Patients usually require supplementary oxygen for a period of time in the post‐anaesthesia care unit (recovery area) [1]. Patients with COVID‐19 still require elective or emergency surgery and there appears to be a lower threshold for tracheal intubation in these patients [2], necessitating the use of mechanical ventilation and neuromuscular blocking drugs. It, therefore, follows that they will likely need supplementary oxygen for a period of time following tracheal extubation. A study by Hui et al. in 2006 showed that while wearing a simple facemask with an oxygen flow rate of 4 l.min−1, breathing 12 breaths per minute with a tidal volume of 500 ml, an expiratory plume of potentially infectious air can be detected around the patient up to a distance of 0.4 m [3].
Covering the nose and mouth with a facemask of individuals symptomatic with COVID‐19 has been recommended by several authorities, including WHO, as well as government organisations from several countries including Australia [4] and the UK. It has been shown that wearing a mask will reduce coronavirus detection in droplet and aerosol samples in symptomatic patients [5]. The recent consensus guidelines published in Anaesthesia recommend that patients wear a facemask in addition to their oxygen mask or nasal cannulae following tracheal extubation, where this is practicable [2].
The question has arisen in our institution as to whether the facemask should be applied over a Hudson mask, or if it should be applied underneath the Hudson mask, and if there is any difference in FIO2 between the two approaches. Using a carbon dioxide sampling line attached to a 16G cannula, we measured the FIO2 at the lips in a healthy volunteer in three situations. The first, breathing air wearing a surgical mask on the face; second, breathing 6 l.min−1 oxygen via a Hudson mask placed over the top of a surgical mask; and third, breathing 6 l.min−1 oxygen via a Hudson mask placed underneath a surgical mask. The FIO2 measured was 0.20, 0.50 and 0.54, respectively (Fig. 1).
Figure 1.
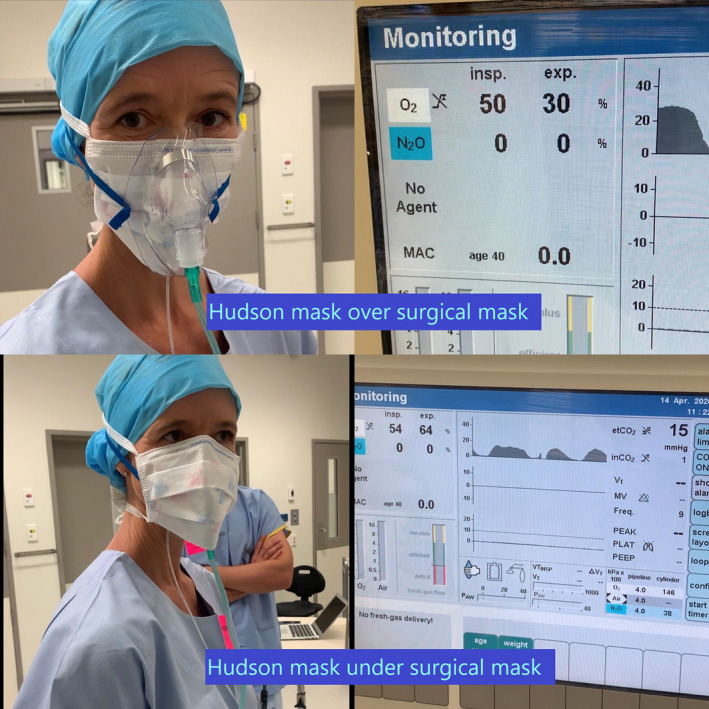
FIO2 shown with Hudson mask over, then under, a surgical face mask.
Given the negligible difference in FIO2 when the Hudson mask is placed over a surgical mask, our COVID‐19 extubation protocols now call for a surgical mask to be placed over the patient’s nose and mouth immediately following extubation, and for a Hudson mask to be placed on top. This could also have implications for patients in the rest of the hospital. If a patient needs to be transported around the hospital, WHO guidelines suggest they should be wearing a surgical mask. If they also need supplementary oxygen, these data would suggest they can wear the oxygen mask over the top of a surgical mask without compromising their FIO2.
No competing interests declared.
References
- 1. Karcz M, Papadakos P. Respiratory complications in the post‐anesthesia care unit: a review of pathophysiological mechanisms. Canadian Journal of Respiratory Therapy 2013; 49: 21–9. [PMC free article] [PubMed] [Google Scholar]
- 2. Cook TM, El‐Boghdadly K, McGuire B, et al. Consensus guidelines for managing the airway in patients with COVID‐19. Anaesthesia 2020; 75: 785–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hui DS, Ip M, Tang JW, et al. Airflows around oxygen masks – a potential source of infection? Chest 2006; 130: 822–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Australian Government Department of Health . Information on the Use of Surgical Masks. 14/4/2020. https://www.health.gov.au/sites/default/files/documents/2020/04/coronavirus‐covid‐19‐information‐on‐the‐use‐of‐surgical‐masks_0.pdf (accessed 19/05/2020).
- 5. Leung NH, Chu DK, Shiu EY, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine 2020; 26: 676–80. [DOI] [PMC free article] [PubMed] [Google Scholar]


