Short abstract
The COVID‐19 pandemic has presented an opportunity to evaluate current practices in cancer care. This letter to the editor focuses on one example, making the case for stereotactic body radiotherapy in Hepatocellular Carcinoma.
As the COVID‐19 pandemic spreads across the globe, major transformations are rapidly being implemented because of the unprecedented pressure on health care systems. Management of patients with cancer has been particularly affected by the reduced access to cancer treatments related to prolonged wait times for diagnostic and interventional procedures, treatment delays or interruptions, fragmentation of multidisciplinary management with a shrinking oncology workforce, and self‐isolation for fear of nosocomial infection. Consequently, there is a risk of detrimental consequences for this highly vulnerable patient population. This dire scenario represents an opportunity to evaluate current practices and provide a lesson for the future in the post–COVID‐19 era. The case of stereotactic body radiotherapy (SBRT) in hepatocellular carcinoma (HCC) is emblematic.
SBRT has emerged as a noninvasive, painless, and effective therapeutic modality delivered in a few daily fractions over less than 1 week for patients with HCC, from early to advanced stage.
In early stage HCC, local therapy can be offered as a definitive or bridging treatment [1]. Because of current restrictions in access to operating rooms and the redeployment of anesthesiologists to intensive care units, SBRT represents an appealing option compared with invasive local therapies such as surgery, radiofrequency or microwave ablation, and regional therapies such as transarterial or radioembolization, which may require general anesthesia and recovery. Although randomized trials are lacking, indirect comparisons suggest comparable efficacy of SBRT with these treatment modalities for similar stage patients [2, 3, 4]. The use of SBRT may reduce the need for systemic therapy in advanced patients with symptomatic involvement or poor responders to standard treatment, e.g., macroscopic vascular invasion [5].
Despite the numerous studies demonstrating efficacy, long‐term survival, and low toxicity rates [6, 7, 8], many current HCC treatment algorithms do not incorporate SBRT in the management of HCC. Most limit its use to patients who are ineligible for or refractory to other invasive local and/or regional therapies. The significant time and effort required, coupled with the limited funding and lack of pharmaceutical and vendor support, have been an impediment to conducting large‐scale, potentially practice‐changing clinical trials of SBRT for HCC: thus, SBRT may be indefinitely relegated to an ancillary role.
It is expected that, during the COVID‐19 pandemic and its aftermath, SBRT will increasingly represent a preferred treatment that may relieve the burden of interrupted and deferred cancer treatments, the overload of chemotherapy facilities, and patient exposure and risk of COVID‐19 infection because of repeated visits and prolonged stays in the hospital [9]. With more widespread clinical use of SBRT, there may be an increase in support for trials of this effective HCC treatment. It is crucial that outcome and toxicity data be recorded during this time when nonstandard therapies are offered. These data will hopefully provide further evidence to reconsider SBRT as a first‐line treatment option for HCC (proposed algorithm is shown in Fig. 1).
Figure 1.
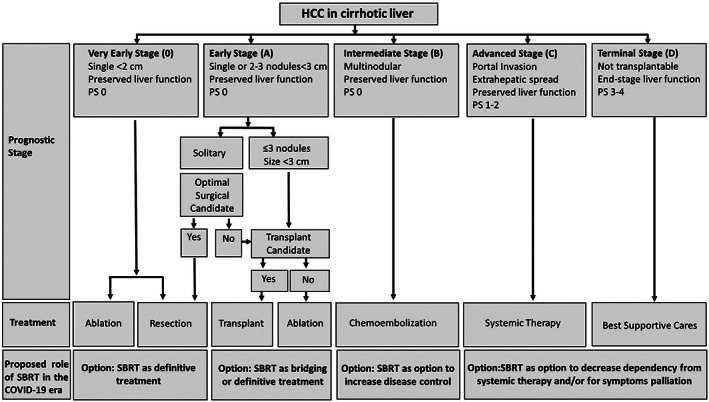
Proposal for a modified Barcelona Clinic Liver Cancer staging system (BCLC)‐based treatment algorithm during the COVID‐19 pandemic.
Abbreviations: HCC, hepatocellular carcinoma; PS, performance status; SBRT, stereotactic body radiotherapy.
It is our hope that the cumulative global experience gained during the COVID‐19 pandemic may allow for a full recognition of SBRT as a useful therapy in the management of HCC based on real‐life evidence.
Disclosures
Jinsil Seong: Accuray (RF); Laura A. Dawson: Raysearch Oncology (OI). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact Commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
References
- 1. Durand‐Labrunie J, Baumann AS, Ayav A et al. Curative irradiation treatment of hepatocellular carcinoma: A multicenter phase 2 trial. Int J Radiat Oncol Biol Phys 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2. Lee J, Shin IS, Yoon WS et al. Comparisons between radiofrequency ablation and stereotactic body radiotherapy for liver malignancies: Meta‐analyses and a systematic review. Radiother Oncol 2020;145:63–70. [DOI] [PubMed] [Google Scholar]
- 3. Shen PC, Chang WC, Lo CH et al. Comparison of stereotactic body radiation therapy and transarterial chemoembolization for unresectable medium‐sized hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 2019;105:307–318. [DOI] [PubMed] [Google Scholar]
- 4. Sapir E, Tao Y, Schipper MJ et al. Stereotactic body radiation therapy as an alternative to transarterial chemoembolization for hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 2018;100:122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shui Y, Yu W, Ren X et al. Stereotactic body radiotherapy based treatment for hepatocellular carcinoma with extensive portal vein tumor thrombosis. Radiat Oncol 2018;13:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jang WI, Kim MS, Bae SH et al. High‐dose stereotactic body radiotherapy correlates increased local control and overall survival in patients with inoperable hepatocellular carcinoma. Radiat Oncol 2013;8:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Takeda A, Sanuki N, Tsurugai Y et al. Phase 2 study of stereotactic body radiotherapy and optional transarterial chemoembolization for solitary hepatocellular carcinoma not amenable to resection and radiofrequency ablation. Cancer 2016;122:2041–2049. [DOI] [PubMed] [Google Scholar]
- 8. Kim N, Cheng J, Jung I et al. Stereotactic body radiation therapy vs. radiofrequency ablation in Asian patients with hepatocellular carcinoma. J Hepatol 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 9. Tchelebi LT, Haustermans K, Scorsetti M et al. Recommendations on the use of radiation therapy in managing patients withgastrointestinal malignancies in the era of COVID‐19. Radiother Oncol 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


