Abstract
Allocation of limited resources in pandemics begs for ethical guidance. The issue of ventilator allocation in pandemics has been reviewed by many medical ethicists, but as localities activate crisis standards of care, and health care workers are infected from patient exposure, the decision to pursue cardiopulmonary resuscitation (CPR) must also be examined to better balance the increased risks to healthcare personnel with the very low resuscitation rates of patients infected with coronavirus disease 2019 (COVID‐19). A crisis standard of care that is equitable, transparent, and mindful of both human and physical resources will lessen the impact on society in this era of COVID‐19. This paper builds on previous work of ventilator allocation in pandemic crises to propose a literature‐based, justice‐informed ethical framework for selecting treatment options for CPR. The pandemic affects regions differently over time, so these suggested guidelines may require adaptation to local practice variations.
Keywords: COVID‐19, CPR, Ethics, pandemic, resource constraints, resuscitation, SOFA, ventilator‐allocation
1. INTRODUCTION
In 2020, the World Health Organization declared a pandemic of coronavirus disease 2019 (COVID‐19), caused by the SARS‐CoV‐2 virus. 1 At the time of this writing, there have been 6,089,705 confirmed cases and 369,651 deaths worldwide, with 1,770,384 cases and 103,781 deaths occurring in the United States. 2 As the virus has spread throughout the world, health systems in numerous areas (eg, in Italy, Spain, Wuhan, and New York City) have been overwhelmed with crowded inpatient and critical care units and lack of respiratory support equipment, especially ventilators. Currently, there is no vaccination or scientifically established pharmacologic treatment for the infection. COVID‐19 causes a wide spectrum of illness, from asymptomatic infections and mild respiratory or gastrointestinal illnesses to pneumonia, acute respiratory distress syndrome, severe sepsis, myocarditis, congestive heart failure, and cardiac arrest.
In addition to pulmonary complications of COVID‐19, acute cardiovascular complications appear to be significant sequelae of infection. In general, cardiovascular decompensation may be an end‐stage manifestation of sepsis, primary respiratory failure, or primary cardiac etiology. Proposed mechanisms for cardiac arrest related to COVID‐19 include acute hypoxemic respiratory failure, myocarditis, malignant tachydysrhythmia, coronary plaque instability (ie, type 1 myocardial infarction) secondary to inflammation, 3 stress‐induced cardiomyopathy, or coagulopathy. 4 In the 2003 SARS‐coronavirus epidemic, other suspected mechanisms of sudden death included acute decompensated heart failure from catecholamine excess and even the mild physiologic stress related to defecation. 5 COVID‐19 patients with myocardial injury have a much higher rate of mortality (51%) versus those without myocardial injury (4.5%). 6 Emergency physicians rarely know the COVID‐19 status of patients in the emergency department (ED) who experience cardiac arrest and each patient should be treated as a possible case.
Patients who decompensate to cardiac arrest and undergo cardiopulmonary resuscitation (CPR) represent a very high‐risk group for transmission of the SARS‐CoV‐2 virus to healthcare workers. Aerosolization of SARS‐CoV‐2, especially during intubation or chest compressions is an ongoing area of investigation and a focus of infection control guidance. 7 Infections in healthcare workers can impair the workforce of an ED and hospital, putting the community at greater risk of worse health outcomes. Infected healthcare workers can also unwittingly spread the infection to other patients during an asymptomatic prodrome, active infection, and potentially through viral shedding after recovery. 4
Emergency physicians are often tasked with resuscitating patients who suffer cardiac arrest and the COVID‐19 pandemic may require modifying typical approaches to CPR. Even in environments with adequate resources prior to the pandemic, the mortality for out‐of‐hospital cardiac arrest in the United States was high (≈90%) 8 and still very high (70%–80%) when the arrest occurs in the hospital. 9 Cardiac arrest with COVID‐19 patients is extremely lethal with a poor outcome in >99% of patients, making the benefit‐to‐patient/risk‐to‐healthcare‐team ratio even more stark. 10 Resource constraints coupled with a high volume of COVID‐19 patients may force emergency providers to make difficult decisions. Because of the special risks to the healthcare facilities and individual providers by COVID‐19, health care providers must be provided with evidence‐based guidance in making decisions about attempted resuscitation of patients. Prolonged high‐risk procedures such as CPR may result in transmission of the virus to poorly protected personnel, especially with critical shortages of high‐efficiency particulate air (HEPA) filters for intubation and appropriate personal protective equipment (PPE).
Multiple states have recognized the need for civil liability relief for physicians in catastrophic health emergency proclamations leading to Crisis Standards of Care. 11 , 12 , 13 The American College of Emergency Physicians, through its Disaster Preparedness and Response Committee has defined “crisis care” as, “what a reasonable practitioner would do (and want for himself and his loved ones), given the limited resources at hand.” 14 The interim guidance by the American Heart Association (AHA) has recommended that “health care systems consider policies to guide front‐line providers in determining the appropriateness of starting and terminating CPR, taking into account COVID‐19 status, comorbidities, and severity of illness to estimate the likelihood of survival.” 15 This paper seeks to inform the practicing emergency physician of ethical considerations while offering a potential framework for selective CPR. This framework is based on patient‐specific criteria for selective resuscitation with an adaptable treatment algorithm.
2. POLICY AND ETHICAL CONSIDERATIONS DURING THE COVID‐19 PANDEMIC
Multiple treatment changes that have been advocated in this pandemic are expert‐opinion based and any guidelines thus far proposed will likely continue to evolve. The sequential organ failure assessment (SOFA) score is part of proposed guidelines for ethical ventilator allocation during a public health emergency. 16 Multiple states have draft guidelines published online on resource allocation of ventilators, but there are sparse data on the efficacy of these guidelines. 17 , 18 , 19 During the 2009 H1N1 influenza pandemic, a hospital in the United Kingdom found that ventilator guidelines may have led to overtriage and withdrawal of ventilator support, but H1N1 influenza affected the young more heavily than the current COVID‐19 pandemic. 20 The ventilator allocation guidelines have the benefit of a committee that can review the data, age, and course of the patient to decide whether to continue therapy or withdraw and reallocate the ventilator. In the resuscitation bay, clinical‐based risk‐stratification metrics can provide a starting base for which resuscitations of the adult patient are the most likely to succeed. Practicing emergency physicians do not have the luxury of time or a committee at bedside during CPR and must be able to make a rapid bedside decision that weighs the odds of benefit to the patient with the risks to their team and health system.
The medical ethical decisionmaking process involves the concepts of non‐maleficence, beneficence, patient autonomy, along with hope and distributive justice. 21 The emergency physician must consider five specific components: duty to care, duty to steward resources (that takes into account the need for a ventilator and potential exposure to the health care providers), duty to plan (multiple states have planning algorithms for ventilator allocation), distributive justice (avoiding socioeconomic considerations), and transparency (providing intelligible information to all involved). Other ethical considerations described have included accountability, proportionality, solidarity, reciprocity, utility, fairness, consistency, and veracity. 22 The following sections of the paper discuss existing and proposed policy guidelines with careful exploration of the challenging ethical questions facing emergency providers.
3. PROPOSED CRITERIA FOR ATTEMPTING RESUSCITATION
Our proposed guidelines may be described as a justice‐informed utilitarian framework that provides the greatest good to the largest number of potentially healthy patient‐years while also giving everyone at least a chance. Any guidelines for limiting patient treatment to a potentially life‐saving intervention require significant scrutiny and should only be used in dire circumstances. Physicians must exercise their best clinical judgment in how to proceed with each individual patient, as their COVID‐19 status may be unknown. These guidelines are not ideal for out‐of‐hospital patients, because their COVID‐status is usually unknown, and hospital labs can help inform the decisionmaking criteria.
For the practicing clinician, the decision to cease CPR efforts is difficult to make and can create even more distress when prolonging largely futile efforts may further expose the medical team to SARS‐CoV‐2 viral particles despite adequate PPE. 23 Informed guidance is often sought, although not frequently available, especially in emergent situations. Deciding on resuscitation length based on age alone may not be fair or ethical, as elderly patients may be more fit or functionally independent than younger patients with multiple comorbidities. Subjective evaluations of a patient's quality of life are fraught with potential for discrimination, especially against the chronically disabled. Discussing the critical nature of the patient with their power‐of‐attorney could resolve much anxiety about initiating CPR as they may agree to consider palliative care for the unstable COVID‐19 patient. University of Pennylvania legal scholars have recently recommended, in the present crisis that 24 :
Attending physicians are not obligated to offer or to provide CPR if resuscitative treatment would be medically inappropriate, even at the request of a patient or legally authorized representative.
If the attending physician determines that CPR is not medically appropriate, they should solicit the independent review of a second attending physician not involved in the patient's care.
Physicians who decide not to offer CPR should inform the patient or legally authorized representative of this decision and rationale and assure the patient that all other forms of indicated care will continue. Assent should be sought but is not required.
The ethical allocation of scarce medical resources may take into consideration workers who perform “essential social functions,” as is the case in Michigan but this may not be true in all states. 13 “Essential” workers specifically for this pandemic include emergency physicians, hospitalists, intensivists, non‐physician practitioners and nurses treating COVID‐19 patients, mental health professionals, first responders and public health scientists. 25 Military, energy grid and telecommunication personnel are also deemed critical for the ongoing functioning of society. Prioritizing the resuscitation of “essential” workers may be useful when the illness recovery period is shorter than the pandemic length and they could contribute to ongoing mitigation efforts. However, the definition of “essential” varies between states and segments of society and will need further discussion that is beyond the scope of this paper.
4. UNACCEPTABLE CRITERIA FOR RESUSCITATION ATTEMPTS
Michigan has helped define criteria that are ethically unacceptable to consider when allocating ventilators to patients. 13 , 17 Similarly, health care personnel should not use these characteristics in deciding whom to attempt cardiac arrest resuscitation on due to their inherent lack of fairness and potential for abuse or discrimination.
Social characteristics including ethnicity, gender, national origin, sexual orientation, religious affiliation, and disabilities unrelated to immediate medical prognosis.
Social worth including employment status, training or education‐level, social standing, personal or familial relationships, belief systems, political affiliations, and ability to pay currently or in the future.
The option of lottery for ventilator allocation within subgroups of populations such as age or comorbidities does not directly apply to resuscitation in an ED. On admission after resuscitation, critical and palliative care teams can apply definable metrics that can help provide estimations of prognosis and help with inpatient risk stratification. Unfortunately, this option is unavailable in most EDs within a reasonable timeframe.
5. ANTICIPATING THE DECOMPENSATION OF PATIENTS IN THE COVID‐19 ERA
The Ontario Health Plan for an Influenza Pandemic first described in 2006 a critical care triage tool based in part on the SOFA score, which takes into account clinical measures of functioning in key organs and systems: pulmonary, hematologic, hepatic, cardiac, neurologic, and renal. 26 A perfect SOFA score (0) indicates normal function in all 6 categories. As the score increases due to dysfunction, the risk of acute mortality also increases, with the worst possible score of 24 representing significant impairment in all 6 systems. If the physician must respond to a sudden arrest in the ED, they should attempt to enlist a colleague to calculate the SOFA score based on the electronic medical record to help with risk‐stratification and inform the need to provide more than a few minutes of resuscitation. Currently in development are criteria for predicting decompensation in the ED, although COVID‐19 patients were not included in the study population. 27
The largest limitation of the SOFA score is the need to have the lab results available to calculate the score. Using the electronic medical record to find the most recent lab results may help expedite the decision, although labs from the acute presentation are ideal. Other prognostic scores considered include the systemic inflammatory response syndrome (SIRS), quick SOFA (qSOFA), modified SOFA (mSOFA), and Acute Physiology and Chronic Health Evaluation (APACHE II). SIRS and qSOFA, while much quicker to calculate, suffer from worse prognostic accuracy as compared to SOFA. 28 mSOFA is simpler than SOFA but still requires blood testing. APACHE II can help determine the admission mortality risk as well but requires lab work, includes age as a factor, and has not been as well‐cited by crisis‐guidance literature. 29 The CRASS formula has been helpful in predicting hospital discharge of patients who have suffered an out‐of‐hospital cardiac arrest and awaits further adoption and comparison to the more studied SOFA score as the pandemic progresses. 30 In the ED, patients often decompensate before the laboratory results needed for the SOFA score and in these cases, a second, non‐treating physician consultation is advised.
5.1. Step 1—Highl Lethal Risk Factors
CPR may be considered medically inappropriate, especially in conditions of crisis standards of care, in patients with very high probability of death. New York State has defined a list of criteria loosely based on the exclusion criteria from the 2008 Ontario Health Plan for an Influenza Pandemic clinical ventilator allocation protocol and a concept paper from Hick and O'Laughlin. 31
If the patient has a condition on the highly lethal risk factor list and is acutely declining, involve an independent review by a second clinician or palliative consult to consider comfort care. 24 , 25 These are the patients with the highest probability of immediate or near‐immediate death even with CPR and mechanical ventilation. In crisis‐level constraints, the risks of infection of the health care team greatly outweighs the small chance of benefit to a patient who has highly lethal risk factors and so the physician may consider a limited resuscitation effort, if any. Additionally, patients who have had an unwitnessed, asystolic arrest rarely survive to hospital discharge 32 and have been recommended by others to not have in‐hospital CPR initiated if the hospital is in a pandemic crisis. 33
Highly Lethal Risk Factors for Adult Patients
Immediate or Near‐Immediate Mortality Despite Aggressive Therapy
(adapted from the NYS DOH Draft Statement 18 )
Cardiac arrest: unwitnessed arrest in asystole, recurrent arrest unresponsive to standard ACLS; trauma‐related arrest
Persistent systolic blood pressure <90 despite adequate fluid resuscitation and vasopressor therapy
Traumatic brain injury with no motor response to pain (best motor response = 1) (see Supporting Information Appendix S1)
Severe burns: where predicted survival ≤10% even with aggressive therapy (see Supporting Information Appendix S1)
Any other conditions resulting in immediate or near‐immediate mortality even with aggressive therapy (eg, subarachnoid hemorrhage with herniation, exsanguination, terminal cancer)
5.2. Step 2—mortality risk assessment
Among patients who do not meet the above criteria, the initial SOFA score (Table 1) may be used to predict the likelihood of mortality for patients requiring ventilatory support. 34 Ideally, calculation of their SOFA score will occur before clinical deterioration. Clinicians should discuss and consider recommending do‐not‐resuscitate status to patients with a SOFA score >11 (80% mortality) or if recent labs are unavailable. A non‐treating clinician can access the electronic medical record‐based data and help calculate a SOFA score. Patients with a pre‐arrest SOFA score between 8 and 11 have a reasonable chance of survival on the ventilator (<50% mortality) and may benefit from the standard ACLS algorithm performed by health care providers in appropriate PPE. 35 Patients with a SOFA score >11 calculated based on lab data within the past 90 days are the least likely to survive intubation following cardiac arrest. Blanket do‐not‐resuscitate (DNR) orders for patients with cardiac arrest during the COVID‐19 pandemic have been discussed but these orders ignore the principle of Duty to Treat, especially with patients who might have a reasonable chance of survival with timely intervention. 36
TABLE 1.
SOFA score a
| Variable | 0 | 1 | 2 | 3 | 4 | Score (0–4) |
|---|---|---|---|---|---|---|
| Pulmonary: PaO2/FiO2 mm Hg | >400 | <400 | <300 | <200 | <100 | |
| Hematologic: Platelets, ×103/μL | >150 | <150 | <100 | <50 | <20 | |
| Hepatic: Bilirubin, mg/dL | <1.2 | 1.2–1.9 | 2.0–5.9 | 6.0–11.9 | >12 | |
| Cardiac: Hypotension | None | Mean ABP <70 mm Hg | Dop <5 | Dop 6–15 or Epi <0.1 or Norepi <0.1 | Dop >15 or Epi >0.1 or Norepi >0.1 | |
| Neurologic: Glasgow coma score | 15 | 13–14 | 10–12 | 6–9 | <6 | |
| Renal: Creatinine, mg/dL | <1.2 | 1.2–1.9 | 2.0–3.4 | 3.5–4.9 | >5 | |
| Total (0–24): |
Dop, dopamine; Epi, epinephrine; Norepi, norepinephrine; SOFA, sequential organ failure assessment.
Dop, Epi, and Norepi doses in μg/kg/min (administered for at least 1 hour).
With permission by Springer Nature.
We propose an adaptable decision matrix (Figure 1) that can be applied to cardiac arrest patients during the COVID‐19 pandemic based on the criteria above. For patients who have unwitnessed, asystolic events, we recommend ceasing efforts and initiating comfort care measures after just 6–10 minutes of CPR, if initiated. Ten to fifteen minutes may be considered for those with a calculated SOFA score of 8–11. This provides time to address immediately reversible life threats. As fewer resources are available (eg, lack of HEPA filters or negative pressure rooms) even the time to provide resuscitation for patients in this category may constitute a significant risk to the health care team. A suggested maximum of 30 minutes may be considered for those with SOFA <8 as they are more likely to recover with less organ dysfunction. Physicians will always have clinical discretion to continue beyond 30 minutes. Consider a second opinion with a licensed physician to help with determination of futility of medical care especially when labs are not available to assist with the SOFA score calculation.
FIGURE 1.
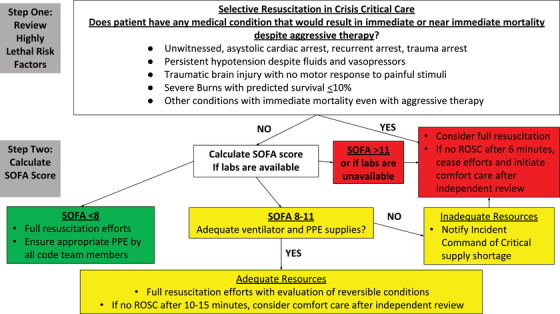
Selective resuscitation in crisis critical care
Ventilator allocation schemes have considered appeals by the disabled or family members who feel the withdrawal of care would be unjust to their family members. 37 The appeals process would focus on looking for technical errors to determine if reconsideration of withdrawal of ventilatory support could proceed. With minutes to decide, and family not at the bedside in the suspected COVID‐19 patient, we support a 2‐physician mechanism with one of the physicians not directly involved in the care of the patient to act as an advocate of the patient. 19 , 38 This scheme would work in departments where there are 2 attending emergency physicians; in small facilities, a single attending may need to reach out to a hospitalist or other specialist. If consultation with another physician is not feasible, by default, the decision would be left to the clinical judgment of the single attending emergency physician.
6. RESOURCE‐TIERED APPROACH TO CPR FOR CANDIDATE PATIENTS
Much will be written about the response to COVID‐19 in the ED in the coming months and years. Each hospital system will have different levels of resources that may change as the pandemic evolves and supply lines adapt. Below is a description of potential options available for ED management of patients who suffer cardiac arrest. With the variety of presentations of the pandemic, it may be difficult to differentiate between patients with suspected COVID‐19 and those not suspected of a COVID‐19 infection. 39 Available resuscitation options will also evolve over time as health care providers who return to work after becoming infected with or vaccinated for COVID‐19 are re‐introduced to the health care system. These providers may be useful in forming the responding team, although strength of immunity after COVID‐19 infection is unknown and asymptomatic carriage and potential transmission via fomites may require continued use of PPE to minimize inadvertent passage to non‐immune health care personnel.
6.1. Ideal option
Consider airborne PPE‐protected teams 24/7, immediately available for cardiac arrests throughout the hospital and positioned closely to patients who have a high risk of decompensating based on monitored clinical data such as eCART (electronic Cardiac Arrest Risk Triage) score, MEWS (Modified Early Warning System), or NEWS (National Early Warning Score) for inpatients 40 or pre‐admission MuLBSTA 41 for viral pneumonia. PSI (Pneumonia Severity Index and CURB‐65 scores are appropriate for bacterial pneumonia). There are no prognostic scores yet developed for COVID‐19 pneumonia. 42 Placing defibrillation pads on the electrically unstable patient prepares for timely defibrillations and minimizes the need to perform chest compressions. Mechanical compression devices can help minimize the number of responders needed.
6.2. Interim recommendations
The AHA's interim guidance recognizes the limited availability of mechanical compression devices, but emphasizes provider protection with techniques to reduce aerosolization risk. 15 Their recommendations include limiting personnel and donning PPE before any compressions and moving quickly to endotracheal intubation. Ventilate with bag‐mask only in a negative pressure room with a HEPA filter and tightly seal with a securable BIPAP mask. Intubate only under first‐pass maximal success settings or use a supraglottic airway with HEPA filter attached until the patient has return‐of‐spontaneous‐circulation. Sterilizable intubation boxes may help reduce aerosolization risk; additional aerosol mitigation strategies and discussion of the further AHA guidance on out‐of‐hospital and in‐hospital cardiac arrests are beyond the scope of this paper.
6.3. Crisis option
If appropriate PPE is unavailable, ask for informed clinical volunteers to assist in the resuscitation with any available personal protective equipment. Inform the volunteers of the risk‐stratification specific to the patient prior to any resuscitation attempt. This is extremely important in cases where there is the lack of N‐95s or even facemasks as compression‐only CPR (CO‐CPR) may be considered an aerosol‐generating procedure. 43 , 44 Defibrillation is likely safe. 43 In the most recent severe acute respiratory syndrome outbreak, surveyed family members who had just been taught compression‐only CPR were just as willing to perform CPR as before the outbreak; whereas, unrelated bystanders were significantly less willing in a pandemic. 45 These options may be adapted by dispatcher‐assisted cardiac arrest responses with appropriate personal protective equipment guidance.
7. POST‐RESUSCITATION CARE
If resuscitation has been successful but no ventilators remain, contact the closest available hospital, expedite transport and use the EMS system's ventilator equipment while having respiratory therapy provide bag‐valve‐HEPA‐filter ventilations. This method will occupy the respiratory therapist until EMS can arrive. Consider having PPE‐protected EMS personnel assist the respiratory therapist/nurse with the transport ventilator. If there are no ventilators available within reasonable transport distance and no chance of ventilators opening up, the last option would be to terminate mechanical ventilation when necessary and initiate palliative care to free up staff to care for patients with an improved chance of survival. Few institutions have the ability to provide extracorporeal membrane oxygenation (ECMO) for patients with acute respiratory distress syndrome and these proposed guidelines are not applicable for patients on ECMO.
8. LEGAL CONCERNS
These guidelines will need to be applied consistently across each individual state, region and health system and reviewed continuously with periodic reassessments. Each state will have their own legal considerations but with declarations of disaster, suspensions of state statutes, local laws and ordinances can occur. Many states have protections from liability in a public health emergency such as an influenza pandemic and, although not yet tested, should apply to this COVID‐19 pandemic. Good Samaritan laws do not apply in a facility that has proper and necessary medical equipment. 46 With lack of sufficient PPE and ventilators, this law may be tested and unfortunately there are incomplete protections for delays in care with existing laws. As the pandemic evolves, the executive branches of government may implement selective waivers to HIPAA and EMTALA. At the time of this writing, New York, Michigan, and 9 other states have issued executive orders protecting physicians from civil liabilities related to COVID‐19 management. 47
9. WITHDRAWAL OF LIFE‐SUSTAINING THERAPY
Palliative care resources, including spiritual care, will need to be made available when requested by the family or the clinical team. Consult the hospital system's palliative care team, possibly through telemed, to interface with the power‐of‐attorney before decompensation or intubation to support the wishes of the patient and minimize the risk of civil litigation. 48 It is currently unknown whether patients who die from COVID‐19 may be able to provide organ donation. 49 , 50 Bedside viewing of the deceased may be not safe when PPE supplies are constrained due to persistent fomites. 51
CONFLICTS OF INTEREST
None.
DISCLOSURES
AH is a co‐author on the Interim Guidance for Basic and Advanced Life Support in Adults, Children, and Neonates with Suspected or Confirmed COVID‐19. Circulation. 2020 April 9. RK is a member of the American College of Cardiology Ethics and Compliance Committee.
Supporting information
Appendix S1. Additional clinical information regarding highly lethal risk factors (step 1)
ACKNOWLEDGMENTS
The authors would like to thank the members of the American College of Emergency Physicians Public Health Injury Prevention Committee and Nicholas Johnson, MD, FACEP; Rebecca Barron, MD, MPH; Courtney Edwards, DNP, MPH, CCRN; and Margaret Montgomery, RN, MSN for their valuable feedback.
Hsu A, Weber W, Heins A, Josephson E, Kornberg R, Diaz R. A proposal for selective resuscitation of adult cardiac arrest patients in a pandemic. JACEP Open. 2020;1:408–415. 10.1002/emp2.12096
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Catherine A. Marco, MD.
REFERENCES
- 1. WHO Director‐General's opening remarks at the media briefing on COVID‐19‐11 March 2020. World Health Organization. http://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%201411-march-2020. Accessed April 17, 2020.
- 2. Coronavirus COVID‐19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Johns Hopkins University. coronavirus.jhu.edu/map.html. Accessed June 1, 2020.
- 3. Sutherland M. COVID‐19 Complications. Critical Care Project. http://covid19.ccproject.com. Accessed April 17, 2020.
- 4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pan SF, Zhang HY, Li CS, Wang C. Cardiac arrest in severe acute respiratory syndrome: analysis of 15 cases. Zhonghua Jie He He Hu Xi Za Zhi. 2003;26(10):602‐605. [PubMed] [Google Scholar]
- 6. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID‐19 in Wuhan, China. JAMA Cardiol. 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID‐19) in Healthcare Settings. Centers for Disease Control. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html. Accessed April 17, 2020.
- 8. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67‐e492. [DOI] [PubMed] [Google Scholar]
- 9. Anderson LW, Holmberg MY, Berg KM, Donnino MW, Granfeldt A. In‐Hospital cardiac arrest: a review. JAMA. 2019;321(12):1200‐1210. ncbi.nlm.nih.gov/pmc/articles/PMC6482460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shao F, Xu S, Ma X, et al. In‐hospital cardiac arrest outcomes among patients with COVID‐19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hick JL, Hanfling D, Wynia MK, Pavia AT. Duty to Plan: Health Care, Crisis Standards of Care, and Novel Coronavirus SARS‐CoV‐2. NAM Perspectives. Discussion paper. Washington, DC: National Academy of Medicine; 2020. 10.31478/202003b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. EXECUTIVE ORDER No. 2020–30 Temporary relief from certain restrictions and requirements governing the provision of medical services. https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-523481-,00.html. Accessed April 17, 2020.
- 13. Maryland Public Safety Section 14‐3A‐06. https://law.justia.com/codes/maryland/2005/gps/14-3A-06.html. Accessed April 17, 2020.
- 14. Guidelines for Crisis Standards of Care during Disasters, 2013, June. https://www.acep.org/globalassets/uploads/uploaded-files/acep/clinical-and-practice-management/policy-statements/information-papers/guidelines-for-crisis-standards-of-care-during-disasters.pdf. Accessed April 17, 2020.
- 15. Edelson DP, Sasson C; Chan PS, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID‐19. Circulation. 2020; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16. Powell T, Christ KC, Birkhead GS. Allocation of ventilators in a public health disaster. Disaster Med Public Health Prep. 2008;2(1):20‐26. [DOI] [PubMed] [Google Scholar]
- 17. Romney D, Fox H, Carlson S, et al. Allocation of scarce resources in a pandemic: a systematic review of U.S. State Crisis Standards of Care Documents. Disaster Med Public Health Prep. 2020:1‐19. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ventilator Allocation Guidelines . New York State Task Force on Life and the Law. New York State Department of Health. 2015. https://www.health.ny.gov/regulations/task_force/reports_publications/docs/ventilator_guidelines.pdf. Accessed April 17, 2020.
- 19. Oregon Crisis Care Guidance: Providing a Framework for Crisis Healthcare. https://www.theoma.org/OMA/Learn-content/Public-Health-Library/Crisis-Care.aspx. Accessed April 17, 2020.
- 20. Khan Z, Hulme J, Sherwood N. An assessment of the validity of SOFA score based triage in H1N1 critically ill patients during an influenza pandemic. Anaesthesia. 2009;64(12):1283‐1288. [DOI] [PubMed] [Google Scholar]
- 21. The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research, Report of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Federal Register 44(76):23191‐23197. https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html. Accessed April 17, 2020. [Google Scholar]
- 22. Guidelines for Ethical Allocation of Scarce Medical Resources and Services During Public Health Emergencies in Michigan. Version 2.0. www.mimedicalethics.org/Documentation/Michigan%20DCH%20Ethical%20Scarce%20Resources%20Guidelines%20v2%20rev%20Nov%202012.0.pdf. Accessed April 17, 2020.
- 23. Hwang SY, Yoon H, Yoon A, et al. N95 filtering facepiece respirators do not reliably afford respiratory protection during chest compression: a simulation study. Am H Emerg Med. 2020;38(1):12‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guidance for Decisions Regarding Cardiopulmonary Resuscitation during the COVID‐19 Pandemic. https://adobe.ly/3bujCW9. Accessed April 17, 2020.
- 25. Farmer JC, Wax R, Baldisseri MR. Preparing your ICU for Disaster Response. Chapter 8: Ethical Decision Making in Disasters: Key Ethical Principles and the Role of the Ethics Committee. Society of Critical Care Medicine; 2012. https://sccm.org/getattachment/Disaster/PreparingforDisasterResponse.pdf. Accessed April 17, 2020.
- 26. Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis‐related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707‐710. [DOI] [PubMed] [Google Scholar]
- 27. Mitchell OJL, Edelson DP, Abella BS. Predicting cardiac arrest in the emergency department. JACEP Open. 2020;1‐6. 10.1002/emp2.12015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, Pilcher DV; Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE) . Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for In‐Hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317(3):290‐300. [DOI] [PubMed] [Google Scholar]
- 29. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818‐829. [PubMed] [Google Scholar]
- 30. Seewald S, Wnent J, Lefering R, et al. CaRdiac Arrest Survival Score (CRASS) ‐ A tool to predict good neurological outcome after out‐of‐hospital cardiac arrest. Resuscitation. 2020;146:66‐73. [DOI] [PubMed] [Google Scholar]
- 31. Hick JL, O'Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Academic Emergency Medicine 2006;13(2):223‐229. [DOI] [PubMed] [Google Scholar]
- 32. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63‐81. [DOI] [PubMed] [Google Scholar]
- 33. Väyrynen T, Kuisma M, Määttä T, Boyd J. Medical futility in asystolic out‐of‐hospital cardiac arrest. Acta Anaesthesiol Scand. 2008;52(1):81‐87. [DOI] [PubMed] [Google Scholar]
- 34. Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis‐related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis‐Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707‐710. [DOI] [PubMed] [Google Scholar]
- 35. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754‐1758. [DOI] [PubMed] [Google Scholar]
- 36. ‘We're going to be coding dead people’: Hospitals consider do‐not‐resuscitate order for all COVID‐19 patients https://www.beckershospitalreview.com/public-health/we-re-going-to-be-coding-dead-people-hospitals-consider-do-not-resuscitate-order-for-all-covid-19-patients.html. Accessed April 17, 2020.
- 37. Complaint of Disability Rights Washington, Self Advocates in Leadership, The Arc of the United States, and Ivanova Smith Against the Washington State Department of Health (WA DOH), the Northwest Healthcare Response Network (NHRN) and the University of Washington Medical Center (UWMC) https://www.centerforpublicrep.org/wp-content/uploads/2020/03/OCR-Complaint_3-23-20-final.pdf. Accessed April 17, 2020.
- 38. ACEP Guidelines for Crisis Standards of Care during Disasters. https://www.acep.org/globalassets/uploads/uploaded-files/acep/clinical-and-practice-management/policy-statements/information-papers/guidelines-for-crisis-standards-of-care-during-disasters.pdf. Accessed March 24, 2020.
- 39. Emanuel EJ, Persad G, Upshad R, et al. Fair Allocation of scarce medical resources in the time of Covid‐19. N Engl J Med. 2020. [DOI] [PubMed] [Google Scholar]
- 40. Green M, Lander H, Snyder A, Hudson P, Churpek M, Edelson D. Comparison of the Between the Flags calling criteria to the MEWS, NEWS and the electronic Cardiac Arrest Risk Triage (eCART) score for the identification of deteriorating ward patients. Resuscitation. 2018;123:86‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guo L, Wei D, Zhang X, Wu Y, Li Q, Zhou M, Qu J. Clinical features predicting mortality risk in patients with viral pneumonia: the MuLBSTA score. Front Microbiol. 2019;10:2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chen JH, Chang SS, Liu JJ, Chan RC, Wu JY, Wang WC, Lee SH, Lee CC. Comparison of clinical characteristics and performance of pneumonia severity score and CURB‐65 among younger adults, elderly and very old subjects. Thorax. 2010;65(11):971‐977. [DOI] [PubMed] [Google Scholar]
- 43. COVID‐19 Practical Guidance for Implementation. www.ilcor.org/covid-19. Accessed April 20, 2020.
- 44. Tran K, Cimon K, Severn M, Pessoa‐Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lam KK, Lau FL, Chan WK, Wong WN. Effect of severe acute respiratory syndrome on bystander willingness to perform cardiopulmonary resuscitation (CPR)–is compression‐only preferred to standard CPR. Prehosp Disaster Med. 2007;22(4):325‐329. [DOI] [PubMed] [Google Scholar]
- 46. Clark PA. Medical Futility: Legal and Ethical Analysis. Virtual Mentor. 2007;9(5):375‐383. [DOI] [PubMed] [Google Scholar]
- 47. Executive Order. Continuing Temporary Suspension and Modification of Laws Relating to the Disaster Emergency. www.governor.ny.gov/sites/governor.ny.gov/files/atoms/files/EO_202.10.pdf. Accessed April 17, 2020.
- 48. Cohen IG, Crespo AM, White DB. Potential legal liability for withdrawing or withholding ventilators during COVID‐19: assessing the risks and identifying needed reforms. JAMA. 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 49. Pan L, Zeng J, Yang H. Challenges and countermeasures for organ donation during the SARS‐CoV‐2 epidemic: the experience of Sichuan Provincial People's Hospital. Intensive Care Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gift of Life Marrow Registry COVID‐19 Statement. https://www.giftoflife.org/posts/post/Gift-of-Life-Marrow-Registry-COVID-19-Statement. Accessed April 17, 2020.
- 51. Santarpia JL, Rivera DN, Herrera V, et al. Transmission potential of SARS‐CoV‐2 in viral shedding observed at the University of Nebraska Medical Center. Preprint. March 26, 2020. 10.1101/2020.03.23.20039446 [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Additional clinical information regarding highly lethal risk factors (step 1)


