What is Quality Improvement (QI)? Paul Batalden and Frank Davidoff, in 2008, described QI as “the combined and unceasing efforts of everyone—healthcare professionals, patients and their families, researchers, payers, planners and educators—to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development” [1]. The concept of QI intimately links front-line staff with a fundamental responsibility to improve the systems they work in. In essence, Quality Improvement asserts that everyone has two jobs: first, to do the job they were trained to do, and second to improve the system in which they do that job [2].
While this definition is recent, the application of formal QI methods to healthcare has been evolving over the past century [3], [4], [5]. Important historical eras, individuals and events which have influenced the evolution of Quality Improvement in healthcare is shown in Table 1. QI methodologies, originally used in industry, include frameworks such as the Plan-Do-Study-Act (PDSA), the Malcolm Baldridge model, Lean and Six-Sigma. All of these QI frameworks require adhering to an iterative, methodical process where the underlying system is systematically examined at the project outset. A number of different tools may be employed to understand variation in underlying performance. Typically, a detailed exploration of the underlying system, and thus an understanding of the drivers of variation in performance need to be made clear before solutions are generated. Interventions to address those performance gaps, which must not have been pre-determined, may evolve during the project and are tailored to the specific context of the clinical setting.
Table 1.
Important milestones in the evolution of QI in healthcare.
| Dates | Event Description | Importance |
|---|---|---|
| 1911 | Ernest Codman opens his “end results” hospital in Boston | Errors were reported and shared, with the intent of improving performance |
| 1920s–1940s | Walter Shewhart and W. Edwards Deming pioneer Quality Management within manufacturing | Applied foundational concepts of studying a system, understanding variation and understanding human behavior to improve performance |
| 1951 | Joint Commission established | Formal regulatory oversight of hospitals |
| 1966 | Avedis Donabedian publishes “Evaluating the Quality of Medical Care” | Established framework for evaluating Quality in healthcare including the concept of Structure-Process and Outcome Measures |
| 1980 | Toyota develops its Lean production system; Motorola develops Six-Sigma tools | Principles from these approaches to improvement are eventually widely adopted in healthcare |
| 1986 | The National Demonstration Project on Quality Improvement in Health Care (NDP) is launched | First modern, large-scale effort bringing together thought leaders and innovators in Healthcare Improvement |
| 1991 | Institute for Healthcare Improvement is established | IHI has been the leading organization promoting Quality Improvement in Health Care over the past 25 years |
| 1994 | Lucian Leape publishes “Error in Medicine” | Describes the prevalence and underlying drivers of medical error |
| 1998 | “To err is human” report published by the Institute of Medicine | Increased public attention brought to Quality and Safety within healthcare |
| 2006 | “Keystone study” published by Pronovost et al. | Establishes the importance of the standard use of checklists to improve patient safety; subsequently leads to recognition of the role of context in application of Quality Improvement interventions |
| 2015 | MACRA (Medicare access and CHIP reauthorization act) passed | Numerous incentives created to link payment for healthcare services to the Quality of care provided |
Infrastructures which formally support the adoption and application of these formal QI frameworks are now present in many large healthcare organizations within the United States [6]. While these methodologies have been widely adopted in American healthcare, they have shown variable success in improving system performance and patient outcomes in healthcare [7], [8], [9]. There are many common challenges to full, consistent implementation of sound QI methods across any healthcare organization: competing strategic priorities, inadequate leadership support, limited QI education, limited physician engagement, inappropriate focus on interventions, and lack of recognition for QI are among the challenges that organizations face [6], [10], [11]. Working to overcome these and other barriers in an expanding healthcare work-force is a challenge that healthcare organizations will continue to face in the years ahead.
Here, we describe the Mayo Clinic Quality Academy’s (MCQA) blended approach to application of QI methods across a diverse and complex healthcare organization.
1. The blended approach: an introductory toolkit for quality improvement
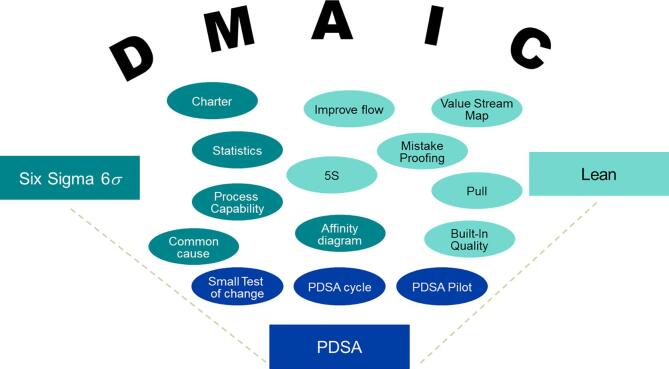
There are a variety of different tools used for quality improvement in healthcare. At Mayo Clinic, we view the “plan-do-study-act” (PDSA) cycle as the fundamental tool used in our quality improvement framework. Using this framework, a small test of change can identify a potential solution to a problem, and using appropriate techniques, scaled and improved to a larger level. In this “blended framework,” we view the tools of six sigma and lean as complementary ways of going from a PDSA cycle to a larger comprehensive quality project. We fit the larger project into the Define-Measure-Analyze-Improve-Control (DMAIC) framework from Six Sigma, though the phases of DMAIC this can be applied to lean and other projects (see Fig. 1.).
Fig. 1.
The Blended Approach To Quality Improvement.
1.1. “Just do it”
The most basic kind of quality improvement effort “just do it.” This is a simple, low risk local project where a problem can be identified and fixed by a small group of people who completely control that process. These are things like fixing a broken piece of equipment or eliminating a clearly unnecessary step in an isolated workflow. Empowering workers to feel that they can contribute to the quality of their work is critical to creating a “culture of quality,” and recognizing that not every improvement has to be a project helps ensure that quality improves continuously. In a “just do it” situation, however, there is a risk of not understanding the upstream and downstream effects that a change may have, so adequate understanding of the systems processes and global workflows remains important when deciding if an opportunity for improvement is really of the “just do it” variety. The most effective kind of “just do it” interventions may be seen as part of a larger project, where some low hanging fruit are identified as targets for short-cycle interventions and implemented before the larger project is completed. This is similar to a “Kaizen blitz” approach.
1.2. PDSA
The PDSA is a step up from the “just do it” mentality. In these projects, a structured planning approach is used to appropriately plan an intervention, test on a small level, and iteratively improve and enlarge the project. A tool or process could be piloted by an individual, studied, improved, adopted by a work unit, improved again, and rolled out to a larger department. PDSA cycles allow for more opportunities for studying some of the downstream impacts a change may have, and optimizing a process. More importantly, PDSA brings in change management principles, allowing for studying how to adapt and implement successful models of change from one area or pilot into other similar areas, studying the culture and workflow as it spreads throughout.
1.3. Lean
Lean is an approach to reduction of waste. The goal of Lean is to improve value as perceived by the customer (in healthcare, typically the patient) by recognizing those activities that do not add value and reducing or eliminating them. The most common example in healthcare is waiting and delays. Although there are certain wait time that are unavoidable (e.g. analytic time for laboratory tests), the amount of time spent in a exam room, hospital room or waiting room without any kind of provider is a known dissatisfier to patients and contributes little to their overall care. Lean projects identify which sort of wasteful activities like that can be reduced through serial process improvements, such as improving the flow of persons or materials throughout an emergency department to reduce the total “down time” a patient may have during an intense evaluation.
The aggressive elimination of waste in Lean involves attempting to understand what is key to a system and identifying where value is not being added. This may include steps where a process is redone or over-worked, or where a inadequate product or resource is delivered to a required step. Tools such as value stream mapping are used to understand where value is added, and where bottlenecks exist that can be eliminated to allow for efficient and timely delivery of a quality product.
5S is probably the best known example of a “lean” tool, though lean can be adopted without 5S (and to a certain extent, 5S can be implemented without a broader Lean approach). In 5S, a workplace is organized in such a way as to reduce inefficiency and waste. In healthcare, examples typically include stockrooms, laboratories and even procedure carts. The first “S” is “sorting,” going through the area and removing that which is truly not necessary. Items which are not needed make it harder to find those that are in an efficient way, and by removing them, work can be more effective. The second “S” is “set in order,” where items are rearranged to fit the workflows; commonly required tools are co-located to make them easier to find and quicker to gather together. The third S is “Shine,” where a workplace is clean and organized enough to make it obvious when something is out of place. This leads to the fourth “S,” “standardize,” where procedures are put in place to help ensure that the organizational schema is easy to follow. Visual guides may be implemented to make it clear what belongs where, checklists to ensure restocking follows the same protocol, and training materials to make sure all those who work in this space know how to optimally apply it. The final S “Sustain,” looks to move the first 4S’s into the organizational culture, encouraging workers to continuously find areas for improvement, and reassess if an area slips into disorder to restart the process.
Although typically thought of as a way of organizing physical space, 5S principles have been successfully applied to time in schedule-based projects, and to virtual space with one of the quality academy’s most successful offerings “take control of your e-mail,” a 5S approach to optimizing in box management. Thus, the principles can be applied to a broad array of situations where there is a gap in efficiency.
1.4. Six sigma
Six Sigma is traditionally associated with quality improvement, and has its roots in manufacturing. Unlike Lean, where the emphasis is on waste reduction and improving efficiency, Six Sigma targets defects and finds ways to reduce defects. Indeed, it gets its name from the target – that a defect should only occur at the sixth standard deviation (sigma), or 3.4 defects per million opportunities. This is equivalent to a 99.99966% rate of quality performance. Put in healthcare terms, this can seem daunting, but if we are to accept only a target of 99.9% quality, every day in the USA, this would work out to 11 babies being given to the wrong patient [12]. In 2008, transfusion fatalities due to mismatch operated at a 19.4 DMPO/6.1 sigma level [13]. Although the six sigma level may be more conceptual or aspirational for many areas in healthcare, in many more, it can and has been achieved.
Six sigma works via a five step process. In the first step, a problem is “defined.” Ensuring an adequate definition of the gap between the current state and an achievable future state informs all future steps in a six sigma project. Without a clear vision or criteria for success, a six sigma project cannot succeed. The define stage is summed up in the (perhaps apocryphal) quote from Yogi Berra “If you don’t know where you’re going, you’ll end up someplace else.” Tools often used in the “define” stage include stakeholder assessment, project charters, critical to quality trees, and aim statements.
The second step, “Measure,” emphasizes the statistical and scientific elements of Six Sigma. A thorough baseline evaluation of the present state to assess current functionality in a way that’s reliable and reproducible so that performance can be re-measured and re-analyzed as needed. The measure phase may include mapping a process, histograms, observations and check sheets.
In the third phase, “Analyze,” data from the measurement is reviewed to determine what driving the gap in quality identified in “define.” This emphasizes some statistical tools like control charts, correlation analysis and Pareto diagrams, but can also include more qualitative analytic tools like root cause analysis and cause and effect diagrams. From the analyze phase, drivers of the quality gap are identified and targeted for improvement.
The fourth phase, “Improve,” is where the improvements are actually developed and trialed. There are some standard improvements for specific project (e.g. some of the Lean toolkit if waste is identified as a driver, future state mapping and brainstorming to effectively crowdsource solutions), but often times, this ends up being a phase of iterative improvement, harkening back to the PDSA cycle. With appropriate measurement tools and analysis, however, these PDSA cycles can be more targeted for more complicated problems than a simple “just do it” problem could hope to achieve.
Once a project is successful, it moves into the “control” phase, where the team seeks to ensure gains aren’t lost by transitioning ownership to a group that will continue to function once the quality project team is disbanded, and appropriate guard rails are in place to prevent backsliding. This often includes such features as a measurement which can continue to be followed and an action plan if defects or adverse events exceed a certain threshold. Control phase methodology is often a stumbling point for otherwise successful projects, as sustaining the gains as processes and tools are transitioned into other operational owners is inherently difficult. A combination of tools to ensure ongoing compliance (e.g. checklists) and measures to follow.
All of these tools exist on a continuum, and tools from Six Sigma may be applied to smaller projects and vice versa. Also, although presented linearly, there is often a need to loop back to a prior step and cycle through again when problems are better understood. A culture that accepts and encourages continuous improvement is more important to effective QI work than any stream of steps or individual process.
2. Tuberculosis and quality improvement
Tuberculosis care is an area ripe for quality improvement initiatives. In any situation where patients, practitioners, guidelines and healthcare agencies attempt to simultaneously engage for a time-sensitive project, the complexity will inherently lend itself to inefficiency and errors. Individuals make such a system work through meticulous attention detail and follow up, but this comes at the expense of the valuable provider’s time and energy.
Many of the problems surrounding tuberculosis care are typical Lean problems. The processes followed by clinics and public health to enroll patients in tuberculosis treatment are paperwork-heavy, and can be a cause of extensive over- and re-processing, common targets for Lean initiatives. Another area which would be well suited to lean is mis-triage, where a patient may be referred to a tuberculosis clinic for active TB when they actually have latent TB, or vice versa. In either situation, matching the required resources to the task cannot be done efficiently a priori, and methodically studying the drivers to this kind of waste would be a perfect application of lean.
TB care also presents typical six sigma problems. In the context of patient care, loss to follow up, missed appointments and preventable drug toxicities are all “defects” in the Six Sigma sense of the word, and each are the end result of a complex series of processes and opportunities that can be defined, measured, analyzed, improved and ultimately controlled.
These are some typical examples of quality improvement work applied to this setting, but ultimately, effective QI in TB care will have to be driven by knowledgeable TB providers. In Japanese manufacturing, the term “get to Gemba” is used to describe the need for management or quality improvement personnel to walk the production line and understand the processes by which their products are made before they work on changing them. TB needs to have leaders educated in quality tools.
3. The Mayo Clinic Quality Academy
The Mayo Clinic Quality Academy (MCQA) was established in 2006 as a ‘grass-roots’ effort to support ongoing quality improvement activities in the institution. This effort was led by health systems engineering staff and a handful of Mayo physician and administrative leaders who had pursued external training in quality improvement (QI). MCQA’s functions fulfill the Education mission of our institution’s three shield mission (Education, Practice and Research), and reports to the Executive Dean of the Mayo Clinic College of Medicine and Sciences. MCQA’s primary mission is to develop core knowledge and capabilities in quality improvement (QI) and to build capacity within the Mayo Clinic staff to apply QI methods to address identified gaps in quality. In addition to providing support to individuals and teams engaged in QI, MCQA also leads institutionally directed strategic large-scale collaboratives to address Enterprise-wide quality deficiencies.
MCQA is staffed by 50 QA faculty, 4 quality improvement advisors with expertise in QI and 8 operational staff (operations manager and administrative assistants). Our faculty design curriculum, teach courses, coach and mentor teams engaged in QI. MCQA staff attend to the administrative needs of our various subgroups including an Education committee, Communications group, Mayo Clinic Quality Fellows Program, Curriculum Oversight Subcommittee and an Office of QI Scholarship. The MCQA staff are also responsible of coordinating and planning all QI related activities across all campuses including annual quality conferences, Lean collaborative team presentations and Quality grand rounds events among many other events to recognize and share QI efforts broadly.
The MCQA offers a broad range of services including a comprehensive curriculum composed of face-face and online courses, collaboratives, longitudinal certification programs, team coaching and mentoring, QI project review and faculty development offerings. This curriculum is reviewed periodically, based upon learner feedback, current knowledge about successes and failures of the applications of existing QI methods and practice needs as determined by the Practice Quality Subcommittee. Quality improvement training at all levels is designed to support two key components of Mayo Clinic’s strategic plan, 1) to deliver the highest-value, and most trusted care for our patients and 2) to achieve operational excellence by improving and maintaining efficiency, productivity, and quality (outcomes, safety, patient experience) in order to provide high quality, affordable outcomes at a low cost. Primary services offered by the MCQA include, the development and delivery of a broad-based QI curriculum, coaching and mentoring QI teams, consultation with work unit leaders on QI training needs, curation of training resources, tracking and monitoring QI training of staff.
MCQA faculty comprise physicians, advanced practice providers, nurses, allied health staff and administrative staff in areas that are involved in direct and indirect patient care. Faculty holds primary assignments in other areas of the institution, and have QI expertise. They have successfully trained and coached individuals and teams in quality improvement, resulting in measurable improvements in inter-professional staff engagement and empowerment, scholarship and improved clinical and financial outcomes. Outcome metrics include numbers of staff (trainees, physicians, allied health staff) who have taken courses through MCQA or who have achieved certification at the Bronze, Silver and Gold levels, periodic surveys of MCQF participants, and team-reported time, cost and FTE savings associated with interventions.
MCQA courses are drawn from existing frameworks in Six Sigma, Lean, PDSA and problem solving. A collaborative model of work unit based, inter-professional training is a successful model for teaching quality improvement to teams at Mayo Clinic. When an educational intervention is desired to aid work unit based quality improvement activities, QA provides consultative services and work unit based didactic teaching and coaching resources to these teams. Our collaboratives aim to engage health care teams that work together in practice and strive to address deficiencies in the quality or safety of health care. In these collaboratives, didactic coursework on specific QI tools and methods is coupled with their application in a quality improvement project using the DMAIC framework to address identified gaps in quality.
Several strategies are employed to engage and empower staff in quality improvement training. The Mayo Clinic Quality Fellows (MCQF) certification program is one of such strategies. This is a longitudinal certification program that certifies staff at escalating levels of QI competency (Bronze, Silver, and Gold) from novice through expert levels. MCQF certification is eligible to all staff at Mayo Clinic. At the Bronze level, staff learn the importance of quality improvement in their daily work, understand their role in recognizing and addressing gaps in quality and how these may impact patient care, recognize key components of quality including safety, outcomes and patient experience. The Silver level is focused on the application of QI tools and methods to eliminate quality deficiencies in practice. At the Gold level, participants demonstrate competencies in facilitating, coaching and leading project teams through process improvement, incorporating change management principles in the course of the project and leading the diffusion and dissemination of improvements throughout the practice.
MCQA arose organically in our institution in response to a growing recognition amongst staff of the value of quality improvement in advancing our daily work and ultimately ensuring delivery of high quality and safe patient care. The evolution of MCQA has resulted in continual refinement of our curricular content, delivery methods, mentorship and coaching capabilities and our recognition and reward activities. These experiences have yielded many lessons that would be of benefit to others seeking to institute similar programs or strategies. Key attributes of a successful educational QI program include:
-
•
Early senior leadership support to champion the quality movement and ensure adequate allocation of resources
-
•
Visible reward of staff and recognition of their QI accomplishments
-
•
Provision of opportunities for both Individual and team-based QI training
-
•
Celebration and promotion of a culture of quality improvement
-
•
Monitor and respond to results, both quantitative and qualitative
MCQA leadership continually works with institutional leaders and the Practice Quality Subcommittee to align curriculum development efforts with current quality initiatives and objectives. Working through MCQA faculty who have education and quality improvement expertise, faculty design and teach courses to equip Mayo Clinic staff with the necessary knowledge and skills to meet the needs of the both the patient and the practice.
4. Conclusion
Quality improvement is more traditionally associated with manufacturing and business due to its historical roots. Nonetheless, these same tools can and have been used to deliver better care at lower cost at the bedside. Educating clinicians in effective quality improvement techniques is critical to the future of healthcare. Our blended approach of quality improvement methodologies coupled with health care subject matter expertise has made the Mayo Clinic Quality Academy successful in this charge.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jctube.2020.100170.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Batalden P.B., Davidoff F. BMJ Publishing Group Ltd; 2007. What is “quality improvement” and how can it transform healthcare? [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nelson E.C., Godfrey M.M., Batalden P.B., Berry S.A., Bothe A.E., Jr., McKinley K.E. Clinical microsystems, part 1. The building blocks of health systems. Joint Commission J Qual Patient Saf. 2008;34(7):367–378. doi: 10.1016/s1553-7250(08)34047-1. [DOI] [PubMed] [Google Scholar]
- 3.Marjoua Y., Bozic K.J. Brief history of quality movement in US healthcare. Curr Rev Musculoskeletal Med. 2012;5(4):265–273. doi: 10.1007/s12178-012-9137-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parry G.J. A brief history of quality improvement. J Oncol Pract. 2014;10(3):196–199. doi: 10.1200/JOP.2014.001436. [DOI] [PubMed] [Google Scholar]
- 5.Chassin MR, O’Kane ME. History of the quality improvement movement. Toward Improving the Outcome of Pregnancy III; 2010. p. 2.
- 6.D’Andreamatteo A., Ianni L., Lega F., Sargiacomo M. Lean in healthcare: a comprehensive review. Health Policy. 2015;119(9):1197–1209. doi: 10.1016/j.healthpol.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Grimshaw J., McAuley L., Bero L., Grilli R., Oxman A., Ramsay C. Systematic reviews of the effectiveness of quality improvement strategies and programmes. BMJ Qual Saf. 2003;12(4):298–303. doi: 10.1136/qhc.12.4.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor M.J., McNicholas C., Nicolay C., Darzi A., Bell D., Reed J.E. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf. 2014;23(4):290–298. doi: 10.1136/bmjqs-2013-001862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ting H.H., Shojania K.G., Montori V.M., Bradley E.H. Quality improvement: science and action. Circulation. 2009;119(14):1962–1974. doi: 10.1161/CIRCULATIONAHA.108.768895. [DOI] [PubMed] [Google Scholar]
- 10.Dixon-Woods M., Martin G.P. Does quality improvement improve quality? Future Hosp J. 2016;3(3):191–194. doi: 10.7861/futurehosp.3-3-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson J.K., Sollecito W.A. Jones & Bartlett Learning; 2018. McLaughlin & Kaluzny's continuous quality improvement in health care. [Google Scholar]
- 12.Centers for Disease Control and Prevention. Births and Natality. Available from: https://www.cdc.gov/nchs/fastats/births.htm.
- 13.US Department of Health and Human Services office of the Assistant Secretary of Health. Report of the US Department of Health and Human Services. In: The 2009 national blood collection and utilization survey report. Washington, DC; 2011.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.