Abstract
In this study, we performed a single‐centered study of 307 severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infected patients. It was found that co‐infection of SARS‐CoV‐2 and influenza virus was common during COVID‐19 outbreak. And patients coinfected with SARS‐CoV‐2 and influenza B virus have a higher risk of developing poor outcomes so a detection of both viruses was recommended during COVID‐19 outbreak.
Keywords: co‐infection, influenza A virus, influenza B virus, SARS‐CoV‐2 infection
1. INTRODUCTION
Novel coronavirus disease 2019 (COVID‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) is becoming a serious global public health crisis. 1 Thus far, more than 5 000 000 people have been diagnosed with COVID‐19 worldwide with over 330 000 deaths. 2 Coincidently, influenza viral infection were also prevalent during this period. In previous studies, co‐infection of influenza virus has been reported in a small number of patients with Middle East respiratory syndrome coronavirus, while the risk of increased or decreased severity of diseases in these co‐infectious patients was still controversial. 3 Moreover, it has been found that influenza A virus positive will increase diagnostic difficulties in SARS‐CoV‐2 infected patients. 4 And influenza viral positive patients were normally ruled out for testing for SARS‐CoV‐2 in China, who may become SARS‐CoV‐2 shedder if the co‐infection did occur. Therefore, it is crucial to investigate the clinical features and impact of co‐infection on COVID‐19 patients.
2. METHODS
2.1. Study population
A single‐centered retrospective study was performed in Tongji hospital (Wuhan, China) between 12 January and 21 February 2020 during the COVID‐19 outbreak. SARS‐CoV‐2 infection was confirmed by viral nucleotide positive in quantitative reverse transcription‐polymerase chain reaction and influenza virus infection was diagnosed by influenza virus immunoglobulin M antibody positive in serum. According to test results, patients were grouped into three group, including SARS‐CoV‐2 single positive, co‐infection with influenza A virus or co‐infection with influenza B virus.
2.2. Statistical analyses
Continuous variables were compared using analysis of variance or the Kruskal‐Wallis test, as appropriate. Categorical variables were assessed using Pearson's χ 2 test or Fisher's exact test, as appropriate. All significance tests were two‐tailed, and P ≤ .05 were considered statistically significant different. The results were analyzed using SPSS for Windows, version 26.0 (IBM Corp, Armonk, NY).
3. RESULTS
A total of 307 patients were diagnosed as SARS‐CoV‐2 positive during the outbreak (Figure 1A). Unexpectedly, there were only 42.7% (131) of SARS‐CoV‐2 single positive patients (Figure 1B). Most of the SARS‐CoV‐2 infected patients were also positive for influenza viruses, including influenza A (49.8%) and influenza B (7.5%), taking up 57.3% (176/307) in total (Figure 1A,B). Notably, early patients with COVID‐19 were almost all coinfected with influenza B virus while influenza A virus infection has become prominent in the co‐infection patients since 28 January onwards (Figure 1A), which indicated that the two types of influenza viruses appeared a competing relationship.
Figure 1.
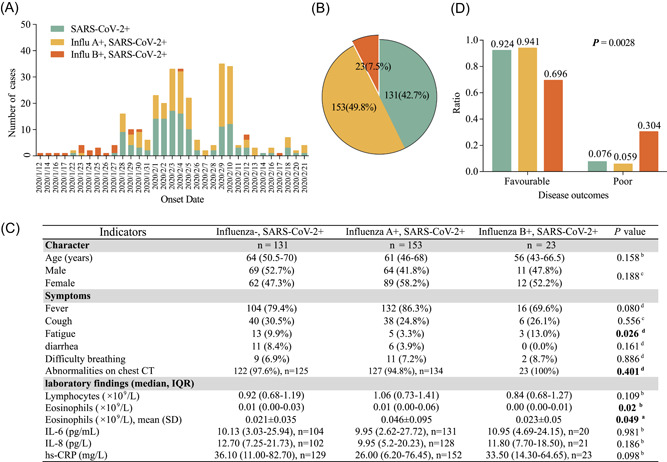
Co‐infection of SARS‐CoV‐2 and influenza viruses among patients. A, Records of daily new cases in a single‐centered study at Tongji hospital (Wuhan, China) from 12 January to 21 February 2020. Flu A: influenza type A virus; Flu B: influenza type B virus. Patients were grouped into SARS‐CoV‐2 single positive (green color), co‐infection with influenza A virus (yellow color) or co‐infection with influenza B virus (red color). B, Number of cases and percentage of each group. C, Character, clinical symptoms and laboratory comparison of patients among these three groups. Continuous variables were described as median and interquartile range (IQR) or mean and standard deviation (SD) and differences were assessed using analysis of variance (ANOVA) or the Kruskal‐Wallis test. Categorical variables were expressed as number (%) and differences between groups were assessed using Pearson's χ 2 test or Fisher's exact test. A, ANOVA; B, the Kruskal‐Wallis test; C, Pearson's χ 2 test; D, Fisher's exact test. P < .05 was bold. n = 131, 153 or 23 individually unless indicated. D, Disease outcomes for patients among three groups. Favorable means disease alleviated or recovered; poor means disease aggravated with certain deaths. The differences between groups were assessed using Pearson's χ 2 test or Fisher's exact test. Hs‐CRP, hypersensitive C‐reactive protein
To uncovered the clinical risk of this co‐infection, clinical features, laboratory findings and patient outcomes among different groups were analyzed. In general, there was no difference in age, gender or severity of illness at the time of admission. Also, there were no significant differences in heart, liver,kidney function and coagulation function, and inflammatory mediators among three groups (Figure 1C and Table S1). Most patients had typical COVID‐19 symptoms including fever and cough regardless co‐infection or not, which were also similar to influenza symptoms. However, patients coinfected with SARS‐CoV‐2 and influenza B virus are more likely to have fatigue (13%), abnormalities on chest computed tomography (CT) (100%) or decreased lymphocytes (0.84, 0.68‐1.27) and eosinophil (0.00, 0.00‐0.01), indicating a more severe disease. In contrast, patients coinfected with SARS‐CoV‐2 and influenza A virus tended to develop lighter signs of disease, as evidenced by a lower frequency of abnormalities on chest CT (94.8%) or higher levels of lymphocytes (1.06, 0.73‐1.41) and eosinophil (0.01, 0.00‐0.06) (Figure 1C). Remarkably, although all patients were administrated with similar treatment during hospitalization, patients who were coinfected with influenza B virus have a higher rate of presenting poor prognosis (30.4%) compared with SARS‐CoV‐2 single positive patients (7.6%) or influenza A virus coinfected patients (5.9%) (Figure 1D).
4. DISCUSSION
Our study indicated that co‐infection of SARS‐CoV‐2 and influenza viruses is highly prevalent (Influenza A: 49.8% and Influenza B: 7.5%) during the early time of COVID‐19 outbreak in Wuhan (12 January‐21 February 2020), which is significantly different co‐infection rates with Influenza A (0.9%) and Influenza B (0%) during a different time period (3‐25th March) in the recently published study in JAMA 5 and the data (Influenza infection: 0.5%, 10 March‐10 May 2020) from Ozaras et.al 6 published in Journal of Medicine Virology. The difference might be caused by some underlying factors. On one hand, circulation of respiratory viruses differs by geographical region and this may change as COVID‐19 epidemic continues as we exit out of the classical influenza season. Moreover, we have seen a dramatic decline on the circulating respiratory viruses, likely due to the impact of social distancing measures on respiratory virus transmission. 7 Additionally, consistent with the results from Hashemi, et.al and Ozaras et.al, 6 , 8 the clinical manifestations in patients coinfected SARS‐CoV‐2 with influenza present similar symptoms with single SARS‐CoV‐2 infection, which further indicates that timely influenza virus detection in patients with COVID‐19 is necessary so as to distinguish other respiratory pathogen infection and take appropriate treatment measures earlier. Notably, it was found that patients coinfected with SARS‐CoV‐2 and influenza B virus were more likely to develop into severe‐type illness compared with those coinfected with influenza A virus and single SARS‐CoV‐2 infection. More importantly, our study revealed that the type of influenza virus is associated with different clinical outcomes, implying antiflu drug may be used together to these coinfected patients with COVID‐19 and further verifying the fact that COVID‐19 has a lower mortality rate in areas with high flu vaccination rates. 9 However, we should be cautious to interpret the results because influenza virus B was dominant in the early time instead of influenza virus A, which may result in a longer duration of illness in patients coinfected with SARS‐CoV‐2 and influenza B virus. The limitation of our study is that when analyzing the factors associated with prognosis in patients with COVID‐19, we fail to adjust confounding factors, such as age, comorbidities and severity of illness considering that there was no statistical difference in the basic characteristics among these three groups. Second, the sample size of this study still needs to be further enlarged to make the results more convincing. In conclusion, our study provided important information on co‐infection of SARS‐CoV‐2 and influenza viruses and a detection of other respiratory pathogen was strongly recommended, which may have profound impact on the diagnosis and therapeutics for patients with COVID‐19.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
HY, XR, and MZ collected the epidemiological and clinical data. JT, JS, and MZ contributed to the statistical analysis. HY, YD, and JS drafted the origin manuscript. PZ, LX, HL, JS, YD, and XR revised the final manuscript. All authors contributed to data acquisition, data analysis, or data interpretation, and reviewed and approved the final version.
Supporting information
Supporting information
ACKNOWLEDGMENTS
The authors thank all the medical staff members involved in treating patients with COVID‐19 on the front line. This study was supported by SARS‐CoV‐2 Pneumonia Emergency Technology Public Relations Project [grants 2020FCA009 and 2020FCA026]; National Natural Science Foundation of China (grants 81974456).
Yue H, Zhang M, Xing L, et al. The epidemiology and clinical characteristics of co‐infection of SARS‐CoV‐2 and influenza viruses in patients during COVID‐19 outbreak. J Med Virol. 2020;92:2870–2873. 10.1002/jmv.26163
Huihui Yue, Xiaoling Rao, Hong Liu, Jianbo Tian, Peng Zhou, Yan Deng, and Jin Shang contributed equally to this work.
Contributor Information
Xiaoling Rao, Email: nkrxl@163.com.
Hong Liu, Email: 419641721@qq.com.
Jianbo Tian, Email: tianjianbo1992@126.com.
Peng Zhou, Email: peng.zhou@wh.iov.cn.
Jin Shang, Email: 15972949829@163.com.
REFERENCES
- 1. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270‐273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. https://coronavirus.jhu.edu/map.html
- 3. Alfaraj SH, Al‐Tawfiq JA, Alzahrani NA, Altwaijri TA, Memish ZA. The impact of co‐infection of influenza A virus on the severity of Middle East respiratory syndrome coronavirus. J Infect. 2017;74:521‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu XJ, Cai Y, Huang X, et al. Co‐infection with SARS‐CoV‐2 and influenza A virus in patient with pneumonia, China. Emerg Infect Dis. 2020;26(6):1324‐1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim D, Quinn J, Pinsky B, Shah NH, Brown I. Rates of co‐infection between SARS‐CoV‐2 and other respiratory pathogens. JAMA. 2020:e206266. 10.1001/jama.2020.6266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ozaras R, Cirpin R, Duran A, et al. Influenza and COVID‐19 co‐infection: report of 6 cases and review of the literature. J Med Virol. 2020. 10.1002/jmv.26125 [DOI] [PubMed] [Google Scholar]
- 7. Sakamoto H, Ishikane M, Ueda P. Seasonal influenza activity during the SARS‐CoV‐2 outbreak in Japan. JAMA. 2020:e206173. 10.1001/jama.2020.6173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hashemi SA, Safamanesh S, Ghafouri M, et al. Co‐infection with COVID‐19 and influenza A virus in two died patients with acute respiratory syndrome, Bojnurd, Iran. J Med Virol. 2020. 10.1002/jmv.26014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marín‐Hernández D, Schwartz RE, Nixon DF. Epidemiological evidence for association between higher influenza vaccine uptake in the elderly and lower COVID‐19 deaths in Italy. J Med Virol. 2020. 10.1002/jmv.26120 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


