Abstract
Background:
Self-blame following bereavement has been implicated in the development of post-loss psychopathology. However, prior studies have not distinguished between the emotions of shame versus guilt. This study examined the cross-sectional associations among bereavement-related shame, bereavement-related guilt, and two mental disorders that commonly arise after bereavement: complicated grief and depression. In addition, exploratory analyses examined the associations between bereavement-related pride and post-loss psychopathology.
Methods:
Participants included 92 bereaved adults who experienced the death of a family member at least one year prior to the study. Participants completed self-report measures of complicated grief symptoms, depression symptoms, shame, guilt, and pride.
Results:
Shame and guilt were positively correlated with complicated grief and depression symptoms. When controlling for their shared variance, only shame remained a significant predictor of post-loss psychopathology. Follow-up analyses indicated that the effect of guilt on psychopathology depended on the level of shame, and vice versa. At low shame, guilt predicted psychopathology; however guilt did not predict psychopathology at moderate to high shame. At low to moderate guilt, shame predicted psychopathology; however shame did not predict psychopathology at high guilt. Pride negatively predicted depression symptoms, but not complicated grief symptoms, when we controlled for shame and guilt.
Limitations:
Limitations include the cross-sectional design and modest sample size.
Conclusions:
Our analyses identify shame as the more pathogenic moral emotion for bereaved adults. However, whereas guilt in the absence of shame is often considered adaptive, we found that guilt predicted greater psychological distress at low levels of shame in this sample.
Bereavement is a universal human experience. Most people will experience the death of a loved one during their lifetime. However, the ubiquity of loss does not render it any less distressing. Those left behind often experience a host of grief-related symptoms such as preoccupation with thoughts about the deceased, yearning for the deceased, and pangs of painful emotions (Shear et al., 2007). These symptoms typically lessen in intensity and frequency during the first year post-loss (Shear et al., 2007). However, a minority of bereaved individuals (approximately 9.8%; Lundorff et al., 2017) experience a syndrome of persistent and severe grief symptoms associated with distress, psychosocial impairment, and increased risk for suicide (Shear et al., 2011). This syndrome has been called by a variety of names in the literature, including Traumatic Grief, Prolonged Grief, and Complicated Grief. It was included as a condition warranting further study in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM5) under the name Persistent Complex Bereavement Disorder (PCBD; APA, 2013), and listed in the 11th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-11) under the name Prolonged Grief Disorder (WHO, 2018). The diagnostic criteria for this syndrome continue to be debated, and researchers use a variety of diagnostic tests to identify individuals with pathological grief (see O’Connor et al., 2019). Henceforth, we use the term Complicated Grief (CG) to refer to this pathological grief syndrome rather than to a specific set of diagnostic criteria.
Bereavement is also associated with increased risk for Major Depressive Disorder (MDD). The prevalence of MDD among bereaved individuals ranges from 20–60% (Clesse et al., 2015; Zisook et al., 1997), and is elevated relative to non-bereaved populations (Zisook and Shuchter, 1991). MDD following bereavement is associated with social and occupational impairment and physical health problems (Zisook and Shuchter, 1993). Though CG and MDD are highly comorbid (Simon et al., 2007), factor analytic studies suggest they are separate disorders (Boelen and Prigerson, 2007). CG is characterized by symptoms of intense separation distress (e.g., yearning, waves of emotional pain), whereas bereavement-related MDD is characterized by pervasive sadness and anhedonia. Given the morbidity and mortality associated with both disorders, research efforts have focused on identifying factors that may inhibit recovery from loss and lead to the development of CG, bereavement-related MDD, or both.
Grief researchers have long recognized that self-blame and its emotional correlates (e.g., shame and guilt) may hinder healthy grieving. Miles and Demi (1983-84) conducted an early literature review on guilt following loss, noting that it often accompanied post-loss psychopathology. More recently, Li et al. (2014) conducted an updated review of quantitative and qualitative studies on guilt in bereavement, and concluded that guilt is linked with poor physical health, traumatic reactions, and CG symptoms. Several longitudinal studies have further demonstrated that self-blame and guilt prospectively predict more severe grief symptoms following loss (Li et al., 2018; Stroebe et al., 2014). Self-blame following loss can take many forms, including thoughts about contributing to the death or failing to prevent it, self recriminations for acts done or not done during the deceased’s life, or general negative thoughts about surviving the deceased or about experiencing positive emotions in his or her absence (Miles and Demi, 1983-84; Shear et al., 2007).
Emotion science suggests that these kinds of self-blaming cognitions can give rise to two distinct moral emotions: shame and guilt (Tangney et al., 2007). These emotions are differentiated by the focus of negative evaluation; guilt arises when negative evaluation is restricted to a particular behavior (e.g., “I did a bad deed”), whereas shame arises when negative evaluation is applied to the whole self (e.g., “I am a bad person.”; Tangney et al., 2007). This distinction is more than semantic, as those experiencing shame report more intense negative affect as well as greater feelings of inferiority and isolation (Tangney and Dearing, 2002, p. 197). Tangney et al. (2007) theorize that shame is more emotionally painful than guilt because it threatens a person’s identity and is more difficult to resolve. An individual experiencing guilt can apologize or make amends, but an individual experiencing shame must revise his or her entire sense of self (Tangney et al., 2007).
Perhaps not surprisingly, shame also demonstrates a stronger and more consistent relationship with psychopathology than guilt does. Across a range of studies, researchers have shown that individuals with high shame report psychological distress, including heightened levels of anxiety, depression, and suicidal ideation (Candea and Szentagotai-Tata, 2018; Kim et al., 2011; Tangney et al., 2007). Although guilt is also associated with psychological distress in bivariate analyses (Candea and Szentagotai-Tata, 2018; Kim et al., 2011; Tangney et al., 2007), when multivariate models control for the shared variance between guilt and shame, guilt is typically no longer related to anxiety, depression, and other symptoms of psychopathology (Candea and Szentagotai-Tata, 2018; Kim et al., 2011; Tangney et al., 2007).
In the bereavement literature, few studies have used measures that distinguish between shame and guilt or controlled for their shared variance. Thus, the observed relationship between post-loss psychopathology and guilt (e.g., Li et al., 2014; Miles and Demi, 1983-84) may be better explained by an unmeasured relationship between post-loss psychopathology and shame. Duncan and Cacciatore (2015) conducted a systematic review of the literature on self-blame, shame, and guilt among bereaved parents and found that only three studies on this topic used measures that adequately distinguish between shame and guilt. In two of these studies, variants of shame-proneness and guilt-proneness were independently associated with grief after controlling their shared variance, with similar effect sizes for shame-proneness and guilt-proneness (Barr, 2004; Barr and Cacciatore, 2007–2008). In a third study, variants of both shame-proneness and guilt-proneness were associated with grief, but the authors did not control for their shared variance in analyses (Barr, 2012). These results suggest that, distinct from other conditions, both ‘shame-free guilt’ and ‘guilt-free shame’ may be associated with post-loss psychopathology. However, these studies measured dispositional tendencies towards shame and guilt rather than the affective experience of shame and guilt in response to bereavement. It therefore remains unknown whether bereavement-related shame and guilt are independently associated with post-loss psychopathology.
In addition, it is unknown how bereavement-related pride may affect the grieving process. Pride is a moral emotion that arises in response to positive appraisals of one’s behavior (Tangney et al., 2007). Bereavement-related pride could result from providing comfort to the deceased, honoring his or her last wishes, or managing logistics following the loss. Pride may protect against the development of loss-related psychopathology. In one study, self-worth (a composite variable reflecting happiness, relief, and pride post-loss) prospectively predicted reductions in grief symptoms in a conjugally bereaved sample (Bonanno et al., 1999). In another study, individuals with enhanced self-perceptions demonstrated lower grief symptoms following spousal loss (Bonanno et al., 2002). Pride might be protective if it helps to counteract the negative cognitions that often arise following negative life events (Bonanno et al., 2002). However, to our knowledge, no prior studies have directly examined the relationship between bereavement-related pride and post-loss symptoms.
The present study
The primary aim of the present study was to examine the cross-sectional associations between bereavement-related shame, bereavement-related guilt, and symptoms of two disorders that commonly co-occur following bereavement: CG and MDD (Shear et al., 2011). Given that both shame- and guilt-proneness have independently predicted grief (Barr, 2004; Barr and Cacciatore, 2007–2008), we expected that bereavement-related shame and guilt would independently predict more severe CG and depression symptoms in our sample. To gain a more nuanced understanding of the relationship between moral emotions and post-loss psychopathology, we also examined whether shame moderated the effect of guilt on psychopathology, as well as whether guilt moderated the effect of shame on psychopathology.
In addition to this primary aim, we also conducted exploratory analyses to examine the association between bereavement-related pride and post-loss psychopathology. Given that self-worth and self-enhancement have negatively predicted grief symptoms in prior studies (Bonanno et al., 2002; Bonanno et al., 1999), we expected that bereavement-related pride would predict less severe CG and depression symptoms above and beyond the variance accounted for by shame and guilt.
Method
Participants and procedure
The present study is a secondary analysis of data collected as part of a larger study examining the role of cognitive factors in the development and maintenance of post-loss psychopathology (Robinaugh, 2018). Bereaved adults were recruited for the larger study from December 2012 through March 2015 via online advertisements, newspaper advertisements, flyers, referral from local treatment centers, and word of mouth. Individuals qualifying for the present study experienced the death of a family member at least one year prior to participation and were 21–65 years old. Exclusion criteria included an inability to speak English, current mania or psychosis, and any other factors that rendered the participant unable to provide informed consent or understand the study procedures.
The Harvard University Institutional Review Board approved procedures for the larger study, which comprised three laboratory visits. Self-report data included in the present analysis were collected during the first visit. During this visit, participants first provided informed consent and then generated a list of people, places, and objects from their lives, to be used in a later experimental task. Study staff then administered the MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998) to assess for study exclusion criteria. Finally, participants completed demographic and self-report questionnaires via the online survey tool Qualtrics (Qualtrics, Provo, UT). Participants received $20.00 for completion of this first visit and up to $80.00 for participation in the full study. A total of 105 individuals were screened for the larger study and 97 met inclusion/exclusion criteria and completed visit one. Of those participants, 92 completed the State Shame Guilt Scale (Tangney and Dearing, 2002) and are included in the present analyses.
Measures
Demographics and loss-related variables.
A self-report questionnaire was used to obtain information about participants’ demographic characteristics and index loss.
Inventory of Complicated Grief (ICG; Prigerson et al., 1995).
The ICG is a self-report measure that assessed participants’ current CG symptoms. The ICG is comprised of 19 items that assess the frequency with which respondents are currently experiencing CG symptoms. Respondents rate their frequency for each item on a 5-point Likert scale that ranges from 0 (never) to 4 (always). The total score is the sum of all 19 items. Scores range from 0–76 and higher scores indicate more severe CG symptoms. In a sample of conjugally bereaved older adults, a cut-off score of ≥ 26 on the ICG identified the upper quintile of the sample (Prigerson et al., 1995). In this study, those with scores ≥ 26 had significantly worse mental health, physical health, and social functioning, compared to the rest of the sample and thus had probable current CG (Prigerson et al., 1995). However, given that the diagnostic criteria for CG are still under debate, the sensitivity and specificity of this cut-off score cannot be calculated. In the present study, the ICG demonstrated excellent reliability (α = .94).
Quick Inventory of Depressive Symptomatology – Self Report (QIDS-SR; Rush et al., 2003).
The QIDS-SR is a self-report measure that assessed participants’ depression symptom severity over the past week. The QIDS-SR consists of 16 items that assess the 9 Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV; APA, 1994) diagnostic criteria for major depressive disorder (MDD; 4 items assess sleep disturbance, 4 items assess appetite/weight disturbance, 2 items assess psychomotor symptoms, and a single item assesses the remaining criteria). Respondents rate each item on a 4-point Likert scale that ranges from 0 (least severe) to 3 (most severe). The QIDS-SR is scored by first taking the maximum score for the sleep items, the appetite items, and the psychomotor items. The 9 DSM-IV MDD symptom scores are then summed. Scores range from 0–27, with higher scores indicating more severe depression symptoms. The QIDS-SR demonstrated good divergent validity in a mixed psychiatric sample, with individuals with current MDD scoring higher than individuals without current MDD (Weiss et al., 2015). In the same study, a cut-off score of ≥ 12 on the QIDS-SR optimized sensitivity (0.74) and specificity (0.77) for identifying individuals with current MDD (Weiss et al., 2015). In the present study, the QIDS-SR demonstrated good reliability (α = .82).
State Shame and Guilt Scale (Tangney and Dearing, 2002).
A modified version of the State Shame and Guilt Scale assessed participants’ subjective levels of shame, guilt, and pride with regard to the death of their deceased loved one. The State Shame and Guilt Scale is a self-report measure comprising 15 items, with 5 items measuring state shame, guilt, and pride, respectively. Participants rate their agreement with each item on a 5-point Likert scale that ranges from 1 (not feeling this way at all) to 5 (feeling this way strongly). Subscale scores are obtained by summing the relevant items. Subscale scores range from 5–25, with higher scores indicating higher shame, guilt, or pride. In a sample of individuals with current MDD, mean(SD) scores for the shame, guilt, and pride subscales were 13.4(5.1), 14.0(5.0), and 10.3(4.2), respectively (Ghatavi et al., 2002). In a sample of healthy controls, mean(SD) scores for the shame, guilt, and pride subscales were 5.6(1.3), 6.1(2.0), and 20.1(3.3), respectively (Ghatavi et al., 2002). In the present study, the original scale instructions were modified such that participant were instructed to “rate each statement based on how you typically feel when you think about the death of your loved one and the circumstances surrounding the death.” For complete instructions provided to participants, see Supplementary Materials. None of the individual items was modified. In the present study, the three subscales demonstrated good internal consistency: shame (α = .72), guilt (α = .83), and pride (α = 88).
Analytical approach
Prior to analyses, questionnaire responses were screened for item-level missing data. Item-level data were missing for 20 of the possible 3956 item-level responses from which total scores were calculated (0.5% of item-level responses). Given that fewer than 5% of item-level data were missing, these data did not require missing data treatment such as multiple imputation (McKnight and McKnight, 2013). In order to retain all 92 participants in the present analyses, we replaced item-level missing data values with the participant-level mean for the relevant scale or subscale. Total scores were then calculated using these mean-imputed data. Results reported below therefore include data from all 92 participants in the sample. To evaluate the effect of handling missing data in this way, we also performed all analyses with the raw data, eliminating participants with missing values via list-wise deletion. The majority of the results remain unchanged. Where results differ, these differences are noted in the results.
Analyses were conducted with SPSS Version 25.0 (IBM Corp, Amonk, NY). Pearson product-moment correlations were used to examine bivariate associations between the ICG, QIDS-SR, and State Shame and Guilt Scale subscales. Linear regression models were used to examine the independent associations of State Shame and Guilt Scale subscales with post-loss symptoms. We used the PROCESS macro for SPSS (Hayes, 2013) to conduct analyses examining moderation, specifically the analyses examining the interaction of shame and guilt, shame and pride, and guilt and pride as predictors of post-loss symptoms. The PROCESS macro uses hierarchical linear regression to estimate the significance of the interaction between the independent variable (X) and the moderator in predicting the dependent variable (Y). We probed significant interactions via the PROCESS macro by using the Johnson-Neyman technique. The Johnson-Neyman technique identifies the value(s) of the moderator at which the conditional effect of X on Y becomes significant. This objective is achieved by calculating the value or values of M for which the ratio of the conditional effect to its standard error is equal to tcrit where p = α (Hayes, 2013, p. 239). If these calculations yield a single value (JN1), this suggests that the effect of X on Y is significant when M ≤ JN1 or when M ≥ JN1 (Hayes, 2013, p. 240). If these calculations yield two values (JN1 and JN2), this suggests that the effect of X on Y is significant when JN1 ≤ M ≤ JN2 or when M ≤ JN1 and M ≥ JN2 (Hayes, 2013, p. 240). This technique is preferred over the pick-a-point approach to probing interactions, as it does not rely on an arbitrary choice of moderator values for interpretation (Hayes, 2013, p. 238–239).
Results
Sample Characteristics
Most participants were female (65.2%) and ranged in age from 21–65 years old (M = 45.12, SD = 12.51). Most participants identified as either Black/African American (48.9%) or White/Caucasian (41.3%), with 9.8% identifying as other ethnicities. The majority of participants had experienced the death of a family member 1–29 years prior to study entry (M = 5.61, SD = 6.24). Three participants reported a time since the death of less than one year; one reported a time since the death of 363 days, a second reported a time since the death of 98 days, and a third reported a date of death after study participation. For these latter two participants, the recorded date of death likely reflects participant data entry errors, as participants were screened for this inclusion criterion prior to study entry. We repeated all analyses excluding the three participants with a time since the loss of less than one year, and findings were unchanged.
Losses included parents (53.3%), siblings (19.6%), spouses (13.0%), children (6.5%), and other family members (7.6%; four grandparents, an aunt, a cousin, and a grandchild). Losses were a result of long-term illness/natural causes (47.8%), sudden illness (28.3%), accident (7.6%), homicide (7.6%), suicide (3.3%), overdose (1.1%), or unknown/missing (4.3%).
The mean ICG score for the sample was 26.72 (SD = 16.51), with 50.0% of participants scoring above a cut-off score of ≥ 26, which is indicative of probable CG (Prigerson et al., 1995). The mean QIDS score for the sample was 8.12 (SD = 5.33), with 24% scoring above a cut-off score of ≥ 12, which is indicative of probable MDD (Weiss et al., 2015). Overall, participants endorsed relatively low levels of shame (M = 7.80, SD = 3.44) and guilt (M = 9.08, SD = 4.31), and moderate levels of pride (M= 15.64, SD= 5.70), in connection with their index loss.
Bivariate Association
Zero-order correlations between moral emotions and post-loss symptoms appear in Table 1. Shame and guilt were positively associated with CG and depression symptoms. Pride was negatively associated with CG and depression symptoms.
Table 1.
Zero-order correlations of shame, guilt, pride, and CG and depression symptoms.
| Shame | Guilt | Pride | ICG | QIDS | |
|---|---|---|---|---|---|
| Shame | -- | ||||
| Guilt | .54** | -- | |||
| Pride | −.43** | −.28** | -- | ||
| ICG | .45** | .39** | −.25* | -- | |
| QIDS | .43** | .38** | −.41** | .73** | -- |
Note.
p < .05;
p < .01. ICG = Inventory of Complicated Grief, QIDS = Quick Inventory of Depressive Symptomatology.
Shame and Guilt as Predictors of Post-loss Psychopathology
Results of the regression analyses examining shame and guilt as predictors of CG symptoms are presented in Table 2. Shame and guilt were entered in the first step of the model. Consistent with our expectations, shame remained a significant predictor of CG symptoms after controlling for guilt. Contrary to our expectations, guilt was not independently associated with CG symptoms after controlling for shame. The interaction between shame and guilt was entered in the second step of the model. We observed a significant interaction between shame and guilt in the prediction of CG symptoms. To probe this interaction, we first examined shame as a moderator of the effect of guilt on CG symptoms. Guilt was positively associated with CG symptoms at values of shame < 8.99, whereas guilt was not significantly associated with CG symptoms at values of shame ≥ 8.99 (see Figure 1). To further probe the interaction, we also examined guilt as a moderator of the effect of shame on CG symptoms. Shame was positively associated with CG symptoms at values of guilt < 13.04, whereas shame was not significantly associated with CG symptom at values of guilt ≥ 13.04 (see Figure 2).
Table 2.
Grief-related psychopathology predicted by shame, guilt, and their interaction.
| ICG predicted by shame, guilt, and their interaction |
QIDS predicted by shame, guilt, and their interaction |
||||||
|---|---|---|---|---|---|---|---|
| B | SE | P | B | SE | P | ||
| Step 1 | Step 1 | ||||||
| Constant | 6.90 | 4.13 | .098 | Constant | 1.92 | 1.34 | .156 |
| Shame | 1.59 | 0.53 | .003 | Shame | 0.49 | 0.17 | .006 |
| Guilt | 0.82 | 0.42 | .056 | Guilt | 0.26 | 0.14 | .059 |
| Step 2a | Step 2b | ||||||
| Constant | −9.30 | 7.91 | .243 | Constant | −3.48 | 2.57 | .180 |
| Shame | 3.59 | 0.99 | .001 | Shame | 1.16 | 0.32 | .001 |
| Guilt | 2.53 | 0.83 | .003 | Guilt | 0.84 | 0.27 | .003 |
| Shame × Guilt | −0.19 | 0.08 | .020 | Shame × Guilt | −0.06 | 0.03 | .017 |
R2 Δ = .05, F (1,88) = 5.65, p = .020
R2 Δ = .05, F (1,88) = 5.94, p = .017
Note. ICG = Inventory of Complicated Grief; QIDS = Quick Inventory of Depressive Symptomatology.
Figure 1.
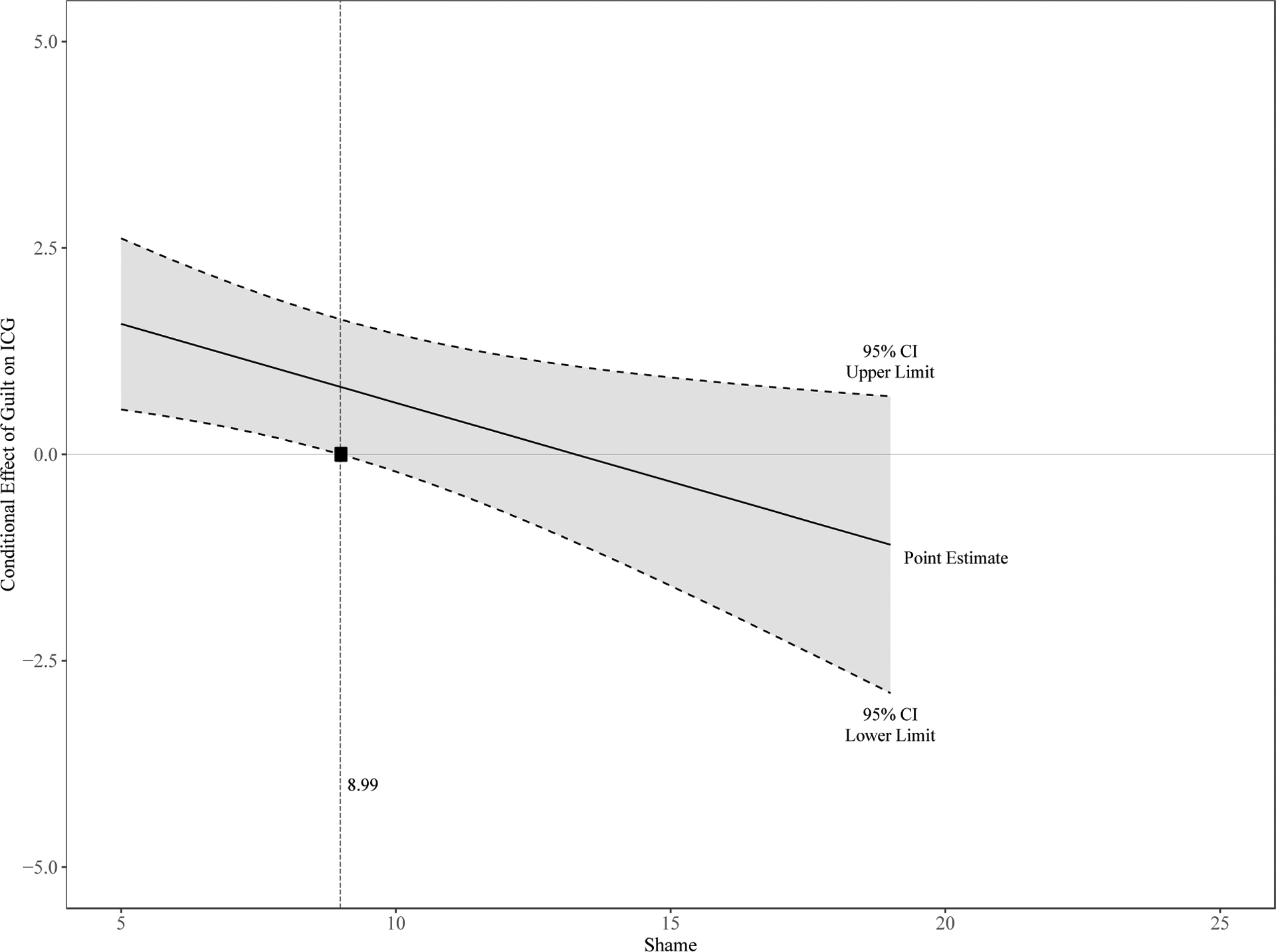
Conditional effect of guilt on CG symptoms at different levels of shame.
Note. Solid line represents the point estimate for the conditional effect of guilt on CG symptoms at different levels of shame. Dashed lines represent the upper and lower limit of the 95% confidence interval around this point estimate. Levels of shame for which the 95% confidence interval does not include zero (i.e. levels of shame from 5–8.99) indicate levels of shame for which the effect of guilt on CG symptoms is significant. The State Shame and Guilt Scale shame subscale ranges from 5–25.
Figure 2.
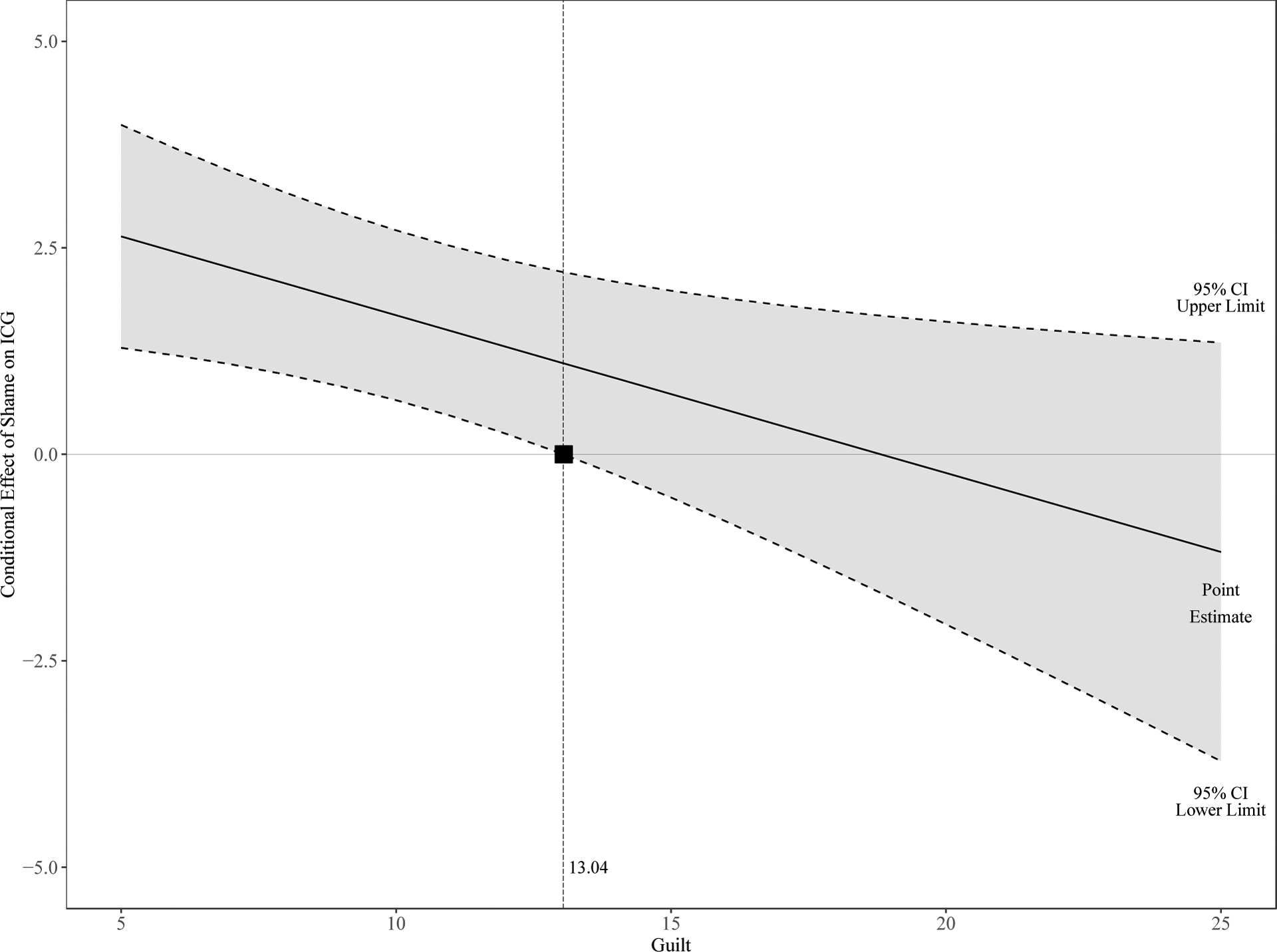
Conditional effect of shame on CG symptoms at different levels of guilt.
Note. Solid line represents the point estimate for the conditional effect of shame on CG symptoms at different levels of guilt. Dashed lines represent the upper and lower limit of the 95% confidence interval around this point estimate. Levels of guilt for which the 95% confidence interval does not include zero (i.e. levels of guilt from 5–13.04) indicate levels of guilt for which the effect of shame on CG symptoms is significant. The State Shame and Guilt Scale guilt subscale ranges from 5–25.
Results of the regression analyses examining shame and guilt as predictors of depression symptoms are presented in Table 2. Shame and guilt were entered in the first step of the model. Consistent with our expectations, shame remained a significant predictor of depression symptoms after controlling for guilt. Contrary to our expectations, guilt was not independently associated with depression symptoms after controlling for shame. The interaction between shame and guilt was entered in the second step of the model. We observed a significant interaction between shame and guilt in the prediction of depression symptoms. To probe this interaction, we first examined shame as a moderator of the effect of guilt on depression symptoms. Guilt was positively associated with depression symptoms at values of shame < 8.94, whereas guilt was not significantly associated with depression symptoms at values of shame ≥ 8.94. We also examined guilt as a moderator of the effect of shame on depression symptoms. Shame was positively associated with depression symptoms at value of guilt < 12.64, whereas shame was not significantly associated with depression symptoms at values of guilt ≥ 12.64.
The Role of Pride
Analyses examining the effect of pride on post-loss psychopathology are summarized here and presented in full in the supplementary materials. We first conducted analyses to examine the effect of shame, pride, and their interaction on CG symptoms. Pride was not associated with CG symptoms after controlling for shame, nor was the interaction between shame and pride a predictor of CG symptoms. The same pattern of findings emerged when guilt and pride were regressed on CG symptoms. We then conducted analyses to examine the effect of shame, pride, and their interaction on depression symptoms. Pride was negatively associated with depression symptoms even after controlling for shame, though the interaction between shame and pride was not significant. The same pattern of findings appeared when guilt and pride were regressed on depression symptoms. Together, these findings suggest that bereavement-related pride may be uniquely associated with depression but not CG symptoms in bereaved adults.
Discussion
The primary aim of the present study was to examine the cross-sectional associations between bereavement-related shame, bereavement-related guilt, and post-loss psychopathology. In bivariate analyses, shame and guilt were both associated with more severe CG and depression symptoms. However, in multivariate analyses that accounted for the shared variance between these emotions, shame remained a significant predictor of CG and depression symptoms, whereas guilt did not. These findings are consistent with prior research showing that the association between guilt and psychopathology is typically nonsignificant after controlling for shame (Candea and Szentagotai-Tata, 2018; Kim et al., 2011). However, the results of our moderation analyses suggest that there is nuance to the interrelationships between shame, guilt, and psychopathology in our bereaved sample. Specifically, guilt was positively associated with post-loss symptoms at low levels of shame, but not significantly associated with symptoms at medium to high levels of shame. Furthermore, shame was positively associated with post-loss symptoms at low to medium levels of guilt, but not significantly associated with symptoms at high levels of guilt. Though cross-sectional, these results suggest that both bereavement-related shame and bereavement-related guilt may interfere with recovery from loss.
Bereavement-related Shame
Our finding that bereavement-related shame predicted both CG and depression symptoms at low to medium levels of guilt was not surprising, as shame is consistently linked with a range of psychological symptoms in the literature, including depression, anxiety, anger, suicidal ideation, and posttraumatic stress disorder (PTSD) symptoms (Tangney et al., 2007; Tangney et al., 1992). The present results indicate that shame is similarly predictive of psychopathology following bereavement. Researchers theorize that the experience of shame leads to intense emotional pain arising from the belief that the self is fundamentally flawed and therefore unacceptable to one’s social group (Tangney et al., 2007). Exclusion from one’s social group would have led to survival threats throughout our evolutionary history, and humans therefore respond to such threats with intense emotional or social pain (see Eisenberg and Lieberman, 2004; MacDonald and Leary, 2005). The intense negative affect associated with shame may be further exacerbated by a lack of apparent coping behaviors, as there are no clear strategies one can employ to reform a defective self (Tangney et al., 2007). As a result, individuals experiencing shame typically engage in maladaptive coping behaviors such as hiding or responding with hostility (Tangney et al., 2007). Both of these action tendencies could interfere with recovery from loss, as hiding might lead to avoidance behavior (e.g., declining social invitations) and hostility may result in conflict within existing interpersonal relationships. Further research is therefore warranted to understand how bereavement-related shame might contribute to the development of CG and depression. Surprisingly, shame did not predict post-loss symptoms at high levels of guilt in our sample; however, high guilt strongly predicted psychopathology, which likely left limited variance to be explained by shame.
The present results also underscore the importance of assessing and treating shame in clinical practice with bereaved individuals. Clinicians should be aware of risk factors for bereavement-related shame. For example, losses due to suicide and sudden unnatural causes (e.g., drug overdose) have been associated with increased stigma and shame (Pitman et al., 2016; Valentine et al., 2016). With regard to treatment, both opposite-to-emotion action (Rizvi and Linehan, 2005) and self-compassion training (Au et al., 2017) have demonstrated efficacy for reducing shame in clinical populations, and could be studied as adjuncts to empirically-supported interventions for CG and depression.
Bereavement-related Guilt
We found that guilt predicted CG and depression symptoms at low shame, but did not predict symptoms at medium to high shame. Thus, it appears that the effect of shame on psychopathology is so strong that even moderate levels of shame leave limited variance to be explained by guilt. However, for individuals with minimal shame, bereavement-related guilt did predict psychopathology. Guilt scores for participants with shame scores < 9 demonstrated considerable variability (M = 7.72, SD = 3.70), which suggests that a significant proportion of bereaved adults may experience the pernicious effects of guilt in the absence of shame. These findings are surprising given that shame-free guilt is typically considered to be adaptive and is usually unrelated to psychological symptoms (Tangney et al., 2007). However, few prior studies have examined whether shame moderates the effect of guilt on psychological symptoms, which raises the possibility that this pattern of results might generalize to other psychiatric samples. To our knowledge, Robinaugh and McNally (2010) conducted the only prior study to examine the interaction between shame and guilt when predicting psychological symptoms, and found a nonsignificant interaction for the prediction of PTSD and depression symptoms in an unselected sample. Additional research is therefore needed to clarify the boundary conditions of the observed moderation effect. Guilt in the absence of shame may generally be adaptive if it motivates foresight and promotes prosocial behavior (Tangney et al., 2007); however, guilt may be uniquely destructive when experienced in reference to the death of a loved one.
Why might guilt in reference to the death of a loved one be uniquely predictive of psychopathology? One possibility is that guilt is a component of the separation distress that is activated following the death of an attachment figure. Theorists believe that the evolutionary function of guilt was to maintain close relationships (i.e. attachment relationships), which would have been necessary for human survival (Baumeister et al., 1994). The death of an attachment figure is thought to trigger an instinctive response of the attachment system that includes yearning, emotional pain, and preoccupation with thoughts about the deceased (Shear et al., 2007). Guilt may be another instinctive response of the attachment system following loss, as it signals (however illogically) a failure to protect or maintain the relationship (Shear et al., 2007). Thus, the guilt reported by participants in the present study may simply be part of persistent separation distress for some bereaved individuals.
In addition, specific forms of bereavement-related guilt may inhibit recovery from loss, leading to an increased risk for CG or depression. Contextually maladaptive guilt (i.e. guilt for events over which an individual has no control) is a variant of guilt that could interfere with the grieving process. Studies have shown that contextually maladaptive guilt is associated with psychopathology at a magnitude similar to shame (Candea and Szentagotai-Tata, 2018; Kim et al., 2011). Rumination about irrational counterfactual scenarios in which the death could have been prevented might inhibit grief recovery if it distracts the bereaved individual from engaging with painful thoughts about the reality of the loss (Eisma et al., 2013). In support of this hypothesis, research has shown that experiential avoidance mediates the prospective effect of grief-related rumination on CG symptoms (Eisma et al., 2013).
On the other hand, justified guilt could also inhibit grief recovery if the act for which the bereaved individual feels guilty is not directly repairable. In reference to the benign emotional effects of guilt, Tangney et al. (2007) note, “a person (a) often has the option of changing the objectionable behavior; (b) or even better yet, has an opportunity to repair the negative consequences; (c) or at the very least, can extend a heartfelt apology,” (p. 353). Sadly, none of these options is possible with regard to a transgression against the deceased, making it difficult for a bereaved individual to resolve justified guilt related to the loss. Such unresolved guilt could lead to persistent negative affect that impairs grief recovery.
The present results also underscore the importance of addressing guilt, in addition to shame, in clinical practice with bereaved individuals. First, careful assessment to differentiate shame versus guilt is paramount, as these emotions arise from distinct appraisals and likely require different interventions. Future studies should explore whether measures such as the State Shame and Guilt Scale could be integrated into treatment to help patients differentiate between these moral emotions. Second, clinicians may need different interventions to target different forms of guilt. For contextually maladaptive guilt, there is some evidence that cognitive therapy (e.g., Cognitive Processing Therapy) may be effective for dismantling hindsight bias and other irrational beliefs about responsibility (Resick et al., 2002). Less is known about effective strategies for aiding those with justified guilt. Litz et al. (2009) developed a treatment called Adaptive Disclosure to treat psychological distress among individuals who have acted outside of their moral beliefs. As part of Adaptive Disclosure, patients are encouraged to engage in good deeds as a way to promote self-forgiveness and affirm a moral identity (not as a way to make amends, which is typically not possible). Future studies should explore the acceptability and efficacy of these strategies for targeting bereavement-related guilt.
Bereavement-related Pride
Finally, the present study was also the first to investigate the association between bereavement-related pride and CG and depression symptoms. In bivariate analyses, pride was negatively associated with both CG and depression symptoms. In multivariate analyses, pride did not predict significant variance in CG symptoms above and beyond shame or guilt, suggesting that pride fails to exert a protective function with regard to grief recovery beyond its association with these negative moral emotions. However, pride did remain negatively associated with depression symptoms in multivariate models that controlled for shame and guilt. These results are in contrast to prior findings that self-worth and self-enhancement following loss are associated with less severe grief (Bonanno et al., 2002; Bonanno et al., 1999). However, bereavement-related shame and guilt were not controlled in these prior studies and might have driven the observed effects. Alternatively, it may be that pride connected to the loss event does little to ameliorate the intense separation distress that is at the core of CG, whereas global positive beliefs about the self do buffer against separation distress. Future studies should explore these hypotheses. The finding that bereavement-related pride predicted depression symptoms and not CG symptoms in our sample is noteworthy, as it is unusual to find a correlate specific to one disorder in bereaved samples. Individuals with depression have deficits in the experience of positive emotions (Watson et al., 1988), whereas this may not be the case for individuals with CG (see LeBlanc et al., 2016). Furthermore, compared to other positive emotions, pride appears to be particularly dampened among individuals with depression (Gruber et al., 2011). Future studies should therefore seek to replicate the present findings, as they may indicate important phenomenological differences between CG and depression.
Strengths and Limitations
The results of the present study should be interpreted in the context of the study strengths and limitations. The primary strength of the study was the use of the modified State Shame and Guilt Scale to measure experiences of moral emotions in reference to the death of a loved one. Prior studies on moral emotions and grief have failed to distinguish between shame and guilt, or have relied on trait measures of shame- and guilt-proneness (Barr, 2004; Barr and Cacciatore, 2007–2008). The present study addressed this gap in the literature, though we did not measure distinct forms of bereavement-related guilt (e.g., survivor guilt), which would have aided interpretation of the present findings. Notably, we modified the instructions of the State Shame and Guilt Scale, thus raising the possibility that established psychometric properties may not apply for the modified scale. Another strength of the study was the recruitment of a bereaved sample with considerable variability in CG and depression symptoms. Indeed, the prevalence of probable CG in the present study was 50%, which is much higher than the prevalence of 9.8% observed in representative bereaved populations (Lundorff et al., 2017). The severity of the present sample may have illuminated specific relationships between moral emotions and symptoms that would have been missed in a healthier sample. For example, maladaptive forms of guilt (e.g., contextually malapative guilt, surivor guilt) may be most apparent among individuals with more severe symptoms.
The primary limitation of the study was the cross-sectional design, which did not allow for conclusions regarding the direction of observed effects. Longitudinal research has shown that self-blame following loss prospectively predicts more severe grief symptoms above and beyond initial grief symptoms (Stroebe et al., 2014), suggesting that shame and guilt may indeed be risk factors for bereavement-related psychopathology. However, longitudinal studies are needed to examine whether the emotions of shame and/or guilt prospectively predict impaired grief recovery. In addition, we lacked information about the behaviors that participants’ referenced when completing the State Shame and Guilt Scale. This information might have enabled us to distinguish between contextually maladaptive versus justified guilt in our sample. Finally, the present sample was relatively small and the majority of participants were bereaved of a parent. Therefore, replication of these results in a larger and more heterogeneous bereaved sample is important. The modest sample size also prevented us from adjusting analyses for loss-related variables (e.g., relationship to the deceased, cause of death) that predict CG (e.g., Fujisawa et al., 2010). Future studies should therefore explore whether moral emotions explain variance in post-loss symptoms above and beyond these established predictors.
Conclusions
Theorists, researchers, and clinicians have long recognized the relevance of moral emotions to recovery from loss. However, most prior studies on this topic have failed to distinguish between shame and guilt, making it difficult to identify a clear relationship between shame, guilt, and post-loss psychopathology. In the present study, we addressed this limitation by using a measure that carefully distinguishes between bereavement-related shame and bereavement-related guilt. Our findings indicate that individuals experience both of these moral emotions following loss – sometimes separately and sometimes in tandem. Further, our results suggest that both bereavement-related shame and bereavement-related guilt are predictive of post-loss symptoms. The primary implication of these findings is the importance of assessing shame and guilt in bereaved samples, in both clinical practice and research, by using measures that carefully distinguish between these two emotions. In addition, our findings clarify important directions for future research, including the need for longitudinal studies to examine shame and guilt as risk factors for CG and depression, as well as the need for studies examining the efficacy of interventions that target shame and guilt following loss.
Supplementary Material
Highlights.
Shame and guilt are positively correlated with post-loss psychopathology.
Shame predicts post-loss psychopathology when guilt is in the low to medium range.
Guilt predicts post-loss psychopathology when shame is in the low range.
Acknowledgements:
We thank Heidi Vuletich for contributing to the conceptualization of the present study as well as helping with data collection.
Role of the funding source: The present study was supported by the Sackler Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of conflict of interest: None
References
- APA, 1994. Diagnostic and statistical manual of mental disorders, 4th edition (DSM-IV). American Psychiatric Association, Washington, D.C. [Google Scholar]
- APA, 2013. Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association, Washington, D.C. [Google Scholar]
- Au TM, Sauer-Zavala S, King MW, Pretrocchi N, Barlow DH, Litz B, 2017. Compassion-based therapy for trauma-related shame and posttraumatic stress: Initial evaluation using a multiple baseline design. Behavior Therapy 48, 207–221. doi: 10.1016/j.beth.2016.11.012 [DOI] [PubMed] [Google Scholar]
- Barr P, 2004. Guilt- and shame-proneness and the grief of perinatal bereavement. Psychology and Psychotherapy: Theory, Research, and Practice 77, 493–510. doi: 10.1348/1476083042555442 [DOI] [PubMed] [Google Scholar]
- Barr P, 2012. Negative self-conscious emotion and grief: An actor-partner analysis in couples bereaved by stillbirth or neonatal death. Psychology and Psychotherapy: Theory, Research, and Practice 85, 310–326. doi: 10.1111/j.2044-8341.2011.02034.x [DOI] [PubMed] [Google Scholar]
- Barr P, Cacciatore J, 2007–2008. Problematic emotions and maternal grief. OMEGA Journal of Death and Dying 56, 331–348. doi: 10.2190/OM.56.4.b [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Stillwell AM, Heatherton TF, 1994. Guilt: An interpersonal approach. Psychological Bulletin 115, 243–267. doi: 10.1037/0033-2909.115.2.243 [DOI] [PubMed] [Google Scholar]
- Boelen P, Prigerson HG, 2007. The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults. European Archives of Psychiatry and Clinical Neuroscience 257, 444–452. doi: 10.1007/s00406-007-0744-0 [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Field NG, Kovacevic A, Kaltman S, 2002. Self-enhancement as a buffer against extreme adversity: Civil war in Bosnia and traumatic loss in the United States. Personality and Social Psychology Bulletin 28, 184–196. doi: 10.1177/0146167202282005 [DOI] [Google Scholar]
- Bonanno GA, Mihalecz MC, LeJeune JT, 1999. The core emotion themes of conjugal loss. Motivation and Emotion 23, 175–201. doi: 10.1023/A:1021398730909 [DOI] [Google Scholar]
- Candea D, Szentagotai-Tata, 2018. Shame-proneness, guilt-proneness, and anxiety symptoms: A meta-analysis. Journal of Anxiety Disorders 58, 78–106. doi: 10.1016/j.janxdis.2018.07.005 [DOI] [PubMed] [Google Scholar]
- Clesse F, Leray E, Bodeau-Livinec F, Husky M, Kovess-Masfety V, 2015. Bereavement-related depression: Did the changes induced by DSM-V make a difference? Results from a large population-based survey of French residents. Journal of Affective Disorders 182, 82–90. doi: 10.1016/j.jad.2015.04.039 [DOI] [PubMed] [Google Scholar]
- Duncan C, Cacciatore J, 2015. A systematic review of the peer-reviewed literature on self-blame, guilt, and shame. OMEGA Journal of Death and Dying 71, 312–342. doi: 10.1177/0030222815572604 [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Lieberman MD, 2004. Why rejection hurts: A common neural alarm system for physical and social pain. TRENDS in Cognitive Science 8, 294–300. doi: 10.1016/j.tics.2004.05.010 [DOI] [PubMed] [Google Scholar]
- Eisma MC, Stroebe M, Schut HAW, Stroebe W, Boelen PA, van den Bout J, 2013. Avoidance processes mediate the relationship between rumination and symptoms of complicated grief and depression following loss. Journal of Abnormal Psychology 122, 961–970. doi: 10.1037/a0034051 [DOI] [PubMed] [Google Scholar]
- Fujisawa D, Miyashita M, Nakajima S, Ito M, Kato M, Kim Y, 2010. Prevalence and determinants of complicated grief in general population. Journal of Affective Disorders 127, 352–358. doi: 10.1016/j.jad.2010.06.008 [DOI] [PubMed] [Google Scholar]
- Ghatavi K, Nicolson R, MacDonald C, Osher S, Levitt A, 2002. Defining guilt in depression: A comparison of subjects with major depression, chronic medical illness, and healthy controls. Journal of Affective Disorders 60, 307–315. doi: 10.1016/S0165-0327(01)00335-4 [DOI] [PubMed] [Google Scholar]
- Gruber J, Oveis C, Keltner D, Johnson SL, 2011. A discrete emotions approach to positive emotion disturbance in depression. Cognition and Emotion 25, 40–52. doi: 10.1080/02699931003615984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, 2013. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. The Guilford Press, New York, NY. [Google Scholar]
- Kim S, Thibodeau R, Jorgensen RS, 2011. Shame, guilt and depressive symptoms: A meta-analytic review. Psychological Bulletin 137, 68–96. doi: 10.1037/a0021466 [DOI] [PubMed] [Google Scholar]
- LeBlanc NJ, Unger LD, McNally RJ, 2016. Emotional and physiological reactivity in complicated grief. Journal of Affective Disorders 194, 98–104. doi: 10.1016/j.jad.2016.01.024 [DOI] [PubMed] [Google Scholar]
- Li J, Stroebe M, Chan CLW, Chow AYM, 2014. Guilt in bereavement: A review and conceptual framework. Death Studies 38, 165–171. doi: 10.1080/07481187.2012.738770 [DOI] [PubMed] [Google Scholar]
- Li J, Tendeiro JN, Stroebe M, 2018. Guilt in bereavement: Its relationship with complicated grief and depression. The International Journal of Psychology Epub ahead of print. doi: 10.1002/ijop.12483 [DOI] [PubMed] [Google Scholar]
- Litz B, Stein N, Delaney E, Lebowtiz L, Nash WP, Silva C, Maguen S, 2009. Moral injury and moral repair in war veterans: A preliminary model and intervenion strategy. Clinical Psychology Review 29, 695–706. doi: 10.1016/j.cpr.2009.07.003 [DOI] [PubMed] [Google Scholar]
- Lundorff M, Holmgren H, Zachariae R, Farver-Vestergaard I, O’Connor M, 2017. Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. Journal of Affective Disorders 212, 138–149. doi: 10.1016/j.jad.2017.01.030 [DOI] [PubMed] [Google Scholar]
- MacDonald G, Leary MR, 2005. Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin 131, 202–223. doi: 10.1037/0033-2909.131.2.202 [DOI] [PubMed] [Google Scholar]
- McKnight PE, McKnight KM, 2013. Missing data in psychological science, In: Comer JS, Kendall PC (Eds.), The Oxford Handbook of Research Strategies for Clinical Psychology. Oxford University Press, New York, NY, pp. 374–394. [Google Scholar]
- Miles M, Demi AS, 1983–84. Toward the development of a theory of bereavement guilt: Sources of guilt in bereaved parents. Omega 14, 299–314. doi: 10.2190/F8PG-PUN4-8VW6-REWQ [DOI] [Google Scholar]
- O’Connor M, Lasgaard M, Larsen L, Johannsen M, Lundorff M, Farver-Vestergaard I, Boelen PA, 2019. Comparison of proposed diagnostic criteria for pathological grief using a sample of elderly bereaved spouses in Denmark: Perspectives on future bereavement research. Journal of Affective Disorders 251, 52–59. doi: 10.1016/j.jad.2019.01.056 [DOI] [PubMed] [Google Scholar]
- Pitman AL, Osborn DPJ, Rantell K, King MW, 2016. The stigma perceived by people bereaved by suicide and other sudden deaths: A cross-sectional UK study of 3432 bereaved adults. Journal of Psychosomatic Research 87, 22–29. doi: 10.1016/j.jpsychores.2016.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigerson HG, Maciejewski PK, Reynolds C, Bierhals AJ, Newsom JT, Fasiczka A, Frank E, Doman J, Miller M, 1995. Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research 59, 65–79. doi: 10.1016/0165-1781(95)02757-2 [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin M, Feuer CA, 2002. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology 70, 867–879. doi: 10.1037/0022-006X.70.4.867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Linehan MM, 2005. The treatment of maladaptive shame in borderline personality disorder: A pilot study of “opposite action”. Cognitive Behavioral Practice 12, 437–447. doi: 10.1016/S1077-7229(05)80071-9 [DOI] [Google Scholar]
- Robinaugh DJ, 2018. Examining cognitive impairments in bereaved adults with and without complicated grief, Psychology. Harvard University, Dissertation Abstracts International: section B: The Sciences and Engineering, Vol 78(9-B)(E). [Google Scholar]
- Robinaugh DJ, McNally RJ, 2010. Autobiographical memory for shame or guilt provoking events: Association with psychological symptoms. Behaviour Research and Therapy 48, 646–652. doi: 10.1016/j.brat.2010.03.017 [DOI] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DK, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB, 2003. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiarty 54, 573–583. doi: 10.1016/S0006-3223(03)01866-8 [DOI] [PubMed] [Google Scholar]
- Shear K, Monk T, Houck T, Melhem N, Frank E, Reynolds C, Sillowash R, 2007. An attachment-based model of complicated grief including the role of avoidance. European Archives of Psychiatry and Clinical Neuroscience 257, 453–461. doi: 10.1007/s00406-007-0745-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear K, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, Reynolds C, Lebowtiz L, Sung S, Ghesquiere A, Gorscak B, Clayton P, Ito M, Nakajima S, Konishi T, Melhem N, Meert K, Schiff M, O’Connor M, First M, Sareen J, Bolton J, Skritskaya N, Mancini A, Keshaviah A, 2011. Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety 28, 103–117. doi: 10.1002/da.20780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC, 1998. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiartic interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry 59, 22–33. [PubMed] [Google Scholar]
- Simon NM, Shear MK, Thompson EH, Zalta AK, Perlman C, Reynolds C, Frank E, Melhem N, Silowash R, 2007. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry 48, 395–399. doi: 10.1016/j.comppsych.2007.05.002 [DOI] [PubMed] [Google Scholar]
- Stroebe M, Stroebe W, van de Schoot R, Schut H, Abakoumkin G, Li J, 2014. Guilt in bereavement: The role of self-blame and regret in coping with loss. PLoS ONE 9, e966606. doi: 10.1371/journal.pone.0096606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney JP, Dearing RL, 2002. Shame and Guilt. The Guilford Press, New York. [Google Scholar]
- Tangney JP, Stuewig J, Mashek DJ, 2007. Moral Emotions and Moral Behavior. Annual Review of Psychology 58, 345–372. doi: 10.1146/annurev.psych.56.091103.070145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney JP, Wagner P, Gramzow R, 1992. Proneness to shame, proneness to guilt, and psychopathology. Journal of Abnormal Psychology 101, 469–478. doi: 10.1037/0021-843X.101.3.469 [DOI] [PubMed] [Google Scholar]
- Valentine C, Bauld L, Walter T, 2016. Bereavement following substance misuse: A disenfranchised grief. OMEGA - Journal of Death and Dying 72, 283–301. doi: 10.1177/0030222815625174 [DOI] [Google Scholar]
- Watson D, Clark LA, Carey G, 1988. Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology 97, 346–353. doi: 10.1037/0021-843X.97.3.346 [DOI] [PubMed] [Google Scholar]
- Weiss RB, Aderka IM, Lee J, Beard C, Bjorgvinsson R, 2015. A comparison of three brief depression measures in an acute psychiartic population: CES-D-10, QIDS-SR, and DASS-21-DEP. Journal of Psychopathology and Behavioral Assessment 37, 217–230. doi: 10.1007/s10862-014-9461-y [DOI] [Google Scholar]
- WHO, 2018. International classification of diseases for mortality and morbidity statistics (11th revision). World Health Organization. [Google Scholar]
- Zisook S, Martin P, Shuchter SR, Judd LL, 1997. The many faces of depression following spousal bereavement. Journal of Affective Disorders 45, 85–95. doi: 10.1016/S0165-0327(97)00062-1 [DOI] [PubMed] [Google Scholar]
- Zisook S, Shuchter SR, 1991. Depression through the first year after the death of a spouse. American Journal of Psychiatry 148, 1346–1352. doi: 10.1176/ajp.148.10.1346 [DOI] [PubMed] [Google Scholar]
- Zisook S, Shuchter SR, 1993. Major depression associated with widowhood. The American Journal of Geriatric Psychiatry 1, 316–326. doi: 10.1097/00019442-199300140-00006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


