The Hospital/Health Care Incident Command System (HICS) provides the operational coordination needed for an institution to respond to disease outbreaks.1 Although some institutions may have used HICS to prepare for the Ebola outbreak of 2014 or other high-consequence infectious diseases (HCIDs), the coronavirus disease 2019 (COVID-19) pandemic has presented different challenges related to patient surge and to implementing system-wide operational adaptations.2 , 3 Herein, we describe some of the lessons learned through COVID-19 HICS activation at Mayo Clinic.
Institutional Preparedness for Disease Outbreaks
Although focus is often placed on the response to disease outbreaks, an institution’s readiness is based on the preparedness work done beforehand, including HCID and pandemic planning. In HCID planning, an institution prepares to care for a small number of patients who have a wide array of possible highly pathogenic infections, such as Ebola, smallpox, or Middle East Respiratory Syndrome. In contrast, pandemic planning involves preparing an institution to care for a large number of patients with one infectious disease.3
HCID Planning
Mayo Clinic has a categorical approach to HCID planning, with four response pathways created based on the operational needs of an institution to safely and effectively care for patients with a suspected HCID.3 Each site within our health system has the personal protective equipment (PPE) and trained personnel needed to care for patients with suspected HCIDs until a patient is transferred to a designated treatment facility. For example, our campus in Rochester, Minnesota, is the designated treatment facility for the Mayo Clinic Health System sites in the Midwest. HCID preparedness in Rochester includes an HCID treatment unit with an on-unit HCID laboratory as well as two sets of three-room HCID suites for PPE donning, PPE doffing, and patient care. A multidisciplinary HCID core team maintains PPE proficiency through quarterly training.
Pandemic Planning
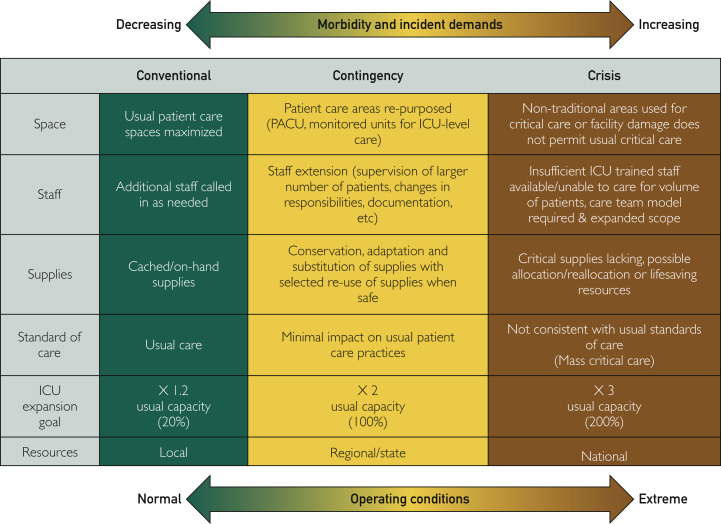
Pandemic planning involves preparing health care systems to care for a prolonged surge of patients. Although similar to planning for mass casualty scenarios that are geographically contained, pandemic planning includes the caveat that the incident is affecting the whole region, nation, and world. This situation complicates the regional capacity to assist with the surge and decreases the availability of key supplies (eg, PPE) because of increased global demand and supply chain disruption. Surge planning includes three basic components essential to delivering safe patient care: staff, space, and supplies (Figure 1 ). As an example, the ability to provide mechanical ventilation for a surge of patients involves more than just ventilator availability. Any limitation of critical care components—physicians, nurses, respiratory therapists, intensive care unit (ICU) beds, ventilator circuits, or pharmaceuticals—potentially limits the institution’s capacity to care for a surge of patients.4 , 5
Figure 1.
Framework for Surge Capacity Planning and the Continuum of Care. The framework spans conventional to contingency to crisis care.
Used with permission from Hick et al.4 ICU = intensive care unit.
As staff, space, and supply constraints progress during a pandemic, the surge response can escalate through the continuum of care: from conventional to contingency to crisis.4 Conventional care occurs when optimized routine processes are able to meet patient needs. Contingency care occurs when resources must be reallocated from areas of low priority to meet patient needs and provide the usual standard of care, albeit through nonroutine means. For example, if a surge outstrips ICU room capacity, a space contingency could be to use the postanesthesia care unit for critically ill patients. If maximizing contingency efforts are unable to meet patient needs with the usual standard of care, then the incident has transitioned to crisis care. Crisis care emphasizes the welfare of the population over the individual, concentrating resources to those most likely to benefit. If insufficient efforts are made in surge planning, an institution may unnecessarily find itself in crisis care.
In early planning for surge, modeling potential pandemic scenarios can help identify likely resource limitations. Mitigation strategies can be planned and tested in advance (eg, cross-training staff or stockpiling PPE).6 Business continuity planning can inform understanding of the prioritized functions, staff, space, and supplies that each work unit will need to perform critical functions. Such planning can help identify what resources can be reallocated during contingency care.7 Meticulous supply chain management through computerized systems gives an institution near real-time understanding of critical supply inventory and anticipated supply chain vulnerabilities.8 During a surge event, tiered plans must be implemented to meet the anticipated shortage of staff, space, and supplies brought on by the incident.
Shifting From an HCID Approach to a Pandemic Approach
Early in the COVID-19 outbreak, when known cases were either in China or linked epidemiologically to China, Mayo Clinic approached COVID-19 as an HCID. For the Mayo Clinic Health System in the Midwest, this included preparing front-line staff to safely isolate suspected imported cases and transferring patients requiring hospitalization to the Rochester campus. In Rochester, facilities updates for our HCID unit were expedited, and our HCID teams and laboratory were readied.
As the COVID-19 outbreak progressed, it became clear that 1) efficient human-to-human transmission was occurring and a global pandemic was inevitable, and 2) patients with COVID-19 could be safely cared for in usual hospital settings with adapted infection-prevention measures. At that point, we shifted preparedness efforts from an HCID approach to a pandemic approach. This included shifting staff to handle the increasing clinical and nonclinical workloads, identifying hospital and community space for surge capacity, and preparing conservation measures for critical supplies that could become scarce, such as PPE.
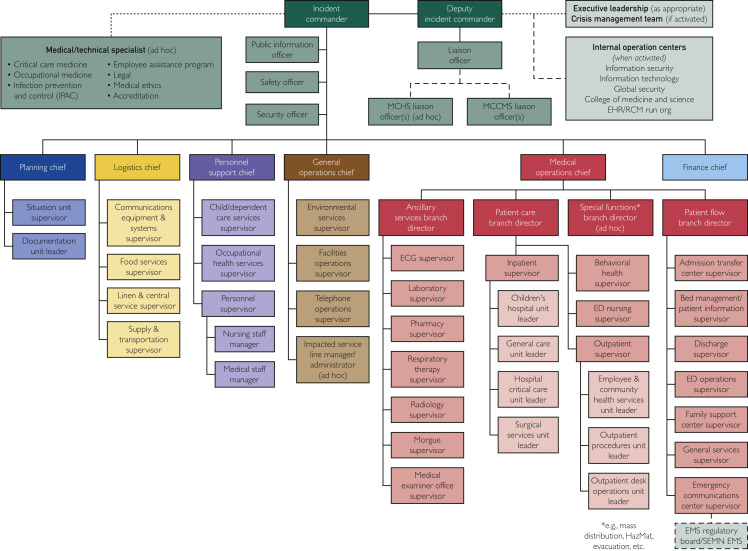
Activating HICS Early, Maintaining Discipline in Structure
The role of HICS in any rapidly evolving complex incident is to help manage the information, logistics, and operational needs in a systematic manner.1 Requests to HICS and finished work from HICS should flow through the incident commander, and work done in HICS should flow within the HICS chain of command (Figure 2 ) to ensure all work items are coordinated and accounted for. Although maintaining HICS activities requires immense personnel resources, HICS should be activated when the urgency, pace, or complexity of an incident overwhelms routine operations. Activating HICS early in the COVID-19 outbreak allowed Mayo Clinic to ready operations ahead of an anticipated surge. As pandemic work accelerated, it became increasingly important for HICS to maintain discipline and efficiency. It was imperative that section chiefs were updated on each pending work item within their section and that they presented these updates at the daily command and general staff HICS meetings.
Figure 2.
Organizational Structure of Hospital/Health Care Incident Command System.
(Used with permission of Mayo Foundation for Medical Education and Research.) ECG = electrocardiogram; ED = emergency department; EHR = electronic health record; EMS = emergency medical services; MCCMS = Mayo Clinic College of Medicine and Science; MCHS = Mayo Clinic Health System; RCM = revenue cycle management; SEMIN EMS = Southeast Minnesota Emergency Medical Services.
Integrating Clinical Practice Decision-Making and HICS Operations
For most short-term incidents requiring HICS activation, the goals are clear—return to usual operations. For longer complex events, such as the COVID-19 pandemic, novel clinical processes and decisions are rapidly needed. Although HICS is well-suited to making rapid, short-term changes to the clinical practice, it is not well-suited to creating sustained changes in clinical operations. Creation of a multidisciplinary COVID-19 practice group helped streamline the process of making clinical practice decisions extending beyond the initial response and allowed the group to begin thinking about operations of the clinic in the new normal, anticipated for at least the next several months. These ideas were advanced to HICS to operationalize the immediate steps needed to transition to this new mode of operations. Similarly, if HICS encountered areas of ambiguity, these issues were sent to the COVID-19 practice group for a clear directive. These integrated, but separate processes helped our organization meet the rapid pace of change of the pandemic and look to the longer-term response required for this event.
Planning for Crisis Care and Bereavement
Outbreaks can overwhelm resources even when contingency plans are in place. When this occurs, crisis care begins and poignant decisions regarding allocation of scarce resources become necessary, for example, which patients will receive mechanical ventilation and which patients will not.4 To ensure fairness and consistency, organizations must thoughtfully plan for crisis care.9 This planning includes having 1) thresholds to activate the triage teams and procedures to do so, 2) an ethical framework for resource allocation consistent with regional or statewide frameworks (where available), 3) a multidisciplinary triage team separate from the treatment teams, 4) processes to quickly provide the triage team with clinical data needed to make their resource allocation decisions, and 5) a means of transparent communication about crisis standards of care with staff, patients, and the broader community.
During the course of an outbreak, health care workers may become infected with and succumb to the pathogen, either by acquiring it in the community or at work. These events are tragic in their own right. Besides a normal grief response, the death of staff members may provoke a high degree of fear among their colleagues. At the most extreme, fear can result in workplace abandonment. A proactive and compassionate response can help alleviate both the personal injury and the potential for disrupted patient care. Health care organizations must have staff support and bereavement plans available to provide work unit supervisors with the resources needed to support their employees.
Returning to Routine Operations
After the initial HICS activities to ready an institution for a pandemic, organizations must transition to a maintenance mode of ongoing pandemic-related operations and to deactivate HICS. To do so, developed pandemic functions need a smooth transition plan to usual operational owners. The pandemic response likely created new processes that did not exist before the pandemic, and in those cases, new operational owners must be identified. As organizations transition to routine operations and decommission HICS, it is also important to catalogue the COVID-19 plans and processes to serve as a blueprint for future pandemics or other disasters.
Conclusion
The COVID-19 pandemic has been challenging for health care organizations globally. HICS offers a systematic approach to operationalizing the changes needed to address the pandemic. The lessons learned from the COVID-19 response can help better prepare organizations for future surge and pandemic events.
Acknowledgments
Editing, proofreading, and reference verification were provided by Scientific Publications, Mayo Clinic.
Footnotes
This supplement is sponsored by Mayo Clinic Foundation for Medical Education and Research and is authored by experts from multiple Departments and Divisions at Mayo Clinic.
Potential Competing Interests: The authors report no competing interests.
References
- 1.Banach D.B., Johnston B.L., Al-Zubeidi D. Outbreak response and incident management: SHEA guidance and resources for healthcare epidemiologists in United States acute-care hospitals. Infect Control Hosp Epidemiol. 2017;38(12):1393–1419. doi: 10.1017/ice.2017.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah A., Kashyap R., Tosh P., Sampathkumar P., O’Horo J.C. Guide to understanding the 2019 novel coronavirus. Mayo Clin Proc. 2020;95(4):646–652. doi: 10.1016/j.mayocp.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tosh P.K., Callies B.I. Sustaining hospital readiness for Ebola. Curr Treat Options Infect Dis. 2016;8(3):212–214. doi: 10.1007/s40506-016-0084-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hick J.L., Einav S., Hanfling D. Surge capacity principles: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(suppl 4):e1S–e16S. doi: 10.1378/chest.14-0733. [DOI] [PubMed] [Google Scholar]
- 5.Einav S., Hick J.L., Hanfling D. Surge capacity logistics: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(suppl 4):e17S–e43S. doi: 10.1378/chest.14-0734. [DOI] [PubMed] [Google Scholar]
- 6.Abramovich M.N., Hershey J.C., Callies B., Adalja A.A., Tosh P.K., Toner E.S. Hospital influenza pandemic stockpiling needs: a computer simulation. Am J Infect Control. 2017;45(3):272–277. doi: 10.1016/j.ajic.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 7.Tosh P.K., Feldman H., Christian M.D. Business and continuity of operations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(suppl 4):e103S–e117S. doi: 10.1378/chest.14-0739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tosh P.K., Burry L. Essential institutional supply chain management in the setting of COVID-19 pandemic. 2020. https://www.chestnet.org/Guidelines-and-Resources/Resources/Essential-Institutional-Supply-Chain-Management-in-the-Setting-of-COVID-19-Pandemic
- 9.Biddison L.D., Berkowitz K.A., Courtney B. Ethical considerations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(suppl 4):e145S–e155S. doi: 10.1378/chest.14-0742. [DOI] [PubMed] [Google Scholar]