Highlights
-
•
The progression of the COVID-19 pandemic was slowed by implemented social isolation measures and adaptation of the healthcare system.
-
•
Still, no effective treatments for severe lung complications are available for the most susceptible populations.
-
•
Optical theranostics methods can identify COVID-19 pulmonary manifestations and provide automated and real-time control of the treatment dosimetry.
-
•
Optical methods are flexible for combination with existing medical devices and drug repurposing protocols.
-
•
Implementation of reliable and safe theranostics methods requires strong collaboration among researchers, industry and medical institutions.
The containment of the COVID-19 pandemic has changed the management priorities of the healthcare system and led to the adoption of social isolation measures worldwide. Although these measures slowed the progress of the pandemic, no effective treatments for lung complications of COVID‑19 are available for the most susceptible populations including the elderly and individuals with preexisting health conditions. This letter aims to propose optical methods for theranostics of COVID-19 pulmonary infection and associated lung complications and foster research on protocol optimization using these methods.
Pulmonary manifestations of COVID-19 including pneumonia, acute respiratory distress syndrome (ARDS) and lymphadenopathy [1] are identified by using chest X-rays or computed tomography (CT) scans. These manifestations are currently managed through mechanical ventilation and critical care strategies, which are not useful to decrease the death rates of vulnerable groups. Recently ultrasound was proposed as a diagnostic method for COVID-19 infection [2], whereas discussed treatment options include currently approved antivirals and repurposed drugs [3]. However, diagnosis and therapeutic protocols are still not well established for in every medical institution due to the shortage of space and medical equipment capable of minimizing the contact with infected patients. This makes the early detection of lung complications especially difficult and, as a consequence, the COVID-19 infection becomes deadly for vulnerable individuals. Early detection can be achieved with optical methods, which allow molecular-sensitive and real-time analysis of biological tissues [4,5]. Optical methods are suitable for theranostics applications involving on-site treatment and control of its dosimetry based on the infection status. In addition, optical devices can be miniaturized and integrated with existing optical-medical equipment used to measure patient vital signs such as blood oxygenation, heart rate, respiratory rate and temperature.
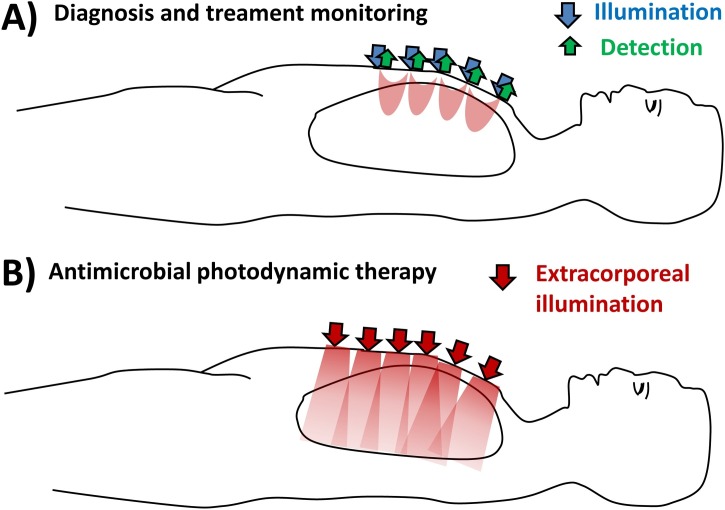
Early COVID-19 detection and treatment monitoring can be performed by using near-infrared (NIR) spectroscopy to monitor the pulmonary water content, blood oxygenation and heart rate [4,5]. Since blood oxygenation decreases in ARDS patients and the water content increases and in the pneumonia ones, NIR spectroscopy is especially useful in cases with these manifestations. Also, NIR spectroscopy has already been used for diagnosis and treatment monitoring in a variety of conditions in the brain, heart, breast, cervix, lung, skin, and others [6], which opens the opportunity for distant monitoring of patient diseases in addition to those related to COVID-19. Both diagnosis and treatment monitoring rely on devices with integrated classification models based on large datasets containing optical signals associated to the probed disorders [7] and can be performed together with other medical modalities including X-rays, CT scans, ultrasound images and magnetic resonance imaging (MRI) [8]. Other techniques such as gas in scattering media absorption spectroscopy (GASMAS) can be used to determine the oxygen gas concentration inside the lungs and identify respiratory complications [9]. Oxygenation signals of both NIR spectroscopy and GASMAS can be used to control the light and drug dosimetry for antimicrobial photodynamic therapy (aPDT) with extracorporeal illumination [10]. In this case, spectroscopic signals can be captured from reflectance or reemittance of red and NIR light [9,11] at the same time aPDT controls COVID-19 infections by activating photosensitizer-antibody conjugates targeting coronavirus structures (such as the RBD of the S1 subunit of their spike proteins, which binds to the cellular angiotensin-converting enzyme 2 (ACE2), or S2 subunits mediating the membrane fusion between the virus and infected cell). While most of the lung volume can be illuminated for optical treatments, their monitoring can be performed by probing the outer centimeters of the lung with light sources and detectors placed at multiple positions of the chest, as illustrated in the Fig. 1 below:
Fig. 1.
Geometries for A) optical diagnosis and treatment monitoring (e.g. NIR spectroscopy and GASMAS) and B) antimicrobial photodynamic therapy of lung infection.
The light and drug dosimetry of aPDT and drug repurposing/repositioning treatments can be adjusted in real-time according to the infection severity, oxygen availability and generated heating due to the light absorption in tissues. If systemic doses can be optically detected, drug repurposing therapies may be based on the feedback provided by the systemic levels of specific drugs instead of only relying on infection severity. Additional guidance on treatment monitoring and effectiveness can also be performed with existing methods such as ultrasound. Finally, microbial inactivation can be performed on tracheally intubated COVID‑19 patients by using ultraviolet-C (UV-C) tracheo‑bronchial irradiation treatment, especially in ARDS patients. Stawicki [12] proposes a protocol of repeated illumination cycles for short-term infection management by using diffusive optical fibers for light delivery. Proposed application times and UV-C power levels are based on previous microbial inactivation studies for SARS-CoV. UV-C can also be used with photosensitizer-antibody conjugates for both identification of infected lung areas and subsequent treatment. As for the other therapies discussed in this letter, eye and skin protection is necessary for the safety of every individual on the treatment room (e.g. treatment providers and patients on hospital isolation rooms). Radiation doses should not exceed the safety standards for light exposure, especially considering UV-C mutagenic effects.
With the discussed theranostics and treatment dosimetry applications in mind, optical methods can be used to monitor and treat patients from a distance. This ensures the safety of healthcare workers and helps overcoming the pandemic. Even though the current technology is still immature to be applied to control the virus spread, I would like to emphasize the potential of optical theranostics methods to detect and treat COVID-19 pulmonary manifestations, especially on vulnerable populations. Multiple opportunities arise from the flexibility of optical technologies to be automated, incorporated into medical tools (potentially integrated with existing devices), and combined to ultrasound and drug repurposing. To exploit these opportunities, the collaboration among researchers, industry and medical institutions is vital more than ever before.
Ethical approval
Not required.
Funding sources
No funding was received to conduct the research shown in the manuscript. Marcelo Saito Nogueira receives a scholarship from Science Foundation Ireland for his PhD candidate position at Tyndall National Institute/University College Cork.
Declaration of Competing Interest
No conflicts of interest to declare.
References
- 1.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30086-4. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peng Q.-Y., Wang X.-T., Zhang L.-N., Group CCCUS Findings of lung ultrasonography of novel corona virus pneumonia during the 2019--2020 epidemic. Intensive Care Med. 2020;1 doi: 10.1007/s00134-020-05996-6. Nature Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosa S.G.V., Santos W.C. Clinical trials on drug repositioning for COVID-19 treatment. Rev Panam Salud Pública. 2020;44 doi: 10.26633/RPSP.2020.40. Pan American Health Organization. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nogueira M.S. Biophotonic telemedicine for disease diagnosis and monitoring during pandemics: overcoming COVID-19 and shaping the future of healthcare. Photodiagnosis Photodyn. Ther. 2020 doi: 10.1016/j.pdpdt.2020.101836. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saito Nogueira M. Biophotonics for pandemic control: large-area infection monitoring and microbial inactivation of COVID-19. Photodiagnosis Photodyn. Ther. 2020 doi: 10.1016/j.pdpdt.2020.101823. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sakudo A. Near-infrared spectroscopy for medical applications: current status and future perspectives. Clin. Chim. Acta. 2016;455:181–188. doi: 10.1016/j.cca.2016.02.009. Elsevier. [DOI] [PubMed] [Google Scholar]
- 7.Carvalho L.Fdas Ce S., Saito Nogueira M. Optical techniques for fast screening--towards prevention of the coronavirus COVID-19 outbreak. Photodiagnosis Photodyn. Ther. 2020 doi: 10.1016/j.pdpdt.2020.101765. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Güneyli S., Atçeken Z., Dougan H., Altinmakas E., Atasoy K.Ç. Radiological approach to COVID-19 pneumonia with an emphasis on chest CT. Diagn. Interv. Radiol. 2020 doi: 10.5152/dir.2020.20260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Svanberg E.K., Lundin P., Larsson M., Åkeson J., Svanberg E.K., Svanberg S. Diode laser spectroscopy for noninvasive monitoring of oxygen in the lungs of newborn infants. Pediatr Res. Nature Publishing Group. 2016;79:621–628. doi: 10.1038/pr.2015.267. [DOI] [PubMed] [Google Scholar]
- 10.Geralde M.C., Leite I.S., Inada N.M., Salina A.C.G., Medeiros A.I., Kuebler W.M. Pneumonia treatment by photodynamic therapy with extracorporeal illumination-an experimental model. Physiol. Rep. 2017;5 doi: 10.14814/phy2.13190. Wiley Online Library. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinti P., Tachtsidis I., Hamilton A., Hirsch J., Aichelburg C., Gilbert S. The present and future use of functional near-infrared spectroscopy (fNIRS) for cognitive neuroscience. Ann. N. Y. Acad. Sci. 2018 doi: 10.1111/nyas.13948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stawicki S.P. 2020. Could Tracheo-bronchial Ultraviolet C Irradiation Be a Valuable Adjunct to the Management of Severe COVID-19 Pulmonary Infections? [Google Scholar]