.
clinical departments include medicine, surgical and intensive care unit and non-clinical departments include laboratory, pharmacy, administrative, maintenance and restoration departments.
Fig. 1.
Prevalence of symptoms in health care workers diagnosed with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Pitié-Salpêtrière University Hospital, according to sex (A) or age (B). A. Each symptom is represented in the x-axis, the prevalence of each one according to gender are represented on the left y-axis (percentage) and the total number of health care worker with each symptom on the right y-axis (number). B. Each symptom is presented in the x-axis and the prevalence of each one according to age category on the left y-axis (percentage). Others included dyspnea (n = 20), chest pain (n = 4), conjunctivitis (n = 2), and neck pain (n = 1) One patient presented both dyspnea and chest pain.
The mean number of symptoms was higher in women (3.6 versus 3.0, p = 0.003) and they tended to consult occupational medicine later than men (3.2 versus 2.6, p = 0.09). No differences in term of symptoms number or delay to consultation were found between age categories or HCW department (Supplementary Table 1 and Table 1). By regression logistic analysis, only gender was associated with the number of symptoms and women had a higher risk of having 3 or more symptoms compared to men (OR= 1.86 [1.03–3.3]; p = 0.04).
By increasing age categories order, 88%, 90%, 89% and 93% of the participants reported at least one of the following symptoms: cough, myalgia or fever, as well as 90% of men and 90% of women. These symptoms were the most prevalent excepted for the “20–29 years” category, in which 49% reported headache, before fever (Fig. 1B). According to the department, cough, myalgia, and fever were also the most prevalent symptoms and 92% and 84% of cases reported at least one of these symptoms in clinical and non-clinical department, respectively (Supplementary Table 2). Fever was associated with a shorter delay between onset of symptoms and consultation (fever: 2.0 [1.0–3.0] days versus no fever: 3.0 [2.0–5.0] days, p =< 0.0001) whereas anosmia-ageusia and asthenia were associated with a longer delay before consultation (anosmia-ageusia: 3.0 [2.0–6.0] days versus no anosmia-ageusia: 2.0 [1.0–3.0] days, p < 0.0001, and asthenia: 3.0 [2.0–4.0] days versus no asthenia: 2.0 [1.0–4.0] days, p = 0.04).
We reported for the first time the characteristics of HCW working in a French University Hospital with laboratory-confirmed SARS-CoV-2 infection. Although only symptomatic participants were tested, the majority of infected HCW were working in clinical department. This may be expected as they are more exposed to the risk of SARS-CoV-2 transmission by direct contact with patients experiencing Covid-19 but also by applying respiratory devices or collecting respiratory samples.2 , 4 Indeed, although results of Ye and al are limited to SARS-CoV-2 RNA detection, they reported higher level of SARS-CoV-2 contamination in Covid-19 departments. They also reported that the most contaminated zones were in ICU taking care of Covid-19 patients whereas we evidenced that HCW from medicine were the most infected followed by surgical and ICU units. Different explanations can be put forward for these discrepancies. In the present study, we have not distinguished Covid-19 from Covid-19 free departments and medicine units are the largest units in our hospital. As reported by Ye and al, the prevalence of contaminated objects as desktop/keyboard and doorknob is about 15% in hospital, thus contaminated hand and surfaces by HCW, patients and visitors could potentially lead to SARS-CoV-2 exposure even in Covid-19 free departments; the transition to a focused care of Covid-19 patients was quick and thus HCW from department not designated as Covid-19 specifics unit may receive less infection prevention training. Overall, as the global delay during the onset of symptoms and consultation was 2 days, it is essential to reinforce barrier gestures, such as masks, especially since the majority of infected HCW are in direct contact with patients but also because transmission has been described a few days before the onset of symptoms or from asymptomatic cases.5, 6, 7
Many studies reported fever and cough as the most prevalent initial symptoms in mild form of Covid-19.8 , 9 With myalgia, having one of these 3 symptoms would identify at least 90% of Covid-19 cases, regardless of gender or age. About a third of cases also reported anosmia-ageusia and surprisingly, this symptom was associated with an increased delay to consultation. However, anosmia-ageusia was firstly reported in the media and in the literature at the end of March 202010 and given our study period, participants probably did not identify immediately such symptom to be related to Covid-19.
In conclusion, the quick identification of Covid-19 HCW should be improve in both Covid-19 and Covid-19 free departments, to prevent the in-hospital transmission of SARS-CoV-2; the presence of a cough, fever, myalgia, as well as anosmia-ageusia, should lead to systematic screening for SARS-CoV-2 infection and isolation of suspected HCW until a definite diagnosis is made.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding
This study was funded by Sorbonne Université, Agence Nationale de recherche and the Agence Nationale de Recherche sur le SIDA et les hépatites virales (ANRS).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2020.06.048.
Appendix. Supplementary materials
References
- 1.Guangming Y., Hualiang L., Song C., Shichan W., Zhikun Z., Wei W. Environmental contamination of SARS-CoV-2 in healthcare premises. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease 2019 (Covid-19) Interim Guidance. 2020.
- 3.World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) When Covid-19 Disease Is Suspected: Interim Guidance. 2020.
- 4.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2020. Personal Protective Equipment (PPE) Needs in Healthcare Settings for the Care of Patients With Suspected or Confirmed 2019-nCoV. [Google Scholar]
- 5.Yan B., Lingsheng Y., Tao W., Fei T., Dong-Yan J., Lijuan C. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhen-Dong T., An T., Ke-Feng L., Peng L., Hong-Ling W., Jing-Ping Y. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26(5):1052–1054. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camilla R., Mirjam S., Peter S., Gisela B., Guenter F., Claudia W. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei-Jie G., Zheng-Yi N., Yu H., Wen-Hua L., Chun-Quan O., Jian-Xing H. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaolin H., Yeming W., Xingwang L., Lili R., Jianping Z., Yi H. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet Lond Engl. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gareth I. Sixty seconds on . . . anosmia. BMJ. 2020;368:m1202. doi: 10.1136/bmj.m1202. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.