1. Introduction
In the United States (US), suicide claims more than 45,000 lives each year (Kochanek et al., 2019), affects individuals of all socioeconomic backgrounds (Denney et al., 2009), and is the 2nd and 4th leading cause of death among people aged 10–34 and 35–54, respectively (National Institute of Mental Health, 2019). Over the past two decades, suicide rates in the US increased nearly 25% (Curtin et al., 2016). Further, nearly 10 million US adults have suicidal ideation and over 1 million US adults attempt suicide each year (Crosby et al., 2011). In addition to the significant emotional burden of suicide on loved ones, the economic cost of suicide and suicide attempts, including costs for medical treatment and work lost (e.g., loss of future productivity and salaries), is tremendous reaching nearly $100 billion yearly in the US (Shepard et al., 2016).
The current standard-of-care to prevent suicide and keep an individual safe in psychiatric inpatient units includes a visual check (e.g., every 15-minutes) (Grant, 2007). This is largely because real-time monitoring tools to examine acute suicide risk do not presently exist. The development of real-time monitoring technology for suicide risk has been slow due to the fact that over the past five decades, suicide research has primarily focused on the distal nature of risk factors of suicide which has not unlocked key proximal risk factors of suicide (Franklin et al., 2017; Zalsman et al., 2016). Even risk factors considered ‘proximal’ or warning signs (e.g., increased substance use, hopelessness, talking about or planning suicide, giving away prized possessions) likely have days, weeks, or months between the onset and suicidal behavior. Therefore, it is unsurprising that a recent meta-analysis found that these warning signs and more distal risk factors (e.g., childhood trauma, depression diagnosis) were weak and inaccurate predictors of suicide risk (Franklin et al., 2017).
There is more recent emerging literature that has identified new, objective, and more acute risk factors of suicide (see Table 1 for abbreviations of objective measures). For example, a recent meta-analysis found that the National Institute of Mental Health’s Research Domain Criteria (NIMH RDoC) construct of arousal and regulatory systems as measured by sleep-wakefulness, heart rate (HR) and heart rate variability (HRV), were as powerful predictors of suicide risk as rumination, depression, aggression and loneliness (Glenn et al., 2018). Importantly, unlike the constructs within the negative valence system and systems for social processes, those in the arousal and regulatory systems (e.g., sleep disturbances, physical activity level [PAL], HR/HRV) may have significant benefit in predicting acute suicide risk: these are time series data that can be collected with a very fine temporal resolution, even second-to-second (e.g., HR/HRV = beat to beat). Another significant benefit of these objective measurements is that all of these variables are measurable using wearable technology.
Table 1.
Abbreviations of objective measures
| Abbreviations | Full Name |
|---|---|
| ECG | Electrocardiography |
| EEG | Electroencephalography |
| HF | High-frequency power |
| HR | Heart rate |
| HRV | Heart rate variability |
| LF | Low-frequency power |
| NREM | Non-rapid eye movement |
| PAL | Physical activity level |
| PSG | Polysomnography |
| REM | Rapid eye movement |
| RMSSD | Root mean square of successive differences |
| RSA | Respiratory sinus arrhythmia |
| SDRR | Standard deviation of normal R-R intervals |
| VLF | Very low-frequency power |
To date, there is no systematic review of objective measurements of sleep disturbances, HR/HRV and PAL associated with suicidality. In this review, the term “suicidality” or “suicidal” included completed suicide, a history of suicide, suicidal ideation and suicidal behavior. As such, the aim of this systematic review is to summarize findings on objectively measured acute risk factors and warning signs of death by suicide, a history of suicide, suicidal ideation and suicidal behavior including sleep disturbance, HR/HRV and PAL. The research questions posed in this systematic review are: 1) are sleep problems (e.g., increased nighttime awakenings, longer sleep onset latency), 2) are decreased HRV (or respiratory sinus arrhythmia [RSA]), and 3) decreased PAL associated with more suicidality across studies?
2. Materials and methods
2.1. Search strategy
For this systematic review, we followed the guidelines in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2009). A web-based, systematic literature search was performed using two databases, PubMed and EMBASE, for articles published before March 5, 2019. We used the following keywords for literature search: ‘suicide’, ‘attempted suicide’, ‘suicidal behavior’, ‘suicidal ideation’, ‘suicidality’, ‘depressive disorder’, ‘bipolar disorder’, ‘anxiety’, ‘mental health’, ‘mood disorders’, ‘psychosis’, ‘inhibition’, ‘impulsiveness’, ‘hopelessness’, ‘guilt’, ‘loneliness’, ‘psychomotor agitation’, ‘insomnia’, ‘sleep deprivation’, ‘sleep initiation and maintenance disorders’, ‘physiological stress’, ‘psychological stress’, ‘heart rate’, ‘HRV’, ‘vagal tone’, ‘respiratory sinus arrhythmia’, ‘circadian rhythm’, ‘physical activity’, ‘exercise’, ‘biomarker’, ‘ECG’, ‘EEG’, ‘polysomnography’, ‘fitness tracker’, ‘wearable electronic devices’, ‘actigraphy’, ‘sensor’, ‘smartphone’ (see Table 2 for full search strategy). Search results were limited to those studies with human subjects and articles published in peer-reviewed journals in English.
Table 2.
Full search strategy.
| PUBMED | |
| AND | “suicidality”[tiab] OR “suicide”[tiab] OR “suicidal”[tiab] OR “suicide”[MESH] OR “suicidal ideation”[tiab] OR “suicidal behavior*”[tiab] OR “suicide death” [tiab] OR “suicide, attempted”[mesh] OR “suicide attempted”[tiab] |
| “electrocardiography”[mesh] OR “ECG”[tiab] OR “electrocardiography”[tiab] OR “Electroencephalography”[mesh] or “Electroencephalography”[tiab] OR “EEG”[tiab] OR “EKG”[tiab] OR “polysomnography”[tiab] OR “polysomnography”[mesh] OR “fitness trackers”[mesh] OR “fitness tracker*”[tiab] OR “smart band*”[tiab] OR “fitbit*”[tiab] “apple watch”[tiab] “mobile”[tiab] OR “Biomarkers”[mesh] OR “Biomarker*”[tiab] OR “biological”[tiab] OR “Wearable electronic devices”[MESH] OR “actigraphy”[MESH] OR “actigraphy”[tiab] OR “sensor*”[tiab] OR “wearable*”[tiab] OR “electrocardiography”[MESH] OR “electrocardiography”[tiab] OR “smartphone”[mesh] OR “smartphone*”[tiab] OR “heart rate variability”[tiab] OR “HRV”[tiab] OR “heart rate”[mesh] OR “heart rate”[tiab] OR “Respiratory Sinus Arrhythmia”[mesh] OR “Respiratory Sinus Arrhythmia”[tiab] OR “RSA”[tiab] | |
| “Stress, Physiological”[MESH] OR “Stress”[tiab] OR “Stress, Psychological”[Mesh] OR “Depression”[mesh] OR “depression”[tiab] OR “Sleep initiation and maintenance disorders”[mesh] OR “circadian rhythm”[mesh] OR “circadian rhythm”[tiab] OR “exercise”[mesh] OR “exercise”[tiab] OR “depressive disorder”[mesh] OR “anxiety”[mesh] OR “anxiety”[tiab] OR “physical activity”[tiab] OR “insomnia”[tiab] OR “sleep deprivation”[tiab] OR “mental health”[mesh] OR “mental health”[tiab] OR “bipolar disorder”[mesh] OR “bipolar disorder”[tiab] OR “vagal tone”[tiab] OR “sleep quality”[tiab] OR “nightmare*” OR “Mood Disorders”[mesh] OR “Mood Disorders”[tiab] OR “psychosis”[tiab] OR “psychotic”[tiab] OR “Inhibition (Psychology)”[Mesh] OR “inhibition”[tiab] OR “impulsiveness”[tiab] OR “Dysthymic Disorder”[Mesh] OR “Dysthymic Disorder”[tiab] OR “hopelessness”[tiab] OR “Guilt”[Mesh] OR “Guilt”[tiab] OR “Self Concept”[Mesh] OR “Self Concept”[tiab] OR “Self esteem*”[tiab] OR “Social Isolation”[Mesh] OR “Social Isolation”[tiab] OR “Loneliness”[Mesh] OR “Loneliness”[tiab] OR “Psychomotor Agitation”[Mesh] OR “Psychomotor Agitation”[tiab] OR “Agitation*”[tiab] | |
| EMBASE | |
| AND | ‘suicidal behavior’/exp OR ‘suicide’/exp OR ‘suicide attempt’/exp OR ‘suicidal ideation’/exp ‘suicidal behavior’/exp OR ‘suicide’/exp OR ‘suicide attempt’/exp OR ‘suicidal ideation’/exp OR ‘suicide’ OR ‘suicidal behavior’ OR ‘suicide attempted’ OR ‘suicidal ideation’ OR ‘suicide death’ OR ‘suicidality’ |
| ‘electrocardiogram’/exp OR ‘electrocardiography’/exp OR ‘electroencephalogram’/exp OR ‘electroencephalography’/exp OR ‘polysomnography’/exp OR ‘activity tracker’/exp OR ‘fitbit’/exp OR ‘biological marker’/exp OR ‘actigraph’/exp OR ‘wearable sensor’/exp OR ‘wearable device’/exp OR ‘wearable technology’/exp OR ‘smartphone’/exp OR ‘heart rate variability’/exp OR ‘heart rate’/exp OR ‘respiratory sinus arrhythmia’/exp OR ‘electrocardiogram’ OR ‘electrocardiography’ OR ‘electroencephalogram’ OR ‘electroencephalography’ OR ‘polysomnography’ OR ‘activity tracker’ OR ‘fitbit’ OR ‘biological marker’ OR ‘actigraph’ OR ‘actigraphy’ OR ‘wearable sensor’ OR ‘wearable device’ OR ‘wearable technology’ OR ‘smartphone’ OR ‘heart rate variability’ OR ‘heart rate’ OR ‘respiratory sinus arrhythmia’ OR ‘fitness tracker’ OR ‘biomarker’ | |
| ‘stress’/exp OR ‘physiological stress’/exp OR ‘depression’/exp OR ‘sleep disorder’/exp OR ‘circadian rhythm’/exp OR ‘exercise’/exp OR ‘major depression’/exp OR ‘anxiety disorder’/exp OR ‘anxiety’/exp OR ‘physical activity’/exp OR ‘insomnia’/exp OR ‘sleep deprivation’/exp OR ‘rem sleep deprivation’/exp OR ‘mental health’/exp OR ‘bipolar disorder’/exp OR ‘sleep quality’/exp OR ‘vagus tone’/exp OR ‘nightmare’/exp OR ‘mood disorder’/exp OR ‘inhibition (psychology)’/exp OR ‘impulsiveness’/exp OR ‘dysthymia’/exp OR ‘hopelessness’/exp OR ‘guilt’/exp OR ‘self concept’/exp OR ‘self esteem’/exp OR ‘social isolation’/exp OR ‘loneliness’/exp OR ‘agitation’/exp OR’stress’ OR ‘physiological stress’ OR ‘depression’ OR ‘sleep disorder’ OR ‘circadian rhythm’ OR ‘exercise’ OR ‘major depression’ OR ‘anxiety disorder’ OR ‘anxiety’ OR ‘physical activity’ OR ‘insomnia’ OR ‘sleep deprivation’ OR ‘rem sleep deprivation’ OR ‘mental health’ OR ‘bipolar disorder’ OR ‘sleep quality’ OR ‘vagus tone’ OR ‘nightmare’ OR ‘mood disorder’ OR ‘inhibition (psychology)’ OR ‘impulsiveness’ OR ‘dysthymia’ OR ‘hopelessness’ OR ‘guilt’ OR ‘self concept’ OR ‘self esteem’ OR ‘social isolation’ OR ‘loneliness’ OR ‘agitation’ OR ‘psychosis’ OR ‘ activity level’ |
2.2. Study selection
This systematic review studies included studies that reported quantitative variables that measured sleep, HR/HRV or PAL that had been collective via polysomnography (PSG), electrocardiogram (ECG), or actigraphy in individuals with a history of suicide attempt, or current or a history of suicidal ideation, or individuals who completed suicide. We did not restrict subject age, sex, duration of measurements, types of mental illnesses, and other comorbid conditions. Studies that provided qualitative description of sleep and PAL using subjective measurements (e.g., self-report of sleep on the Pittsburgh Sleep Quality Index) were excluded. In addition, conference abstracts, letters to the editor, case reports and review articles were excluded from the final literature selection.
Two independent reviewers (G.K., H.N.) performed the initial screen of the total searched articles based on the title and abstract. Another independent reviewer (M.P.) provided the deciding vote on disagreements (N = 36). After final selection of the searched articles, compliance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) was evaluated because all of the included articles were observational studies (Von Elm et al., 2007).
3. Results
3.1. Search results
A total of 3,338 records were identified through the electronic database searches of PubMed and EMBASE. After obtaining the initial record of articles, 309 records were removed due to duplication using a citation managing software (EndNote, Philadelphia, PA). The remaining 3,029 articles were screened, and 3,001 articles were excluded based on the title and abstract not including objective and/or subjective measures of suicide. Another 5 articles were excluded after evaluating eligibility based on full-text review. Consequently, 23 articles were included in the current systematic review (see Table 3). The flow diagram for literature selection is shown in Figure 1. Mean compliance rate with the STROBE across all studies was 90.9%.
Table 3.
Characteristics of studies of objective measurement of sleep, HR/HRV and PAL in suicide included for full review.
| Study Study design Country |
Sample characteristics | Suicide measure(s) | Objective measure(s) | Duration Settings |
Key results | STROBE |
|---|---|---|---|---|---|---|
|
Dahl et al. (1990) Cross-sectional USA |
MDD with attempted suicide or SI (N=13, 54% female, 15.5±1.4 years); MDD without attempted suicide or SI (N=14, 64% female, 15.2±1.5 years); HC (N=30, 57% female, 15.0±1.6 years) Note: Adolescents; Medication not reported |
Current SI (the item for SI or attempts on K-SADS-P ≥ 4) |
Sleep (EEG): Sleep latency; Awake; Total sleep; Stages 1, 2, 3 and 4; Stage REM; REM period latency; REM density |
3 nights Laboratory |
↑ Sleep latency in suicidal MDD vs. non-suicidal MDD and HC | 20/22 |
|
Sabo et al. (1991) Cross-sectional USA |
MDD with a history of suicide attempt (N=17, 71% female, 39.3±11.6 years); MDD without a history of suicide attempt (N=17, 71% female, 39.4±12.3 years); HC (N=17, 71% female, 39.3±11.4 years) Note: Inpatients/Outpatients; Free of psychotropic drugs for at least 2 weeks |
History of suicide attempt (SADS-L) |
Sleep (EEG): Sleep latency; Sleep efficiency; Late-night delta counts; REM time; Number of REM periods; % REM sleep; REM sleep activity; Minimum REM latency; REM density; REM intensity |
Overnight Clinic |
↑ Sleep latency in attempters vs. HC; ↓ Sleep efficiency and late-night delta counts in attempters vs. HC; ↑ REM time and activity in period 2, and more delta wave counts in NREM period 4 in attempters vs. non-attempters | 19/22 |
|
Keshavan et al. (1994)
Cross-sectional USA |
SA/SZ with a history of SI or attempt (N=19, 58% female, 30.6±7.7 years); SA/SZ without a history of SI or attempt (N=20, 40% female, 32.3±8.6 years) Note: Inpatients; Free of psychotropic drugs for at least 2 weeks |
History of SI or suicide attempt (review of medical records) |
Sleep (EEG): Number of REM periods; REM latency-awake; Total REM time; Total REM activity; Total REM density; REM time, activity and density in REM P1 |
2 nights Clinic |
↑ REM activity in suicidal SA/SZ vs. non-suicidal SA/SZ | 18/22 |
|
Goetz et al. (2001) Cross-sectional USA |
MDD with SI or attempt at baseline (N=18, 14.5±1.3 years); MDD without SI or attempt at baseline but with SI or attempt during approximately 12-year follow-up period (i.e., future suicidality) (N=11, 14.5±2.5 years); MDD with non-SI (N=24, 14.8±1.6 years); HC (N=17, 41% female, 15.1±1.4 years) Note: Adolescents; Gender not reported; Free of psychotropic drugs for at least 2 weeks |
Current SI (the item for SI or attempts on K-SADS-P ≥ 4) |
Sleep (EEG): Sleep latency; Awake; Total sleep Stages 1, 2, 3 and 4; Stage REM; REM period latency; REM density |
3 nights Laboratory |
↑ First REM period in MDD with current and future suicidality vs. MDD with non-suicidality and HC | 20/22 |
|
Agargun and Cartwright. (2003) Cross-sectional USA |
MDD with SI (N=13); MDD without SI (N=13) Note: Non-patients depressed sample; All met a diagnosis of current MDD (SCID, BDI ≥ 14 or HDRS ≥ 18); Unmedicated; Gender and age not reported |
Current SI (item 9 on BDI ≥ 1 or item 3 on HDRS ≥ 1) |
Sleep (EEG): REM latency; % REM sleep; Number of REM periods; Total sleep time; Sleep efficiency |
3 nights Laboratory |
↓ REM latency in suicidal MDD vs. non-suicidal; ↑ REM % in suicidal MDD vs. non-suicidal |
18/22 |
|
Lemogne et al. (2011) Cross-sectional France |
Individuals who completed suicide (N=133, 20% female, 44.6±13.0 years); Individuals who did not complete suicide (N=323,577, 37% female, 44.7±11.8 years) Note: Medication not reported |
Completed suicide (review of medical records); Follow-up time period was 9.1 years on average to death by suicide |
HR (ECG): HR |
10 minutes Laboratory |
↑ HR predicted suicide | 21/22 |
|
Chang et al. (2012) Cross-sectional Taiwan |
MDD with SI (N=261, 49% female, 42.3±14.3 years); MDD without SI (N=237, 52% female, 35.6±13.2 years); HC (N=462, 49% female, 40.7±14.9 years) Note: Outpatients; Free of psychotropic drugs for at least 2 weeks |
Current SI (Item 3 on HDRS ≥ 1) |
HRV (ECG): HR; SDRR; VLF; LF; HF; LF/HF |
5 minutes Laboratory |
↑ HR in suicidal MDD vs. non-suicidal MDD; ↓ SDRR, LF and HF in suicidal MDD vs. non-suicidal MDD; ↓ SDRR and HF in suicidal MDD vs. HC |
20/22 |
|
Chang et al. (2013) Cross-sectional Taiwan |
MDD with SI (N=237, 48% female, 40.8±14.3 years); MDD without SI (N=233, 52% female, 38.9±14.1 years); HC (N=462, 49% female, 40.7±14.9 years) Note: Remitted MDD; Outpatients; Free of psychotropic drugs for at least 2 weeks |
History of SI during past depression (it was not reported how they assessed) |
HRV (ECG): HR; SDRR; VLF; LF; HF; LF/HF |
5 minutes Laboratory |
↓ SDRR, LF and HF in suicidal MDD vs. non-suicidal MDD and HC | 20/22 |
|
Singareddy et al. (2013) Cross-sectional USA |
Children with self-harm behavior (N=27, 54% female, 8.8±1.9 years); Children without self-harm behavior (N=666, 52% female, 8.8±1.7 years) Note: Self-harm behavior includes suicide attempt; Medication not reported |
Current symptoms of self-harm behavior (questions to the parent about self-harm and suicide attempt over the past 2 months) |
Sleep (PSG): Sleep latency; REM latency; Total sleep time; Sleep efficiency; % Stages 1 and 2; % REM; Wake after sleep onset; Apnea hypopnea index |
Overnight Laboratory |
↑ % REM in self-harm behavior group vs. non self-harm behavior group | 20/22 |
| Guitierrez et al. (2016) Cross-sectional USA |
Veterans with a history of or current SI (N=97, 54.6±11.3 years) Note: Gender and medication not reported |
History of SI (review of medical record or SBQ-R ≥ 1) |
HRV (ECG): Resting RSA |
Duration and setting not reported | No significant association between RSA and SI | 15/22 |
|
Ballard et al. (2016) Cross-sectional USA |
MDD or BPD with SI (N=39, 44% female, 44.0±13.1 years); MDD or BPD without SI (N=26, 69% female, 43.5±12.3 years); Note: Treatment-resistant inpatients; Free of psychotropic drugs for at least 2 weeks (MDD); Lithium or valproate (BPD) |
Current SI (item 3 on HDRS ≥ 1 or item 10 on MADRS ≥ 4) |
Sleep (EEG): Total sleep time; Wake after sleep onset; Sleep efficiency; Nocturnal wakefulness |
Overnight Laboratory |
↑ Nocturnal wakefulness between 4am and 4:59am in suicidal group vs. non-suicidal group; Significant association between nocturnal wakefulness between 4am and 4:59am and HDRS and MADRS suicide items | 21/22 |
|
Forkman et al. (2016) Cross-sectional Germany |
Individuals with SI (N=13); Individuals without SI (N=24); Note: Students (N=37, 73% female, 24.5±4.1 years); No history of suicide attempt; Unmedicated |
Lifetime SI (Four questions on lifetime SI ≥ 1) (e.g., “I wished I were dead”: 0 “never” to 3 “often”) |
HR/HRV (ECG): HR; RMSSD; HF |
Duration not reported Setting not reported |
Significant correlation between a spectral frequency measures of resting vagally mediated HRV and SI, and mean HR and SI after controlling for depression; A trend correlation between RMSSD and SI | 19/22 |
|
Wilson et al. (2016) Cross-sectional USA |
MDD with a history of suicide attempt (N=13, 100% female, 34.1±10.1 years); MDD without a history of suicide attempt (N=22, 100% female, 31.2±11.5 years) Note: Unmedicated (N=31); Antidepressants (N=4); Borderline personality disorder (N=23); Substance use disorder (N=16) |
A history of suicide attempt (it was not reported how the authors confirmed a history of suicide attempt) |
HRV (ECG): HF |
5 minutes Laboratory |
↓ HF during stressor task in attempters vs. non-attempters | 21/22 |
|
Chang et al. (2016) Cross-sectional Taiwan and Norway |
In Taiwan (N=532,932), Individuals who completed suicide (N=569, 42% female, 46.3±15.6 years); Individuals who did not complete suicide (N=532,363, 52% female, 41.4±13.9 years) In Norway (n=74,922), Individuals who completed suicide (N=188, 23% female, 47.9±16.0 years); Individuals who did not complete suicide (N=74,734; 51% female, 49.5±17.6 years) Note: MJ cohort (Taiwan); HUNT cohort (Norway); Medication and diagnosis not reported |
Completed suicide (review of medical records) |
HR (ECG): HR |
Duration not reported Setting not reported |
↑ HR in suicidal group vs. in the non-suicidal group in both countries | 20/22 |
|
Khandoker et al. (2017) Cross-sectional UAE |
MDD with SI (N=16, 69% female, 37.5±10.4 years); MDD without SI (N=16, 81% female, 15.2±1.5 years); HC (N=29, 59% female, 28.0±6.4 years) Note: Outpatients; Medication not reported |
Current SI (MINI – ‘C’ module > 9) |
HR/HRV (ECG): HR; RMSSD; SDRR; VLF; HF; LF; LF/HF |
10 minutes Setting not reported |
↓ RMSSD in suicidal MDD vs. non-suicidal MDD and HC | 19/22 |
| Tsypes et al. (2017) Cross-sectional USA |
Individuals with a history of suicide attempt (N=56, 100% female, 35.5±5.4 years); Individuals without a history of suicide attempt (N=56, 100% female, 35.0±6.3 years) Note: Community sample; Medication not reported; Suicide attempt group: Lifetime MDD (N=36), Lifetime anxiety disorder (N=24), Lifetime anorexia or bulimia (N=2), Lifetime alcohol use disorder (N=24), Lifetime substance use disorder (N=21); No suicide attempt group: Lifetime MDD (N=38), Lifetime anxiety disorder (N=16), Lifetime anorexia or bulimia (N=2), Lifetime alcohol use disorder (N=18), Lifetime substance use disorder (N=12) |
A history of suicide attempt (One interview question: “A suicide attempt is defined as intentionally hurting yourself with at least some wish to die at that time. How many times have you attempted suicide in your life?”) |
HRV (ECG): Resting RSA |
2 minutes Laboratory |
↓ Resting RSA in attempters vs. non-attempters after controlling for lifetime history of psychiatric diagnoses and current symptoms of depression and anxiety, age, income, race/ethnicity | 21/22 |
|
Chang et al. (2017) Cross-sectional Taiwan |
MDD with current SI (N=58, 40% female, 32.4±11.2 years); MDD without a history of SI (N=61, 39% female, 31.9±12.8 years) Note: Outpatients; Unmedicated |
History of SI (C-SSRS) |
HR/HRV (ECG): HR; SDRR; VLF; LF; HF; LF/HF |
5 minutes Laboratory |
↓ SDRR, HF and LF in suicidal MDD vs. non-suicidal MDD after controlling for age, gender, BMI, exercise, smoking, alcohol consumption, stress, depression and cortisol level; Negative correlation between the intensity of SI and SDRR, LF and HF |
21/22 |
|
Bernert et al. (2017a) Longitudinal USA |
Undergraduate students with a history of suicide attempt and recent suicide ideation (≤ 6 months) or no history of suicide attempt but current SI (≤ 1 month) (N=50, 72% female, 19.2±1.4 years) Note: Antidepressants (N=5); SNRI (N=2); Anxiolytics (N=1); Antipsychotic (N=1); Mood stabilizer (N=1) |
History of suicide attempt and recent suicide ideation (BSS for Suicide Ideation, Pierce SIS for intent and severity of past suicide attempts) |
Sleep (actigraphy): Sleep-onset latency; Total sleep time; Wake after sleep onset; Sleep efficiency; Sleep variability; Time in bed; Nap and sleep interval frequency |
3 weeks Home |
Significant correlation between total sleep time and sleep variability and changes in BSS for SI between baseline and 7-day follow-up; Significant correlation between sleep variability and changes in BSS for SI between baseline and 21-day follow-up |
22/22 |
|
Bernert et al. (2017b) Cross-sectional USA |
MDD or BPD with current SI (N=31); MDD or BPD without current SI (N=23) Note: Treatment-resistant patients; Free of psychotropic drugs for at least 2 weeks (MDD) Lithium or depakote (BPD); MDD (N=30, 33% female, 47.4±13.3 years); BPD (N=24, 71% female, 44.4±11.6 years) |
Current SI (Item 3 on HDRS ≥ 1) |
Sleep (EEG): Sleep efficiency; REM latency; Wakefulness after sleep onset; Total sleep time; Percent of REM sleep; Duration of NREM |
Overnight Laboratory |
↓ Stage 4 NREM sleep in suicidal group vs. non-suicidal group after controlling for depression | 21/22 |
| James et al. (2017) Cross-sectional USA |
Children with a history of SI and parental criticism (N=20, 35% female, 8.9±1.3 years); Children with a history of SI who did not have critical parents (N=51, 44% female, 8.9±1.3 years); Children with no history of SI but with parental criticism (N=83, 33% female, 9.4±1.5 years); Children with no history of SI nor parental criticism (N=242, 52% female, 9.5±1.5 years); Note: MDD (N=2); GAD (N=12); PTSD (N=6); OCD (N=8); SAD (N=31); Medication not reported |
Endorsement in suicide question from K-SADS-P (“sometimes children who get upset or feel bad think about dying or even killing themselves. Has your child ever had these types of thoughts”) Or item 9 on CDI (“I think about killing myself but would not do it” or “I want to kill myself” were coded as having SI”) |
HRV (ECG): RSA |
12 minutes Laboratory |
↔ Changes in RSA between resting and experiencing positive or negative emotions in children with a history of SI and parental criticism; ↓ RSA when experiencing positive or negative emotions compared to resting in all other children |
21/22 |
|
Littlewood et al. (2019) Longitudinal UK |
Individuals experiencing a MDD episode with current SI (N=51, 67% female, 35.5±12.8 years) Note: Antidepressants (N=34) |
Current SI (BSS) |
Sleep (actigraphy): Sleep efficiency; Sleep onset latency; Total sleep time |
1 week Home |
Significant correlation between shorter total sleep time and higher next-day suicide ideation | 21/22 |
|
Boafo et al. (2019) Cross-sectional Canada |
MDD with acute risk of suicide (N=17, 82% female, 15.0±1.2 years); HC (N=17, 82% female, 14.9±1.1 years) Note: Adolescents; Inpatients; Antidepressants (N=15); Mood stabilizer (N=1); Antipsychotic (N=4) |
Risk of suicide (SBQ-R ≥ 8) |
Sleep (PSG): Sleep latency; Total sleep time; REM latency; REM density; Wake after sleep onset; NREM and REM stages |
Overnight Laboratory |
↑ Sleep latency, REM latency, REM density and relative sleep duration for NREM-stage 1 in suicidal MDD vs. HC | 21/22 |
|
Benard et al. (2019) Cross-sectional France |
BPD with a history of suicide attempt (N=57, 72% female, 47.2±12.6 years); BPD without a history of suicide attempt (N=90, 54% female, 44.8±13.0 years); HC (N=89, 54% female, 39.7±13.4 years) Note: Outpatients; Antidepressants (N=15); Mood stabilizer (N=1); Antipsychotic (N=4) |
History of suicide attempt (DIGS or SCID) |
Sleep and PAL (actigraphy): Time in bed; Assumed sleep; Actual wake time; Sleep efficiency; Sleep latency; Mean activity score; Fragmentation index; Inter-daily variability; Time of the start of the most active 10-h period in daily activities |
3 weeks Home |
Suicidal BPD group began their daily activities significantly earlier than non-suicidal BPD and HC groups | 22/22 |
Abbreviations for diagnosis, medications and assessment tools: BDI = Beck depressive inventory, BPD = Bipolar disorder, BSS = Beck scale for suicide ideation, CDI = Children’s depression inventory, C-SSRS = Columbia suicide severity rating scale, DIGS = Diagnostic interview for genetic studies, GAD = Generalized anxiety disorder, HC = Healthy controls, HDRS = Hamilton depression rating scale, K-SADS-P = Kiddie diagnostic schedule for affective disorders and schizophrenia for school age children, MADRS = Montgomery-Asberg depression rating scale, MDD = Major depressive disorder, MINI = Mini-international neuropsychiatric interview, OCD = Obsessive-compulsive disorder, Pierce SIS = Pierce suicidal intent scale, PTSD = Post-traumatic stress disorder, SA/SZ = Schizoaffective disorder/Schizophrenia, SAD = Social anxiety disorder, SADS-L = Schedule for affective disorders and schizophrenia – lifetime version, SBQ-R = Suicide behaviors questionnaire-revised, SCID = Structured clinical interview for DSM-IV axis I disorders, SI = Suicidal ideation, Stimulant/nonstimulant selective serotonin reuptake inhibitors (SNRI).
Fig. 1.
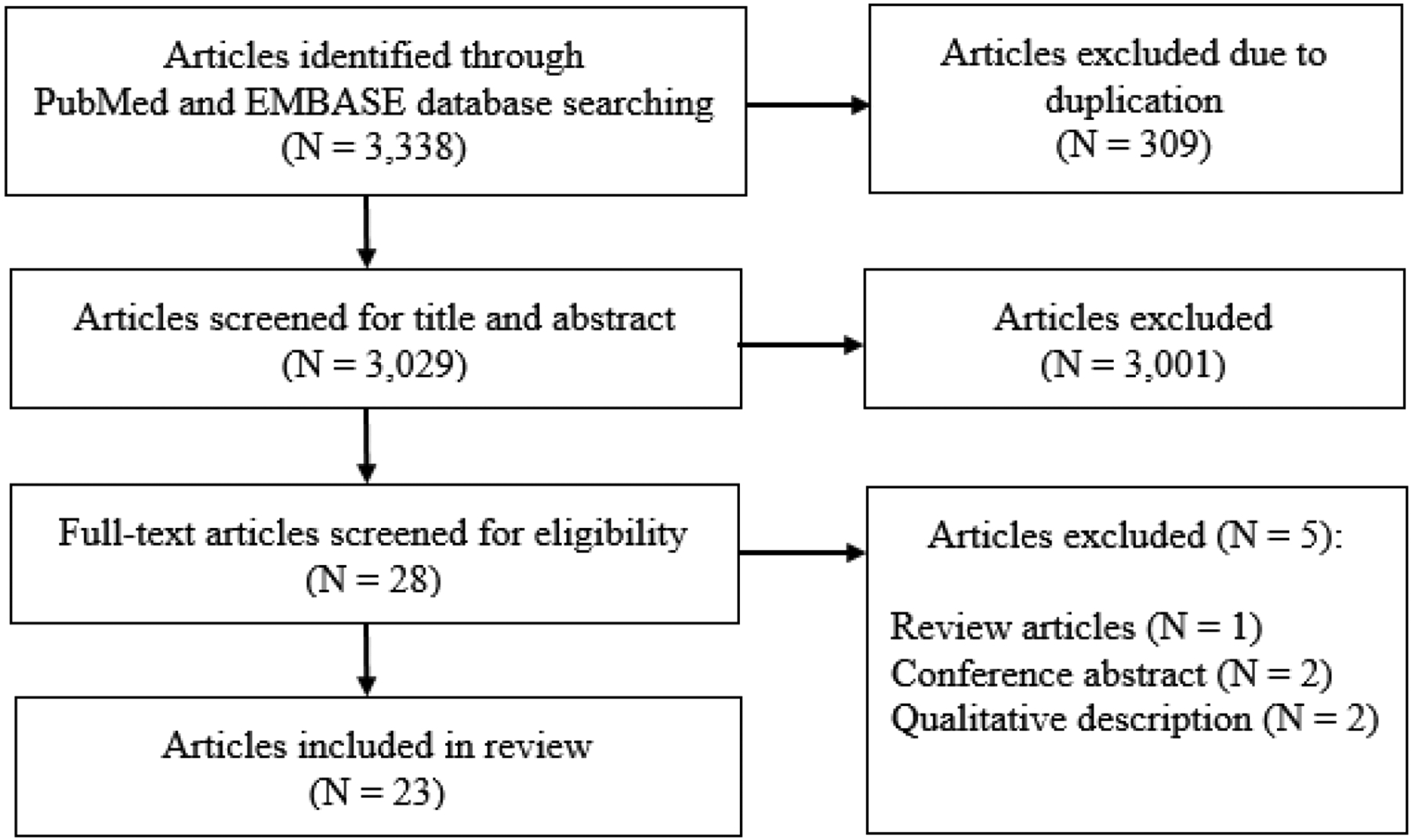
PRISMA consort diagram for literature selections
3.2. Study design and countries
Among the 23 studies included, 18 studies (78.3%) were published in the last 10 years. The vast majority of the included studies (N = 21; 91.3%) reported cross-sectional findings that compared sleep, HR/HRV or PAL between a suicidal group (e.g., individuals with a diagnosis of mental illnesses such as major depressive disorder [MDD] or bipolar disorder [BPD] with a history of suicide attempt) and a control group (e.g., individuals with MDD or BPD without a history of suicidal ideation or suicide attempt). Two studies (8.7%) reported longitudinal findings about associations between changes in current suicidal ideation and changes in sleep variables over the course of 3 weeks (Bernert et al., 2017a; Littlewood et al., 2019). The countries in which the included studies were conducted were: USA (N = 13; 56.6%), Taiwan (N = 4; 17.4%; among these, one study was conducted together with Norway), France (N = 2; 8.7%), Canada (N = 1; 4.3%), Germany (N = 1; 4.3%), United Arab Emirates (N = 1; 4.3%), and United Kingdom (N = 1; 4.3%).
3.3. Characteristics of study subjects
In 17 studies (73.9%), the suicidal group included individuals with a diagnosis of mental illnesses such as MDD, BPD, schizoaffective disorder/schizophrenia (SA/SZ), post-traumatic stress disorder and obsessive-compulsive disorder or individuals currently experiencing an MDD episode. Five studies (21.7%) did not report psychiatric diagnoses of their participants (Chang et al., 2016; Forkmann et al., 2016; Gutierrez et al., 2016; Lemogne et al., 2011; Singareddy et al., 2013). The age group across studies were children (N = 2 studies; 8.7%), adolescents (N = 3 studies; 13.0%) and adults (N = 18 studies; 78.3%). Participants were hospitalized patients with MDD or SA/SZ in three studies (13.0%), and a subgroup were hospitalized patients with MDD in another study (4.3%). In all other studies (N = 19; 82.6%), participants were non-hospitalized patients or from a community sample (e.g. university-based setting). The effects of psychotropic drugs were controlled by using a wash-out period (2 weeks or more) or including unmedicated or mostly unmedicated individuals (> 80% of the study participants) in ten studies (52.2%). In three studies, participants were taking antidepressants, benzodiazepine, mood stabilizers or atypical antipsychotics. Information about psychotropic drugs was not reported in eight studies (34.8%).
3.4. Assessment of suicidality
Participants’ level of suicidality was assessed as current or a history of suicidal ideation or suicide attempt (N = 20; 87.0%), completed suicide (N = 2; 8.7%), or self-harm behavior that includes suicide attempts (N = 1; 4.3%). Assessment tools for suicidality were standardized interviews or questionnaires such as the Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) (First et al., 1994), Kiddie Diagnostic Schedule for Affective Disorders and Schizophrenia for School Age Children (K-SADS-P) (Chambers et al., 1985), and Hamilton Depression Rating Scale (HDRS) (Hamilton, 1986) (N = 15; 65.2%). Three studies (13.0%) reviewed medical records to assess a history of suicidal ideation or suicide attempt (N = 1; 4.3%) and cause of death (i.e., suicide) (N = 2; 8.7%). Another three studies (13.0%) used non-standardized questionnaires for assessing suicidality. Two studies (8.7%) did not report how they assessed participant suicidality.
3.5. Objective measurements
For objective measurements, 11 studies (47.8%) measured sleep using EEG (N = 7; 30.4%), PSG (N = 2; 8.7%) and actigraphy (N = 2; 8.7%). Other eleven studies (47.8%) measured HR/HRV using ECG. One study (4.3%) measured sleep and PAL using actigraphy. The objective measurements were performed in laboratory settings in 14 studies (60.9%), clinic settings (i.e., patient room in inpatients units) in two studies (8.7%), or in naturalistic settings (i.e., home) in three studies (13.0%). The settings were not reported in three studies (13.0%). For the sleep studies, the duration varied from an overnight study to across three weeks of data collection. For the HR/HRV studies, the duration of data collection was between 2 and 12 minutes while participants were resting in a lying posture, watching a video of nature scenes, or discussing topics between children and their parents. Among the eleven HR/HRV studies, three did not report the epoch lengths (27.2%). For the sleep and PAL study, the duration was three weeks.
3.6. Sleep and PAL
All of the 11 sleep studies (overnight to 3-week monitoring) reported abnormal sleep patterns for patients with elevated levels of suicidality. For example, three studies found that sleep latency, the duration between full wakefulness and falling asleep, measured using EEG and PSG was significantly greater in individuals with MDD with current suicidal ideation compared to individuals with MDD without current suicidal ideation or healthy controls (Boafo et al., 2019; Dahl et al., 1990; Sabo et al., 1991). One study found that MDD or BPD with current suicidal ideation had greater duration of being awake between 4am and 5am (i.e., nocturnal wakefulness) as measured using EEG compared to MDD or BPD without current suicidal ideation, and the nocturnal wakefulness was significantly associated with severity of suicidality (Ballard et al., 2016). Seven studies found that activity during rapid eye movement as measured using EEG and PSG was greater in suicidal individuals compared to non-suicidal individuals (Agargun and Cartwright, 2003; Bernert et al., 2017b; Goetz et al., 2001; Keshavan et al., 1994; Sabo et al., 1991; Singareddy et al., 2013). The two longitudinal studies of sleep found that shorter total sleep time as measured by actigraphy was related to increased suicidal ideation within those with current or recent suicidal ideation (Benard et al., 2019; Littlewood et al., 2019).
The association between PAL and suicidality was investigated in one study (3-week monitoring). Individuals with BPD with a history of a suicide attempt began daily activities earlier compare to individuals with BPD without a history of a suicide attempt and healthy controls (Benard et al., 2019).
3.7. HR/HRV
Among the 11 HR/HRV studies (5 to 15 minutes-monitoring), nine studies found abnormal patterns in HR or HRV variables. For example, two studies found greater resting HR in individuals whose cause of death was suicide compared to individuals whose cause of death was not suicide (Chang et al., 2016; Lemogne et al., 2011). In addition, another study found resting HR was greater in individuals with MDD with current suicidal ideation compared to individuals with MDD without current suicidal ideation (Chang et al., 2012). Six studies reported that HRV parameters such as variance of R-R intervals, RSA, low-frequency (LF) or high-frequency (HF) HRV were lower at resting or watching a video of nature scenes for individuals with current or a history of suicidal ideation or suicide attempt than for control groups (Chang et al., 2017; Chang et al., 2012, 2013; Khandoker et al., 2017; Tsypes et al., 2018; Wilson et al., 2016). One study reported reduced variance of R-R intervals was associated with lifetime suicidal ideation (Forkmann et al., 2016). One study reported that there was no association between resting RSA and a history of suicidal ideation among veterans (Gutierrez et al., 2016), however, due to a lack of some important information in their methods (e.g., the authors did not report how long and in what settings and conditions they measured RSA, and their participants’ characteristics such as medication), replication is needed.
4. Discussion
4.1. Summary of key findings
The goal of this paper was to provide a systematic review of the literature regarding objective measurement of sleep, HR/HRV and PAL and their relationship to suicidality including completed suicide, a history of suicide, suicidal ideation and suicidal behavior. Sleep-wakefulness and HR/HRV are variables in the NIMH RDoC arousal and regulatory systems that have been suggested as warning signs of suicide in a recent meta-analysis (Glenn et al., 2018). In the present systematic review, a total of 23 studies were found that objectively collected data regarding sleep, HR/HRV and PAL, and associated them with suicide.
Across the studies reviewed, these objective indices demonstrated consistent patterns associated with suicidality that indicates the potential of their predictive strength to monitor acute suicide risk. Specifically, findings indicate across studies that suicide is related to greater insomnia including greater sleep onset latency and lower sleep efficiency as well as a heightened autonomic state at baseline (i.e., higher HR, lower variance of R-R intervals). Importantly, it is possible that these objective indices (e.g., chronic poor sleep) could lead to increased suicidal ideation. Future studies will need to be conducted that examine the potential bidirectional relationship between these objective data and suicide. To our knowledge, this is the first systematic review of objective patterns in sleep-wakefulness and HR/HRV associated with suicide.
4.2. Limitations
One limitation of this systematic review was that studies that used different methods particularly for sleep studies (PSG, EEG, actigraphy) were combined, and potential differences in their findings due to the different methods could not be considered. However, PSG and EEG are both considered as gold standards, and actigraphy has been well-validated (McCall and McCall, 2012). Due to the limited literature, studies that both controlled for medication (e.g., 2-week washout) and did not control for medication were included, which might have affected the sleep results since psychotropic medications such as antidepressants affect sleep patterns (Wilson and Argyropoulos, 2005). Further, durations of the objective measurements were considerably varied among the sleep studies: from only overnight to three nights. These durations may be insufficient to consider daily or weekly variations in sleep patterns associated with suicide (Baranowski et al., 2008; Van Someren, 2007). In addition, findings from all of the HR/HRV studies were based on only 5–15 minute data collection point, and there was no study that collected HR/HRV for a relatively longer period (e.g., 24 hours). This short-term measurement might have affected results for VLF power and LF/HF (Shaffer and Ginsberg, 2017; Shaffer et al., 2014). In addition, prior studies suggested that sleep, HR/HRV, PAL and mental illnesses such as MDD are not independent of each other but correlated. For example, decreased PAL is associated with poor sleep quality (Benloucif et al., 2004), and decreased variance of R-R intervals is associated with MDD (Nahshoni et al., 2004) and insomnia (Dodds et al., 2017). Thus, it is unclear whether these warning signs serve as independent risk factors of suicide. It will be important to know the effects of each warning sign on suicide risk after accounting for confounding effects of the other warning signs.
4.3. Implications and future direction
Prediction and prevention of suicide is a great challenge, and lack of a method to monitor suicide risk in real-time is one of the primary reasons for the challenge (Kleiman and Nock, 2018). Identifying objective, acute warning signs of suicide can enhance real-time monitoring of suicide risk and address this challenge. It has been suggested that proximal/imminent time-varying factors (i.e., warning signs) are necessary to develop the best prediction model of suicide (Franklin et al., 2017; Zalsman et al., 2016).
Taken together, we found preliminary evidence of sleep, HR/HRV and PAL as objective warning signs of suicide. Notably, previous studies suggested decreased PAL in individuals at risk of suicide (Sibold et al., 2015; Simon et al., 2004; Taliaferro et al., 2008; Taliaferro et al., 2009). In their studies, they measured PAL using subjective self-questionnaire (Sibold et al., 2015; Simon et al., 2004; Taliaferro et al., 2008; Taliaferro et al., 2009). However, there was too little research (i.e., only one study) on objectively measured PAL thus we were unable to determine a possible association between suicidality and PAL.
Given the emerging patterns in the identified objective metrics, areas for future study include: (1) longitudinal studies to investigate trait- or state-like characteristics of sleep, HR/HRV and PAL associated with suicide in order to examine the relationship between changes in suicidal ideation or suicidal behavior and objective variables, (2) field studies (e.g., home settings) are necessary to understand whether current findings for sleep-wakefulness and HR/HRV patterns with suicide are consistent across settings, and (3) continuous sleep, HR/HRV and PAL monitoring in high-risk populations (e.g., psychiatric inpatients) to identify the patterns of these variables related to acute warning signs of suicidal behavior.
5. Conclusion
Based on the present systematic review, the findings provide initial evidence for consistent patterns of objective variables with suicide; however, more studies are needed in order to identify the precise objective variables (e.g., sleep onset latency, LF HRV, HF HRV, LF/HF), as well as time-varying patterns in these variables, that are related to acute suicide risk. Once identified, the potential to invent new ways to monitor and assess suicide risk could be developed, as physiologically-based algorithms could be used within wearable technology, mHealth technology and telemedicine for individuals at risk of suicide to provide real-time monitoring of suicide risk, prevent suicide attempts, and save lives.
Highlights.
Sleep disturbances such as low sleep efficiency was associated with suicidality.
Increased heart rate was associated with suicidality.
Decreased heart rate variability tended to be associated with suicidality.
Evidence of objectively measured physical activity in suicidality was too little.
In 91.3% of the 23 included studies, findings were cross-sectional.
Acknowledgements
Dr. Kang is supported by the National Heart, Lung, and Blood Institute T32 Training Grant (T32HL139430-02). Dr. Salas is supported by the Veteran Health Administration (VHA1I21RX002588). Drs. Matthew and Salas are supported through the use of facilities and resources at the Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX.
References
- Agargun MY, Cartwright R, 2003. REM sleep, dream variables and suicidality in depressed patients. Psychiatry Research 119, 33–39. [DOI] [PubMed] [Google Scholar]
- Ballard ED, e Voort JL, Bernert RA, Luckenbaugh DA, Richards EM, Niciu MJ, Furey ML, Duncan WC, Zarate CA, 2016. Nocturnal wakefulness is associated with next-day suicidal ideation in major depressive disorder and bipolar disorder. Journal of Clinical Psychiatry 77, 825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranowski T, Masse LC, Ragan B, Welk G, 2008. How many days was that? We’re still not sure, but we’re asking the question better! Medicine and Science in Sports and Exercise 40, S544–S549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benard V, Etain B, Vaiva G, Boudebesse C, Yeim S, Benizri C, Brochard H, Bellivier F, Geoffroy PA, 2019. Sleep and circadian rhythms as possible trait markers of suicide attempt in bipolar disorders: An actigraphy study. Journal of Affective Disorders 244, 1–8. [DOI] [PubMed] [Google Scholar]
- Benloucif S, Orbeta L, Ortiz R, Janssen I, Finkel SI, Bleiberg J, Zee PC, 2004. Morning or evening activity improves neuropsychological performance and subjective sleep quality in older adults. Sleep 27, 1542–1551. [DOI] [PubMed] [Google Scholar]
- Bernert RA, Hom MA, Iwata NG, Joiner TE, 2017a. Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. Journal of Clinical Psychiatry 78, e678–e687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Luckenbaugh DA, Duncan WC, Iwata NG, Ballard ED, Zarate CA, 2017b. Sleep architecture parameters as a putative biomarker of suicidal ideation in treatment-resistant depression. Journal of Affective Disorders 208, 309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boafo A, Armitage R, Greenham S, Tavakoli P, Dale A, Nixon A, Lafrenière A, Ray LB, De Koninck J, Robillard R, 2019. Sleep architecture in adolescents hospitalized during a suicidal crisis. Sleep medicine 56, 41–46. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M, 1985. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Archives of General Psychiatry 42, 696–702. [DOI] [PubMed] [Google Scholar]
- Chang CC, Tzeng NS, Kao YC, Yeh CB, Chang HA, 2017. The relationships of current suicidal ideation with inflammatory markers and heart rate variability in unmedicated patients with major depressive disorder. Psychiatry Research 258, 449–456. [DOI] [PubMed] [Google Scholar]
- Chang HA, Chang CC, Chen CL, Kuo TBJ, Lu RB, Huang SY, 2012. Major depression is associated with cardiac autonomic dysregulation. Acta Neuropsychiatrica 24, 318–327. [DOI] [PubMed] [Google Scholar]
- Chang HA, Chang CC, Chen CL, Kuo TBJ, Lu RB, Huang SY, 2013. Heart rate variability in patients with fully remitted major depressive disorder. Acta Neuropsychiatrica 25, 33–42. [DOI] [PubMed] [Google Scholar]
- Chang SS, Bjørngaard J, Tsai M, Bjerkeset O, Wen C, Yip P, Tsao C, Gunnell D, 2016. Heart rate and suicide: findings from two cohorts of 533 000 Taiwanese and 75 000 Norwegian adults. Acta Psychiatrica Scandinavica 133, 277–288. [DOI] [PubMed] [Google Scholar]
- Crosby A, Gfroerer J, Han B, Ortega L, Parks SE, 2011. Suicidal thoughts and behaviors among adults aged >_18 Years--United States, 2008–2009. US Department of Health and Human Services, Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Curtin SC, Warner M, Hedegaard H, 2016. Increase in suicide in the United States, 1999–2014. US Department of Health and Human Services, Centers for Disease Control and Prevention. [Google Scholar]
- Dahl RE, Puig-Antich J, Ryan ND, Nelson B, Dachille S, Cunningham SL, Trubnick L, Klepper TP, 1990. EEG sleep in adolescents with major depression: The role of suicidality and inpatient status. Journal of Affective Disorders 19, 63–75. [DOI] [PubMed] [Google Scholar]
- Denney JT, Rogers RG, Krueger PM, Wadsworth T, 2009. Adult suicide mortality in the United States: marital status, family size, socioeconomic status, and differences by sex. Social Science Quarterly 90, 1167–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodds KL, Miller CB, Kyle SD, Marshall NS, Gordon CJ, 2017. Heart rate variability in insomnia patients: a critical review of the literature. Sleep medicine reviews 33, 88–100. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J, 1994. Structured clinical interview for Axis I DSM-IV disorders. New York: Biometrics Research. [Google Scholar]
- Forkmann T, Meessen J, Teismann T, Sütterlin S, Gauggel S, Mainz V, 2016. Resting vagal tone is negatively associated with suicide ideation. Journal of Affective Disorders 194, 30–32. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK, 2017. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychological Bulletin 143, 187. [DOI] [PubMed] [Google Scholar]
- Glenn CR, Kleiman EM, Cha CB, Deming CA, Franklin JC, Nock MK, 2018. Understanding suicide risk within the Research Domain Criteria (RDoC) framework: A meta‐analytic review. Depression and Anxiety 35, 65–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetz RR, Wolk SI, Coplan JD, Ryan ND, Weissman MM, 2001. Premorbid polysomnographic signs in depressed adolescents: A reanalysis of EEG sleep after longitudinal follow-up in adulthood. Biological Psychiatry 49, 930–942. [DOI] [PubMed] [Google Scholar]
- Grant JE, 2007. Failing the 15-minute suicide watch: Guidelines to monitor inpatients. Current Psychiatry 6, 41–43. [Google Scholar]
- Gutierrez PM, Davidson CL, Friese AH, Forster JE, 2016. Physical activity, suicide risk factors, and suicidal ideation in a veteran sample. Suicide and Life‐Threatening Behavior 46, 284–292. [DOI] [PubMed] [Google Scholar]
- Hamilton M, 1986. The Hamilton rating scale for depression, Assessment of depression. Springer, pp. 143–152. [Google Scholar]
- Keshavan MS, Reynolds CF, Montrose D, Miewald J, Downs C, Sabo EM, 1994. Sleep and suicidality in psychotic patients. Acta Psychiatrica Scandinavica 89, 122–125. [DOI] [PubMed] [Google Scholar]
- Khandoker AH, Luthra V, Abouallaban Y, Saha S, Ahmed KI, Mostafa R, Chowdhury N, Jelinek HF, 2017. Predicting depressed patients with suicidal ideation from ECG recordings. Medical & Biological Engineering & Computing 55, 793–805. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Nock MK, 2018. Real-time assessment of suicidal thoughts and behaviors. Current Opinion in Psychology 22, 33–37. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Murphy SL, Xu J, Arias E, 2019. Deaths: Final data for 2017. National Vital Statistics Reports 68. [PubMed] [Google Scholar]
- Lemogne C, Thomas F, Consoli SM, Pannier B, Jégo B, Danchin N, 2011. Heart rate and completed suicide: evidence from the IPC cohort study. Psychosomatic Medicine 73, 731–736. [DOI] [PubMed] [Google Scholar]
- Littlewood DL, Kyle SD, Carter L-A, Peters S, Pratt D, Gooding P, 2019. Short sleep duration and poor sleep quality predict next-day suicidal ideation: an ecological momentary assessment study. Psychological Medicine 49, 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall C, McCall WV, 2012. Comparison of actigraphy with polysomnography and sleep logs in depressed insomniacs. Journal of Sleep Research 21, 122–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Nahshoni E, Aravot D, Aizenberg D, Sigler M, Zalsman G, Strasberg B, Imbar S, Adler E, Weizman A, 2004. Heart rate variability in patients with major depression. Psychosomatics 45, 129–134. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health, 2019. Suicide is a leading cause of death in the United Stats. Retrieved April 20, 2019, from https://www.nimh.nih.gov/health/statistics/suicide.shtml
- Sabo E, Reynolds ICF, Kupfer DJ, Berman S, 1991. Sleep, depression, and suicide. Psychiatry Research 36, 265–277. [DOI] [PubMed] [Google Scholar]
- Shaffer F, Ginsberg J, 2017. An overview of heart rate variability metrics and norms. Frontiers in Public Health 5, 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer F, McCraty R, Zerr CL, 2014. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Frontiers in Psychology 5, 1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepard DS, Gurewich D, Lwin AK, Reed GA Jr, Silverman MM, 2016. Suicide and suicidal attempts in the United States: costs and policy implications. Suicide and Life‐Threatening Behavior 46, 352–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibold J, Edwards E, Murray-Close D, Hudziak JJ, 2015. Physical activity, sadness, and suicidality in bullied US adolescents. Journal of the American Academy of Child & Adolescent Psychiatry 54, 808–815. [DOI] [PubMed] [Google Scholar]
- Simon TR, Powell KE, Swann AC, 2004. Involvement in physical activity and risk for nearly lethal suicide attempts. American Journal of Preventive Medicine 27, 310–315. [DOI] [PubMed] [Google Scholar]
- Singareddy R, Krishnamurthy VB, Vgontzas AN, Fern, ez-Mendoza J, Calhoun SL, Shaffer ML, Bixler EO, 2013. Subjective and objective sleep and self-harm behaviors in young children: A general population study. Psychiatry Research 209, 549–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taliaferro LA, Rienzo BA, Miller MD, Pigg RM Jr, Dodd VJ, 2008. High school youth and suicide risk: exploring protection afforded through physical activity and sport participation. Journal of School Health 78, 545–553. [DOI] [PubMed] [Google Scholar]
- Taliaferro LA, Rienzo BA, Pigg RM, Miller MD, Dodd VJ, 2009. Associations between physical activity and reduced rates of hopelessness, depression, and suicidal behavior among college students. Journal of American College Health 57, 427–436. [DOI] [PubMed] [Google Scholar]
- Tsypes A, James KM, Woody ML, Feurer C, Kudinova AY, Gibb BE, 2018. Resting respiratory sinus arrhythmia in suicide attempters. Psychophysiology 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Someren EJ, 2007. Improving actigraphic sleep estimates in insomnia and dementia: how many nights? Journal of Sleep Research 16, 269–275. [DOI] [PubMed] [Google Scholar]
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, 2007. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Annals of Internal Medicine 147, 573–577. [DOI] [PubMed] [Google Scholar]
- Wilson S, Argyropoulos S, 2005. Antidepressants and sleep. Drugs 65, 927–947. [DOI] [PubMed] [Google Scholar]
- Wilson ST, Chesin M, Fertuck E, Keilp J, Brodsky B, Mann JJ, Sönmez CC, Benjamin-Phillips C, Stanley B, 2016. Heart rate variability and suicidal behavior. Psychiatry Research 240, 241–247. [DOI] [PubMed] [Google Scholar]
- Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, Carli V, Höschl C, Barzilay R, Balazs J, 2016. Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry 3, 646–659. [DOI] [PubMed] [Google Scholar]


