H5 viruses continue to be a threat for public health. Because these viruses are immunologically novel to humans, they could spark a pandemic when adapted to transmit between humans. Avian influenza viruses need several adaptive mutations to bind to human-type receptors, increase hemagglutinin (HA) stability, and replicate in human cells. However, knowledge on adaptive mutations during human infections is limited. A previous study showed substantial diversity within the receptor binding site of H5N1 during human infection. We therefore analyzed the observed amino acid changes phenotypically in a diverse set of assays, including virus replication, stability, and receptor specificity. None of the tested substitutions resulted in a clear step toward a human-adapted virus capable of aerosol transmission. It is notable that acquiring human-type receptor specificity needs multiple amino acid mutations, and that variability at key position 226 is not tolerated, reducing the risk of them being acquired naturally.
KEYWORDS: influenza virus, H5N1, human adaptation, receptor specificity, hemagglutinin
ABSTRACT
Highly pathogenic avian influenza (HPAI) viruses are enzootic in wild birds and poultry and continue to cause human infections with high mortality. To date, more than 850 confirmed human cases of H5N1 virus infection have been reported, of which ∼60% were fatal. Global concern persists that these or similar avian influenza viruses will evolve into viruses that can transmit efficiently between humans, causing a severe influenza pandemic. It was shown previously that a change in receptor specificity is a hallmark for adaptation to humans and evolution toward a transmittable virus. Substantial genetic diversity was detected within the receptor binding site of hemagglutinin of HPAI A/H5N1 viruses, evolved during human infection, as detected by next-generation sequencing. Here, we investigated the functional impact of substitutions that were detected during these human infections. Upon rescue of 21 mutant viruses, most substitutions in the receptor binding site (RBS) resulted in viable virus, but virus replication, entry, and stability were often impeded. None of the tested substitutions individually resulted in a clear switch in receptor preference as measured with modified red blood cells and glycan arrays. Although several combinations of the substitutions can lead to human-type receptor specificity, accumulation of multiple amino acid substitutions within a single hemagglutinin during human infection is rare, thus reducing the risk of virus adaptation to humans.
IMPORTANCE H5 viruses continue to be a threat for public health. Because these viruses are immunologically novel to humans, they could spark a pandemic when adapted to transmit between humans. Avian influenza viruses need several adaptive mutations to bind to human-type receptors, increase hemagglutinin (HA) stability, and replicate in human cells. However, knowledge on adaptive mutations during human infections is limited. A previous study showed substantial diversity within the receptor binding site of H5N1 during human infection. We therefore analyzed the observed amino acid changes phenotypically in a diverse set of assays, including virus replication, stability, and receptor specificity. None of the tested substitutions resulted in a clear step toward a human-adapted virus capable of aerosol transmission. It is notable that acquiring human-type receptor specificity needs multiple amino acid mutations, and that variability at key position 226 is not tolerated, reducing the risk of them being acquired naturally.
INTRODUCTION
Highly pathogenic avian influenza A/H5N1 (HPAI A/H5N1) viruses first emerged in China in 1996. From 2003 onwards, they started spreading to Southeast Asia, Europe, and Africa. Since then, HPAI A/H5N1 viruses have become enzootic in several countries in Asia and the Middle East and infected wild aquatic birds in many countries. HPAI A/H5N1 viruses repeatedly caused devastating outbreaks in poultry as well as sporadic human infections with high mortality. As of 2019, more than 850 confirmed human H5N1 virus infections have been reported to the WHO, with most cases occurring in Indonesia (200), Vietnam (127), and Egypt (359). Interestingly, the case fatality rates (CFR) among laboratory-confirmed human infections differed substantially between these geographic regions, with rates of 84%, 50%, and 33% in Indonesia, Vietnam, and Egypt, respectively.
The majority of human HPAI A/H5N1 virus infections to date resulted from direct contact with infected poultry (1–3). However, there is global concern that HPAI A/H5N1 and related viruses may evolve toward efficient transmission among humans and cause a new influenza pandemic. For an avian influenza virus to evolve toward a human pathogen with pandemic potential, it must acquire several phenotypic changes to allow efficient transmission between humans via aerosol or respiratory droplets (here abbreviated as airborne transmission). In recent years, several key phenotypic traits and corresponding genetic changes have been identified to play a role in human adaption of avian influenza viruses (4–6). A key requirement is the ability of viruses to replicate efficiently at the relatively low temperature of the human upper respiratory tract, which can be conferred by substitutions in the viral polymerase proteins, including E627K and D701N in PB2 (7, 8). It is very possible that other polymerase complex substitutions could result in similar adaptation (9–11). Another key requirement is a change in receptor preference of the hemagglutinin surface protein (HA) from binding to α-2,3-linked sialic acid receptors, present in the intestinal and respiratory tracts of birds and lower respiratory tracts of humans, to binding to α-2,6-linked sialic acids that are predominantly present in the upper respiratory tracts of humans (12, 13). Identification of the amino acid changes necessary for attachment of H5N1 viruses to α-2,3- versus α-2,6-linked sialic acids has been a subject of intense research, and several different combinations of substitutions were identified in distinct genetic clades of H5 viruses (14).
The HA receptor binding site (RBS) domain contains several conserved amino acids (Y95, W153, H183, and Y195) and has conserved structural features that include the 130- and 220-loops and the 190-helix. Several hallmark substitutions that have led to specificity for human receptors have been identified in the putative avian precursors of human influenza viruses. For H1N1, H2N2, and H3N2 viruses, these were E190D/G225D and Q226L/G228S, respectively (15, 16), although these simple 2-amino-acid substitutions are clearly an oversimplification (17, 18). They impact receptor specificity in the context of other amino acids in the receptor binding pocket (17, 18) and cannot be simply generalized to other subtypes, such as H5 (19, 20). Moreover, as seen for H3N2, receptor specificity continues to evolve during passage in humans (21, 22). Regardless, several reports have used this information and found that different sets of multiple substitutions can generate HPAI A/H5N1 viruses that bind human-type receptors (reviewed in reference 14). However, introducing these substitutions in the RBS alone did not result in robust airborne virus transmission in the ferret model (23). To obtain HPAI A/H5N1 viruses that were able to transmit between ferrets, several forced viral evolution approaches with virus harboring HA containing two of the aforementioned substitutions in the RBS have been applied with success (24, 25). Several substitutions in the RBS of HA (e.g., N224K, Q226L, and G228S) have resulted in the switch of receptor specificity that supported airborne virus transmission when accompanied by other genetic changes in HA and other viral genes obtained during the forced viral evolution (14, 26).
These evolution studies also showed that besides receptor specificity, stability is a key feature of HA for the potential to become an aerosol-transmittable virus with pandemic potential. In general, human influenza viruses have a more stable HA than avian (precursor) viruses (27). In addition, it was shown that substitutions within the RBS can hamper the stability of the HA, which needs to be compensated by additional substitutions in HA, for example, in the trimer interface (6).
While these studies showed that HPAI A/H5N1 viruses can evolve to become airborne transmissible when several key mutations in the HA and the polymerase were introduced prior to infection of ferrets, it remains to be determined to what extent these or other adaptive evolutionary pathways occur during natural infection of humans. Extensive genetic characterization of HPAI viruses was performed by next-generation deep sequencing of 71 clinical specimens from confirmed human HPAI A/H5N1 virus infections (9). In contrast to earlier studies, clinical specimens were used without prior culture in cells or embryonated eggs for whole-genome deep sequencing, to not only identify consensus sequences but also detect minority variants within the cloud of viral quasispecies. High levels of genetic variation were identified, with the highest variation in the polymerase genes and HA. Phenotypic analyses revealed the presence of a series of substitutions within the polymerase complex that increased polymerase activity to levels comparable to that of the known mammalian adaptation substitution PB2-E627K.
However, the phenotypic consequences of the genetic variation in and around the H5 RBS were not yet investigated. Therefore, in this study, we analyzed the biological phenotype conferred by amino acid substitutions in the RBS that arose during H5N1 virus infection in humans. The novel single amino acid substitutions investigated did not confer human-type receptor specificity, whereas combinations of substitutions did. However, virus replication, entry, and stability were often impeded. Our data indicate that while a combination of naturally occurring amino acid mutations allow H5N1 viruses to bind human-type receptors, the number of mutations required is unlikely to occur during a single human infection to enable human-to-human transmission, although accumulation cannot be excluded during long-term infections in immunocompromised humans or in a scenario for which specific substitutions are fitness neutral or positive in poultry (28, 29).
RESULTS
A human infection results in high genetic diversity in the RBS.
Recently, Welkers et al. (9) published work on detection of virus variants that emerged during human infections, using 71 samples from 44 patients with confirmed HPAI A/H5N1 virus infection. Following whole-virus genome amplification from extracted RNA, next-generation sequencing (NGS; Roche 454), and pre- and postmapping quality controls, viral populations were analyzed, including minority-variant detection (9).
In the NGS data set, most variation was observed in the 190-helix and 220-loop, with high variability at position 188. However, this residue is on the backside of the helix facing away from the RBS and is therefore unlikely to be involved in receptor binding. Nonetheless, several residues in both the 190-helix and 220-loop multiple variants were observed, including positions previously shown to be important for receptor specificity of HA: N186H/K/S, E190A/G/K, and R193K/M for the 190-helix and N224D/H/K/S, G225E/R, Q226K/L/R, S227G/N/R, and G228S/R in the 220-loop (23, 30–43). These include the positions 224, 226, and 228 identified to be essential for airborne transmission of HPAI A/H5N1 in the ferret transmission model (24, 25). Interestingly, novel substitutions at positions that were shown to be important for receptor specificity previously were often observed (Table 1, Fig. 1), prompting us to investigate the biological phenotypes of the observed substitutions.
TABLE 1.
Genetic variations observed within the RBS of H5N1 during human infection
| Domain | H3 no.a | H5 no.a | Ind/05b | No. of samplesc | Residue(s) (no. of samples [%])d |
|---|---|---|---|---|---|
| Conserved interface residue | 95 (98) | 91 | Y | 12 | Y: 12 (100) |
| 130-loop | 132 | 128 | S | 12 | S: 12 (100) |
| 133 | 129 | S | 12 | S: 12 (92–100); P: 1 (8) | |
| 134 | 130 | G | |||
| 135 | 131 | V | |||
| 136 | 132 | S | |||
| Conserved interface residue | 153 | 149 | W | 60 | W: 60 (97–100) |
| Antigenic site | 155 | 151 | I | 60 | I: 60 (98–100) M: 1 (1), N: 1 (2) |
| Conserved interface residue | 183 | 179 | H | 59 | H: 59 (98–100); R: 1 (2) |
| 190-helix | 186 | 182 | N | 59 | N: 59 (95–100); S: 3 (3–5); H: 1 (3) |
| 187 | 183 | D | 59 | N: 40 (25–100); D: 19 (75–100); T: 1 (100) | |
| 188 | 184 | A | 59 | E: 38 (3–100); A: 18 (75–100); G: 3 (95–97); K: 3 (2–100); V: 2 (100); T: 1 (6) | |
| 189 | 185 | A | 59 | A: 58 (98–100); E: 1 (99); K: 1 (1); T: 1 (2) | |
| 190 | 186 | E | 59 | E: 59 (92–100); G: 5 (1–4); A: 1 (3); K: 1 (3) | |
| 191 | 187 | Q | 59 | Q: 59 (99–100) | |
| 192 | 188 | T | 59 | T: 59 (98–100); A: 2 (2–2) | |
| 193 | 189 | R | 59 | M: 37 (26–100); R: 17 (74–100); K: 6 (100) | |
| 194 | 190 | L | 59 | L: 59 (99–100) | |
| Conserved interface residue | 195 | 191 | Y | 59 | Y: 59 (98.33–100) |
| 220-loop | 224 | 220 | N | 59 | N: 59 (94–100); D: 1 (4); H: 1 (1); K: 1 (6); S: 1 (3) |
| 225 | 221 | G | 59 | G: 59 (82–100); E: 2 (2–2.3); R: 1 (18) | |
| 226 | 222 | Q | 59 | Q: 59 (80–100); R: 4 (2–20); K: 1 (5) | |
| 227 | 223 | S | 59 | S: 59 (97–100); R: 1 (1) | |
| 228 | 224 | G | 59 | G: 59 (97–100); R: 1 (3) |
Position according to H3 and H5 numbering after removal of the signal peptide.
Amino acid present in the sequence of reference strain A/Indonesia/5/2005 used in this work.
Number of samples with sequencing data available at the position mentioned.
Residues observed, number of samples in which the amino acid is observed, and proportion or proportion range within the sample(s).
FIG 1.
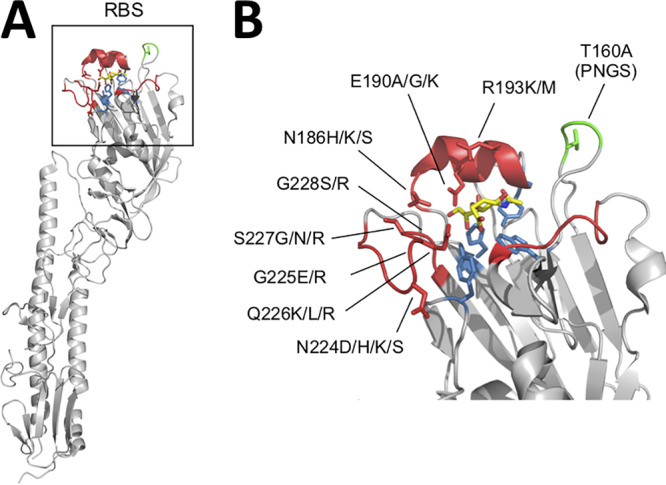
Genetic diversity within the receptor binding site (RBS) of HPAI A/H5N1 during human infections. (A) Molecular model of influenza virus HA indicating the RBS. (B) Close-up of the RBS showing the domains related to receptor specificity: the 30-loop, 190-helix, and 220-loop and residues included for functional characterization (PDB 4K63 [58]).
Naturally occurring genetic changes in the RBS result in viable virus.
Based on previous investigations of avian-to-human receptor binding switches (reviewed in reference 14), we selected several residues within the RBS of HA that showed genetic variation within the human H5N1 virus specimens that we sequenced: 186, 190, 193, 224, 225, 226, 227, and 228 (Fig. 1). We first examined whether the observed genetic variation would affect production of viable viruses. To this end, we introduced the selected substitutions one at a time into the H5 HA gene of reference strain A/Indonesia/5/2005 from which the multibasic cleavage site was removed. Recombinant viruses were produced for each mutant HA in combination with the corresponding NA gene of A/Indonesia/5/2005 and the internal genes of lab-adapted strain A/Puerto Rico/8/34 (PR8). The combination of the PR8 and an H5 without a multibasic cleavage site was made to facilitate experiments at biosafety level 2 and to allow any observed differences in phenotypes to be attributed to the introduced mutations in HA. We rescued all mutant viruses except for the G228R mutant, for which all cultures remained negative despite several rescue attempts, possibly due to the introduction of the bulky charged sidechain of arginine at this position. These results indicate that the observed genetic diversity within the RBS can result in viable virus.
Minimal change in receptor binding specificity by single amino acid substitutions.
To determine if any of these single amino acid substitutions affected receptor-binding specificity, we first determined hemagglutination titers to wild-type and resialylated turkey erythrocytes, a well-established method as a first screen to determine receptor specificity (31). Erythrocytes were treated with bacterial neuraminidase to remove all terminal sialic acids and thereafter resialylated to obtain either α2,3- or α2,6-linked sialic acid bearing red bloods cells. As controls, we used a human H3N2 virus that bound both the untreated and the α2,6-resialylated erythrocytes and an avian H5 virus that only bound untreated and α2,3-resialylated erythrocytes, as expected (Table 2). Next, we tested all viruses with single amino acid substitutions, again including novel variants originating from our sequence data set and substitutions previously described. All mutants identified in the NGS study of Welkers et al. (9) solely bound to untreated and α2,3-resialylated red blood cells. Viruses with E190G and Q226K lost hemagglutination after α2,3-resiaylation, indicating they attached to a receptor that is a substrate for the bacterial neuraminidase but not a substrate for the α,2,3-sialyltransferase. Previously described variants Q226L and G228S bound to α2,6-resialylated erythrocytes, with a modest increase in binding to human-type receptors, while maintaining binding to α2,3-resialylated red blood cells.
TABLE 2.
Receptor specificity of H5N1 RBS mutant viruses as determined by the modified tRBC hemagglutination assay
| Mutanta | HA titer (HAUb
/50 μl) |
|||
|---|---|---|---|---|
| Untreated tRBC | VCNA treated | α-2,3 resialylated | α-2,6 resialylated | |
| Human H3 control | 32 | 0 | 0 | 32 |
| Avian H5 control | 32 | 0 | 64 | 0 |
| WT | 32 | 0 | 64 | 0 |
| T160A | 32 | 0 | 32 | 0 |
| N186H | 24 | 0 | 16 | 0 |
| N186K | 32 | 0 | 24 | 0 |
| N186S | 32 | 0 | 32 | 0 |
| E190A | 32 | 0 | 32 | 0 |
| E190G | 24 | 0 | 0 | 0 |
| E190K | 24 | 0 | 24 | 0 |
| R193K | 32 | 0 | 32 | 0 |
| R193M | 32 | 0 | 32 | 0 |
| N224D | 32 | 0 | 32 | 0 |
| N224H | 64 | 0 | 64 | 0 |
| N224K | 32 | 0 | 32 | 0 |
| N224S | 64 | 0 | 32 | 0 |
| G225E | 16 | 0 | 32 | 0 |
| G225R | 32 | 0 | 32 | 0 |
| Q226K | 16 | 0 | 0 | 0 |
| Q226L | 32 | 0 | 32 | 4 |
| Q226R | 64 | 0 | 64 | 0 |
| S227G | 48 | 0 | 32 | 0 |
| S227N | 48 | 0 | 32 | 0 |
| S227R | 48 | 0 | 32 | 0 |
| G228S | 32 | 0 | 48 | 4 |
All amino acid substitutions are indicated based on H3 numbering. Results are based on at least two independent experiments.
HAU, hemagglutination units.
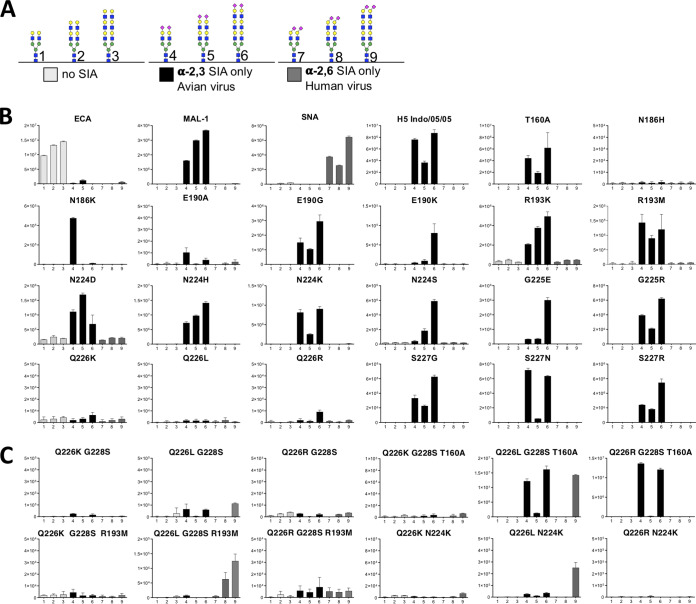
To better understand which receptors were bound by the viruses with single amino acid substitutions, we cloned the open reading frame of the HA ectodomains to express soluble trimeric fluorescent trimers as previously described (44) to make them amendable for glycan microarray analyses. We used a glycan array specifically made for influenza virus with nine relevant N-glycan structures (45) (Fig. 2A). The array consisted of N-glycans with 1 to 3 galactose-N-acetylglucosamine (LacNAc) repeats that were either nonsialylated, capped with α2,3-linked sialic acids, or capped with α2,6-linked sialic acids. We first analyzed if all structures were properly printed using the well-defined plant lectins ECA, MAL-1, and SNA that bind nonsialylated glycans and glycans with α2,3-linked sialic acids and α2,6-linked sialic acids, respectively (Fig. 2B). We tested recombinant H5 proteins containing the same single amino acid substitutions as in the viruses investigated as described above, except for N186S, which did not yield protein. Almost all proteins maintained an avian-type receptor binding profile as they specifically bound α2,3-linked sialic acid on N-glycans, comparable to wild-type (WT) A/Indonesia/5/2005 HA. N186H lost nearly all binding to the array, indicating another core glycan as a receptor, as did mutants Q226K/R/L. This latter substitution is known to have a decreased overall binding avidity (18, 46). The lack of binding to the array by the Q226K/R/L proteins was not apparent in the hemagglutination assays, which might be in part explained by the multivalent character of HA-receptor interactions by virus particles. HA protein with E190A only bound weakly to the glycan with short α2,3-linked sialic acid. Another interesting observation was the strict specificity of N186K to α2,3-linked sialic acid on a single LacNAc, whereas the majority of H5 mutant proteins preferred three LacNAc repeats.
FIG 2.
Glycan array analyses do not show binding to human-type receptors for H5N1 mutant viruses, but a combination of amino acid mutations can lead to human-type receptor specificity. (A) Structures 1 to 3 represent unsialylated glycans (negative controls), 4 to 6 represent glycans containing terminal α2,3-linked sialylation (SIA), and 7 to 9 represent glycans containing terminal α2,6-linked SIA. (B) Binding of control lectins, WT H5N1, and single mutant HA. (C) Binding of H5 HA containing substitutions identified in patients combined with substitutions known to aid to receptor specificity changes. Representative graphs from two biologically independent experiments are presented.
Taken together, the data from the complementary modified red blood cell assay and the glycan array indicated that single amino acid substitutions in the RBS as observed during human infection did not result in a receptor specificity switch toward human-type receptor for H5N1 mutants.
Combinations of amino acid substitutions can lead to human-type receptor specificity.
We hypothesized that combinations of the amino acid substitutions may confer a switch in receptor specificity from α2,3- to α2,6-linked sialic acids. To evaluate whether the novel substitutions identified can contribute to receptor specificity toward the human-type receptor, we constructed combinations of novel and previously reported substitutions. We focused on the novel substitutions at positions 193 and 226, as these residues have been identified as key positions for receptor specificity. Substitutions Q226K/L/R were combined with substitutions that have been reported to confer human-type receptor specificity in the H5 A/Indonesia/05/2005 virus or other backgrounds (14). First, G228S was added in the Q226K/L/R backgrounds, as the combination of Q226L and G228S showed increased binding to α2,6-linked sialic acids before (18), but none of these proteins bound to the array with signals that were substantially higher than those for Q226K/L/R alone (Fig. 2C). Such a low signal was observed before with Q226L and G228S (18). We then added the T160A substitution to the two substitutions at positions 226 and 228, as removal of the N-glycan by the T160A substitution was previously shown to cause an increase in receptor binding avidities (18, 47). Indeed, we now observed binding to the N-glycans printed on the array for the Q226L G228S T160A mutant previously identified in ferret transmission studies (24) and the novel designed Q226R G228S T160A, but not when a lysine was present at position 226. When a leucine was present at position 226, we observed binding to both avian- and human-type receptors. However, binding was still restricted to α2,3-linked sialic acids with 226R.
Besides position 226, we investigated combinations of substitutions with the R193M substitution that was identified during the human infections included in this study. Substitutions at position 193 can be important for receptor specificity when combined with other substitutions within the RBS; therefore, the novel substitution R193M was combined with substitutions at positions 226 and 228. Specific human-type receptor binding was observed for Q226L G228S when combined with R193M. In contrast, when the R193M substitution was combined with an arginine or lysine at position 226, these mutant proteins did not show any responsiveness on the array.
Finally, we decided to add N224K in the Q226K/L/R backgrounds, because human-type receptor specificity has been reported for the double mutant N224K Q226L (25). As previously shown, this mutant specifically bound to human-type receptor, but again, the Q226K and Q226R variants did not bind to the array when combined with N224K. From this we conclude that although H5 viruses with different amino acid substitutions at position 226 can arise in humans, only viruses with 226L were able to bind to sialic acid receptors when combined with other adaptation substitutions. Other substitutions within the RBS of H5N1 did not result in a switch to human-type receptor specificity, although we cannot exclude that other combinations of substitutions might be required.
Single amino acid substitutions have different effects on viral fitness.
As single substitutions within the RBS do not result in a switch to human-type receptor specificity and, rather, a combination of multiple substitutions is required, it is important to know what the effects of these single substitutions are on virus fitness to provide insight in the evolutionary barriers for the selection of these intermediate states.
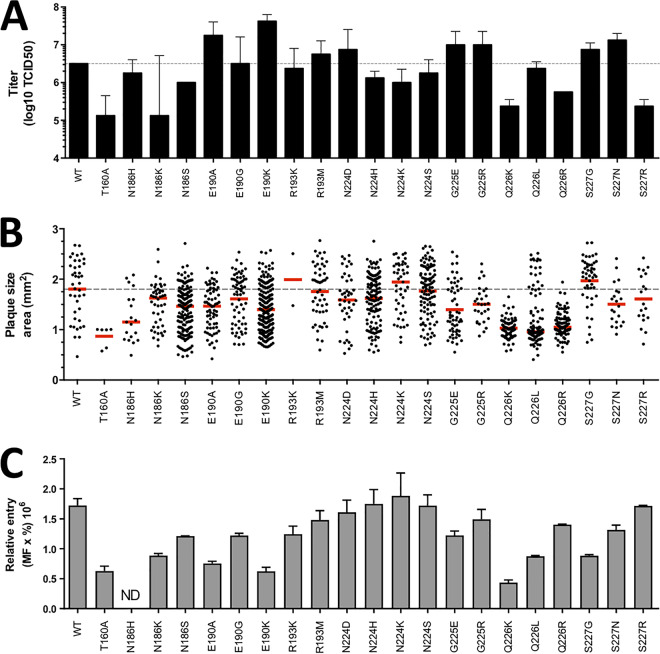
Virus fitness of selected mutant viruses was examined in multicycle replication assays, plaque assays, and virus entry assays. To analyze the replication capacity of mutant viruses, MDCK cells were inoculated with a low multiplicity of infection (MOI; 0.01) and virus titers were determined 24 h later (Fig. 3A). All viruses replicated in MDCK cells, but several mutant viruses (T160A, N186K, Q226K, and S227R mutants) showed 10- to 30-fold lower titers than WT virus. In contrast, viruses E190A and E190K showed approximately 10-fold higher virus titers than the WT. Next, plaque assays were performed to determine virus replication efficiency in a more sensitive way, with larger plaque sizes corresponding to increased efficiency in multicycle replication (48). Plaques displayed a large distribution in size, for which median values were calculated (Fig. 3B). In this assay, most viruses exhibited lower replicative fitness than the WT virus, as indicated by smaller median plaque sizes. Viruses T160A, N186H, and Q226K/L/R showed the lowest replication and virus spread, with reductions of median plaque size of 30% to 50%. No single substitution yielded a statistically significant increase in plaque size (unpaired t test). To further investigate the effect of the introduced substitutions on HA function, we indirectly quantified virus entry by inoculating MDCK cells and staining infected cells (Fig. 3C). In this assay, primarily differences in virus entry efficiency were measured and clearly showed that most substitutions in the RBS investigated in this study resulted in reduced entry efficiency.
FIG 3.
Replication capacity of HPAI A/H5N1 virus containing substitutions within the receptor binding site. (A) Virus replication on MDCK cells. Virus titers were measured 24 h postinoculation. Mean titers and standard deviations are indicated from two independent replicates. (B) Plaque assays were performed to determine virus replication efficiency in a more sensitive way, with larger plaque sizes corresponding to more efficient virus replication. The plaque radius (in millimeters) is shown. All data measurements are indicated by individual data points. (C) Quantification of virus entry 6 h postinfection by staining intracellular levels of NP. Percentage of positive cells multiplied by mean fluorescence is shown. Mean values and standard deviations are indicated from two independent replicates. ND, not determined.
Taken together, these data show that all genetic variants observed in the RBS resulted in viable virus, but entry function and overall virus replication were reduced for most of them, most consistently for T160A, N186K, and Q226K/R mutants in all three assays and E190A/G/K, Q226L, and S227G/N mutants in the more sensitive plaque and entry assays. Substitutions at positions 193 and 224 had relatively modest effects on viral fitness. Thus, although the negative impact on HA function was relatively minor for some substitutions, most variants investigated indicated that single amino acid substitutions in the RBS are deleterious for the virus.
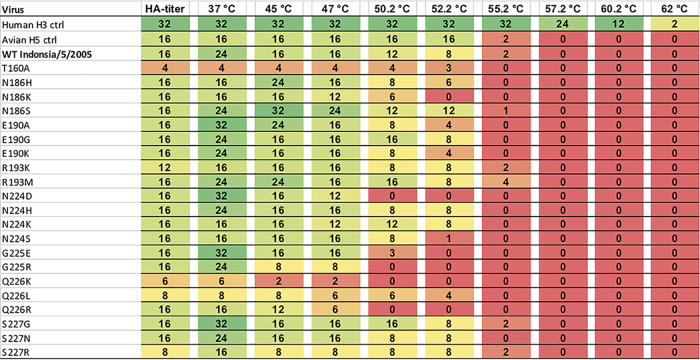
Substitutions in the RBS destabilize the H5 HA.
It was previously shown that HA stability is important for airborne transmission of influenza viruses and that substitutions in the RBS of HA can hamper stability (6). To investigate this further, we characterized the temperature stability of the RBS mutant viruses. Viruses were incubated for 30 min at a range of temperatures and residual hemagglutination titers were measured and compared to those of virus incubated at 4°C. Not all viruses replicated to high hemagglutination titers; therefore, initial titers differed between mutant viruses. As previously shown, a control human H3 virus was more stable upon incubation at increasing temperatures than an avian H5 control virus (Fig. 4) (47). In general, RBS mutant viruses showed similar or decreased temperature stability compared to that of WT virus. Especially, substitutions in the 220-loop had a profound effect on stability, decreasing the HA stability with 5°C to 8°C. None of the substitutions resulted in a substantial increase in HA stability. Therefore, amino acid substitutions in the 220-loop that conferred human-type receptor specificity likely need to be accommodated by compensatory substitutions that stabilize HA.
FIG 4.
Mutations within the RBS of H5N1 viruses generally reduce thermal stability. Residual hemagglutination titers were measured after 30-min incubations at a range of temperatures. Residual hemagglutination titers of RBS mutant viruses. The first column represents the titer before incubations, and subsequent columns show residual hemagglutination units (HAU) after incubation at the indicated temperature. Representative values from two independent experiments are presented.
DISCUSSION
Estimating the risk of an avian influenza virus to cause a pandemic is difficult due to limited understanding of the evolutionary requirements of H5N1 viruses to cross the species barrier and adapt to humans. Here, we focused on the detailed characterization of genetic diversity within the RBS of H5N1 HA during human infection as measured by NGS analyses (9) and the effects on receptor binding preferences, HA stability, and replication in mammalian cells as key requirements for human adaptation.
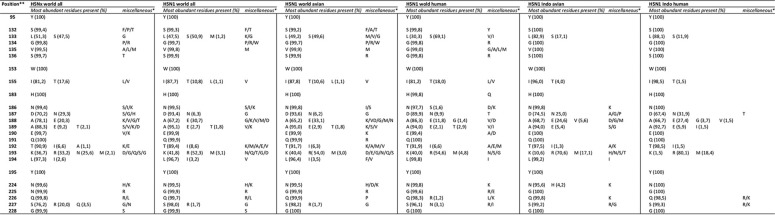
In general, the RBS of H5 HA is very conserved for all H5Nx viruses worldwide, including both human and avian H5N1 viruses (Table 3) (https://www.gisaid.org/). Despite this relative conservation on a consensus level, high genetic variability during human infections was observed when including minority variants (9). Unfortunately, limited sequencing data were available for the residues within the 130-loop of the RBS, because primers used for genome amplification prior to NGS overlap this part of HA. However, it was noted that the 130-loop was especially conserved compared to other domains in the RBS when analyzing available H5 sequences from databases (Table 3).
TABLE 3.
Genetic conservation of the H5 HA receptor binding site
H3 numbering of the mature protein.
Prevalence of 0.1% to 1% in the GISAID database (https://www.gisaid.org).
Several of the observed variants in the NGS study by Welkers et al. (9) appeared at residues of the RBS previously indicated to be important for airborne transmission in the ferret model (24, 25). However, we often identified novel amino acid substitutions compared to the ones previously described in these and other H5 studies (14, 23–25). We found that previously identified single amino acid changes in the RBS, as well as the novel variants described here, did not alter receptor specificity toward the human receptor by themselves. Rather, a combination of multiple amino acid substitutions was necessary to obtain human-type receptor specificity.
Interestingly, several other substitutions at position Q226 were observed than the human adaptive substitution Q226L. Q226L is a known amino acid substitution essential to confer a switch from avian- to human-type receptor specificity in multiple relevant subtypes. For example, for the human H3N2 virus, Q226L was indispensable, together with several other changes in HA (17). After several decades of being fixed, position 226 became a V and now is an I, which was probably only possible due to other epistatic substitutions, as single amino acid substitutions at position 226 are hardly viable (21, 49). Although we were able to rescue the single mutants, including those at position 226, many mutant viruses demonstrated severely diminished titers, plaque sizes, and entry. Substitutions at position 226, including Q226L, demonstrated severe diminished binding to N-linked glycans. A combination of substitutions was able to improve the binding to N-linked glycans in the glycan array; however, H5 HA mutants containing Q226R or Q226K still only showed low signal in the glycan array, despite the presence of 2 additional substitutions that increased binding of the Q226L mutant HA.
Others also observed the 226R/K substitutions during human infection (35, 40, 50): 226R was also observed during contact transmission studies of chickens that were infected with the aerosol transmittable H5N1 virus containing Q226L/G228S (29). Richard et al. (29) showed that besides substitutions PB2-E627K, HA substitutions Q226L and G228S caused substantial attenuation in chickens. This attenuation resulted in delayed mortality and diminished transmission and resulted in either reversion to 226Q or the selection of 226R (in a mixture with 226Q) (29). The selection of 226R in humans, or the biochemically similar 226K from an avian virus containing 226Q or from an adapted virus containing 226L in chickens, could suggest that 226R functions as an intermediate during the receptor specificity switch despite the lack of a clear phenotype toward human-type receptors in the assays described here. This intermediate genotype could either further mutate at the same position toward other codons or needs additional substitutions elsewhere in the RBS, currently still unknown. The significance of the selection of such an intermediate, with reduced binding to avian receptors in the absence of increased preference for human receptors, is not immediately apparent. However, there have been speculations about a possible explanation or functional role for such an intermediate phenotype. First, the glycan array might not contain the appropriate glycan structures preferred by the HA of interest, missing the preference for either human- or avian-type receptors. Alternatively, loss of binding to α-2,3-linked sialic acid receptors may benefit efficient viral replication in the human respiratory tract by evading the inhibitory effects of glycans present in mucins in the human respiratory tract (51, 52).
Our data, combined with the previous findings regarding the combination of 2 or even more substitutions within the RBS of zoonotic influenza viruses required for a switch toward the human-type receptor, indicate a high genetic barrier to establish full α-2,6-linked sialic acid preference. Other combinations of previously identified substitutions, as well as combinations of substitutions from this study, should be studied to further explore which combinations of substitutions may lead to a switch toward the human-type receptor. Other HA backgrounds, from other genetic clades, can be included to address the importance of substitutions outside the RBS for the characteristics presented (32, 53).
In addition, our study showed that many substitutions within the RBS lead to a less stable HA. Therefore, compensatory substitutions elsewhere in the HA trimer are probably necessary to compensate for the loss in stability due to substitutions in the RBS to obtain a fully functional and transmittable phenotype. This was previously shown in two ferret studies that investigated H5N1 virus transmission, leading to the identification of two different ways to obtain increased stability, by natural selection of substitutions in two different domains important for HA trimerization (24, 25). This requirement would therefore further increase the genetic threshold of HA toward a pandemic outbreak of H5N1 in addition to the genetic barrier to obtain recognition of the human-type receptor. However, long-term infections in immunocompromised patients could result in the accumulation of such substitutions. In addition, fitness-neutral or -positive substitutions could circulate in poultry, as is the case for the human-adaptive PB2-E627K substitution. Similarly, substitutions within HA that play roles in stability and receptor specificity could be more or less fit in poultry, allowing stepwise accumulation of such substitutions (29), although it is not known how likely such a scenario would be.
In conclusion, we found substantial genetic diversity in the RBS of H5N1 viruses during human infections, including novel variations at positions previously shown to be important for receptor specificity. Most substitutions in the RBS resulted in viable virus; however, virus replication, entry, and stability were often diminished. Interestingly, none of the observed substitutions resulted in a switch in receptor specificity from avian-like to human-like.
MATERIALS AND METHODS
Clinical samples of human influenza A/H5N1 infection receptor binding site variant selection.
As part of the national procedure for avian influenza case investigation in Indonesia, respiratory specimens were collected from suspected H5N1 cases and sent to the national reference laboratory for influenza at the National Institute of Health Research and Development (NIHRD) in Jakarta. Because Indonesian clinical specimens are obtained from suspected H5N1 cases as part of the national outbreak procedure for HPAI A/H5N1 case investigations, requirement for informed consent has been waived by the Indonesian Ministry of Health. Seventy-one respiratory tract specimens from 44 patients who were diagnosed with A/H5N1 infection between 2006 and 2011 were previously analyzed by next-generation sequencing (9). Based on the sequencing data, all variants above a cutoff of 1% and at least 5 independent sequencing reads within the RBS of HA were selected for further phenotypic characterization.
Viruses.
A/Indonesia/5/2005 HA and NA genes were available in the bidirectional reverse genetics plasmid pHW2000 as described (31), as were the internal genes for A/Puerto Rico/8/1934 (PR8). To be able to work at biosafety level 2 (BSL2) laboratories, the multibasic cleavage site was removed and replaced by a low-pathogenic monobasic cleavage site as described (31). Substitutions of interest were introduced into A/Indonesia/5/2005 HA using the QuikChange II site-directed mutagenesis kit (Agilent). Recombinant viruses were rescued by reverse genetics upon transfection of 293T cells as previously described (54). Virus stocks were propagated in MDCK cells and titrated on MDCK cells as described below.
Titrations.
MDCK cells were inoculated with 10-fold serial dilutions of virus stocks. The cells were washed with phosphate-buffered saline (PBS) 1 h after inoculation and cultured in infection medium consisting of Eagle’s minimum essential medium (EMEM) supplemented with 100 IU/ml penicillin, 100 IU/ml streptomycin, 2 mM l-glutamine (Gibco), 0.15% sodium bicarbonate (Gibco), 10 mM HEPES (Gibco), 1% nonessential amino acids (NEAA; Gibco), and 1 μg/ml N-tosyl-l-phenylalanine chloromethyl ketone (TPCK)-treated trypsin (Sigma), incubated at 37°C and 5% CO2. Three days after inoculation, supernatants of cell cultures were tested for agglutinating activity using turkey red blood cells (tRBCs) as an indicator of virus replication. Infectious virus titers were calculated by the method of Reed and Muench (55).
Viral replication kinetics.
MDCK cells were infected with a multiplicity of infection (MOI) of 0.01 (50% tissue culture infective dose [TCID50]/cell) for 1 h. The cells were washed with phosphate-buffered saline (PBS) 1 h after inoculation and cultured in infection medium consisting of EMEM supplemented with 100 IU/ml penicillin, 100 IU/ml streptomycin, 2 mM l-glutamine (Gibco), 0.15% sodium bicarbonate (Gibco), 10 mM HEPES (Gibco), 1% NEAA (Gibco), and 1 μg/ml TPCK-treated trypsin (Sigma), incubated at 37°C and 5% CO2. Supernatant was harvested at 24 h postinoculation. Viral titers were determined by titration on MDCK cells as described above.
Plaque assay.
The assay was performed as described previously (56). In brief, recombinant wild-type (WT) and mutant viruses were used to inoculate an ∼90% monolayer of MDCK cells in 6-well plates. Cells were washed twice with PBS, and 1 ml of infection medium was added to each well. One hundred microliters of diluted virus stock was added to each well in 6 technical replicates to obtain a plaque density of ∼10 plaques per well. After incubation for 1 h at 37°C and 5% CO2, cells were washed with PBS once, and 4 ml of an overlay containing 2× EMEM (Lonza) and Avicel (FMC BioPolymer, Newark, DE, USA) in a 1:1 ratio was added. Plates were incubated at 37°C and 5% CO2. After 24 h, cells were washed with PBS twice and 1 ml of 80% acetone was added. Plates were incubated at −20°C overnight, and virus infection was determined by NP antibody staining. Briefly, NP monoclonal antibody (IgG2a, clone Hb65; American Type Culture Collection, Wesel, Germany) and goat-anti-mouse Ig fluorescein isothiocyanate (FITC; BD biosciences, USA) antibodies were used to detect NP-positive cells. The plaques were scanned using a Typhoon scanner (GE Healthcare, Diegem, Belgium), and plaque size was calculated using ImageQuant.
Entry assay.
The assay was performed as described previously (48). In short, MDCK cells were plated in a 24-well plate 1 day prior to the experiment to obtain a confluent culture. Cells were inoculated with WT and mutant viruses at an MOI of 0.1 (TCID50/cells) and incubated at 37°C and 5% CO2 for 6 h. The cells were washed with PBS once, and 250 μl of 0.05% trypsin-EDTA (Life Technologies, Bleiswijk, the Netherlands) was added to the cells and incubated at 37°C. After 5 to 10 min of incubation, the cells were transferred to a tube containing PBS-1% fetal calf serum (FCS) and centrifuged for 5 min at 1,500 rpm. Next, the cells were resuspended in 200 μl PBS-1% FCS and transferred to a 96-well v-bottom plate (Corning Life Sciences, Amsterdam, the Netherlands). The plate containing all the samples was centrifuged for 5 min at 1,500 rpm and 4°C. The cells were resuspended in 100 μl of Cytofix/Cytoperm (BD Biosciences, Breda, the Netherlands) and incubated on ice for 20 min. Subsequently, the plate was centrifuged for 5 min at 500 × g and 4°C, and the cells were resuspended in 100 μl Perm/wash buffer (BD Biosciences). The plates were stored overnight at 4°C in the dark. The next day, the cells were stained for NP as described previously (57). Primary antibodies against NP (IgG2A, clone Hb65; ATCC) were used at a 10- to 20-μg/ml dilution in Perm/wash buffer. Secondary polyclonal rabbit anti-mouse immunoglobulins-FITC (Dako/Agilent) were diluted 1:100 in Perm/wash buffer. NP-positive cells and mean fluorescence were measured by flow cytometry on a FACS Canto (BD Biosciences, Breda, the Netherlands). The data were analyzed using FACSDiva software (BD Biosciences).
HA stability assay.
The assay was performed as described previously (47). In short, viruses were incubated for 30 min at different temperatures between 37°C and 62°C before performing an HA assay using tRBCs. Twofold dilutions of virus in PBS containing 0.25% red blood cells were prepared in a U-shaped 96-well plate and were incubated for 1 h at 4°C and agglutination was recorded. HA titers were compared to those of virus incubated at 4°C.
Modified tRBC hemagglutination assay.
Modified tRBCs were prepared with modifications as described previously (31). Briefly, all α2,3-, α2,6-, α2,8-, and α2,9-linked sialic acid (SAs) were removed from the surfaces of tRBCs by incubating 20% tRBCs in PBS with 50 mU Vibrio cholerae NA (VCNA; Roche) in 8 mM calcium chloride at 37°C for 1 h. Removal of sialic acids was confirmed by a complete loss of hemagglutination of the tRBCs (Table 2). Subsequently, resialylation was performed using 0.5 mU of α2,3-(N)-sialyltransferase (Sigma) or 2 mU of α2,6-(N)-sialyltransferase (Sigma) and 1.5 mM CMP-sialic acid (Merck) at 37°C for 2 h to produce α2,3-tRBC and α2,6-tRBC, respectively. After a washing step, the tRBCs were resuspended in PBS containing 1% bovine serum albumin to a final concentration of 0.5% tRBCs. Resialylation was confirmed by hemagglutination of viruses with known receptor specificity, human H3N2 and avian H5N1. The receptor specificity of mutant viruses was tested by performing a standard HA assay with untreated tRBCs, VCNA-treated tRBCs, and the modified tRBCs. Serial 2-fold dilutions of virus in PBS were made in a 50-μl volume; 50 μl of 0.5% tRBCs was added, followed by incubation for 1 h at 4°C before determining the hemagglutination titer.
Expression, purification, and glycan array analysis of recombinant soluble trimeric H5 proteins.
pCD5 plasmids were used which contained an HA sequence originating from A/Indonesia/05/05 H5N1 as previously described. pCD5-H5/IN/05/05 GCN4-TEV-sfGFP plasmid encodes a GCN4 leucine zipper trimerization motif, RMKQIEDKIEEIESKQKKIENEIARIKK, followed by a seven-amino-acid cleavage recognition sequence (ENLYFQG) of tobacco etch virus (TEV) and an sfGFP fused to a Strep-tag II (WSHPQFEKGGGSGGGSWSHPQFEK; IBA, Germany) C terminally (44). pCD5-A/Indonesia/05/05-GCN4-sfGFP expression vectors were transfected into HEK293S GNT1(-) cells (which are modified HEK293S cells lacking glucosaminyltransferase I activity [ATCC CRL-3022]) with polyethyleneimine I (PEI) in a 1:8 ratio (micrograms DNA/micrograms PEI) as previously described. The transfection mix was replaced after 6 h by 293 SFM II suspension medium (11686029 [Invitrogen], supplemented with 2.0 g/liter glucose, 3.6 g/liter sodium bicarbonate, 3.0 g/liter Primatone [Kerry], 1% GlutaMAX [Gibco], 1.5% dimethyl sulfoxide [DMSO], and 2 mM valproic acid). Culture supernatants were harvested 5 days posttransfection. The HA expression was analyzed with SDS-PAGE followed by Western blotting on a polyvinylidene difluoride (PVDF) membrane (Bio-Rad) using α-Strep-tag mouse antibodies (1:3,000; IBA Life Sciences). Subsequently, HA proteins were purified with Sepharose Strep-Tactin beads (IBA Life Sciences) as previously described. Purified, soluble trimeric HA was directly applied to the array or precomplexed with horseradish peroxidase (HRP)- or Alexa Fluor 647-linked α-Strep-tag mouse antibody and with HRP- or Alexa Fluor 647-linked α-mouse IgG (4:2:1 molar ratio) prior to incubation for 15 min on ice in 100 μl PBS with Tween 20 (PBS-T) and incubated on the array surface in a humidified chamber for 90 min. Slides were subsequently washed by successive rinses with PBS-T, PBS, and deionized water. Washed arrays were dried by centrifugation and immediately scanned for Alexa 647 signal on an Innopsys confocal microarray scanner. Fluorescent signal intensity was measured using InnoScan software and processed with an in-house-developed Excel macro. Mean total intensity was calculated and graphed using MS Excel and GraphPad Prism. For each glycan, the mean signal intensity was calculated from 6 replicates spots. The highest and lowest signals of the 6 replicates were removed, and the remaining 4 replicates were used to calculate the mean signal and standard deviation (SD).
ACKNOWLEDGMENTS
We thank Lard Montessori and Lieke de Jong for technical assistance.
D.E. is a recipient of a European Union H2020 Marie Curie International Incoming Fellowship. R.A.M.F. is supported by NIAID/NIH contract HHSN272201400008C. J.C.P. is supported by NIH Grant AI114730. R.P.D.V. is supported by an ERC starting grant and a Beijerinck Premium of the Royal Dutch Academy of Sciences (KNAW; 802780). C.A.R. is supported by an ERC consolidator grant. Synthesis and microarray analysis were funded by a grant from the Netherlands Organization for Scientific Research (NWO TOPPUNT 718.015.003) to G.-J.B.
REFERENCES
- 1.Kandun IN, Wibisono H, Sedyaningsih ER, Yusharmen, Hadisoedarsuno W, Purba W, Santoso H, Septiawati C, Tresnaningsih E, Heriyanto B, Yuwono D, Harun S, Soeroso S, Giriputra S, Blair PJ, Jeremijenko A, Kosasih H, Putnam SD, Samaan G, Silitonga M, Chan KH, Poon LL, Lim W, Klimov A, Lindstrom S, Guan Y, Donis R, Katz J, Cox N, Peiris M, Uyeki TM. 2006. Three Indonesian clusters of H5N1 virus infection in 2005. N Engl J Med 355:2186–2194. doi: 10.1056/NEJMoa060930. [DOI] [PubMed] [Google Scholar]
- 2.Ungchusak K, Auewarakul P, Dowell SF, Kitphati R, Auwanit W, Puthavathana P, Uiprasertkul M, Boonnak K, Pittayawonganon C, Cox NJ, Zaki SR, Thawatsupha P, Chittaganpitch M, Khontong R, Simmerman JM, Chunsutthiwat S. 2005. Probable person-to-person transmission of avian influenza A (H5N1). N Engl J Med 352:333–340. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 3.Wang H, Feng Z, Shu Y, Yu H, Zhou L, Zu R, Huai Y, Dong J, Bao C, Wen L, Wang H, Yang P, Zhao W, Dong L, Zhou M, Liao Q, Yang H, Wang M, Lu X, Shi Z, Wang W, Gu L, Zhu F, Li Q, Yin W, Yang W, Li D, Uyeki TM, Wang Y. 2008. Probable limited person-to-person transmission of highly pathogenic avian influenza A (H5N1) virus in China. Lancet 371:1427–1434. doi: 10.1016/S0140-6736(08)60493-6. [DOI] [PubMed] [Google Scholar]
- 4.de Wit E, Kawaoka Y, de Jong MD, Fouchier RA. 2008. Pathogenicity of highly pathogenic avian influenza virus in mammals. Vaccine 26 (Suppl 4):D54–D58. doi: 10.1016/j.vaccine.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Graaf M, Fouchier RA. 2014. Role of receptor binding specificity in influenza A virus transmission and pathogenesis. EMBO J 33:823–841. doi: 10.1002/embj.201387442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imai M, Herfst S, Sorrell EM, Schrauwen EJ, Linster M, De Graaf M, Fouchier RA, Kawaoka Y. 2013. Transmission of influenza A/H5N1 viruses in mammals. Virus Res 178:15–20. doi: 10.1016/j.virusres.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Massin P, van der Werf S, Naffakh N. 2001. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J Virol 75:5398–5404. doi: 10.1128/JVI.75.11.5398-5404.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao Y, Zhang Y, Shinya K, Deng G, Jiang Y, Li Z, Guan Y, Tian G, Li Y, Shi J, Liu L, Zeng X, Bu Z, Xia X, Kawaoka Y, Chen H. 2009. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog 5:e1000709. doi: 10.1371/journal.ppat.1000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welkers MRA, Pawestri HA, Fonville JM, Sampurno OD, Pater M, Holwerda M, Han AX, Russell CA, Jeeninga RE, Setiawaty V, de Jong MD, Eggink D. 2019. Genetic diversity and host adaptation of avian H5N1 influenza viruses during human infection. Emerg Microbes Infect 8:262–271. doi: 10.1080/22221751.2019.1575700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arai Y, Kawashita N, Daidoji T, Ibrahim MS, El-Gendy EM, Takagi T, Takahashi K, Suzuki Y, Ikuta K, Nakaya T, Shioda T, Watanabe Y. 2016. Novel polymerase gene mutations for human adaptation in clinical isolates of avian H5N1 influenza viruses. PLoS Pathog 12:e1005583. doi: 10.1371/journal.ppat.1005583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manz B, de Graaf M, Mogling R, Richard M, Bestebroer TM, Rimmelzwaan GF, Fouchier R. 2016. Multiple natural substitutions in avian influenza A virus PB2 facilitate efficient replication in human cells. J Virol 90:5928–5938. doi: 10.1128/JVI.00130-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, Kuiken T. 2006. H5N1 virus attachment to lower respiratory tract. Science 312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 13.Rogers GN, Pritchett TJ, Lane JL, Paulson JC. 1983. Differential sensitivity of human, avian, and equine influenza A viruses to a glycoprotein inhibitor of infection: selection of receptor specific variants. Virology 131:394–408. doi: 10.1016/0042-6822(83)90507-x. [DOI] [PubMed] [Google Scholar]
- 14.Paulson JC, de Vries RP. 2013. H5N1 receptor specificity as a factor in pandemic risk. Virus Res 178:99–113. doi: 10.1016/j.virusres.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matrosovich M, Tuzikov A, Bovin N, Gambaryan A, Klimov A, Castrucci MR, Donatelli I, Kawaoka Y. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J Virol 74:8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers GN, Paulson JC. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127:361–373. doi: 10.1016/0042-6822(83)90150-2. [DOI] [PubMed] [Google Scholar]
- 17.Van Poucke S, Doedt J, Baumann J, Qiu Y, Matrosovich T, Klenk HD, Van Reeth K, Matrosovich M. 2015. Role of substitutions in the hemagglutinin in the emergence of the 1968 pandemic influenza virus. J Virol 89:12211–12216. doi: 10.1128/JVI.01292-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peng W, Bouwman KM, McBride R, Grant OC, Woods RJ, Verheije MH, Paulson JC, de Vries RP. 2018. Enhanced human-type receptor binding by ferret-transmissible H5N1 with a K193T mutation. J Virol 92:e02016-17. doi: 10.1128/JVI.02016-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Vries RP, Peng W, Grant OC, Thompson AJ, Zhu X, Bouwman KM, de la Pena ATT, van Breemen MJ, Ambepitiya Wickramasinghe IN, de Haan CAM, Yu W, McBride R, Sanders RW, Woods RJ, Verheije MH, Wilson IA, Paulson JC. 2017. Three mutations switch H7N9 influenza to human-type receptor specificity. PLoS Pathog 13:e1006390. doi: 10.1371/journal.ppat.1006390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tzarum N, de Vries RP, Peng W, Thompson AJ, Bouwman KM, McBride R, Yu W, Zhu X, Verheije MH, Paulson JC, Wilson IA. 2017. The 150-loop restricts the host specificity of human H10N8 influenza virus. Cell Rep 19:235–245. doi: 10.1016/j.celrep.2017.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin YP, Xiong X, Wharton SA, Martin SR, Coombs PJ, Vachieri SG, Christodoulou E, Walker PA, Liu J, Skehel JJ, Gamblin SJ, Hay AJ, Daniels RS, McCauley JW. 2012. Evolution of the receptor binding properties of the influenza A(H3N2) hemagglutinin. Proc Natl Acad Sci U S A 109:21474–21479. doi: 10.1073/pnas.1218841110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng W, de Vries RP, Grant OC, Thompson AJ, McBride R, Tsogtbaatar B, Lee PS, Razi N, Wilson IA, Woods RJ, Paulson JC. 2017. Recent H3N2 viruses have evolved specificity for extended, branched human-type receptors, conferring potential for increased avidity. Cell Host Microbe 21:23–34. doi: 10.1016/j.chom.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. 2012. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology 422:105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imai M, Kawaoka Y. 2012. The role of receptor binding specificity in interspecies transmission of influenza viruses. Curr Opin Virol 2:160–167. doi: 10.1016/j.coviro.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mair CM, Ludwig K, Herrmann A, Sieben C. 2014. Receptor binding and pH stability - how influenza A virus hemagglutinin affects host-specific virus infection. Biochim Biophys Acta 1838:1153–1168. doi: 10.1016/j.bbamem.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 28.Russell CA, Fonville JM, Brown AE, Burke DF, Smith DL, James SL, Herfst S, van Boheemen S, Linster M, Schrauwen EJ, Katzelnick L, Mosterin A, Kuiken T, Maher E, Neumann G, Osterhaus AD, Kawaoka Y, Fouchier RA, Smith DJ. 2012. The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science 336:1541–1547. doi: 10.1126/science.1222526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richard M, Herfst S, van den Brand JMA, de Meulder D, Lexmond P, Bestebroer TM, Fouchier R. 2017. Mutations driving airborne transmission of A/H5N1 virus in mammals cause substantial attenuation in chickens only when combined. Sci Rep 7:7187. doi: 10.1038/s41598-017-07000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ayora-Talavera G, Shelton H, Scull MA, Ren J, Jones IM, Pickles RJ, Barclay WS. 2009. Mutations in H5N1 influenza virus hemagglutinin that confer binding to human tracheal airway epithelium. PLoS One 4:e7836. doi: 10.1371/journal.pone.0007836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chutinimitkul S, van Riel D, Munster VJ, van den Brand JM, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA, de Wit E. 2010. In vitro assessment of attachment pattern and replication efficiency of H5N1 influenza A viruses with altered receptor specificity. J Virol 84:6825–6833. doi: 10.1128/JVI.02737-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gambaryan A, Tuzikov A, Pazynina G, Bovin N, Balish A, Klimov A. 2006. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 344:432–438. doi: 10.1016/j.virol.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 33.Gao R, Gu M, Liu K, Li Q, Li J, Shi L, Li X, Wang X, Hu J, Liu X, Hu S, Chen S, Peng D, Jiao X, Liu X. 2018. T160A mutation-induced deglycosylation at site 158 in hemagglutinin is a critical determinant of the dual receptor binding properties of clade 2.3.4.4 H5NX subtype avian influenza viruses. Vet Microbiol 217:158–166. doi: 10.1016/j.vetmic.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 34.Han P, Hu Y, Sun W, Zhang S, Li Y, Wu X, Yang Y, Zhu Q, Jiang T, Li J, Qin C. 2015. Mouse lung-adapted mutation of E190G in hemagglutinin from H5N1 influenza virus contributes to attenuation in mice. J Med Virol 87:1816–1822. doi: 10.1002/jmv.24257. [DOI] [PubMed] [Google Scholar]
- 35.Imai H, Dinis JM, Zhong G, Moncla LH, Lopes TJS, McBride R, Thompson AJ, Peng W, Le MTQ, Hanson A, Lauck M, Sakai-Tagawa Y, Yamada S, Eggenberger J, O'Connor DH, Suzuki Y, Hatta M, Paulson JC, Neumann G, Friedrich TC, Kawaoka Y. 2018. Diversity of influenza A(H5N1) viruses in infected humans, northern Vietnam, 2004–2010. Emerg Infect Dis 24:1128–1238. doi: 10.3201/eid2407.171441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stevens J, Blixt O, Chen LM, Donis RO, Paulson JC, Wilson IA. 2008. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J Mol Biol 381:1382–1394. doi: 10.1016/j.jmb.2008.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stevens J, Blixt O, Glaser L, Taubenberger JK, Palese P, Paulson JC, Wilson IA. 2006. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J Mol Biol 355:1143–1155. doi: 10.1016/j.jmb.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 38.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 39.Watanabe Y, Arai Y, Daidoji T, Kawashita N, Ibrahim MS, El-Gendy EE-DM, Hiramatsu H, Kubota-Koketsu R, Takagi T, Murata T, Takahashi K, Okuno Y, Nakaya T, Suzuki Y, Ikuta K. 2015. Characterization of H5N1 influenza virus variants with hemagglutinin mutations isolated from patients. mBio 6:e00081-15. doi: 10.1128/mBio.00081-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watanabe Y, Arai Y, Kawashita N, Ibrahim MS, Elgendy EM, Daidoji T, Kajikawa J, Hiramatsu H, Sriwilaijaroen N, Ono T, Takagi T, Takahashi K, Shioda T, Matsumoto K, Suzuki Y, Nakaya T. 2018. Characterization of H5N1 influenza virus quasispecies with adaptive hemagglutinin mutations from single-virus infections of human airway cells. J Virol 92:e02004-17. doi: 10.1128/JVI.02004-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, Muramoto Y, Ito M, Kiso M, Horimoto T, Shinya K, Sawada T, Kiso M, Usui T, Murata T, Lin Y, Hay A, Haire LF, Stevens DJ, Russell RJ, Gamblin SJ, Skehel JJ, Kawaoka Y. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444:378–382. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
- 42.Yang ZY, Wei CJ, Kong WP, Wu L, Xu L, Smith DF, Nabel GJ. 2007. Immunization by avian H5 influenza hemagglutinin mutants with altered receptor binding specificity. Science 317:825–828. doi: 10.1126/science.1135165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu X, Viswanathan K, Raman R, Yu W, Sasisekharan R, Wilson IA. 2015. Structural basis for a switch in receptor binding specificity of two H5N1 hemagglutinin mutants. Cell Rep 13:1683–1691. doi: 10.1016/j.celrep.2015.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nemanichvili N, Tomris I, Turner HL, McBride R, Grant OC, van der Woude R, Aldosari MH, Pieters RJ, Woods RJ, Paulson JC, Boons GJ, Ward AB, Verheije MH, de Vries RP. 2019. Fluorescent trimeric hemagglutinins reveal multivalent receptor binding properties. J Mol Biol 431:842–856. doi: 10.1016/j.jmb.2018.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Broszeit F, Tzarum N, Zhu X, Nemanichvili N, Eggink D, Leenders T, Li Z, Liu L, Wolfert MA, Papanikolaou A, Martinez-Romero C, Gagarinov IA, Yu W, Garcia-Sastre A, Wennekes T, Okamatsu M, Verheije MH, Wilson IA, Boons GJ, de Vries RP. 2019. N-Glycolylneuraminic acid as a receptor for influenza A viruses. Cell Rep 27:3284.e6–3294.e6. doi: 10.1016/j.celrep.2019.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xiong X, Coombs PJ, Martin SR, Liu J, Xiao H, McCauley JW, Locher K, Walker PA, Collins PJ, Kawaoka Y, Skehel JJ, Gamblin SJ. 2013. Receptor binding by a ferret-transmissible H5 avian influenza virus. Nature 497:392–396. doi: 10.1038/nature12144. [DOI] [PubMed] [Google Scholar]
- 47.Linster M, van Boheemen S, de Graaf M, Schrauwen EJ, Lexmond P, Manz B, Bestebroer TM, Baumann J, van Riel D, Rimmelzwaan GF, Osterhaus AD, Matrosovich M, Fouchier RA, Herfst S. 2014. Identification, characterization, and natural selection of mutations driving airborne transmission of A/H5N1 virus. Cell 157:329–339. doi: 10.1016/j.cell.2014.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spronken MI, van de Sandt CE, de Jongh EP, Vuong O, van der Vliet S, Bestebroer TM, Olsthoorn RCL, Rimmelzwaan GF, Fouchier RAM, Gultyaev AP. 2017. A compensatory mutagenesis study of a conserved hairpin in the M gene segment of influenza A virus shows its role in virus replication. RNA Biol 14:1606–1616. doi: 10.1080/15476286.2017.1338243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu NC, Xie J, Zheng T, Nycholat CM, Grande G, Paulson JC, Lerner RA, Wilson IA. 2017. Diversity of functionally permissive sequences in the receptor-binding site of influenza hemagglutinin. Cell Host Microbe 21:742.e8–753.e8. doi: 10.1016/j.chom.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moncla LH, Bedford T, Dussart P, Horm SV, Rith S, Buchy P, Karlsson EA, Li L, Liu Y, Zhu H, Guan Y, Friedrich TC, Horwood PF. 2020. Quantifying within-host evolution of H5N1 influenza viruses in humans and poultry in Cambodia. PLoS Pathog 16:e1008191. doi: 10.1371/journal.ppat.1008191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Couceiro JN, Paulson JC, Baum LG. 1993. Influenza virus strains selectively recognize sialyloligosaccharides on human respiratory epithelium; the role of the host cell in selection of hemagglutinin receptor specificity. Virus Res 29:155–165. doi: 10.1016/0168-1702(93)90056-s. [DOI] [PubMed] [Google Scholar]
- 52.Baum LG, Paulson JC. 1990. Sialyloligosaccharides of the respiratory epithelium in the selection of human influenza virus receptor specificity. Acta Histochem Suppl 40:35–38. [PubMed] [Google Scholar]
- 53.Shinya K, Hatta M, Yamada S, Takada A, Watanabe S, Halfmann P, Horimoto T, Neumann G, Kim JH, Lim W, Guan Y, Peiris M, Kiso M, Suzuki T, Suzuki Y, Kawaoka Y. 2005. Characterization of a human H5N1 influenza A virus isolated in 2003. J Virol 79:9926–9932. doi: 10.1128/JVI.79.15.9926-9932.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.de Wit E, Spronken MI, Bestebroer TM, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2004. Efficient generation and growth of influenza virus A/PR/8/34 from eight cDNA fragments. Virus Res 103:155–161. doi: 10.1016/j.virusres.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 55.Reed LJ, Muench H. 1938. A simple method of estimating fifty per cent endpoints. Am J Epidemiol 27:493–497. doi: 10.1093/oxfordjournals.aje.a118408. [DOI] [Google Scholar]
- 56.Matrosovich M, Matrosovich T, Garten W, Klenk HD. 2006. New low-viscosity overlay medium for viral plaque assays. Virol J 3:63. doi: 10.1186/1743-422X-3-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Spronken MI, Short KR, Herfst S, Bestebroer TM, Vaes VP, van der Hoeven B, Koster AJ, Kremers G-J, Scott DP, Gultyaev AP, Sorell EM, de Graaf M, Bárcena M, Rimmelzwaan GF, Fouchier RA. 2015. Optimisations and challenges involved in the creation of various bioluminescent and fluorescent influenza A virus strains for in vitro and in vivo applications. PLoS One 10:e0133888. doi: 10.1371/journal.pone.0133888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang W, Shi Y, Lu X, Shu Y, Qi J, Gao GF. 2013. An airborne transmissible avian influenza H5 hemagglutinin seen at the atomic level. Science 340(6139):1463–1467. doi: 10.1126/science.1236787. [DOI] [PubMed] [Google Scholar]