Abstract
Currently, a few of studies revealed that there is an association between mastication and cognitive impairment. There is no study of Korean adult representative samples in relation to mastication and cognitive decline. This study was to investigate the relationship between mastication and mild cognitive impairment in Korean adults.
A population-based cross-sectional study was conducted in which a total of 7029 subjects (2987 men and 4042 women) over 45 years old were surveyed from the Korea Longitudinal Study on Aging (KLoSA), Round 5th survey. Logistic regression analysis was performed for the study data controlling for confounding factors such as age, gender, education, income, smoking, drinking, exercise, wearing denture, and the number of chronic diseases.
Decreased chewing function is associated with mild cognitive impairment (odds ratio [OR] = 3.24, 95% confidence interval [CI] = 2.67–3.93) after controlling for confounding variables. In the participants who did not wear dentures, the reduction of chewing function was strongly correlated with mild cognitive impairment (OR = 3.97, 95% CI = 3.11–5.08).
Mastication was associated with mild cognitive impairment. To prevent cognitive decline, health specialists should pay more attention to the decline of the mastication in people without dentures.
Keywords: dentures, mastication, mild cognitive impairment, oral health
1. Introduction
With on-going population aging worldwide, the elderly are not only susceptible to diseases but also have a substantial economic burden due to healthcare services and therefore, have a lower quality of life.[1–3] Among the diseases in elderly, interest in cognitive impairment is increasing because of its rapidly increasing prevalence and its catastrophic consequences.[4]
Recent clinical and population-based studies estimate an mild cognitive impairment (MCI) prevalence of 10% to 20% among adults aged 65 years and older although there is variation in the diagnostic criteria and sample characteristics across studies.[4,5] The prevalence of MCI increases with age, apolipoprotein E e4 genotype, low education attainment, cardiovascular disease, and its risk factors (e.g., diabetes and hypertension), prior critical illness (e.g., sepsis), lack of nutrients such as vitamin B, and income inequality.[4–8] In addition, a reduced mastication in animal experiments has been identified as one of the factors. A previous animal study using a mouse model on a liquid diet reported that a reduced masticatory function results in morphological change and reduced activity of the hippocampus, and another study using senescence-accelerated mouse prone-8 (SAMP8) mice with lost molars reported a reduced concentration and number of hippocampal neurons consequently resulting in a spatial learning disability.[9] Moreover, a study using a mouse model with the upper molar extracted showed a consequently increased deposition of ß–amyloids, which are associated with encephalopathies, and a reduced number of cells in the hippocampus.[10]
In a population-based study, it was confirmed that mastication may be related to mild cognitive function. A few clinical studies have reported that younger people (20–34 years old) experienced an increased activity in the frontal lobe during the mastication process, which consequently induced an increased attentiveness and improved cognitive function.[11] Another study demonstrated an increased cerebral blood flow during a voluntary mastication process in edentulous patients, after the recovery of masticatory function using dentures.[12] Moreover, elderly people (70–74 years old) in a community showed an association between reduced masticatory function and reduced brain function in a study that used a model that adjusted for various factors including age, gender, socioeconomic factors, health-related activities, and chronic diseases.[13] Another larger-scale study on a population of ≥50 year olds reported that individuals with a normal masticatory function exhibit a greater vocabulary memory and richer vocabulary compared to the individuals with a poor masticatory function.[14]
However, traditional studies have measured the masticatory function of individuals by counting the number of teeth,[15] and not many studies have considered the wearing of dentures to assist with the masticatory function of people. In a cross-sectional study that considered the wearing of dentures and assessed the association between mild cognitive function and the number of teeth in the elderly population (≥65 years old), only the subjects without dentures exhibited a more severe cognitive impairment with less number of teeth.[16] Furthermore, another 4-year follow-up study of an elderly population (≥65 years old) showed similar results in which edentulous subjects without dentures had a significantly higher risk of MCI.[17] Lastly, a long-term follow-up study (18 years) on a large cohort of subjects aged 52 years and older showed that among the male patients experiencing difficulties in mastication, only the subjects without dentures had a significantly higher incidence rate of cognitive impairment.[18]
Therefore, the aim of this study was to investigate the relationship between mastication and mild cognitive function taking into consideration the wearing of dentures in Korean people.
2. Methods
2.1. Study population
The survey data were collected from the Korea Longitudinal Study on Aging (KLoSA).[19] This is a representative sample cohort of a middle-aged Korean population selected for a long-term follow-up study of the aging process. The project was conducted by a trained researcher who directly visited the subjects household and asked questions and recorded the answers on a computer. A detailed questionnaire was used to assess demographic factors, socioeconomic factors, health behaviors, and medical history to assess the normal aging process over time. The study on the aging population conducted by the Korea Employment Information Service (KEIS) under the Ministry of Employment and Labor only includes subjects over 45 years old which represent the middle-aged population in Korea.[19] Based on 90% of the data from the 2005 Population and Housing Census, the regions including 15 different metropolitan cities and provinces, Dongs, Eups, and Myeons (different administrative districts in Korea) were stratified. From each stratum, subjects were selected after applying a two-stage stratified sampling (individuals from houses and from apartments). Detailed information about the study is available on the KLoSA website (https://survey.keis.or.kr). The first wave of KLoSA was conducted in 2006, consisting of 4460 men and 5794 women out of a total of 10,254. The 5th wave was used in this study, a total of 7029 people (2987 men and 4042 women) surveyed in 2014. Informed consent was obtained from the study participants. The Institutional Review Boards (IRB) approval of this study was replaced by a research ethics review because KLoSA was nationally approved statistics and publicly available data (http://survey.keis.or.kr).
2.2. Wearing denture and mastication assessment
The masticatory function of the subjects was measured using a self-report questionnaire. A trained investigator asked the question “Can you chew hard food such as apples or meat” to both groups, and the subjects were asked to provide an answer from the following options: “very poor,” “poor,” “moderate,” “good” and “very good.”
The subjects were further categorized into a group with dentures and a group without dentures after the investigator collected the relevant information by asking the question of “Are you currently wearing a denture” and asked the subjects to provide either a “Yes” or “No” answer.
2.3. Cognitive impairment assessment
To assess possible MCI, a widely used clinical tool, the Mini-Mental State Examination, (MMSE) was used.[20] The MMSE is a tool used internationally that assesses directionality, immediate memory, attentiveness, calculation ability, short-term memory, and vocabulary in subjects. The results are converted into a numerical score between 1 and 30 to provide information on the cognitive function of the subject. The MMSE includes questions about the orientation of time and place, registration, calculation, memory, recall, language, and visual construction. Correlation among different MMSEs typically ranges between 0.80 and 0.95.[21] The cut-off value of the MMSE used in this study was 23/24 as used in previous studies.[22,23]
2.4. Covariate assessment
Confounding variables were controlled for in the statistical analysis. Demographical variables including age and gender, socioeconomic variables including educational level and income level, and personal health-related variables including smoking, drinking, regular exercise were the confounding factors that were adjusted for. In addition, the number of chronic diseases for the subjects was adjusted to reflect the changes in the disease state due to the natural aging process. The number of chronic diseases was calculated by assessing if the subject was previously diagnosed with any of the following 9 chronic diseases by an attending physician: hypertension, diabetes, cancer, pulmonary diseases, hepatic diseases, cardiovascular disease, cerebrovascular diseases, psychiatric diseases, and arthritis (including rheumatic diseases). Moreover, the prosthetic devices that were used as dentures–one of the important explanatory variables–were used as a parameter.
2.5. Statistical analysis
The subjects who participated in this study were 7029. Among the subjects responses, 371 variables of cognitive function response, 99 variables of smoking, and 1 variable of chronic disease data were missing and these values were estimated by applying multiple imputations. We generated 5 data sets to replace missing values with different substitutions according to the (a certain) algorithm, analyzed each of the 5 completed data sets, and calculated the parameter estimates and standard errors from the analysis results of each data set. Finally, the results of each dataset were combined with Rubin rule and to produce the final data. After dividing the 7029 subjects into either the normal cognitive function group or the reduced cognitive function group, t test and Chi-Squared test were used to assess the differences between the prosthetic devices used as dentures and the following: differences in sociodemographic factors, differences in health-related activities and the number of chronic diseases (Table 1). To confirm the correlations between the main explanatory variables and the outcome variables after adjusting for confounding variables, we performed multivariate logistic regression (Tables 2 and 3). The collected data were analyzed with the IBM SPSS (IBM SPSS 25.0 for Windows, SPSS Inc, Chicago, IL, USA) program, and statistical significance was considered as 0.05.
Table 1.
Demographic characteristics of the subjects (n = 7029).
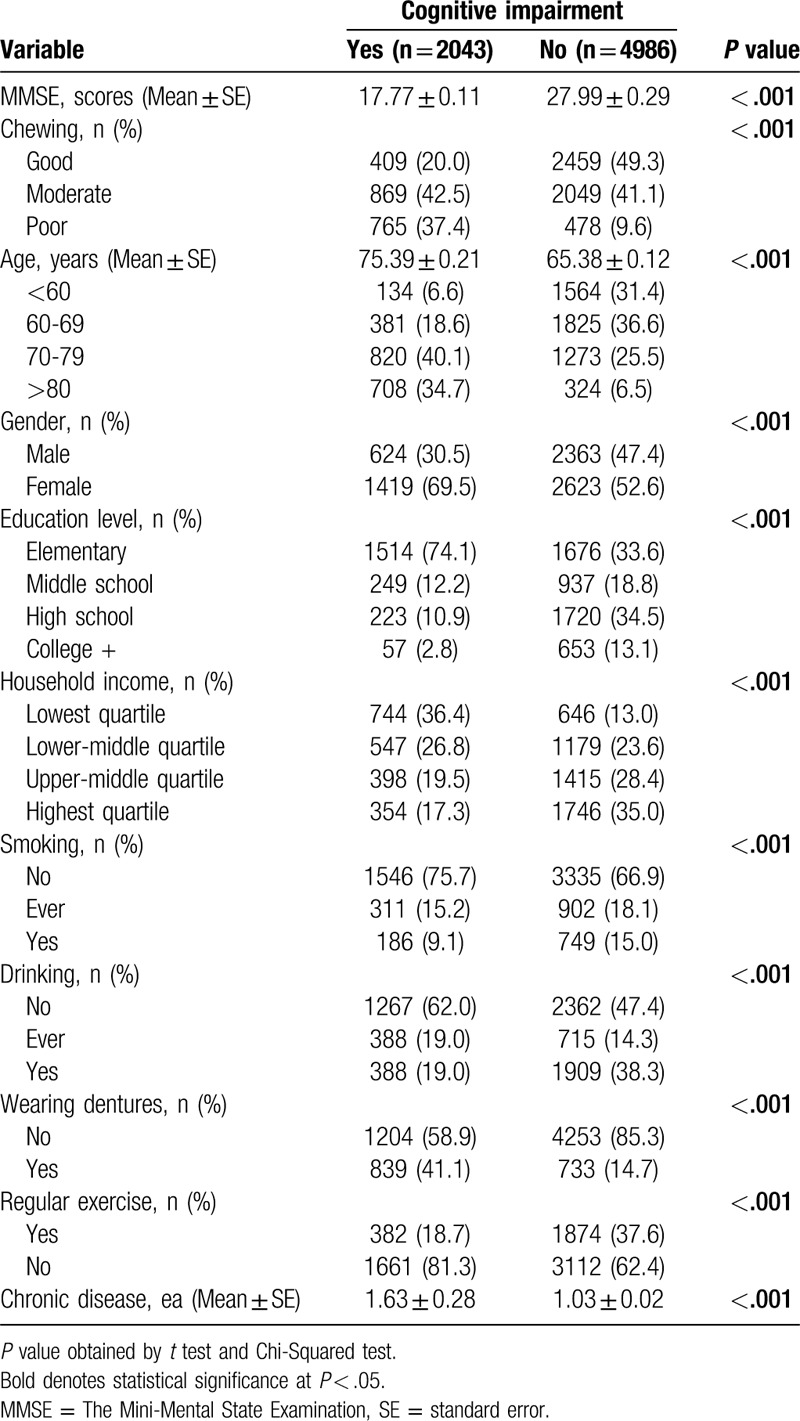
Table 2.
Adjusted associations between chewing ability and mild cognitive impairment (no = 0, yes = 1) using logistic regression model (n = 7029).
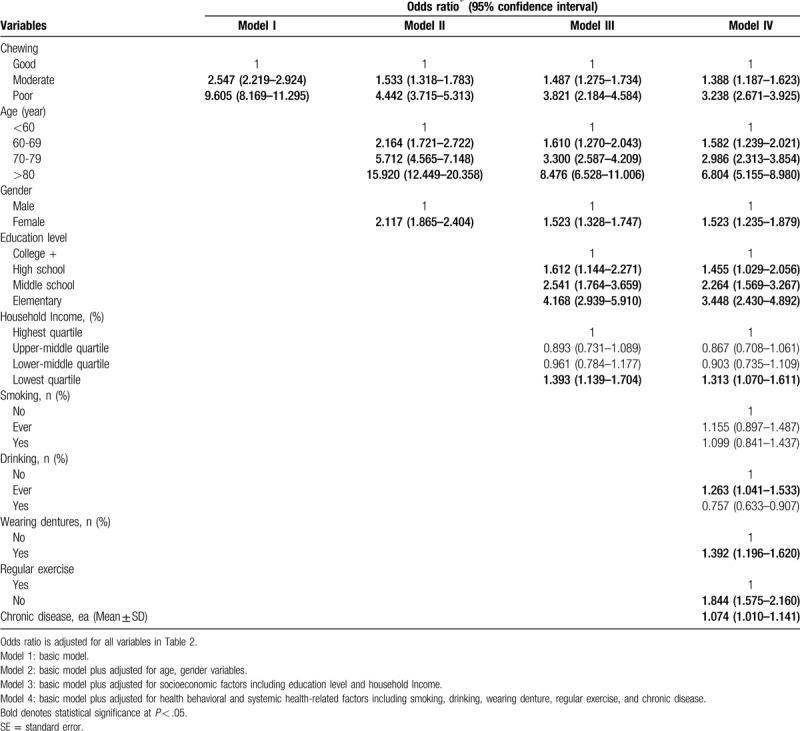
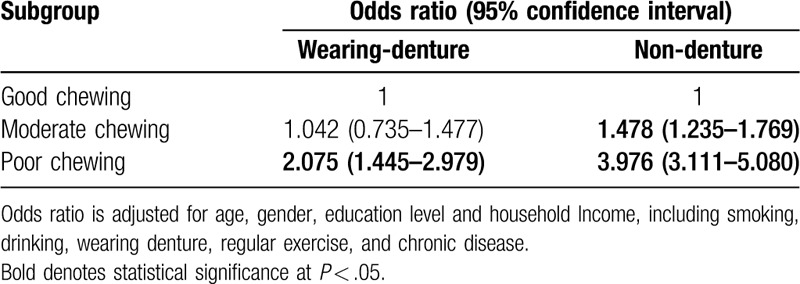
Table 3.
Adjusted associations between chewing ability with wearing denture and mild cognitive impairment (no = 0, yes = 1) using logistic regression model (n = 7029).
3. Results
Among the 7029 subjects who participated in the study, 29.1% exhibited a reduced cognitive function, and 70.9% had a normal cognitive function. Average MMSE scores for the impaired group and the normal group were 17.77 ± 0.11 and 27.99 ± 0.29, respectively. There were differences in age, gender, educational level, household income, smoking, drinking, regular exercise, prosthetic devices used as dentures, and the number of chronic diseases between the impaired group and the normal group (Table 1).
Individuals with a poorer masticatory function had an odds ratio (OR) 9.61-fold higher (95% confidence interval [CI]=18.17–11.30) for MCI compared to those with a good masticatory function. When adjusted for age and gender, the ORs were 1.53-fold (95% CI=1.32–1.78) and 4.44-fold (95% CI=3.72–5.31) higher for individuals with a moderate and poor masticatory function, respectively, compared to those with good masticatory function. Therefore, the dose-dependent effect between masticatory function and MCI was statistically significant. Similarly, in Model 3 that controlled for gender, age, education level, and household income, the OR (3.82, 95% CI = 2.18–4.58) showed a similar pattern. Once again, in the final model that controlled for all confounding variables, the OR was 3.24-fold (95% CI = 2.67–3.93) higher in the individuals with a poor masticatory function compared to those with a good masticatory function (Table 2).
Although smoking was not significant in the final model, the prosthetic devices used as dentures showed a negative correlation with mild cognitive function (OR = 1.39, 95% CI = 1.20–1.62). Looking at the analysis of the interaction effect between masticatory function and wearing denture, the OR was 0.96-fold (95% CI = 0.93–0.99). Therefore, we performed a subgroup analysis after categorizing the subjects into a group with dentures and a group without dentures. In both groups, there was an association between a poor masticatory function and MCI. In the group with dentures, the OR was 2.08-fold (95% CI = 1.45–2.98) higher in the individuals with a poor masticatory function compared to those with a good masticatory function. The difference was not significant for the individuals with a moderate masticatory function. On the other hand, the group without dentures showed a stronger positive correlation between masticatory function and MCI compared to the group with dentures. More specifically, the individuals with a moderate masticatory function showed a 1.48-fold (95% CI = 1.24–1.77) higher OR, and the individuals with a poor masticatory function showed a 3.98-fold (95% CI = 3.11–5.08) higher OR compared to the individuals with a good masticatory function (Table 3).
4. Discussion
This cross-sectional analysis is a deduced study from the nationally representative KLoSA data for a population aged 45-years and older and is the first study to analyze the association between masticatory function and MCI taking into consideration the prosthetic devices used as dentures.
The mechanism behind the association between masticatory function and reduced cognitive function can be summarized into the following 4 aspects. First, mastication directly stimulates the hippocampus and therefore increases the area and number of neurons. An increased number of cells in the hippocampus – responsible for cognitive function and memory – activates brain function and prevents cognitive impairment. Second, mastication increases cerebral blood flow and thereby provides a greater oxygen supply, and the increased cerebral blood flow promotes the activity of brain cells and consequently strengthens cognitive function. Third, mastication allows for more frequent nutritional intake, and especially, the consumption of vitamin B strengthens brain function. Lastly, cell damage from inflammatory cells can induce the loss of brain cells and the consequent brain function impairment. This can be supported by several previous studies that demonstrated the association between various inflammatory diseases and MCI.[24]
The results of this study show, after controlling for confounding variables, the association between masticatory function and mild cognitive function, which are similar to the outcomes of previous studies.[25,26] Another study that included a large cohort of a middle-aged population from 14 European countries also demonstrated that individuals with poor masticatory function exhibited a poorer vocabulary memory and impaired vocabulary.[14] The level of impairment was more pronounced for vocabulary than for calculation ability, which can explain the fact that the progression of dementia often causes greater difficulties in maintaining a rich vocabulary rather than a simple calculation ability. However, to draw a more clear interpretation of this result, there is a need for additional anatomical studies to identify clearly the mechanisms for the abilities associated with calculation and vocabulary.
In this study, the OR between masticatory function and MCI was 3.98 (95% CI = 3.11–5.08) in the group without dentures, which is 1.9-fold higher than the OR of 2.08 (95% CI = 1.45–2.98) in the group with dentures. We observed a strong positive correlation between reduced masticatory function and MCI, and more specifically, the dose-dependent effect between masticatory difficulties and MCI was only observed in the group without dentures. A previous study that performed a 6-year follow-up on patients admitted due to mental disorders demonstrated that the trend for the incidence rate of mental disorders was 2-fold higher in the group of patients without dentures compared to the group with dentures[27] and another 4-year follow-up study on a cohort of subjects aged ≥65 years showed that the group with masticatory discomfort exhibited a 2.73-fold higher incidence rate of dementia after 4 years. More specifically, from the larger group of edentulous subjects, the group with dentures exhibited a 2.70-fold increase in the incidence rate of dementia while the group without dentures exhibited a 4.57-fold increase. The difference between the group with and without dentures was 1.7-fold, similar to the difference in the OR between the group with and without dentures in our study.[17] These outcomes further support the hypothesis of our study that the prosthetic devices that were used as dentures assist with masticatory function and thus prevent brain function impairment.
Another previous study on a smaller, regional cohort of an elderly population aged ≥65 years in Korea reported that the prevalence of dementia was 50% higher in the group without dentures compared to the group with dentures after considering the number of teeth, gender, age, educational level, and chronic diseases. More specifically, elderly people (≥65-years of age) had greater difficulties in consuming fish and fruits than meats as they lost their teeth.[16] Several key vitamins for brain function are included in fish and fruits, and the limited consumption of a certain food type due to the loss of teeth appears to accelerate the impairment of brain function. Therefore, individuals with the progressive loss of teeth should be treated to improve masticatory function and consequently restore a balanced nutritional intake and increased cerebral blood flow and brain cell functionality, thereby preventing or delaying the onset of MCI.
However, we were not able to determine a clear causal relationship whether MCI results in poor masticatory function, or poor masticatory function results in MCI. A recent literature review of studies assessed the association between masticatory function and mild cognitive function reported from 17 cross-sectional and 6 longitudinal studies, and a significant association between reduced masticatory function and MCI was observed in 16 and 5 of the studies, respectively. Furthermore, 5 out of 6 longitudinal studies and 4 out of 5 cross-sectional studies have reported an association between reduced masticatory function and the incidence rates of dementia and memory disorders. Therefore, a reduced masticatory function can be considered as one of the important risk factors of MCI.[28]
This study has dental policy implications. Regular dental care is known to be associated with a decreased risk of dementia occurrence among older adults.[29] Under the universal health insurance system, middle-aged and older Korean adults might have more access than non-universal health system countries such as the United States where older adults with public health insurance or uninsured middle-aged adults have limited access to dental care.[30] Appropriate denture use, at least, and regular dental care among MCI patients might have a protective role in the progression from MCI to dementia. Future comparative studies are urgently warranted to see whether a link between appropriate denture use and the progression from MCI to dementia can be replicated in countries where different health care systems, universal vs. non-universal, have been adopted.
This study has 3 main strengths. First, the sample cohort in this study is a representative cohort of a middle-aged Korean population. Most studies have used samples from a specific population or region, but we used large-scale national data from the KLoSA and performed weighted composite sample analysis to represent the middle-aged population of Korea. Second, all data were collected by an experienced investigator trained for the establishment of a national database. Therefore, the reliability and validity of the responses are high. Third, trained interviewers for the collection of responses directly visited the household and performed in-person interviews although, because obtained responses were independent of the interviewees visual capabilities or capability of understanding the questions, the responses from illiterate individuals or individuals with visual impairment could be included in the study.
We do however acknowledge several important limitations of this study. First, the masticatory function in this study was assessed using a subjective variable, and the MMSE value was used as a variable over clinical mild cognitive assessment values. Second, an assessment of the natural teeth and the prosthetic devices used as dentures was not clinically performed. Therefore, there is no information available to explain the reason for not wearing a denture – whether because it was unnecessary or because of other reasons. Third, there is no information regarding the status of the dentures in the subjects wearing a denture, whether it is a partial denture or a full denture. Lastly, the assessment of masticatory function was based on a self-report, and a threshold difference for the objective masticatory function may exist between the subjects with and without dentures. Therefore, interpretation of the results should be carefully done. Nonetheless, when considering the impracticality of performing clinical assessments of all 7000 subjects on site to analyze a large, representative cohort of subjects, the results obtained using the direct interview method in this study are still very meaningful. This study used the most recent cohort data designed for a longitudinal study on aging in Korea and performed a cross-sectional analysis. Future studies to validate the relationship between oral health and mild cognitive function using the data from 2006 until now will undoubtedly produce more valuable experimental results.
Our findings confirm that mastication is associated with MCI even after controlling for various confounding factors including drinking, smoking, exercise, and chronic illnesses. In particular, wearing a denture can delay or alleviate MCI. Therefore, to prevent cognitive decline, dentists, doctors and oral health specialists should pay attention to the decline of the mastication.
Acknowledgments
We would like to thank all the investigators, staff, and clinicians who participated in this study.
Author contributions
Conceptualization: Donghun Han.
Data curation: Mi-Sun Kim, Donghun Han.
Formal analysis: Mi-Sun Kim, Donghun Han.
Methodology: Ji Won Yoo.
Supervision: Donghun Han.
Writing – original draft: Mi-Sun Kim.
Writing – review & editing: Bumjo Oh, Ji Won Yoo, Donghun Han.
Footnotes
Abbreviations: CI = confidence interval, KEIS = Korea Employment Information Service, KLoSA = Korea Longitudinal Study on Aging, MCI = mild cognitive impairment, MMSE = Mini Mental State Examination, OR = odds ratio, SAMP8 = senescence-accelerated mouse prone-8.
How to cite this article: Kim MS, Oh B, Yoo JW, Han DH. The association between mastication and mild cognitive impairment in Korean adults. Medicine. 2020;99:23(e20653).
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Prince M, Wimo A, Guerchet M, et al. World Alzheimer Report 2015. The Global Impact of Dementia. An Analysis of Prevalence, Incidence, Cost and Trends 2015;London, UK: Alzheimer's Disease International, pp. 6–9. [Google Scholar]
- [2].Hurd MD, Martorell P, Delavande A, et al. Monetary costs of dementia in the United States. N Engl J Med 2013;368:1326–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Klotz AL, Hassel AJ, Schroder J, et al. Oral health-related quality of life and prosthetic status of nursing home residents with or without dementia. Clin Interv Aging 2017;12:659–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA 2014;312:2551–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med 2008;148:427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010;304:1787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Aida J, Kondo K, Kondo N, et al. Income inequality, social capital and self-rated health and dental status in older Japanese. Soc Sci Med 2011;73:1561–8. [DOI] [PubMed] [Google Scholar]
- [8].Vogiatzoglou A, Smith AD, Nurk E, et al. Cognitive function in an elderly population: interaction between vitamin B12 status, depression, and apolipoprotein E epsilon4: the Hordaland Homocysteine Study. Psychosom Med 2013;75:20–9. [DOI] [PubMed] [Google Scholar]
- [9].Onozuka M, Watanabe K, Mirbod SM, et al. Reduced mastication stimulates impairment of spatial memory and degeneration of hippocampal neurons in aged SAMP8 mice. Brain Res 1999;826:148–53. [DOI] [PubMed] [Google Scholar]
- [10].Oue H, Miyamoto Y, Okada S, et al. Tooth loss induces memory impairment and neuronal cell loss in APP transgenic mice. Behav Brain Res 2013;252:318–25. [DOI] [PubMed] [Google Scholar]
- [11].Hirano Y, Obata T, Takahashi H, et al. Effects of chewing on cognitive processing speed. Brain and Cogn 2013;81:376–81. [DOI] [PubMed] [Google Scholar]
- [12].Miyamoto I, Yoshida K, Tsuboi Y, et al. Rehabilitation with dental prosthesis can increase cerebral regional blood volume. Clin Oral Implants Res 2005;16:723–7. [DOI] [PubMed] [Google Scholar]
- [13].Moriya S, Tei K, Murata A, et al. Associations between self-assessed masticatory ability and higher brain function among the elderly. J Oral Rehabil 2011;38:746–53. [DOI] [PubMed] [Google Scholar]
- [14].Listl S. Oral health conditions and cognitive functioning in middle and later adulthood. BMC Oral Health 2014;13:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Li J, Xu H, Pan W, et al. Association between tooth loss and cognitive decline: A 13-year longitudinal study of Chinese older adults. PloS One 2017;12:e0171404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kim JM, Stewart R, Prince M, et al. Dental health, nutritional status and recent-onset dementia in a Korean community population. Int J Geriatr Psychiatry 2007;22:850–5. [DOI] [PubMed] [Google Scholar]
- [17].Yamamoto T, Kondo K, Hirai H, et al. Association between self-reported dental health status and onset of dementia: a 4-year prospective cohort study of older Japanese adults from the Aichi Gerontological Evaluation Study (AGES) project. Psychosom Med 2012;74:241–8. [DOI] [PubMed] [Google Scholar]
- [18].Paganini-Hill A, White SC, Atchison KA. Dentition, dental health habits, and dementia: the Leisure World Cohort Study. J Am Geriatr Soc 2012;60:1556–63. [DOI] [PubMed] [Google Scholar]
- [19].Korea Employment Information Service. Korean Longitudinal Study of Ageing. Available at: https://survey.keis.or.kr/index.jsp. Published October 2016. Updated August 2017. Accessed July 11, 2018. [Google Scholar]
- [20].Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- [21].Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 1992;40:922–35. [DOI] [PubMed] [Google Scholar]
- [22].Okamoto N, Morikawa M, Okamoto K, et al. Relationship of tooth loss to mild memory impairment and cognitive impairment: findings from the Fujiwara-kyo study. Behav Brain funct 2010;6:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Park H, Suk SH, Cheong JS, et al. Tooth loss may predict poor cognitive function in community-dwelling adults without dementia or stroke: the PRESENT project. J Korean Med Sci 2013;28:1518–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Iwasaki M, Yoshihara A, Kimura Y, et al. Longitudinal relationship of severe periodontitis with cognitive decline in older Japanese. J Periodontal Res 2016;51:681–8. [DOI] [PubMed] [Google Scholar]
- [25].Elsig F, Schimmel M, Duvernay E, et al. Tooth loss, chewing efficiency and cognitive impairment in geriatric patients. Gerodontology 2015;32:149–56. [DOI] [PubMed] [Google Scholar]
- [26].Kimura Y, Ogawa H, Yoshihara A, et al. Evaluation of chewing ability and its relationship with activities of daily living, depression, cognitive status and food intake in the community-dwelling elderly. Geriatr Gerontol Int 2013;13:718–25. [DOI] [PubMed] [Google Scholar]
- [27].Shimazaki Y, Soh I, Saito T, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dent Res 2001;80:340–5. [DOI] [PubMed] [Google Scholar]
- [28].Tada A, Miura H. Association between mastication and cognitive status: a systematic review. Arch Gerontol Geriatr 2017;70:44–53. [DOI] [PubMed] [Google Scholar]
- [29].Robitaille A, van den Hout A, Machado RJM, et al. Transitions across cognitive states and death among older adults in relation to education: a multistate survival model using data from six longitudinal studies. Alzheimers Dement 2018;14:462–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Reda SF, Reda SM, Thomson WM, et al. Inequality in utilization of dental services: a systematic review and meta-analysis. Am J Public Health 2018;108:e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


