EBOV and MARV, members of the family Filoviridae, are highly pathogenic zoonotic viruses that cause severe disease in humans. Both viruses use several mechanisms to modulate the host innate immune response, and these likely contribute to the severity of disease. Here, we demonstrate that MLAV, a filovirus newly discovered in a bat, suppresses antiviral type I interferon responses in both human and bat cells. Inhibitory activities are possessed by MLAV VP35 and VP40, which parallels how MARV blocks IFN responses. However, whereas MARV activates cellular antioxidant responses through an interaction between its VP24 protein and host protein Keap1, MLAV VP24 lacks a Keap1-binding motif and fails to activate this cytoprotective response. These data indicate that MLAV possesses immune-suppressing functions that could facilitate human infection. They also support the placement of MLAV in a different genus than either EBOV or MARV.
KEYWORDS: Ebola virus, Marburg virus, filovirus, interferon
ABSTRACT
Měnglà virus (MLAV), identified in Rousettus bats, is a phylogenetically distinct member of the family Filoviridae. Because the filoviruses Ebola virus (EBOV) and Marburg virus (MARV) modulate host innate immunity, MLAV VP35, VP40, and VP24 proteins were compared with their EBOV and MARV homologs for innate immune pathway modulation. In human and Rousettus cells, MLAV VP35 behaved like EBOV and MARV VP35s, inhibiting virus-induced activation of the interferon beta (IFN-β) promoter and interferon regulatory factor 3 (IRF3) phosphorylation. MLAV VP35 also interacted with PACT, a host protein engaged by EBOV VP35 to inhibit RIG-I signaling. MLAV VP35 also inhibits PKR activation. MLAV VP40 was demonstrated to inhibit type I IFN-induced gene expression in human and bat cells. It blocked STAT1 tyrosine phosphorylation induced either by type I IFN or overexpressed Jak1, paralleling MARV VP40. MLAV VP40 also inhibited virus-induced IFN-β promoter activation, a property shared by MARV VP40 and EBOV VP24. A Jak kinase inhibitor did not recapitulate this inhibition in the absence of viral proteins. Therefore, inhibition of Jak-STAT signaling is insufficient to explain inhibition of IFN-β promoter activation. MLAV VP24 did not inhibit IFN-induced gene expression or bind karyopherin α proteins, properties of EBOV VP24. MLAV VP24 differed from MARV VP24 in that it failed to interact with Keap1 or activate an antioxidant response element reporter gene due to the absence of a Keap1-binding motif. These functional observations support a closer relationship of MLAV to MARV than to EBOV but also are consistent with MLAV belonging to a distinct genus.
IMPORTANCE EBOV and MARV, members of the family Filoviridae, are highly pathogenic zoonotic viruses that cause severe disease in humans. Both viruses use several mechanisms to modulate the host innate immune response, and these likely contribute to the severity of disease. Here, we demonstrate that MLAV, a filovirus newly discovered in a bat, suppresses antiviral type I interferon responses in both human and bat cells. Inhibitory activities are possessed by MLAV VP35 and VP40, which parallels how MARV blocks IFN responses. However, whereas MARV activates cellular antioxidant responses through an interaction between its VP24 protein and host protein Keap1, MLAV VP24 lacks a Keap1-binding motif and fails to activate this cytoprotective response. These data indicate that MLAV possesses immune-suppressing functions that could facilitate human infection. They also support the placement of MLAV in a different genus than either EBOV or MARV.
INTRODUCTION
Měnglà virus (MLAV) was discovered when its genomic RNA was identified in the liver of a bat of the Rousettus genus that had been collected in Měnglà County, Yunnan Province, China (1). To date, only a nearly complete viral genomic RNA sequence is available, and viable MLAV has not yet been isolated. MLAV has been proposed to represent a new genus, Dianlovirus, within the family Filoviridae. The filovirus family includes three additional genera, Ebolavirus, Marburgvirus, and Cuevavirus, that contain viral species isolated from or identified in mammals (2). Placement of MLAV in a distinct genus was based on its comparatively low sequence identity to other filoviruses and phylogenetic and pairwise sequence comparison (PASC) analyses (1). It was also noted to have, compared to other filoviruses, unique gene overlaps and a unique transcription start signal (1). MLAV displays some features more reminiscent of Marburgvirus members than Ebolavirus members. Specifically, MLAV RNA was identified in tissue from a Rousettus bat, the same genus of bat which serves as a Marburg virus (MARV) reservoir in Africa (3). In addition, the MLAV large (L) protein exhibits closer phylogenetic relatedness to Marburgvirus L than to the L of other filoviruses, and in contrast to Ebolavirus and Cuevavirus members, MLAV can express its glycoprotein (GP) without the need for editing of the GP mRNA (1).
Filoviruses are noteworthy because of their capacity to cause severe human disease (4). Some members of the Ebolavirus and Marburgvirus genera are zoonotic pathogens that have caused repeated outbreaks with substantial lethality in humans (5). The largest such outbreak on record was caused by Zaire ebolavirus (EBOV) and occurred in West Africa between 2013 and 2016. This resulted in upwards of 28,000 infections, more than 11,000 deaths, and the export of infected cases to the United States and Europe (6). EBOV is also the cause of the second-largest filovirus outbreak, which was first recognized in August 2018 and has continued well into 2020 (www.who.int/ebola/situation-reports/drc-2018/en/). The largest outbreak of MARV occurred in Angola between 2004 and 2005 and had a reported case fatality rate of 88% (5).
Likely contributing to the virulence of filoviruses are viral-encoded proteins that target host cell innate immune signaling pathways (4). Filovirus VP35 proteins suppress interferon alpha and beta (IFN-α/β) responses that play critical roles in innate antiviral immunity (7). VP35 impairment of IFN-α/β production occurs by inhibition of RIG-I-like receptor (RLR) signaling through several mechanisms, including VP35 binding to RLR-activating double-stranded RNAs (dsRNAs) and the interaction of VP35 with PACT, a host protein that facilitates RIG-I activation (8–19). VP35s also inhibit the phosphorylation and activation of the IFN-induced kinase PKR (20–23). EBOV VP24, but not MARV VP24, interacts with the NPI-1 subfamily of karyopherin alpha (KPNA) (also known as importin alpha) nuclear transport proteins, which includes KPNA1, KPNA5, and KPNA6 (24, 25). The NPI-1 subfamily also mediates the nuclear import of STAT1 following its activation by IFN (25–27). The interaction of EBOV VP24 with KPNA competes with tyrosine-phosphorylated STAT1 (pY-STAT1), blocking pY-STAT1 nuclear import and suppressing the expression of IFN-stimulated genes (ISGs), a response that mediates the antiviral effects of IFN (24, 25, 28, 29). MARV VP40 protein has been demonstrated to suppress IFN-induced signaling and ISG expression, while EBOV VP40 has no known role in IFN antagonism (30). Activation of the Jak family of kinases associated with IFN receptors is inhibited by MARV VP40, blocking phosphorylation and activation of the downstream STAT proteins, including STAT1 (30–32). EBOV VP24 and MARV VP40 have also been described to modestly inhibit IFN-α/β production, although the mechanism(s) is not well-defined (33, 34). While MARV VP24 does not appear to block IFN responses, it has been demonstrated to interact with Kelch-like ECH-associated protein 1 (Keap1). Under homeostatic conditions, Keap1, a cellular substrate adaptor protein of the Cullin3/Rbx1 ubiquitin E3 ligase complex, targets the transcription factor nuclear factor erythroid 2-related factor 2 (Nrf2) for polyubiquitination and proteasomal degradation (35–37). MARV VP24 disrupts the Keap1-Nrf2 interaction, leading to Nrf2-induced expression of genes possessing antioxidant response elements (ARE) (35–37). This activity induces a cytoprotective state that may prolong the life of MARV-infected cells. MARV VP24 also relieves Keap1 repression of the NF-κB pathway (38).
Given the link between EBOV and MARV innate immune suppressors and virulence and the unknown potential of MLAV to cause human disease, this study sought to determine whether MLAV possesses effective suppressors of innate immunity. Because of the differences in innate immune evasion mechanisms between EBOV and MARV, it was also of interest to determine whether MLAV innate immune evasion mechanisms more closely resemble EBOV or MARV. The data demonstrate that MLAV VP35 functions as an IFN antagonist by mechanisms that mirror those of EBOV and MARV VP35. MLAV VP40 is demonstrated to act as a suppressor of IFN-induced signaling, whereas MLAV VP24 does not, mirroring the inhibitory functions of MARV. MARV and MLAV VP40 were also found to suppress activation of the IFN-β promoter. Both MLAV VP35 and VP40 effectively suppressed IFN responses in human and Rousettus cells. Interestingly, MLAV VP24 does not detectably interact with Keap1 or activate ARE gene expression due to the absence of Keap1-binding sequences found in MARV VP24. Cumulatively, the data demonstrate the presence of IFN evasion functions in MLAV that are effective in human cells, suggesting the virus may have the capacity to cause human disease. The similarities in VP40 immune evasion functions are consistent with a closer genetic relationship of MLAV to MARV than EBOV, but the differences in VP24 function are consistent with MLAV occupying a distinct genus within the filovirus family.
RESULTS
MLAV VP35 blocks virus-induced IFN-β promoter activation in both human and bat cells.
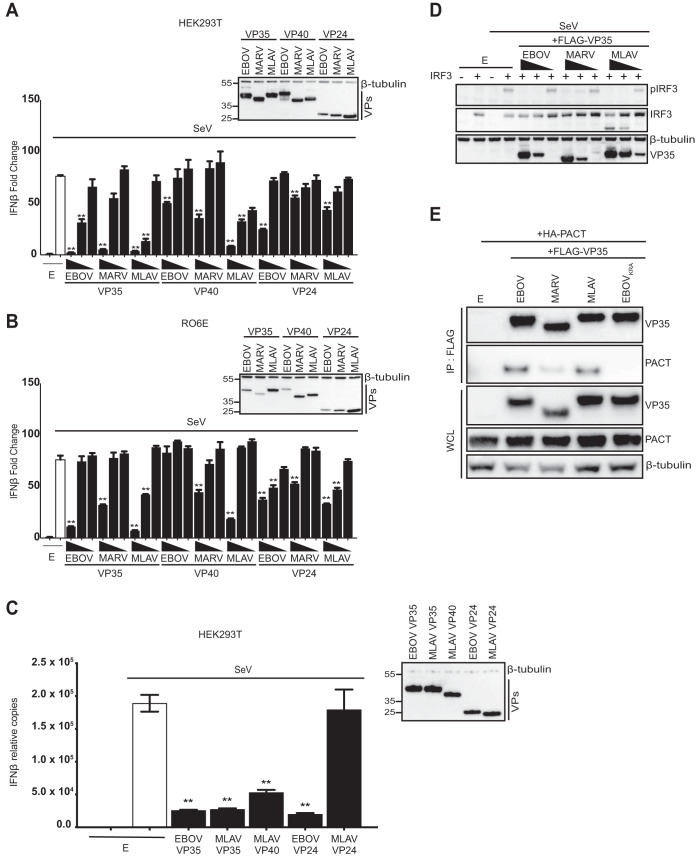
As a measure of the capacity of MLAV VP35, VP40, and VP24 to modulate type I IFN production, the human cell line HEK293T or the Rousettus bat cell line RO6E were transfected with plasmids that express these proteins to determine their effect on Sendai virus (SeV)-induced IFN-β promoter activation. Either an empty vector or FLAG-tagged expression plasmids for the VP35, VP40, and VP24 proteins of EBOV, MARV, and MLAV were cotransfected with an IFN-β promoter-firefly luciferase reporter and a constitutively expressing Renilla luciferase plasmid. Twenty-four hours posttransfection, cells were either mock infected or infected for 18 h with SeV, a potent activator of the IFN-β promoter (39). As expected, SeV infection activated the IFN-β promoter in the absence of viral protein expression. EBOV and MARV VP35 impaired IFN-β reporter activation in a dose-dependent manner in both cell lines, with EBOV exhibiting greater potency, as previously shown (Fig. 1A and B) (9, 19). Similarly, MLAV VP35 dramatically diminished IFN-β promoter activity in a dose-dependent manner (Fig. 1A and B).
FIG 1.
MLAV VP35 blocks Sendai virus-induced IFN-β promoter activation in both human and bat cells. (A) HEK293T cells were transfected with an IFN-β promoter-firefly luciferase reporter plasmid, a constitutively expressed Renilla luciferase reporter plasmid, and either an empty vector (E) or the specified FLAG-tagged viral proteins. The amounts of VP35 and VP40 plasmids were 62.5 ng, 6.25 ng, and 0.625 ng; the amounts of VP24 plasmids were 25 ng, 2.5 ng, and 0.25 ng. Twenty-four hours posttransfection, cells were either mock or Sendai virus (SeV) infected. Firefly and Renilla luciferase activities were determined 18 h postinfection using a dual-luciferase assay. Fold induction was determined relative to the vector-only, mock-infected samples. (B) RO6E cells were assayed as described above, except the amounts of EBOV and MARV VP35, VP40, and VP24 plasmids were 250 ng, 25 ng, and 2.5 ng, and the amounts of MLAV VP35, VP40, and VP24 plasmids were 125 ng, 12.5 ng, and 1.25 ng. (C) HEK293T cells were transfected with 125 ng of an empty vector or the indicated protein expression plasmids and mock or SeV infected for 18 h, and endogenous human IFN-β mRNA levels were measured and normalized to human β-actin mRNA levels. For all experiments in panels A to C, cell lysates were analyzed by Western blotting with anti-FLAG and anti-β-tubulin antibodies (insets). Experiments were performed in triplicate; error bars represent the SEM for the triplicate, and statistical significance was determined by performing a one-way ANOVA followed with Tukey multiple comparison compared to SeV-infected control (white bar). **, P < 0.0001; *, P < 0.001. VPs, viral proteins. (D) HEK293T cells were transfected with an empty vector (E) or IRF3 expression plasmid (100 ng) as indicated, and FLAG-tagged EBOV, MARV, and MLAV VP35. The amounts of VP35 plasmids were 2,000 ng, 400 ng, and 80 ng. Cells were mock or SeV infected for 4 h. Whole-cell lysates were analyzed by Western blotting with anti-pIRF3 (S396), anti-total IRF3, anti-FLAG (VP35), and anti-β-tubulin antibodies. (E) HEK293T cells were transfected with an empty vector (E) or plasmids that express FLAG-tagged EBOV VP35, MARV VP35, MLAV VP35, or dsRNA-binding mutant EBOV VP35KRA and HA-tagged PACT as indicated. Immunoprecipitation (IP) was performed with anti-FLAG antibody. Western blotting was performed for detection of VP35 (anti-FLAG antibody), PACT (anti-HA antibody), and β-tubulin. WCL, whole-cell lysate.
Expression of EBOV VP24, Lloviu virus (LLOV) VP24, or MARV VP40 has also been reported to impair IFN-β and, in the case of EBOV VP24, IFN-λ production (33, 34, 40). In the present study, in HEK293T cells, modest inhibition of IFN-β promoter activation was evident for EBOV VP24, EBOV VP40, and MARV VP40. MLAV VP40 exhibited a potent dose-dependent inhibition of IFN-β promoter activation (Fig. 1A). Weak but statistically significant inhibition of IFN-β reporter gene expression was detected for MARV VP24 and MLAV VP24; however, the biological significance of this minimal inhibition is uncertain. In RO6E cells, MLAV VP40 inhibition of IFN-β promoter activation was also detected but only at the highest concentration of transfected plasmid (Fig. 1B).
To evaluate whether or not the inhibition of the IFN-β reporter also correlates with inhibition of endogenous IFN-β gene expression, reverse transcription-quantitative PCR (qRT-PCR) assays were performed. MLAV VP35 and VP40 showed significant inhibition of IFN-β transcripts consistent with the results of the reporter assays. Expression of MLAV VP24 had no effect on IFN-β copy numbers, which may suggest that the minor inhibition observed in the luminescence assay is not biologically relevant (Fig. 1C).
EBOV and MARV VP35 inhibition of RLR signaling pathways results in inhibition of the phosphorylation and activation of transcription factor interferon regulatory factor 3 (IRF3) (8, 41, 42). In order to determine whether MLAV VP35 can inhibit activation of IRF3, HEK293T cells were cotransfected with either an empty vector or an IRF3 expression plasmid and plasmids that express FLAG-tagged EBOV, MARV, and MLAV VP35 (Fig. 1D). Twenty-four hours posttransfection, cells were either mock or SeV infected to induce IRF3 phosphorylation. Overexpression of IRF3 substantially increased the detection of the phosphorylated form. As previously reported, EBOV VP35 potently inhibited IRF3 phosphorylation. MARV VP35 also inhibited IRF3 phosphorylation, although less efficiently, consistent with less robust inhibition of RIG-I signaling compared to EBOV VP35 (9, 19). MLAV VP35 inhibited IRF3 phosphorylation comparably to EBOV VP35 (Fig. 1D).
EBOV and MARV VP35 interact with host protein PACT, and this interaction contributes to VP35 inhibition of RIG-I signaling (12, 22). To determine if MLAV VP35 might suppress IFN production through a similar mechanism, the PACT-VP35 interactions were evaluated by a coimmunoprecipitation assay (Fig. 1E). FLAG-tagged EBOV, MARV, and MLAV VP35 or empty vector expression plasmids were cotransfected with hemagglutinin (HA)-tagged PACT in HEK293T cells. A VP35 dsRNA-binding mutant (VP35KRA) that has previously been shown to lack the ability to interact with PACT was included as a negative control (12). All three wild-type VP35 proteins were demonstrated to interact with PACT, with MLAV VP35 interacting comparably to EBOV VP35 (Fig. 1E). Together, these data suggest that MLAV VP35 employs mechanisms similar to EBOV and MARV VP35 for inhibition of RIG-I-dependent activation of type I IFN responses and that the potency of inhibition is similar to EBOV VP35.
MLAV VP35 protein inhibits phosphorylation of PKR in human cells.
To assess whether MLAV VP35 can inhibit activation of PKR, HEK293T cells were transfected with FLAG-tagged EBOV, MARV, and MLAV VP35 or empty vector expression plasmids. Consistent with previous literature, EBOV VP35 and MARV VP35 inhibited SeV-induced PKR phosphorylation (Fig. 2). MLAV VP35 also inhibited the activation of PKR in a concentration-dependent manner (Fig. 2).
FIG 2.

MLAV VP35 inhibits Sendai virus-induced PKR activation. HEK293T cells were transfected with an empty vector (E) or expression plasmids for FLAG-tagged EBOV, MARV, and MLAV VP35 as indicated (2,000 ng, 400 ng, and 80 ng). Twenty-four hours posttransfection, cells were mock or SeV infected. Eighteen hours postinfection, whole-cell lysates were assessed by Western blot analysis for levels of total and phosphorylated PKR using anti-FLAG (VP35), anti-total PKR, anti-phospho-PKR (T446) (pPKR), and anti-β-tubulin antibodies.
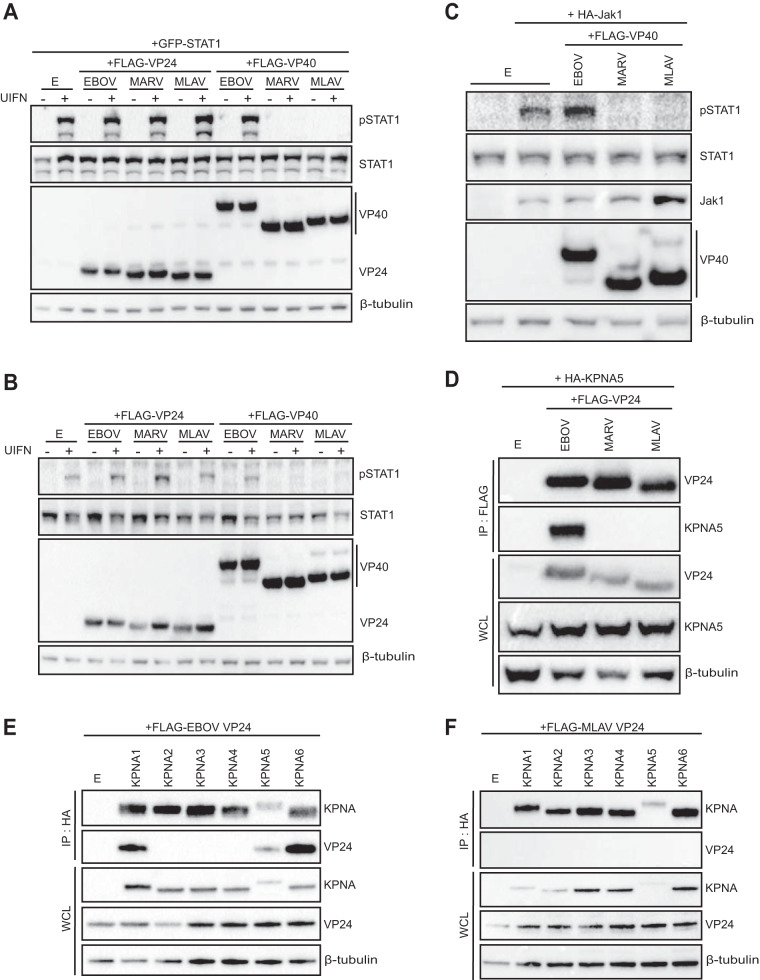
MLAV VP40 protein inhibits responses to type I IFN in both human and bat cells.
To test the effects of MLAV VP35, VP40, and VP24 on the response of cells to exogenous type I IFN, empty vector, or expression plasmids for FLAG-tagged VP35, VP40, and VP24 proteins of EBOV, MARV, and MLAV were cotransfected with an IFN-responsive interferon-stimulated gene 54 (ISG54) promoter-firefly luciferase reporter plasmid and a plasmid that constitutively expresses Renilla luciferase. Twenty-four hours posttransfection, cells were either mock or type I IFN treated. The ISG54 reporter was activated by IFN treatment in the absence of viral protein expression (Fig. 3A and B). As expected, both MARV VP40 and EBOV VP24 strongly inhibited ISG54 reporter activity in both human and bat cell lines (Fig. 3A and B). Similar to MARV VP40, MLAV VP40 potently inhibited the ISG54 reporter in both cell types. Each of the VP35s and MARV and MLAV VP24 modestly inhibited the ISG54 reporter when larger amounts of expression plasmid were tested.
FIG 3.
MLAV VP40 protein inhibits responses to type I IFN in both human and bat cells. (A) HEK293T cells were transfected with an ISG54 promoter-firefly luciferase reporter plasmid, a constitutively expressed Renilla luciferase reporter plasmid, and either an empty vector (E) or the specified FLAG-tagged viral proteins. The amounts of VP35 and VP40 plasmids were 62.5 ng, 6.25 ng, and 0.625 ng; the amounts of VP24 plasmids were 25 ng, 2.5 ng, and 0.25 ng. Twenty-four hours posttransfection, cells were either mock or UIFN treated. Eighteen hours posttreatment, firefly and Renilla luciferase activities were determined. Firefly luciferase values were normalized to Renilla luciferase values, and fold induction was calculated relative to the vector-only, mock-treated samples. (B) RO6E cells were transfected as described above, except the amounts of EBOV and MARV VP35, VP40, and VP24 plasmids were 250 ng, 25 ng, and 2.5 ng, and the amounts of MLAV VP35, VP40, and VP24 plasmids were 125 ng, 12.5 ng, and 1.25 ng. (C) HEK293T cells were assessed for endogenous human ISG54 mRNA levels in the presence of an empty vector or expression plasmids for the indicated viral proteins, 125 ng. Results were normalized to human β-actin mRNA levels. All experiments were performed in triplicate; error bars represent the SEM for the triplicate. Whole-cell lysates were analyzed by Western blotting with anti-FLAG and anti-β-tubulin antibodies (inset). Statistical significance was determined by performing a one-way ANOVA followed with Tukey’s multiple-comparison test compared to UIFN-treated control (white bar). **, P < 0.0001; *, P < 0.001.
To further address this function, endogenous ISG54 transcripts were measured by qRT-PCR. Inhibition of IFN-induced gene expression was demonstrated for MARV VP40, EBOV VP24, and MLAV VP40 (Fig. 3C), consistent with the reporter gene results. Notably, no inhibition was detected with either MLAV VP35 or MLAV VP24 in this assay.
MARV VP40 has been shown to be a potent inhibitor of IFN-α/β-induced phosphorylation of STAT1, whereas EBOV VP24 inhibits this pathway by blocking nuclear transport of pY-STAT1 (24, 25, 29). To determine whether inhibition of IFN responses is due to inhibition of STAT1 phosphorylation, HEK293T cells were cotransfected with empty vector or expression plasmids for FLAG-tagged EBOV, MARV, and MLAV VP24 or VP40. GFP-STAT1 was (Fig. 4A) or was not (Fig. 4B) included in the transfection. Addition of IFN triggered the phosphorylation of GFP-STAT1 and endogenous STAT1 in the vector-only samples. Among the EBOV and MARV constructs, only MARV VP40 was inhibitory. MLAV VP40 inhibited STAT1 tyrosine phosphorylation to a similar degree as MARV VP40; MLAV VP24 did not detectably affect STAT1 phosphorylation.
FIG 4.
MLAV VP40 protein inhibits type I IFN-induced gene expression and Jak-STAT signaling. HEK293T cells were transfected with an empty vector (E) or FLAG-tagged VP24s or VP40s from EBOV, MARV, and MLAV as indicated. Twenty-four hours posttransfection, cells were treated with UIFN for 30 min, and the phosphorylation status of exogenous GFP-STAT1 (A) or endogenous STAT1 (B) was assessed by Western blotting. (C) HEK293T cells were cotransfected with an empty vector (E) or FLAG-tagged VP40s from EBOV, MARV, MLAV, and HA-tagged Jak1 expression plasmids. Twenty-four hours posttransfection, cells were lysed, and the phosphorylation status of endogenous STAT1 was analyzed. Western blotting was performed with anti-FLAG, anti-STAT1, anti-pSTAT1 (Y701), and anti-β-tubulin antibodies. (D) HEK293T cells were cotransfected with FLAG-tagged EBOV, MARV, and MLAV VP24 and HA-tagged KPNA5. IP was performed with anti-FLAG antibody, and precipitates and WCLs were assessed by Western blotting with anti-FLAG (VP24), anti-HA (KPNA5), and anti-β-tubulin antibodies. (E and F) HEK293T cells were cotransfected with either FLAG-tagged EBOV or MLAV VP24 and HA-tagged KPNA1 to KPNA6. IP was performed with anti-HA antibody, and precipitates and WCLs were assessed by Western blotting with anti-FLAG (VP24), anti-HA (KPNA), and anti-β-tubulin antibodies.
MARV VP40 inhibits STAT1 phosphorylation following overexpression of Jak1 (30). To determine whether MLAV VP40 can prevent Jak1-induced STAT1 phosphorylation, HA-tagged Jak1 was cotransfected with an empty vector or FLAG-tagged EBOV, MARV, or MLAV VP40. As expected, expression of exogenous Jak1 induced STAT1 tyrosine phosphorylation, and this was suppressed in the presence of MARV VP40 (Fig. 4C). Similarly, MLAV VP40 prevented Jak1-dependent STAT1 phosphorylation, suggesting that MLAV VP40 inhibits IFN signaling through mechanisms similar to those used by MARV VP40.
EBOV VP24 interacts with NPI-1 subfamily members of the KPNA nuclear transporters, including KPNA5, to block nuclear import of pY-STAT1 (24, 25, 29). To assess whether MLAV VP24 interacts with KPNA5, coimmunoprecipitation assays were performed in HEK293T cells (Fig. 4D). KPNA5 did not precipitate in the absence of a coexpressed protein. Among FLAG-tagged EBOV, MARV, and MLAV VP24, only EBOV VP24 detectably interacted with KPNA5. To determine if MLAV VP24 might interact with other KPNA family members, additional coimmunoprecipitation assays were performed between MLAV VP24 and KPNA1 to KPNA6. EBOV VP24 was used in parallel as a control. As expected, EBOV VP24 coprecipitated with KPNA1, KPNA5, and KPNA6. MLAV VP24 failed to detectably coprecipitate with any of the KPNA family members (Fig. 4E and F). The absence of MLAV VP24-KPNA interactions is consistent with the inability of MLAV VP24 to inhibit IFN-induced gene expression and identifies a functional difference from EBOV VP24.
MLAV and MARV VP40 bud with similar efficiencies from human and bat cells.
Filovirus VP40 proteins play a critical role in budding of new virus particles, and expression of VP40 is sufficient for formation and budding of VLPs (43–47). MLAV VP40 displays more potent activity than MARV VP40 in several assays. To determine whether this might reflect altered cellular accumulation due to different levels of budding from cells, the capacity of EBOV, MARV, and MLAV VP40s to bud as VLPs was assessed. Upon expression in human and bat cells, each VP40 budded from both cell types. Furthermore, significant portions of EBOV, MARV, and MLAV VP40 in cell supernatants were only trypsin sensitive upon addition of Triton X-100 detergent, consistent with the VP40s from both HEK293T and RO6E cells being protected by a membrane, as is characteristic of filovirus particles (Fig. 5A and B).
FIG 5.

MLAV VP40 is capable of forming virus-like particles from both human and bat cells. To compare the budding of EBOV, MARV, and MLAV VP40 proteins from different cell lines, VLP assays were performed in a HEK293T cells (A) and RO6E cells (B). Ten percent of each VLP preparation was subjected to treatment with trypsin (Tryp) or trypsin and Triton X-100 (Tryp + Triton) to determine whether VP40 was contained within a membrane. The presence of VP40 in nontreated (N.T.) and treated VLPs and WCLs was assessed by Western blot analysis with anti-FLAG antibody. Anti-β-tubulin served as a loading control for the WCL.
MLAV VP40 and EBOV VP24 inhibition of IFN-β promoter activation occurs independently of Jak-STAT signaling.
The type I IFN response includes a positive feedback loop whereby secreted IFN upregulates pattern recognition receptors such as RIG-I and transcription factors such as IRF7 to amplify the response (48). It was therefore of interest to test the hypothesis that MLAV VP40, MARV VP40, and EBOV VP24 inhibit virus-induced induction of the IFN response as a result of their inhibition of the IFN-induced positive feedback loop. Activation of the IFN-β promoter by SeV was therefore assessed by a reporter gene assay in the absence or presence of the Jak1/Jak2 inhibitor ruxolitinib. In this experiment, cells were transfected with an empty vector or FLAG-tagged expression plasmids for the EBOV VP35, EBOV, MARV MLAV VP40, and EBOV VP24, pretreated with DMSO or ruxolitinib and then mock or SeV infected, in the absence or presence of the inhibitor (Fig. 6A). EBOV VP35 acted as a potent suppressor of IFN-β promoter activation under these conditions. MARV VP40, MLAV VP40, and EBOV VP24 all suppressed IFN-β promoter activation to similar extents in the absence or presence of the Jak kinase inhibitor. To confirm that inhibition of IFN-induced signaling was complete, cells transfected with an ISG54 promoter reporter gene were dimethyl sulfoxide (DMSO) or ruxolitinib treated and then mock or IFN treated. As expected, IFN activated the ISG54 promoter in the presence of DMSO but not ruxolitinib (Fig. 6B). To validate the inhibitory activities detected in the reporter gene assays, quantitative RT-PCR was performed to detect expression of the endogenous IFN-β and ISG54 mRNA. Consistent with the reporter assays, IFN-β and ISG54 copy numbers were significantly inhibited in the presence of EBOV VP35, EBOV VP24, and both MARV and MLAV VP40 (Fig. 6C). It is notable that inhibition of SeV-induced IFN responses by EBOV VP35 was more robust than for the other proteins. That degrees of inhibition were unaffected by the presence of the ruxolitinib, these data suggest that MARV VP40, MLAV VP40, and EBOV VP24 all utilize mechanisms independent of inhibition of STAT1 phosphorylation to impair induction of type I IFN responses.
FIG 6.
MLAV VP40 blocks Sendai virus-induced IFN-β promoter activation independently of Jak-STAT signaling. (A) HEK293T cells were transfected with an IFN-β promoter-firefly luciferase reporter plasmid, a constitutively expressed Renilla luciferase reporter plasmid, and either an empty vector (E) or the specified FLAG-tagged viral proteins. The amounts of VP35, VP40, and VP24 plasmids were 62.5 ng, 6.25 ng, and 0.625 ng. Twenty-four hours posttransfection, cells were pretreated with either DMSO or the Jak1/Jak2 inhibitor ruxolitinib for 1 h. Posttreatment, cells were mock or SeV infected in the presence of DMSO or ruxolitinib. Firefly and Renilla luciferase activities were determined 18 h later using a dual-luciferase assay (Promega). Fold induction was determined relative to the DMSO vector-only, mock-infected samples. Viral protein expression was confirmed by Western blotting with anti-FLAG antibody (inset). Anti-β-tubulin served as a loading control. (B) HEK293T cells were transfected with an ISG54 promoter-firefly luciferase reporter plasmid, a constitutively expressing Renilla luciferase reporter plasmid, and an empty vector. Twenty-four hours posttransfection, cells were pretreated with DMSO or ruxolitinib for 1 h. Posttreatment, cells were mock or UIFN treated in the presence of DMSO or ruxolitinib. Firefly and Renilla luciferase activities were determined 18 h later using a dual-luciferase assay (Promega). Fold induction was determined relative to the DMSO, mock-treated samples. (C) HEK293T cells were assessed for endogenous human IFN-β and ISG54 mRNA levels in the presence of viral expression plasmids, 125 ng. Results were normalized to human β-actin mRNA levels. Assays were performed in triplicate. Cell lysates were analyzed by Western blotting with anti-FLAG and anti-β-tubulin antibodies (inset). For panels A and C, error bars represent the SEM for the triplicate. Statistical significance was determined by performing a one-way ANOVA followed with Tukey multiple comparison compared to the SeV-infected control. **, P < 0.0001; *, P < 0.001.
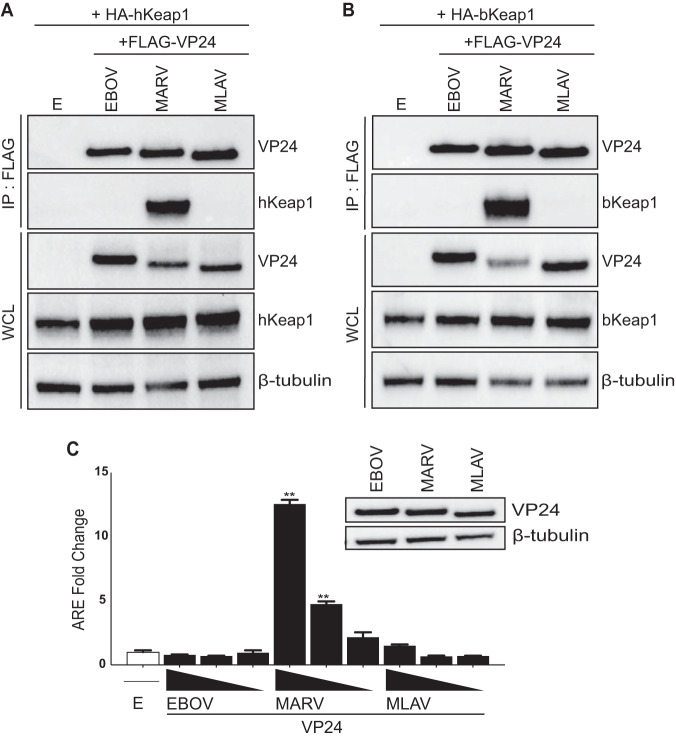
MLAV VP24 fails to interact with Keap1 or activate ARE gene expression due to the absence of a Keap1-interacting K-loop.
MARV VP24 interacts with Keap1 to activate ARE promoters (35, 36). To determine whether MLAV VP24 possesses similar properties, coimmunoprecipitation experiments were performed with HA-tagged human Keap1 (hKeap1) or HA-tagged Keap1 derived from the bat Myotis lucifugus (bKeap1), which is 96.8% identical at the amino acid level, to the predicted Rousettus aegyptiacus Keap1 (data not shown). As previously described, MARV VP24 interacted with both human and bat Keap1, whereas EBOV and MLAV VP24 did not interact (Fig. 7A and B). Consistent with these data, when tested in an ARE promoter reporter gene assay, MARV VP24 activated the ARE reporter relative to an empty vector control, while neither EBOV nor MLAV VP24 activated the ARE response (Fig. 7C).
FIG 7.
MLAV VP24 does not interact with KEAP1 or activate an ARE promoter. (A and B) HEK293T cells were cotransfected with FLAG-tagged EBOV, MARV, and MLAV VP24 as indicated and HA-tagged human Keap1 (hKeap1) (A) or HA-tagged bat Keap1 (bKeap1) (B). Co-IP was performed with an anti-FLAG antibody, and precipitates and WCLs were assessed by using anti-FLAG (VP24), anti-HA (Keap1), and anti-β-tubulin antibodies. (C) HEK293T cells were transfected with a reporter plasmid with the firefly luciferase gene under the control of an ARE promoter, a reporter plasmid that constitutively expresses Renilla luciferase and either an empty vector (E) or the indicated FLAG-VP24 proteins. The amounts of VP24 plasmids were 62.5 ng, 6.25 ng, and 0.625 ng. Firefly and Renilla luciferase activities were determined 18 h posttransfection. Firefly luciferase activity was normalized to Renilla luciferase activities, and fold activity is reported relative to the empty vector-only sample. Protein expression was analyzed by Western blotting using anti-FLAG (VP24) and anti-β-tubulin antibodies (inset). The reporter gene assays were performed in triplicate; error bars represent the SEM for the triplicate. Statistical significance was determined by performing a one-way ANOVA followed with Tukey multiple comparison compared to the vector-only control (white bar). **, P < 0.0001; *, P < 0.001.
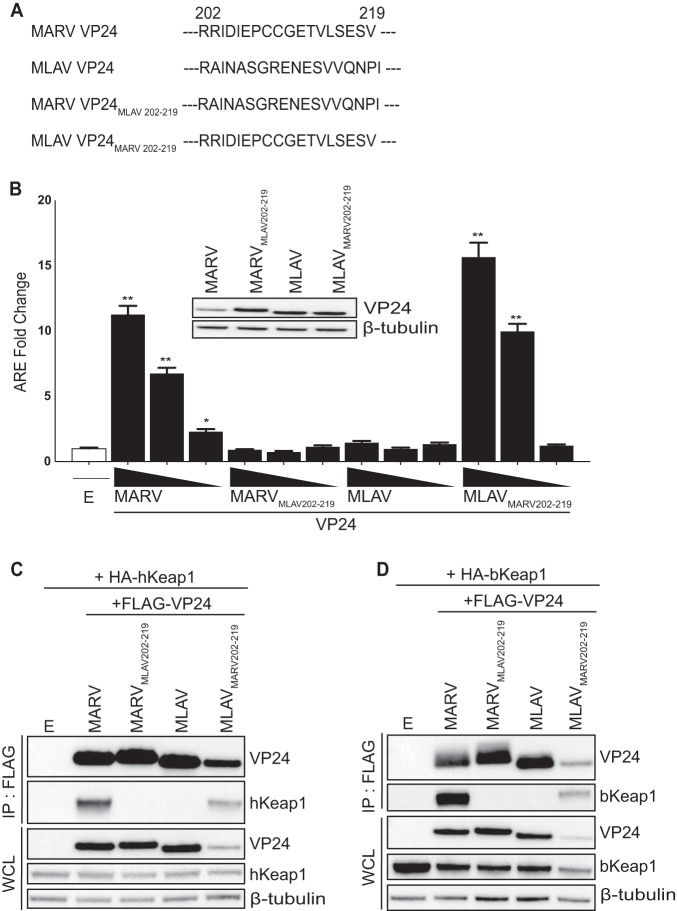
MARV VP24 interaction with Keap1 occurs via a specific motif, the K-loop, and transfer of this sequence to EBOV VP24 confers binding to Keap1 (35). To determine whether this sequence could confer interaction with Keap1 and activation of ARE responses upon MLAV VP24, the MARV VP24 K-loop sequence (amino acid residues 202 to 219) was transferred to MLAV VP24, replacing the corresponding amino acid residues (MLAV VP24MARV 202–219). The reverse chimera was also generated, with MLAV sequences replacing the K-loop in MARV VP24 (MARV VP24MLAV 202–219) (Fig. 8A). Transferring the MARV K-loop sequence to MLAV VP24 conferred the capacity to activate an ARE response, while transfer of the MLAV sequence to MARV VP24 abolished the activation (Fig. 8B). Interaction with human Keap1 (Fig. 8C) and bat Keap1 (Fig. 8D) yielded corresponding data, where interaction was dependent on the MARV VP24 K-loop. Collectively, these data demonstrate that the lack of ARE gene expression by MLAV VP24 is due to the lack of a Keap1-binding motif.
FIG 8.
Transfer of the MARV K-loop sequence confers on MLAV VP24 interaction with Keap1 and activation of ARE signaling. (A) Sequences for amino acid residues 202 to 219, which correspond to the MARV VP24 K-loop, for MARV VP24, MLAV VP24, and the VP24 chimera constructs MLAV VP24MARV 202–219 and MARV VP24MLAV 202–219. (B) HEK293T cells were transfected with reporter plasmid with the firefly luciferase gene under the control of an ARE promoter, a reporter plasmid that constitutively expresses Renilla luciferase and either an empty vector (E) or the indicated FLAG-VP24 proteins. The amounts of VP24 plasmids were 62.5 ng, 6.25 ng, and 0.625 ng. Firefly and Renilla luciferase activities were determined 18 h posttransfection. Firefly luciferase activity was normalized to Renilla luciferase activities, and fold activity is reported relative to the empty vector-only sample. The experiment was performed in triplicate; error bars represent the SEM for the triplicate. Statistical significance was determined by performing a one-way ANOVA followed with Tukey multiple comparison compared to a vector-only control (white bar). **, P < 0.0001; *, P < 0.001. Cell lysates were analyzed by Western blotting with anti-FLAG (VP24) and anti-β-tubulin antibodies (inset). (C and D) HEK293T cells were transfected with FLAG-tagged constructs as indicated and either HA-tagged human Keap1 (hKeap1) (C) or HA-tagged bat Keap1 (bKeap1) (D). Co-IP was performed with anti-FLAG antibody. IPs were analyzed by Western blotting with anti-FLAG (VP24), anti-HA (Keap1), and anti-β-tubulin antibodies.
MLAV VP35 and VP40 proteins maintain their ability to inhibit the IFN response in the presence of other viral proteins.
Both VP35 and VP40 are known to independently interact with the nucleoprotein (NP) and, together with the VP24 protein, NP and VP35, can form mature nucleocapsids (49–52). To determine if the formation of the nucleocapsid complex impacted the ability of VP35 to inhibit IFN-β production, various amounts of EBOV and MLAV VP35 were transfected in the presence of EBOV or MLAV NP and VP24, respectively. Both EBOV and MLAV VP35 were still able to inhibit SeV-induced activation of the IFN-β promoter in the presence of NP and VP24 (Fig. 9A). Similarly, to assess if NP could interfere with the ability of VP40 to inhibit IFN production and signaling, we cotransfected various amounts of MARV VP40 or MLAV VP40 in the presence of NP. MLAV VP40 was still a potent repressor of both SeV-induced activation of the IFN-β promoter and the universal type I IFN (UIFN)-induced activation of the ISG54 promoter in the presence of NP (Fig. 9B and C). Lastly, we evaluated the effect of cotransfecting multiple viral proteins together on the inhibitory capabilities of EBOV, MARV, and MLAV. The respective NP, VP35, VP40, VP30, and VP24 plasmids were transfected together in either the IFN-β or ISG54 promoter assay. Upon activation with either SeV or UIFN, respectively, it was observed that the combination of proteins inhibited the SeV-induced activation of the IFN-β promoter and the UIFN-induced activation of the ISG54 promoter (Fig. 9D and E).
FIG 9.
MLAV VP35 and VP40 maintain their ability to inhibit the IFN response in the presence of other viral proteins. (A to C) HEK293T cells were transfected with either an IFN-β (A and B) or an ISG54 (C) promoter-firefly luciferase reporter plasmid, a constitutively expressed Renilla luciferase reporter plasmid, and either an empty vector (E) or the specified FLAG-tagged viral proteins. (A) The amounts of VP35 plasmid were 62.5 ng, 6.25 ng, and 0.625 ng, and the amounts of NP and VP24 plasmids were 6.25 ng. (B and C) The amounts of VP40 plasmid were 62.5 ng, 6.25 ng, and 0.625 ng, and the amount of NP plasmid was 6.25 ng. Twenty-four hours posttransfection, cells were either mock or SeV infected (A and B) or UIFN treated (C). Eighteen hours posttreatment, firefly and Renilla luciferase activities were determined. Firefly luciferase values were normalized to Renilla luciferase values, and fold induction was calculated relative to the vector-only, mock-treated samples. (D and E) HEK293T cells were transfected with either an IFN-β (D) or an ISG54 (E) promoter-firefly luciferase reporter plasmid, a constitutively expressed Renilla luciferase reporter plasmid, and either an empty vector (E) or 6.25 ng each of the NP, VP35, VP40, VP30, and VP24 plasmids from the indicated virus. Twenty-four hours posttransfection, cells were either mock or SeV infected (D) or UIFN treated (E). Eighteen hours posttreatment, firefly and Renilla luciferase activities were determined. Firefly luciferase values were normalized to Renilla luciferase values, and fold induction was calculated relative to the vector-only, mock-treated samples. Statistical significance was determined by performing a one-way ANOVA followed with a Tukey’s multiple comparison test. Relevant controls for the comparison were the SeV infected (white bar) (panels A, B, and, D) or the UIFN-treated (white bar) (panels C and E) samples. **, P < 0.0001; *, P < 0.001.
DISCUSSION
The data in this study provide functional evidence that MLAV is biologically distinct from other filoviruses and support its classification in its own genus. The placement of MLAV in a distinct genus was based on its relatively low sequence identity to other filoviruses (1). It was also noted to have, compared to other filoviruses, unique gene overlaps and a unique transcription start signal. Despite these distinctions, MLAV mechanisms of entry and RNA synthesis, based on pseudotype and minigenome assays, mirror those of both EBOV and MARV. MLAV also possesses some features that suggest a closer genetic relationship to members of the Marburgvirus genus as opposed to the Ebolavirus and Cuevavirus genera. This includes similarities in large (L) protein sequence and the absence of RNA editing sites in GP (1). In addition, MLAV was identified in Rousettus bats, and Rousettus bats in Africa serve as a reservoir for MARV and Ravn virus (RAVV) (3). The present study demonstrates commonalities and distinctions between MLAV and either EBOV or MARV in terms of how viral proteins antagonize the innate immune response in both bat and human cells. Inhibition of RIG-I-induced IFN responses is thus far a common feature of filoviruses (53). The suppression of IFN-induced signaling and gene expression by VP40, rather than via VP24, parallels MARV and draws a functional distinction between MLAV and EBOV. The absence of MLAV VP24 interaction with human or bat Keap1, and its lack of ARE transcriptional activation, is consistent with MLAV having evolved unique virus-host interactions that are distinct from MARV. These findings further support the placement of MLAV in a distinct genus but also suggest a closer relationship to MARV than EBOV.
The data also demonstrate that MLAV encodes mechanisms to counteract both type I IFN production and cellular responses to exogenous IFN and that this virus has the potential to antagonize these innate antiviral responses in both bat and human cells. MLAV VP35 was demonstrated to effectively block activation of the IFN-β promoter in response to SeV infection, a known inducer of the RIG-I signaling pathway. In addition, inhibition of SeV-induced phosphorylation of IRF3 was demonstrated. Together, these data indicate that MLAV can block RIG-I signaling, consistent with the function of other filovirus VP35s (39, 54). Mechanistically, inhibition of IFN-α/β production by EBOV or MARV VP35 correlates with dsRNA-binding activity (8, 9, 11–13, 15, 18, 19, 42). This may reflect binding and sequestration of RIG-I-activating dsRNAs (12, 19). The VP35 dsRNA-binding domain, also known as the interferon inhibitory domain (IID), directly contacts the phosphodiester backbone of dsRNA via residues that comprise a central basic patch to mediate this interaction (9–11, 16, 17, 42). EBOV VP35 also caps the ends of dsRNA in a manner that likely masks 5′-triphosphates, which contribute to recognition of RNAs by RIG-I (11, 16). VP35 interaction with host protein PACT, which interacts with and facilitates activation of RIG-I, also contributes to inhibition (12, 55). Because the residues that make up the central basic patch are conserved between MLAV and other filoviral VP35s (1), MLAV is likely to bind to dsRNA. Given that it also interacts with PACT (Fig. 1E), its mechanisms of inhibition are likely similar to other filoviral VP35s.
EBOV, MARV, and LLOV VP35 have also been demonstrated to inhibit activation of PKR, an IFN-induced, dsRNA-activated protein kinase that exerts antiviral effects by suppressing translation (20–23, 40). The mechanism by which VP35s inhibit PKR remains ambiguous; however, mutation of multiple central basic patch residues in EBOV or MARV VP35 disrupts the inhibitory activity (21, 22). In contrast, single point mutations that disrupt EBOV VP35 dsRNA binding activity leave PKR inhibition intact, suggesting that inhibition of PKR is not dependent upon VP35-dsRNA interaction or sequestration (20, 21). Consistent with PKR inhibition being an important function for filoviruses, this activity is conserved in MLAV as well. That the inhibition can occur in human cells further supports the likelihood that MLAV could counter human innate antiviral defenses.
The IFN-inhibitory activities of both EBOV and MARV VP35 have been demonstrated to be important for efficient virus replication in IFN-competent systems (13, 41). In addition to blocking the production of antiviral IFNs, VP35 inhibition of RIG-I also suppresses maturation of dendritic cells when expressed alone or in the context of EBOV infection (14, 56, 57). This activity impairs adaptive immunity to EBOV (58, 59). Therefore, VP35 likely inhibits adaptive, as well as innate, antiviral defenses. Disruption of VP35 anti-IFN function in the context of recombinant EBOVs has been demonstrated to render the virus avirulent in mice, guinea pigs, and nonhuman primates (13, 60, 61). Based on these data, VP35 suppression of RIG-I signaling appears to be critical for virulence. The effective function in human cells of MLAV VP35 satisfies one apparent criterion for virulence in humans. It should be noted, however, that suppression of RIG-I signaling by VP35 is not sufficient on its own to confer virulence. Even though MARV VP35 functions in Rousettus cells and likely has evolved in this species, MARV does not appear to cause significant disease in these animals (62–64). It does seem likely that in the reservoir host, VP35 IFN antagonist function will be important for efficient replication and transmission, although this remains to be tested experimentally.
For MARV, either infection or VP40 expression alone blocks IFN-induced phosphorylation of Jak kinases, inhibiting activation and downstream signaling. The absence of these phosphorylation events in response to IFN-α/β or IFN-γ is consistent with the phenotype of Jak1-deficient cells, suggesting that Jak1 function may be targeted by MARV VP40, although there is no evidence to date of VP40-Jak1 interaction (30). Consistent with MARV VP40 impairing Jak1 function, MARV VP40 expression is sufficient to prevent phosphorylation of STAT proteins following Jak1 overexpression or treatment by IFN-α/β or IFN-γ (type II IFN) (30). MLAV VP40 likewise blocks ISG expression and inhibits STAT1 phosphorylation following IFN treatment or overexpression of Jak1. Therefore, inhibition of IFN signaling by MLAV VP40 seems likely to proceed by a mechanism similar to that employed by MARV VP40.
MARV VP24 binds directly to Keap1, a cellular substrate adaptor protein of the Cullin-3/Rbx1 E3 ubiquitin ligase complex, via a shelf-like projection composed of two beta-sheets and a loop called the K-loop (35–37, 65). Keap1 regulates the cellular antioxidant response (66). Under homeostatic conditions, Keap1 promotes Nrf2 polyubiquitination and degradation. Cell stresses, including oxidative stress, disrupt the Keap1-mediated ubiquitination of Nrf2, stabilizing it and promoting Nrf2-dependent expression of antioxidant response genes. Biophysical studies demonstrated that MARV VP24 interacts with the Keap1 Kelch domain at a site that overlaps the region that binds Nrf2 (37). This interaction disrupts Nrf2-Keap1 interaction and activates ARE gene expression (35–37). Keap1 similarly interacts with host IκB kinase complex beta (IKKβ) to repress NF-ĸB responses, and MARV VP24 can also disrupt this interaction, thereby relieving Keap1 repression on the NF-ĸB transcriptional response (38). In contrast, EBOV and LLOV VP24 target KPNA proteins in a manner that prevents pY-STAT1 nuclear transport, inhibiting ISG expression (24, 25, 28, 29, 40).
Given that MLAV VP40 mirrored MARV VP40 in its inhibition of the IFN response, it was of interest to determine whether MLAV VP24 would similarly mimic MARV VP24 in terms of interaction with the Keap1-Nrf2 pathway. However, MLAV VP24 lacks a sequence that resembles the MARV VP24 K-loop and, correspondingly, did not interact with human- or a bat-derived Keap1 and did not activate an ARE promoter. Chimeric MARV-MLAV VP24 proteins confirmed that the absence of the K-loop sequence can explain the lack of MLAV VP24 effects on antioxidant responses. Furthermore, consistent with the absence of MLAV VP24 inhibitory activity in IFN-signaling assays, it also fails to interact with KPNA1, -5, and -6, which can mediate nuclear import of pY-STAT1. The interface between EBOV VP24 and KPNA covers a large surface area and involves multiple points of contact (29). This precluded the mapping of specific amino acid residues that explain the lack of MLAV VP24-KPNA interactions. Nonetheless, these data presented here indicate that MLAV VP24 does not reflect the functions of either MARV or EBOV VP24. It will be of interest to determine whether MLAV VP24 engages a different host signaling pathway(s).
The inhibition of IFN-β promoter activity by MLAV VP40 parallels the inhibition by EBOV VP24 and MARV VP40, although inhibition by MLAV VP40 appeared to be more potent. Interestingly, MLAV VP40 inhibits SeV-induced IFN-β gene expression with an efficiency comparable to EBOV VP35, although MLAV VP35 appears to be more potent than MLAV VP40 in this assay. It will be of interest to determine to what extent VP35 and VP40 contribute to suppression of IFN induction in MLAV-infected cells. MARV VP40 and EBOV VP24 inhibition of IFN-α/β production and, in the case of EBOV VP24, production of IFN-λ as well, have been previously reported (33, 34). However, the mechanism(s) for these inhibitory activities is incompletely defined, although EBOV VP24 was implicated as having an effect post-IRF3 phosphorylation (33). Inhibition of STAT1 activation and IFN-induced gene expression would be expected to impair the positive feedback loop in which IFN-α/β induces expression of IFN-stimulated genes, including RIG-I and IRF7, to amplify IFN responses (48). This prompted additional experiments to determine whether the detected inhibition was a product of blocking a positive feedback loop involving Jak-STAT signaling. Treatment of empty vector-transfected cells with a Jak1/Jak2 inhibitor did not inhibit SeV-induced IFN-β promoter activation, suggesting that in the system used, Jak-STAT signaling does not contribute to the IFN-β response. Further, the dose responses of EBOV VP24, MARV VP40, and MLAV VP40 in the IFN-β promoter assay were unaffected. These data suggest MLAV VP40 has an additional mechanism(s) of IFN antagonism that requires further exploration.
Infectious MLAV is not available to allow us to confirm that suppression of IFN responses occurs in infected cells. As an alternative, we asked whether other viral proteins might modulate these activities. We cotransfected MLAV VP35 and MLAV VP40 with other viral proteins that, based on data from EBOV and MARV, would be expected to form functional complexes. VP35, when coexpressed with NP and VP24, forms nucleocapsid structures (49, 50, 52). Despite this, NP and VP24 coexpression did not prevent inhibition of the IFN-β promoter by either EBOV or MLAV. Similarly, VP40 interacts with NP (51). However, NP affected neither VP40 suppression of the IFN-β nor the ISG54 promoter. Additionally, coexpression of the internal viral proteins except for the large (L) protein, which is expressed at low levels in filovirus-infected cells, also did not prevent suppression of IFN responses. These findings suggest that these innate immune evasion functions will be active during MLAV infection.
Cumulatively, the present study has identified several functions of MLAV proteins that, in conjunction with previously published data, indicate compatibility with infection of humans. These include the capacity of MLAV GP to mediate entry into human cells via interaction with NPC1 and suppression of IFN responses through several mechanisms (1). Notably, given that MLAV VP24 does not detectably interact with the KPNAs or Keap1, it is likely that it may make unique interactions with host cells. Therefore, the existing data also suggests that the outcome of MLAV infection in humans could differ from that of the typical outcome of EBOV or MARV infection.
MATERIALS AND METHODS
Cells and viruses.
HEK293T cells were maintained in Dulbecco’s modified Eagle medium (DMEM), supplemented with 10% fetal bovine serum (FBS), and cultured at 37°C and 5% CO2. RO6E cells, immortalized fetal cells from Rousettus aegyptiacus, were obtained from BEI Resources and maintained in DMEM F12 and supplemented with 5% FBS. Sendai virus (Cantell strain) (SeV) was grown in 10-day-old embryonating chicken eggs for 48 h at 37°C.
Plasmids.
MLAV NP, VP35, VP40, VP30, and VP24 coding sequences (based on GenBank accession number KX371887) were synthesized by GenScript. The synthesized open reading frames were cloned into a pCAGGS expression vector with a FLAG tag at the N terminus of each coding sequence. EBOV and MARV viral proteins, GFP-STAT1, HA-Jak1, HA-PACT, HA-KPNA5, HA-Keap1, and IRF3 expression plasmids were previously described (8, 12, 24, 31, 35). VP24 K-loop chimeras were made using overlapping PCR. MARV VP24 residues 202-RRIDIEPCCGETVLSESV-219 were inserted into MLAV VP24 between residues 202 and 219 (MLAV VP24MARV 202–219), and the corresponding MLAV residues 202-RAINASGRENESVVQNPI-219 were inserted into MARV VP24 at the same position (MARV VP24MLAV 202–219).
Cytokines.
Universal type I IFN (UIFN) (PBL) was used at 1,000 U/ml in DMEM supplemented with 0.3% FBS for 30 min at 37°C unless otherwise stated.
IRF3 and PKR phosphorylation assays.
HEK293T cells (1 × 106) were transfected using Lipofectamine 2000 (Life Technologies). The amount of transfected IRF3 was 100 ng per well. Twenty-four hours posttransfection, cells were mock treated, UIFN treated, or SeV infected, depending on the assay. Subsequently, cells were lysed in NP-40 buffer (50 mM Tris-HCl [pH 8.0], 280 mM NaCl, 0.5% NP-40) supplemented with cOmplete protease inhibitor cocktail (Roche) and PhosSTOP (Roche). Lysates were incubated for 10 min on ice and clarified for 10 min at 21,100 × g at 4°C. The phosphorylation status of the proteins was determined by Western blotting.
IFN-β and ISG54 promoter reporter gene assays.
HEK293T cells (5 × 104) and RO6E cells (2 × 105) were cotransfected using Lipofectamine 2000 with 25 ng of an IFN-β promoter-firefly luciferase reporter plasmid or an interferon-stimulated gene 54 (ISG54) promoter-firefly luciferase reporter plasmid, 25 ng of a constitutively expressing Renilla luciferase plasmid (pRL-TK; Promega), and the indicated viral protein expression plasmids (HEK293T cells, 62.5, 6.25, and 0.625 ng for VP35 and VP40 and 25, 2.5, and 0.25 ng for VP24; RO6E cells, 250, 25, and 2.5 ng for EBOV and MARV proteins and 125, 12.5, and 1.25 ng for MLAV proteins). Twenty-four hours posttransfection, cells were mock treated, SeV infected (150 hemagglutinin activity units [HAU]), or UIFN treated (1,000 U/ml). Eighteen hours postinfection or posttreatment, cells were lysed and analyzed for luciferase activity using a Dual-Luciferase reporter assay system (Promega) per the manufacturer’s protocol. Firefly luciferase activity was normalized to Renilla luciferase activity. Assays were performed in triplicate; error bars indicate the standard error of the mean (SEM) for the triplicate. Viral protein expression was confirmed by Western blot analysis.
IFN-β promoter reporter gene assay in the presence of a Jak1/Jak2 inhibitor.
HEK293T cells (5 × 104) were cotransfected using Lipofectamine 2000 with 25 ng of an IFN-β promoter-firefly luciferase reporter plasmid, 25 ng of pRL-TK Renilla luciferase reporter plasmid, and 62.5, 6.25, and 0.625 ng of the indicated viral protein expression plasmids. Twenty-four hours posttransfection, cells were pretreated for 1 h with 5 μM of ruxolitinib (Selleckchem), a Jak1/Jak2 inhibitor, and then mock or SeV infected in the presence of the inhibitor (67). Eighteen hours postinfection or treatment, cells were lysed and assayed using a dual-luciferase assay and analyzed as above. To verify inhibition of Jak1/Jak2 by ruxolitinib, cells were transfected with 25 ng of an ISG54 promoter-firefly luciferase reporter plasmid and 25 ng of pRL-TK reporter plasmid. Twenty-four hours posttransfection, cells were pretreated for 1 h with 5 μM of ruxolitinib and then mock or UIFN treated for 18 h in the presence of the inhibitor and assayed for luciferase activity as above.
Measurements of endogenous gene expression.
HEK293T cells (5 × 104) were transfected with 125 ng of empty vector or viral expression plasmids using Lipofectamine 2000. Twenty-four hours posttransfection, cells were either mock treated, SeV infected, or UIFN treated (1,000 U/ml). At 14 h posttreatment or postinfection, total cellular RNA was extracted using RNeasy minikit (Qiagen) as per the manufacturer’s protocol. SuperScript IV (Thermo Fisher Scientific) was used to generate oligo(dT) cDNA, which served as the template for quantitative PCR (qPCR). qPCR was performed using PerfeCTa SYBR green FastMix (VWR Scientific) along with gene-specific primers for human β-actin, IFN-β, and ISG54.
ARE reporter assay.
HEK293T cells (5 × 104) were cotransfected using Lipofectamine 2000 with an antioxidant response element (ARE) reporter gene, pGL4.37 (luc2P/ARE/Hygro) (Promega) (30 ng) and a pRL-TK reporter plasmid (25 ng) along with either an empty vector or 62.5, 6.25, and 0.625 ng of EBOV, MARV, MLAV VP24 or chimeric MARV, and MLAV expression plasmids. Eighteen hours posttransfection, luciferase activity was assessed and analyzed as above.
Coimmunoprecipitation assays.
HEK293T cells were cotransfected using Lipofectamine 2000 with plasmids for FLAG-tagged MLAV proteins, HA-tagged host proteins, and pCAGGS empty vector. Twenty-four hours posttransfection, cells were rinsed with phosphate-buffered saline (PBS) and lysed in NP-40 buffer supplemented with cOmplete protease inhibitor cocktail. Lysates were clarified by centrifugation and incubated with anti-FLAG M2 (Sigma-Aldrich) or anti-HA (Thermo Fisher) magnetic beads for 2 h at 4°C. Beads were washed five times in NP-40 buffer, and precipitated proteins were eluted by boiling with SDS sample loading buffer or elution with 3× FLAG peptide (Sigma-Aldrich). Whole-cell lysates and immunoprecipitated samples were analyzed by Western blotting.
Western blot analysis.
Blots were probed with anti-FLAG (Sigma-Aldrich), anti-β-tubulin (Sigma-Aldrich), anti-HA (Sigma-Aldrich), anti-phospho-IRF3 (Ser396; Cell Signaling), anti-IRF3 (Santa Cruz), anti-phospho-STAT1 (Y701; BD Transduction Laboratories), anti-STAT1 (BD Transduction Laboratories), anti-phospho-PKR (T446) (Abcam), or anti-PKR (Cell Signaling) antibodies, as indicated. Antibodies were diluted in Tris-buffered saline with 0.1% Tween 20 (TBST) with 5% milk or, when detecting phospho-proteins, 5% bovine serum albumin.
VP40 budding assay.
Ten micrograms of EBOV, MARV, and MLAV VP40 expression plasmids were transfected into either HEK293T (3 × 106) or RO6E (2 × 106) cells using Lipofectamine 2000. Media were harvested 48 h posttransfection, briefly clarified by centrifugation, and layered over a 20% sucrose cushion in NTE buffer (10 mM NaCl, 10 mM Tris [pH 7.5], 1 mM EDTA [pH 8.0]). The samples were then subjected to ultracentrifugation in a Beckman SW41 rotor at 222,200 × g for 2 h at 10°C; the medium was aspirated after ultracentrifugation, and virus-like particles (VLPs) were solubilized in NTE buffer at 4°C overnight. Cellular lysates were generated by washing transfected cells with PBS and lysing cells in NP-40 buffer containing cOmplete protease inhibitor cocktail. To detect the presence of VP40, 5% of cell lysates and 10% of VLPs were analyzed by Western blotting. To confirm that VP40s from isolated VLPs had a membrane that can protect internal components from protease digestion, 10% of VLPs were incubated in NTE buffer with 500 ng/μl of trypsin solution (Corning), either in the absence or presence of 0.5% Triton X-100 (Sigma), at 37°C for 1 h prior to Western blot analysis.
Statistics.
Statistical significance was determined by one-way analysis of variance (ANOVA) followed with Tukey multiple comparison compared to the indicated control. **, P < 0.0001; *, P < 0.001 (GraphPad Prism 8).
ACKNOWLEDGMENTS
This work was supported by NIH grants P01AI120943 and U19AI109945 and Department of the Defense, Defense Threat Reduction Agency grant HDTRA1-16-1-0033.
The content of the information does not necessarily reflect the position or the policy of the federal government, and no official endorsement should be inferred.
C.F.B. is a Georgia Research Alliance Eminent Scholar in microbial pathogenesis. The RO6E cell line was obtained through BEI Resources, NIAID, NIH, catalog no. NR49168.
REFERENCES
- 1.Yang XL, Tan CW, Anderson DE, Jiang RD, Li B, Zhang W, Zhu Y, Lim XF, Zhou P, Liu XL, Guan W, Zhang L, Li SY, Zhang YZ, Wang LF, Shi ZL. 2019. Characterization of a filovirus (Měnglà virus) from Rousettus bats in China. Nat Microbiol 4:390–395. doi: 10.1038/s41564-018-0328-y. [DOI] [PubMed] [Google Scholar]
- 2.Maes P, Amarasinghe GK, Ayllón MA, Basler CF, Bavari S, Blasdell KR, Briese T, Brown PA, Bukreyev A, Balkema-Buschmann A, Buchholz UJ, Chandran K, Crozier I, de Swart RL, Dietzgen RG, Dolnik O, Domier LL, Drexler JF, Dürrwald R, Dundon WG, Duprex WP, Dye JM, Easton AJ, Fooks AR, Formenty PBH, Fouchier RAM, Freitas-Astúa J, Ghedin E, Griffiths A, Hewson R, Horie M, Hurwitz JL, Hyndman TH, Jiāng D, Kobinger GP, Kondō H, Kurath G, Kuzmin IV, Lamb RA, Lee B, Leroy EM, Lǐ J, Marzano S-YL, Mühlberger E, Netesov SV, Nowotny N, Palacios G, Pályi B, Pawęska JT, Payne SL, et al. 2019. Taxonomy of the order Mononegavirales: second update 2018. Arch Virol 164:1233–1244. doi: 10.1007/s00705-018-04126-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuh AJ, Amman BR, Towner JS. 2017. Filoviruses and bats. Microbiol Aust 38:12–16. doi: 10.1071/MA17005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Messaoudi I, Amarasinghe GK, Basler CF. 2015. Filovirus pathogenesis and immune evasion: insights from Ebola virus and Marburg virus. Nat Rev Microbiol 13:663–676. doi: 10.1038/nrmicro3524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rougeron V, Feldmann H, Grard G, Becker S, Leroy EM. 2015. Ebola and Marburg haemorrhagic fever. J Clin Virol 64:111–119. doi: 10.1016/j.jcv.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO Ebola Response Team, Agua-Agum J, Allegranzi B, Ariyarajah A, Aylward R, Blake IM, Barboza P, Bausch D, Brennan RJ, Clement P, Coffey P, Cori A, Donnelly CA, Dorigatti I, Drury P, Durski K, Dye C, Eckmanns T, Ferguson NM, Fraser C, Garcia E, Garske T, Gasasira A, Gurry C, Hamblion E, Hinsley W, Holden R, Holmes D, Hugonnet S, Jaramillo Gutierrez G, Jombart T, Kelley E, Santhana R, Mahmoud N, Mills HL, Mohamed Y, Musa E, Naidoo D, Nedjati-Gilani G, Newton E, Norton I, Nouvellet P, Perkins D, Perkins M, Riley S, Schumacher D, Shah A, Tang M, Varsaneux O, Van Kerkhove MD. 2016. After Ebola in West Africa–unpredictable risks, preventable epidemics. N Engl J Med 375:587–596. doi: 10.1056/NEJMsr1513109. [DOI] [PubMed] [Google Scholar]
- 7.Basler CF, Wang X, Muhlberger E, Volchkov V, Paragas J, Klenk HD, Garcia-Sastre A, Palese P. 2000. The Ebola virus VP35 protein functions as a type I IFN antagonist. Proc Natl Acad Sci U S A 97:12289–12294. doi: 10.1073/pnas.220398297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cardenas WB, Loo YM, Gale M Jr, Hartman AL, Kimberlin CR, Martinez-Sobrido L, Saphire EO, Basler CF. 2006. Ebola virus VP35 protein binds double-stranded RNA and inhibits alpha/beta interferon production induced by RIG-I signaling. J Virol 80:5168–5178. doi: 10.1128/JVI.02199-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards MR, Liu G, Mire CE, Sureshchandra S, Luthra P, Yen B, Shabman RS, Leung DW, Messaoudi I, Geisbert TW, Amarasinghe GK, Basler CF. 2016. Differential regulation of interferon responses by Ebola and Marburg virus VP35 proteins. Cell Rep 14:1632–1640. doi: 10.1016/j.celrep.2016.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leung DW, Ginder ND, Fulton DB, Nix J, Basler CF, Honzatko RB, Amarasinghe GK. 2009. Structure of the Ebola VP35 interferon inhibitory domain. Proc Natl Acad Sci U S A 106:411–416. doi: 10.1073/pnas.0807854106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung DW, Prins KC, Borek DM, Farahbakhsh M, Tufariello JM, Ramanan P, Nix JC, Helgeson LA, Otwinowski Z, Honzatko RB, Basler CF, Amarasinghe GK. 2010. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat Struct Mol Biol 17:165–172. doi: 10.1038/nsmb.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luthra P, Ramanan P, Mire CE, Weisend C, Tsuda Y, Yen B, Liu G, Leung DW, Geisbert TW, Ebihara H, Amarasinghe GK, Basler CF. 2013. Mutual antagonism between the Ebola virus VP35 protein and the RIG-I activator PACT determines infection outcome. Cell Host Microbe 14:74–84. doi: 10.1016/j.chom.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prins KC, Delpeut S, Leung DW, Reynard O, Volchkova VA, Reid SP, Ramanan P, Cardenas WB, Amarasinghe GK, Volchkov VE, Basler CF. 2010. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J Virol 84:3004–3015. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yen B, Mulder LC, Martinez O, Basler CF. 2014. Molecular basis for ebolavirus VP35 suppression of human dendritic cell maturation. J Virol 88:12500–12510. doi: 10.1128/JVI.02163-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hartman AL, Towner JS, Nichol ST. 2004. A C-terminal basic amino acid motif of Zaire ebolavirus VP35 is essential for type I interferon antagonism and displays high identity with the RNA-binding domain of another interferon antagonist, the NS1 protein of influenza A virus. Virology 328:177–184. doi: 10.1016/j.virol.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Kimberlin CR, Bornholdt ZA, Li S, Woods VL Jr, MacRae IJ, Saphire EO. 2010. Ebolavirus VP35 uses a bimodal strategy to bind dsRNA for innate immune suppression. Proc Natl Acad Sci U S A 107:314–319. doi: 10.1073/pnas.0910547107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bale S, Julien JP, Bornholdt ZA, Krois AS, Wilson IA, Saphire EO. 2013. Ebolavirus VP35 coats the backbone of double-stranded RNA for interferon antagonism. J Virol 87:10385–10388. doi: 10.1128/JVI.01452-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bale S, Julien JP, Bornholdt ZA, Kimberlin CR, Halfmann P, Zandonatti MA, Kunert J, Kroon GJ, Kawaoka Y, MacRae IJ, Wilson IA, Saphire EO. 2012. Marburg virus VP35 can both fully coat the backbone and cap the ends of dsRNA for interferon antagonism. PLoS Pathog 8:e1002916. doi: 10.1371/journal.ppat.1002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dilley KA, Voorhies AA, Luthra P, Puri V, Stockwell TB, Lorenzi H, Basler CF, Shabman RS. 2017. The Ebola virus VP35 protein binds viral immunostimulatory and host RNAs identified through deep sequencing. PLoS One 12:e0178717. doi: 10.1371/journal.pone.0178717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng Z, Cerveny M, Yan Z, He B. 2007. The VP35 protein of Ebola virus inhibits the antiviral effect mediated by double-stranded RNA-dependent protein kinase PKR. J Virol 81:182–192. doi: 10.1128/JVI.01006-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schumann M, Gantke T, Muhlberger E. 2009. Ebola virus VP35 antagonizes PKR activity through its C-terminal interferon inhibitory domain. J Virol 83:8993–8997. doi: 10.1128/JVI.00523-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hume A, Muhlberger E. 2018. Marburg virus viral protein 35 inhibits protein kinase R activation in a cell type-specific manner. J Infect Dis 218:S403–S408. doi: 10.1093/infdis/jiy473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edwards MR, Liu H, Shabman RS, Ginell GM, Luthra P, Ramanan P, Keefe LJ, Kollner B, Amarasinghe GK, Taylor DJ, Leung DW, Basler CF. 2018. Conservation of structure and immune antagonist functions of filoviral VP35 homologs present in microbat genomes. Cell Rep 24:861–872.e6. doi: 10.1016/j.celrep.2018.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reid SP, Leung LW, Hartman AL, Martinez O, Shaw ML, Carbonnelle C, Volchkov VE, Nichol ST, Basler CF. 2006. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J Virol 80:5156–5167. doi: 10.1128/JVI.02349-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reid SP, Valmas C, Martinez O, Sanchez FM, Basler CF. 2007. Ebola virus VP24 proteins inhibit the interaction of NPI-1 subfamily karyopherin alpha proteins with activated STAT1. J Virol 81:13469–13477. doi: 10.1128/JVI.01097-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McBride KM, Banninger G, McDonald C, Reich NC. 2002. Regulated nuclear import of the STAT1 transcription factor by direct binding of importin-alpha. EMBO J 21:1754–1763. doi: 10.1093/emboj/21.7.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sekimoto T, Imamoto N, Nakajima K, Hirano T, Yoneda Y. 1997. Extracellular signal-dependent nuclear import of Stat1 is mediated by nuclear pore-targeting complex formation with NPI-1, but not Rch1. EMBO J 16:7067–7077. doi: 10.1093/emboj/16.23.7067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mateo M, Reid SP, Leung LW, Basler CF, Volchkov VE. 2010. Ebolavirus VP24 binding to karyopherins is required for inhibition of interferon signaling. J Virol 84:1169–1175. doi: 10.1128/JVI.01372-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu W, Edwards MR, Borek DM, Feagins AR, Mittal A, Alinger JB, Berry KN, Yen B, Hamilton J, Brett TJ, Pappu RV, Leung DW, Basler CF, Amarasinghe GK. 2014. Ebola virus VP24 targets a unique NLS binding site on karyopherin alpha 5 to selectively compete with nuclear import of phosphorylated STAT1. Cell Host Microbe 16:187–200. doi: 10.1016/j.chom.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valmas C, Grosch MN, Schumann M, Olejnik J, Martinez O, Best SM, Krahling V, Basler CF, Muhlberger E. 2010. Marburg virus evades interferon responses by a mechanism distinct from Ebola virus. PLoS Pathog 6:e1000721. doi: 10.1371/journal.ppat.1000721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Valmas C, Basler CF. 2011. Marburg virus VP40 antagonizes interferon signaling in a species-specific manner. J Virol 85:4309–4317. doi: 10.1128/JVI.02575-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feagins AR, Basler CF. 2015. Amino acid residue at position 79 of Marburg virus VP40 confers interferon antagonism in mouse cells. J Infect Dis 212:S219–S225. doi: 10.1093/infdis/jiv010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.He F, Melen K, Maljanen S, Lundberg R, Jiang M, Osterlund P, Kakkola L, Julkunen I. 2017. Ebolavirus protein VP24 interferes with innate immune responses by inhibiting interferon-lambda1 gene expression. Virology 509:23–34. doi: 10.1016/j.virol.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 34.Guito JC, Albarino CG, Chakrabarti AK, Towner JS. 2017. Novel activities by ebolavirus and marburgvirus interferon antagonists revealed using a standardized in vitro reporter system. Virology 501:147–165. doi: 10.1016/j.virol.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edwards MR, Johnson B, Mire CE, Xu W, Shabman RS, Speller LN, Leung DW, Geisbert TW, Amarasinghe GK, Basler CF. 2014. The Marburg virus VP24 protein interacts with Keap1 to activate the cytoprotective antioxidant response pathway. Cell Rep 6:1017–1025. doi: 10.1016/j.celrep.2014.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Page A, Volchkova VA, Reid SP, Mateo M, Bagnaud-Baule A, Nemirov K, Shurtleff AC, Lawrence P, Reynard O, Ottmann M, Lotteau V, Biswal SS, Thimmulappa RK, Bavari S, Volchkov VE. 2014. Marburgvirus hijacks nrf2-dependent pathway by targeting nrf2-negative regulator keap1. Cell Rep 6:1026–1036. doi: 10.1016/j.celrep.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 37.Johnson B, Li J, Adhikari J, Edwards MR, Zhang H, Schwarz T, Leung DW, Basler CF, Gross ML, Amarasinghe GK. 2016. Dimerization controls Marburg virus VP24-dependent modulation of host antioxidative stress responses. J Mol Biol 428:3483–3494. doi: 10.1016/j.jmb.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Edwards MR, Basler CF. 2015. Marburg virus VP24 protein relieves suppression of the NF-kappaB pathway through interaction with Kelch-like ECH-associated protein 1. J Infect Dis 212:S154–S159. doi: 10.1093/infdis/jiv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baum A, Sachidanandam R, Garcia-Sastre A. 2010. Preference of RIG-I for short viral RNA molecules in infected cells revealed by next-generation sequencing. Proc Natl Acad Sci U S A 107:16303–16308. doi: 10.1073/pnas.1005077107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feagins AR, Basler CF. 2015. Lloviu virus VP24 and VP35 proteins function as innate immune antagonists in human and bat cells. Virology 485:145–152. doi: 10.1016/j.virol.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 41.Hartman AL, Dover JE, Towner JS, Nichol ST. 2006. Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. J Virol 80:6430–6440. doi: 10.1128/JVI.00044-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ramanan P, Edwards MR, Shabman RS, Leung DW, Endlich-Frazier AC, Borek DM, Otwinowski Z, Liu G, Huh J, Basler CF, Amarasinghe GK. 2012. Structural basis for Marburg virus VP35-mediated immune evasion mechanisms. Proc Natl Acad Sci U S A 109:20661–20666. doi: 10.1073/pnas.1213559109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Timmins J, Scianimanico S, Schoehn G, Weissenhorn W. 2001. Vesicular release of Ebola virus matrix protein VP40. Virology 283:1–6. doi: 10.1006/viro.2001.0860. [DOI] [PubMed] [Google Scholar]
- 44.Harty RN, Brown ME, Wang G, Huibregtse J, Hayes FP. 2000. A PPxY motif within the VP40 protein of Ebola virus interacts physically and functionally with a ubiquitin ligase: implications for filovirus budding. Proc Natl Acad Sci U S A 97:13871–13876. doi: 10.1073/pnas.250277297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jasenosky LD, Neumann G, Lukashevich I, Kawaoka Y. 2001. Ebola virus VP40-induced particle formation and association with the lipid bilayer. J Virol 75:5205–5214. doi: 10.1128/JVI.75.11.5205-5214.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kolesnikova L, Bugany H, Klenk HD, Becker S. 2002. VP40, the matrix protein of Marburg virus, is associated with membranes of the late endosomal compartment. J Virol 76:1825–1838. doi: 10.1128/jvi.76.4.1825-1838.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kolesnikova L, Bamberg S, Berghofer B, Becker S. 2004. The matrix protein of Marburg virus is transported to the plasma membrane along cellular membranes: exploiting the retrograde late endosomal pathway. J Virol 78:2382–2393. doi: 10.1128/jvi.78.5.2382-2393.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Michalska A, Blaszczyk K, Wesoly J, Bluyssen H. 2018. A positive feedback amplifier circuit that regulates interferon (IFN)-stimulated gene expression and controls type I and type II IFN responses. Front Immunol 9:1135. doi: 10.3389/fimmu.2018.01135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang Y, Xu L, Sun Y, Nabel GJ. 2002. The assembly of Ebola virus nucleocapsid requires virion-associated proteins 35 and 24 and posttranslational modification of nucleoprotein. Mol Cell 10:307–316. doi: 10.1016/s1097-2765(02)00588-9. [DOI] [PubMed] [Google Scholar]
- 50.Watanabe S, Noda T, Kawaoka Y. 2006. Functional mapping of the nucleoprotein of Ebola virus. J Virol 80:3743–3751. doi: 10.1128/JVI.80.8.3743-3751.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Noda T, Watanabe S, Sagara H, Kawaoka Y. 2007. Mapping of the VP40-binding regions of the nucleoprotein of Ebola virus. J Virol 81:3554–3562. doi: 10.1128/JVI.02183-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bharat TA, Noda T, Riches JD, Kraehling V, Kolesnikova L, Becker S, Kawaoka Y, Briggs JA. 2012. Structural dissection of Ebola virus and its assembly determinants using cryo-electron tomography. Proc Natl Acad Sci U S A 109:4275–4280. doi: 10.1073/pnas.1120453109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Olejnik J, Hume AJ, Leung DW, Amarasinghe GK, Basler CF, Muhlberger E. 2017. Filovirus strategies to escape antiviral responses. Curr Top Microbiol Immunol 411:293–322. doi: 10.1007/82_2017_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rehwinkel J, Tan CP, Goubau D, Schulz O, Pichlmair A, Bier K, Robb N, Vreede F, Barclay W, Fodor E, Reis e Sousa C. 2010. RIG-I detects viral genomic RNA during negative-strand RNA virus infection. Cell 140:397–408. doi: 10.1016/j.cell.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 55.Kok KH, Lui PY, Ng MH, Siu KL, Au SW, Jin DY. 2011. The double-stranded RNA-binding protein PACT functions as a cellular activator of RIG-I to facilitate innate antiviral response. Cell Host Microbe 9:299–309. doi: 10.1016/j.chom.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 56.Yen BC, Basler CF. 2016. Effects of filovirus interferon antagonists on responses of human monocyte-derived dendritic cells to RNA virus infection. J Virol 90:5108–5118. doi: 10.1128/JVI.00191-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lubaki NM, Ilinykh P, Pietzsch C, Tigabu B, Freiberg AN, Koup RA, Bukreyev A. 2013. The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J Virol 87:7471–7485. doi: 10.1128/JVI.03316-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lubaki NM, Younan P, Santos RI, Meyer M, Iampietro M, Koup RA, Bukreyev A. 2016. The Ebola interferon inhibiting domains attenuate and dysregulate cell-mediated immune responses. PLoS Pathog 12:e1006031. doi: 10.1371/journal.ppat.1006031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ilinykh PA, Lubaki NM, Widen SG, Renn LA, Theisen TC, Rabin RL, Wood TG, Bukreyev A. 2015. Different temporal effects of Ebola virus VP35 and VP24 proteins on global gene expression in human dendritic cells. J Virol 89:7567–7583. doi: 10.1128/JVI.00924-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hartman AL, Bird BH, Towner JS, Antoniadou ZA, Zaki SR, Nichol ST. 2008. Inhibition of IRF-3 activation by VP35 is critical for the high level of virulence of Ebola virus. J Virol 82:2699–2704. doi: 10.1128/JVI.02344-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Woolsey C, Menicucci AR, Cross RW, Luthra P, Agans KN, Borisevich V, Geisbert JB, Mire CE, Fenton KA, Jankeel A, Anand S, Ebihara H, Geisbert TW, Messaoudi I, Basler CF. 2019. A VP35 mutant Ebola virus lacks virulence but can elicit protective immunity to wild-type virus challenge. Cell Rep 28:3032–3046.e6. doi: 10.1016/j.celrep.2019.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paweska JT, Jansen van Vuren P, Masumu J, Leman PA, Grobbelaar AA, Birkhead M, Clift S, Swanepoel R, Kemp A. 2012. Virological and serological findings in Rousettus aegyptiacus experimentally inoculated with Vero cells-adapted Hogan strain of Marburg virus. PLoS One 7:e45479. doi: 10.1371/journal.pone.0045479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jones ME, Schuh AJ, Amman BR, Sealy TK, Zaki SR, Nichol ST, Towner JS. 2015. Experimental inoculation of Egyptian Rousette bats (Rousettus aegyptiacus) with viruses of the Ebolavirus and Marburgvirus genera. Viruses 7:3420–3442. doi: 10.3390/v7072779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Amman BR, Jones ME, Sealy TK, Uebelhoer LS, Schuh AJ, Bird BH, Coleman-McCray JD, Martin BE, Nichol ST, Towner JS. 2015. Oral shedding of Marburg virus in experimentally infected Egyptian fruit bats (Rousettus aegyptiacus). J Wildl Dis 51:113–124. doi: 10.7589/2014-08-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang AP, Bornholdt ZA, Abelson DM, Saphire EO. 2014. Crystal structure of Marburg virus VP24. J Virol 88:5859–5863. doi: 10.1128/JVI.03565-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Copple IM. 2012. The Keap1-Nrf2 cell defense pathway–a promising therapeutic target? Adv Pharmacol 63:43–79. doi: 10.1016/B978-0-12-398339-8.00002-1. [DOI] [PubMed] [Google Scholar]
- 67.Quintas-Cardama A, Vaddi K, Liu P, Manshouri T, Li J, Scherle PA, Caulder E, Wen X, Li Y, Waeltz P, Rupar M, Burn T, Lo Y, Kelley J, Covington M, Shepard S, Rodgers JD, Haley P, Kantarjian H, Fridman JS, Verstovsek S. 2010. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood 115:3109–3117. doi: 10.1182/blood-2009-04-214957. [DOI] [PMC free article] [PubMed] [Google Scholar]