Abstract
Objectives
To evaluate the long‐term efficacy of cannulated internal fixation in patients who sustain femoral neck fracture (FNF) and risk factors influencing the outcomes.
Methods
This retrospective study analyzed data from 73 elderly patients aged ≥60 years old, hospitalized for FNF and treated with cannulated internal fixation between August 2008 and July 2016. The inclusion criteria were: (i) patients aged ≥60 years; (ii) patients with recent femoral neck fracture, with times of injury ranging from 12–72 h; and (iii) patients who underwent Garden II–IV closed reduction and internal fixation. Patients were classified based on the Garden fracture type and Pauwels angle. Clinical data and radiographs before and after the surgery were collected. Subsequently, surgery was performed with the patient in supine position, under general or lumbar epidural anesthesia. Closed reduction was performed until satisfactory fracture reduction quality was achieved. The weight of all included patients were <75 kg, and thus, minimal internal fixation was performed. The ischemic necrosis of the femoral head was diagnosed by considering the symptoms, signs, and radiological findings. Harris hip scores were used to evaluate postoperative recovery of hip function. Furthermore, relationships between Garden fracture type and necrosis rate of the femoral head, Pauwels angle and necrosis rate of the femoral head, Garden fracture type and Harris hip score, and age and Harris hip score were analyzed.
Results
The mean duration of surgery was 1 ± 0.17 h and blood loss for all the patients was approximately 15 mL. The included patients were followed up for 13–128 months, with an average follow‐up of 61 months. Among the included 73 patients, 65 (89.0%) exhibited satisfactory union, seven (9.6%) had femoral head necrosis, and one (1.4%) had nonunion. For seven patients with femoral head necrosis, there were two, two, and three patients classified as Garden IV, Garden III, and Garden II, respectively, and two and five patients classified as Pauwels II and Pauwels III, respectively. Among the seven cases, four underwent hip replacement. Garden fracture type was not significantly associated with femoral head necrosis (χ2 = 0.44, P > 0.05) or Harris score (χ2 = 1.43, P > 0.05). Patients with Pauwels I (0%) and II (4.3%) fractures exhibited a significantly lower necrosis rate than those with Pauwels III fractures (41.7%) (P < 0.05).
Conclusions
Cannulated internal fixation was more suitable for older Chinese patients with Pauwels I/II fractures than those with Pauwels III fractures.
Keywords: Femoral neck fracture, Garden fracture type, Harris hip score, Internal fixation, Pauwels angle
Introduction
With the increasing number of aging populations globally, the incidence of hip‐related fractures have correspondingly increased1. It has been reported that the hip fracture incidence increased from 1.26 mn in the 1990s to 1.6 mn in the 2000s, and is projected to reach 4.5 to 6.3 mn by the year 20502. In the elderly population, hip fractures are associated with a higher risk of loss of independence in the activities of daily living, increased morbidity, and even mortality3. Thus, exploring the effective therapy for hip‐related factures in the elderly population will help to improve clinical outcome.
Femoral neck fracture (FNF), as one of the hip‐related fractures, accounts for >33.33% of all hip fractures4, 5. Treatment options for FNF in elderly individuals include artificial femoral head replacement, total hip arthroplasty, and internal fixation6. However, the optimal treatment strategy for FNF remains controversial. It has been proposed that replacement with the Thompson prosthesis is the best treatment for FNF in elderly cases with high FNF for the advantage of low mortality and high success rate in regaining independence7. Nevertheless, replacement with prosthesis is closely associated with complications of acetabular erosion, loosening, and late sepsis. Hip arthroplastyHip arthroplasty has been also supported as a good option for the patients with femoral neck fracture in the elderly population, especially active patients with a long life expectancy8. In recent years, focus has been centered on the comparison of the outcomes of patients with FNF by treatment with arthroplasty and internal fixation. Wang et al. reported a higher incidence of postoperative complications and disability, with avascular necrosis of the femoral head occurring in 10%–30% of FNF patients who underwent internal fixation9. The femoral head necrosis incidence decreased to 4%–15% when injuries were treated using hollow screw fixation9, 10. Recently, increased complications have been reported with prolonged duration of surgery in patients treated using artificial femoral head replacement including prosthetic loosening, rupture, dearticulation, periprosthetic fractures, postoperative hip infection, and hip pain5. Moreover, patients who undergo arthroplasty must also undergo reoperation due to the limited durability of prostheses. With the closed reduction development and minimally invasive internal fixation techniques, both the unhealed and femoral head necrosis rates have been significantly reduced11. Thus, internal fixation should be recommended to facilitate self‐healing.
The success of current fracture treatment technologies is reported to be associated with several factors. Previous research has demonstrated that bone health is clearly associated with body weight, and femoral neck strength is negatively correlated with body mass index12, 13. A survey conducted by the Alvanon Heath Company in the year 2008 among 250,000 individuals from Europe, the United States, and Asia revealed that the average body weight of the Asian population (male, 65.8 kg; female, 56.7 kg) was significantly lower than that of the American population (male, 86.6 kg; female, 70.3 kg)12. In addition to weight, patient age has also been suggested to be related to successful treatment of FNF fractures. Researchers in a previous international study suggested that the treatment for FNF favors internal fixation in patients <60 and arthroplasty in patients >80 years of age14. Therefore, internal fixation is considered to be a suitable technology for treatment of FNF patients from the East15. Although several studies have identified a relationship between different treatment methods and patient clinical data, to determine the most suitable for FNF therapy we believe that it is still necessary to update previous studies of an Asian population.
Outcome scores for surgical evaluation are generally based on generic questionnaires. The Harris hip score is a disease‐specific measure for hip arthroplasty, which was introduced in the year 196916. It is extensively used, with high validity and reliability demonstrated in several studies17. Hence, the Harris hip score was used in our study for the treatment quality assessment. In the present investigation, we summarized data collected over the past decade from elderly patients who were hospitalized for FNF and underwent closed reduction and internal fixation. Long‐term effect was determined using historical review, questionnaire survey, and clinical follow‐up. Patients were classified based on the Garden fracture type and Pauwels angle. The ischemic necrosis of the femoral head was diagnosed by overall consideration of symptoms, signs, and radiological findings. Harris hip scores were used to evaluate postoperative recovery of hip function. The purpose of this retrospective study was as follows. First, we intended to evaluate the long‐term therapeutic effect of cannulated internal fixation in Chinese elderly patients with FNF by analyzing the relationships between Garden fracture type and necrosis rate of the femoral head, Pauwels angle and necrosis rate of the femoral head, and Garden fracture type and Harris score as well as comparison of hip joint Harris scores in different age groups or in different Pauwels classification groups. Second, we aimed to investigate the risk factors influencing the outcomes of FNF patients via the univariate and multivariate logistic regression analyses of risk factors that affected the Harris hip score and necrosis rate of the femoral head. Third, based on the surgical skills that ensured successful reset and our significant results, we tried to provide more evidence to guide the clinical application of cannulated internal fixation in Chinese elderly patients with FNF.
Patients and Methods
Subjects
The inclusion criteria for enrolling patients were as follows: (i) patients aged ≥60 years, and patients with recent femoral neck fracture, with times of injury ranging from 12–72 h; (ii) patients who underwent Garden II‐IV closed reduction and internal fixation between August 2008 and July 2016; (iii) patients were followed up for 13–128 months, with an average follow‐up of 61 months; and (iv) retrospectively recruited. In contrast, the exclusion criteria were as follows: (i) patients who died (n = 10) in the follow‐up period; (ii) those with incomplete clinical data before and/or after surgery (n = 4); (iii) individuals who refused follow‐up (n = 8); and (iv) those who could not be contacted (n = 5). Except for the last criterion, all patients who met the exclusion criteria did not receive joint replacement before closed reduction and internal fixation surgery.
This retrospective study reviewed a consecutive series of 73 patients who sustained femoral neck fracture caused by low energy injury between August 2008 and July 2016. Among the 73 included patients, 16 were males and 57 were females (mean [± SD] age, 68.22 ± 7.07 years [range, 60–85 years]). All data were collected from the Traumatic Orthopedics Department of Gulou Hospital Affiliated to Medical College of Nanjing University (Nanjing, China), and all included patients (n = 73) were from Jiangsu and Anhui provinces, China. Clinical data, including patient age, gender, fracture type, reduction quality, and X‐ray before and after surgery, were collected. The study was approved by the Ethics Committee of Ruihua Hospital Affiliated to Suzhou University (Jiangsu, China).
Surgical Strategy
Surgery was performed with the patients in supine position under general or lumbar epidural anesthesia. Closed reduction was performed until satisfactory fracture reduction quality was achieved. The weight of all included patients was less than 75 kg, thus minimal internal fixation was performed.
A 2‐cm longitudinal incision was made under the greater trochanter, and then three to four guide pins were inserted in a parallel manner into the head of the femur. Following this, three or four hollow titanium screws were placed into the femoral head with different patterns according to the fracture type and degree of osteoporosis. The distance between the screw tip and cartilaginous surface of the femoral head was 0.5–1.0 cm. Subsequently, the incision was sterilized and sutured layer‐by‐layer. Finally, a successful closed reduction and internal fixation was performed on all the patients.
Postoperative Management
To prevent infection and deep venous thrombosis, patients received antibiotic injection subcutaneously 30 min pre‐ (cefuroxime) and 24 h post‐ (enoxaparin sodium) operatively. In addition, patients were carefully monitored to avoid bedsores and lung infections. After surgery, patients with osteoporosis were advised to wear T‐shaped shoes to avoid weight loading via hip side pressure, excessive adduction, and external rotation. On the second day after internal fixation, patients underwent rehabilitation training including hip flexion (<90°) and strength exercises. Passive hip flexion and extension, and active hip flexion and extension were performed 1 and 2 weeks postoperatively, respectively. Protective weight‐bearing exercise was executed when the fracture line was dim or disappeared on radiography.
Garden Classification and Pauwels Angle Classification
The Garden fracture type and Pauwels classification are the most commonly used classification systems for femoral neck fractures. Fractures were diagnosed and classified based on the Garden and Pauwels angle classification by four experienced physicians as follows: incomplete fracture was defined as Garden I; complete fracture without displacement was defined as Garden II; complete fracture with partial displacement was defined as Garden III; and complete fracture combined with displacement was defined as Garden IV. Furthermore, Pauwels categories were defined as follows: Pauwels I (Pauwels angle < 30°); Pauwels II (Pauwels angle 30° – 50°); and Pauwels III (Pauwels angle > 50°).
Ischemic Necrosis
Ischemic necrosis of the femoral head was diagnosed by overall consideration of symptoms, signs, and radiological findings. For example, increasing symptoms of pain and signs of limited hip rotation occurring 6 months after internal fixation, in combination with special imaging features including: X‐ray revealed sclerosis, cystic change(s) and crescent sign; CT scan revealed necrotic bone surrounded by low‐density band or fracture of cartilage; and/or MRI revealing low signal in T1‐weighted imaging and double line in T2‐weighted imaging.
Harris Hip Score
The Harris hip score was used to evaluate postoperative recovery of hip function in an adult population. There are four aspects in the Harris hip score system, including pain, function, absence of deformity, and range of motion with their corresponding maximum scores of 44, 47, 4, and 5 points, respectively. Finally, the scores for the four aspects were accumulated with a maximum of 100 points. A total score <70 was considered a poor score, 70–80 was fair, 80–90 was good, and 90–100 was excellent.
Statistical Analysis
All data were analyzed by the SPSS software version 21.0 (IBM Corporation, Armonk, NY, USA). The enumeration data were expressed as percentage or rate. The categorical variables were compared by chi‐square test or Fisher Exact Test. Logistic regression analysis was applied to evaluate the risk factors for the Harris hip scores (excellence rate) and necrosis rate of femoral head. An α value of 0.05 was considered to be statistically significant.
Results
Follow‐up
The patients were followed up after operation by medical history review, questionnaire survey, and outpatient follow‐up. As a result, patients were followed up for 13–128 months, with an average follow‐up of 61 months.
Operative Management and Postoperative Improvement
During operation, three or four hollow titanium screws were placed into the femoral head with different patterns according to the fracture type and degree of osteoporosis. The distance between the screw tip and cartilaginous surface of the femoral head was 0.5–1.0 cm. None of the hollow titanium screws were bent, deformed or broken, and there was no failure case.
The mean time of operation was about 1 ± 0.17 h, and the blood loss average of all the patients was approximately 15 mL. After operation, all the patients were reached to the standard reset. The postoperative symptoms were remarkably improved, and there was no complaint of obvious pain and discomfort. Among the included 73 patients, 65 (89.0%) exhibited satisfactory union, seven (9.6%) had femoral head necrosis, and one (1.4%) had nonunion.
Radiographic Improvement
All of them received standard reduction. The lateral radiogram showed that the angle between compression trabeculae and cortical bone was 155° ~ 180°.
Analysis of the Relationship between Ischemic Necrosis and Garden/Pauwels Angle Classification
Based on the Garden classification, among all the included patients, 35, 24, and 24 patients were defined as Garden II, III, and IV, respectively. Based on the Pauwels angle classification, 15 patients were classified as Pauwels I, 46 were classified as Pauwels II, and 12 as Pauwels III. For the seven patients with ischemic necrosis, there were two, two, and three patients classified as Garden IV, III, and II, respectively. Additionally, two and five patients were classified as Pauwels II and III, respectively. Among the seven cases, four underwent hip replacement. No significant relationship was found between the necrosis rate (II: 8.6%, III: 8.3%, and IV: 14.3%) and the different Garden classifications (II: n = 35, III: n = 24, and IV: n = 14) (χ2 = 0.44, P > 0.05) (Table 1). No significant relationship was found between Pauwels I/II classification (n = 61) and necrosis rate (4.3%) (χ2 = 0.67, P > 0.05). However, a higher necrosis rate (41.7%) was significantly associated with Pauwels I/III (n = 27) (χ2 = 5.58, P < 0.05) and Pauwels II/III (n = 58) (χ2 = 12.498, P < 0.05) classifications. Details of the relationship between necrosis rate of the femoral head and Pauwels classification are summarized in Table 2.
Table 1.
Relationship between necrosis rate of femoral head and Garden classification
| Garden classification | Total number (cases) | Femoral head necrosis (cases) | Necrosis rate (%) |
|---|---|---|---|
| II | 35 | 3* | 8.6 |
| III | 24 | 2† | 8.3 |
| IV | 14 | 2‡ | 14.3 |
χ2 = 0.44,P > 0.05
Among the three cases, two were found necrosis 2 years after internal fixation, one was found necrosis 1.5 – 2.0 years after internal fixation, only one case underwent arthroplasty.
Among the two cases, one was found necrosis 5 years after internal fixation, one was found necrosis 2 years after internal fixation and treated with arthroplasty.
Both the two cases were found necrosis 1.5 – 2 years, and treated with arthroplasty.
Table 2.
Relationship between necrosis rate of femoral head and Pauwel classification
| Pauwels classification | Total number (cases) | Femoral head necrosis (cases) | Necrosis rate (%) |
|---|---|---|---|
| I | 15 | 0 | 0 |
| II | 46 | 2* | 4.3 |
| III | 12 | 5* | 41.7 |
The two cases were found necrosis after 2 years and 5 years respectively. Neither of them suffered arthroplasty. Pauwels I vs. II: χ2 = 0.67, P > 0.05; Pauwels I vs. III: χ2 = 5.58, P < 0.05. Pauwels II vs. III: χ2 = 12.498, P < 0.05.
Analysis of the Relationship between the Harris Hip Score and Garden Classification/Age/Pauwels Angle Classification
Patients with Harris hip scores <70 underwent hip replacement before prosthetic replacement surgery. Two patients experienced proximal femur fracture recurrence after removal of the internal fixation components, which were replaced with proximal femoral nail internal fixation. The mean Harris hip score for the 73 patients included in the present study was 90.58 ± 8.61 and 95.58 ± 8.11 for the seven patients who were > 80 years of age. Furthermore, the Harris hip scores were 81, 80, 80, and 69, respectively, for four patients with combined ischialgia, enterorrhexis (treated with abdominal colostomy), gonarthritis, and severe coxarthritis (treated with arthroplasty). Two patients with glaucoma, cataract, and Parkinson's disease demonstrated Harris hip scores of 90. In total, five patients reported satisfactory recovery after fixation with cannulated compression screws for FNF. Three representative cases are presented in Figs 1, 2, 3. Moreover, the relationship between the Garden classification and Harris hip score is summarized in Table 3. The rates of excellent Harris score were 71.4%, 70.8%, and 64.3%, respectively, for Garden classifications II, III, and IV. However, there were no statistically significant relationships between the Garden classification and Harris score (χ2 = 1.43; P > 0.05).
Figure 1.
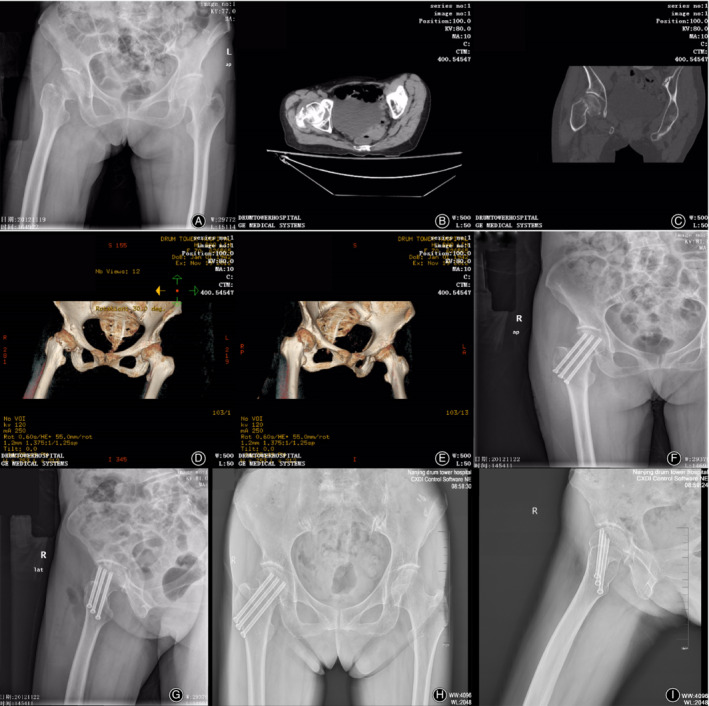
Imaging examinations of a 70‐year‐old woman with Garden III and Pauwels III type of femoral neck fracture (FNF). Preoperative radiograph (A). Postoperative computed tomography (CT) scan (B). Preoperative two‐dimensional CT reconstruction (C). Preoperative three‐dimensional CT reconstruction (D, E). Radiograph 2 days after internal fixation (F, G). Radiograph taken at the 7‐year follow‐up reveals that the bone healed well without femoral osteonecrosis, with a Harris hip score of 99 (H, I).
Figure 2.
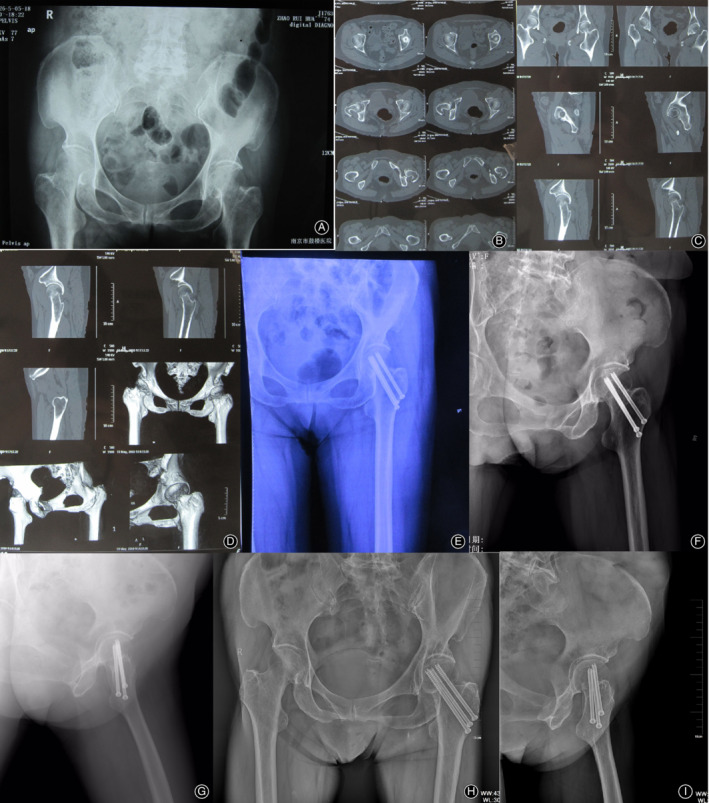
Imaging examinations of a 74‐year‐old woman with Garden III and Pauwels I type of FNF. Preoperative radiograph (A). Postoperative CT scan (B). Preoperative two‐dimensional CT reconstruction (C). Preoperative three‐dimensional CT reconstruction (D). Radiograph 2 days after internal fixation (E). Radiograph 6 months after internal fixation (F). Radiograph taken at the 7‐year follow‐up reveals that the bone healed well without femoral osteonecrosis, with a Harris hip score of 96 (G, H, I).
Figure 3.
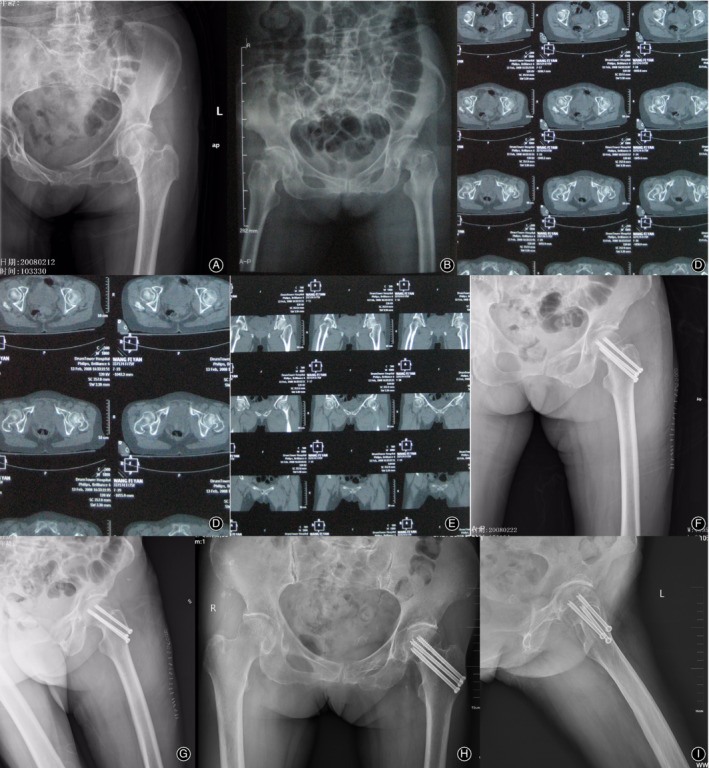
Imaging examinations of a 75‐year‐old woman with Garden III and Pauwels III type of FNF. Preoperative radiograph (A, B). Postoperative CT scan (C, D). Preoperative two‐dimensional CT reconstruction (E). P Radiograph 2 days after internal fixation (F, G). Radiograph taken at the 10‐year follow‐up reveals that the bone healed well without femoral osteonecrosis, with a Harris hip score of 90 (H, I).
Table 3.
Relationship between garden classification and Harris scores
| Garden classification | Cases (cases) | Score ≥ 90 (cases) | 80 < score < 89 (cases) | Score ≤ 79 (cases) | Rate of excellence (%) |
|---|---|---|---|---|---|
| II | 35 | 25 | 8 | 2a | 71.4 |
| III | 24 | 17 | 4 | 3b | 70.8 |
| IV | 14 | 9 | 3 | 2c | 64.3 |
χ2 = 1.43, P > 0.05
Note: a One case received intestinal colostomy which might affect the Harris scores; another was found femoral head necrosis and received joint replacement. b,c Among the 3 cases, 2 complaint of arthritis, which might affect the score; 1 has received joint replacement because of femoral head necrosis.
To clearly establish whether Harris hip score was associated with age, the patients were divided into three groups according to age. As a result, 65.1% of patients 60–69 years of age and 69.6% of patients 70–79 years of age demonstrated excellent Harris score (i.e., >90). In addition, seven patients who were > 80 years of age demonstrated excellent Harris scores. There were no significant differences in the Harris hip scores among the different age groups (χ2 = 3.48; P > 0.05). Results of this analysis are presented in Table 4.
Table 4.
Comparison of hip joint Harris scores in different age groups
| Age (years) | Cases (cases) | Score > 90 (cases) | Score < 90(cases) | Rate of excellence (%) |
|---|---|---|---|---|
| 60 ‐69 | 43 | 28 | 15 | 65.1 |
| 70 ‐79 | 23 | 16 | 7 | 69.6 |
| ≥80 | 7 | 7 | 0 | 100.0 |
χ2 = 3.48, P > 0.05.
Moreover, the relationship between the Pauwels classification and Harris score was also investigated. Among the 15 patients classified as Pauwels I, 13 (86.7%) demonstrated an excellent Harris score (>90). Excellent Harris score (>90) was demonstrated by 71.7 and 41.7% of patients classified as Pauwels II and III, respectively. Compared with Pauwels III, the Harris hip scores were significantly higher than those classified as Pauwels I (χ2 = 9.67; P < 0.05) and II (χ2 = 25.88; P < 0.05). Results of this analysis are summarized in Table 5.
Table 5.
Comparison of hip joint Harris scores in different Pauwels classification groups
| Pauwels classification | Cases | Score ≥ 90 (cases) | 80 < score ≤ 89 (cases) | Score ≤ 79 (cases) | 79 < Score ≤ 89(cases) | Rate of excellence (%) |
|---|---|---|---|---|---|---|
| I | 15 | 13 | 2a | 0 | 0 | 86.7 |
| II | 46 | 33 | 13b | 0 | 0 | 71.7 |
| III | 12 | 5 | 1 | 1 | 5c | 41.7 |
Note: aAmong the 2 cases, one received enterostomy that might affect the Pauwel score; bAmong the 13 cases, one suffered arthritis and one showed unhealed fracture, both might affect the Pauwel score; cAmong the 5 cases, one suffered coxitis that might affect the Pauwel score, and he then received arthroplasty afterwards.
Pauwels I vs. II: χ2 = 1.36, P > 0.05; Pauwels I vs. III: χ2 = 9.67, P < 0.05. Pauwels II vs. III: χ2 = 25.88, P < 0.05.
Analysis of clinical factors affecting necrosisrateof the femoral head and Harris score (excellent rate)
In order to evaluate the risk factors that affected the necrosis rate of the femoral head and Harris hip score (excellent rate), the univariate and multivariate logistic regression analyses were performed. Univariate analysis showed that the factor of Pauwels classification was an influencing factor for femoral head necrosis rate (Tables S1 and S2), and multivariate analysis indicated that the Pauwels II/III were risk factors for necrosis rate (Table S2). For the Harris hip score (excellent rate), age and the Pauwels classification were the influencing factors by univariate analysis (Table S3), and the Pauwels II/III were the risk factors (Table S4).
Complications
Seven patients experienced ischemic necrosis of the femoral head, which appeared in four at 1.5–2 years after surgery, in two at 2 years after surgery, and in one at 5 years after surgery. Four of the seven patients underwent hip replacement. Complete bone union was confirmed through X‐ray re‐examination, except for one patient in whom healing was unsatisfactory, and this patient underwent a hip replacement. The Harris hip score for these patients with hip replacement were all more than 90.
Discussion
FNFs occur frequently in the elderly population (>60 years of age), although they may occur in people of all ages. Treatment options for FNF in elderly individuals include total hip arthroplasty, artificial femoral head replacement, hemiarthroplasty, as well as internal fixation6. In the present study, we evaluated the outcomes of patients with FNF in a long follow‐up period and analyzed the factors influencing the them.
Our data showed that the patients were followed up for 13–128 months. Among the included 73 patients, 65 (89.0%) exhibited satisfactory union, seven (9.6%) had femoral head necrosis, and one (1.4%) had nonunion. The mean Harris hip score of all the patients was 90.58 ± 8.61. A previous retrospective study of 84 FNF patients treated with internal fixation suggested that two patients had nonunion and nine were present with avascular necrosis in the 46 patients at last follow‐up18. The incidence of complications in the previous study was relatively higher than our study. Thus, the internal fixation in the elderly Chinese patients was relatively safe and effective.
Clinically, surgical decision making for FNF is currently guided by such factors as patient age, fracture type, and individual conditions. As such, the treatment has poor operability with less quantitative standardization and more subjectivity19. In this study, we selected internal fixation for FNF treatment based mainly on five related factors: bone quality, body mass index, Garden classification, Pauwels type, and medical status. Patients with good bone condition, other than osteoporosis, are considered to have good bone quality. Moreover, patients with normal body mass index or lean physiques (females <65 kg or male <75 kg) are recommended to undergo internal fixation. After internal fixation, our results revealed that there were no significant differences between the Garden classification and femoral head necrosis rates. Similarly, no significant difference was found between the Garden classification and the Harris hip scores. Although the Harris hip score may be affected by the other clinical features, such as intestinal fistula(s) and arthritis, most patients in Garden II (71.4%), Garden III (70.8%), and Garden IV (64.3%) types demonstrated higher Harris hip scores. Therefore, if only the Garden classification is considered, internal fixation can be used for FNF repair. The Pauwels angle has also been suggested to be associated with hip function. Larger Pauwels angles are probably related to risk of nonunion and femoral head necrosis. Similarly, results of the present study demonstrated no significant differences between Pauwels I and/or II in femoral head necrosis, whereas the femoral head necrosis rate was significantly higher in Pauwels III patients than those with Pauwels I/ II. The Harris hip score was significantly higher in Pauwels I and II patients than that of Pauwels III patients, indicating that internal fixation is more suitable for patients classified as Pauwels I and II.
As discussed above, patient age may be the most important factor affecting surgical outcomes. However, our results suggested that the Harris hip score is significantly higher in elderly patients. This may be explained by other Harris hip score‐related diseases and less physical activity among elderly patients. Consequently, it is not necessarily advanced age that should be considered as affecting surgical outcomes, but systemic physiology20.
As the first step in the management of FNF, adequate fracture reduction is indisputable and imperative. It can protect compromised blood supply in the residual head of the femur induced by displaced fracture. Furthermore, it can also reduce the pressure on the femoral neck sac, which is necessary for regeneration of the microvasculature shaping in the bone trabeculae21, 22. Under radiographic view, the angle between the weight‐bearing medial trabeculae in the head and the medial cortex of the femoral shaft should be maintained between 170° and 180°, and this angle is defined as the Garden's angle22. If the Garden angle is <160° or > 180°, a higher occurrence rate of nonunion and femoral head necrosis was observed, respectively, in post‐reduction patients23. However, under the lateral radiograph, the dorsal and ventral trabeculae should converge into a straight line along the neck center. A lateral angle >20° is the main reason for instability. Therefore, it is recommended that internal fixation be performed by an experienced and skillful operator. In this study, the average Harris hip score was 90.58 ± 8.61 in patients who underwent internal fixation. Conversely, the score was only 82.81 ± 3.9 for patients >80 years of age with total artificial hip replacement reported in a Chinese study24. Thus, hip function recovered well in FNF patients who underwent internal fixation. More factors and individualized strategies should be considered to treat FNF.
There were limitations to this study that should be addressed, the first being the relatively small number of patients, which precluded the analysis of more categories and may have impacted accuracy. Second, the outcomes of different postoperative follow‐up times, which may have affected the outcome assessment, were not analyzed. Third, the present investigation was a single‐center study, and other internal fixation methods were not reported as a control group. More clinical data and longer follow‐up duration are required in future research.
Conclusion
Although the Harris hip score is not significantly corrected with Garden stage and patient age, it is significantly related to the Pauwels classification. Patients with Pauwels I and II fractures were more resistant to femoral head necrosis than those with Pauwels III fractures. Therefore, different fracture types should be treated with special care to achieve stable fixation and anatomical reduction in individuals who sustain FNF.
Supporting information
Table S1 The influencing factor for the femoral head necrosis rate by univariate regression analysis.
Table S2 The risk factor for femoral head necrosis rate by multivariate logistic regression analysis.
Table S3 The factors influencing Hip joint Harris scores (Rate of excellence) by univariate regression analysis.
Table S4 The risk factors for Hip joint Harris scores (Rate of excellence) by multivariate logistic regression analysis.
Acknowledgement
This work was supported by Category B Funding Program of Jiangsu Province “Summit of the Six Top Talents”(Program No. 2015‐WSW‐066) and Young Medical Talent Program in Jiangsu Province (Program No. NRC2016801).
Faxin Ju and Ruixing Hou should be regard as co‐first authors.
Disclosure: The authors declare that they have no competing interests.
Contributor Information
Fa‐xin Ju, Email: 1648764977@qq.com.
Rui‐xing Hou, Email: huarui1000@163.com.
Jun‐fei Wang, Email: wangjf1923@163.com.
References
- 1. Kannan A, Kancherla R, McMahon S, Hawdon G, Soral A, Malhotra R. Arthroplasty options in femoral‐neck fracture: answers from the national registries. Int Orthop, 2012, 36: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zielinski SM, Bouwmans CA, Heetveld MJ, et al The societal costs of femoral neck fracture patients treated with internal fixation. Osteoporos Int, 2014, 25: 875–885. [DOI] [PubMed] [Google Scholar]
- 3. Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ III. Population‐based study of survival after osteoporotic fractures. Am J Epidemiol, 1993, 137: 1001–1005. [DOI] [PubMed] [Google Scholar]
- 4. Ayeni OR, Bedi A, Lorich DG, Kelly BT. Femoral neck fracture after arthroscopic management of femoroacetabular impingement: a case report. J Bone Joint Surg Am, 2011, 93: e47–1‐8. [DOI] [PubMed] [Google Scholar]
- 5. Johansson T, Bachrach‐Lindström M, Aspenberg P, Jonsson D, Wahlström O. The total costs of a displaced femoral neck fracture: comparison of internal fixation and total hip replacement. Int Orthop, 2006, 30: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Liang C, Yang F, Lin W, et al Efficacies of surgical treatments based on Harris hip score in elderly patients with femoral neck fracture. Int J Clin Exp Med, 2015, 8: 6784. [PMC free article] [PubMed] [Google Scholar]
- 7. D'Arcy J, Devas M. Treatment of fractures of the femoral neck by replacement with the Thompson prosthesis. J Bone Joint Surg, 1976, 58: 279–286. [DOI] [PubMed] [Google Scholar]
- 8. Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J, 2016, 98: 291–297. [DOI] [PubMed] [Google Scholar]
- 9. Wang T, Sun JY, Zha GC, Jiang T, You ZJ, Yuan DJ. Analysis of risk factors for femoral head necrosis after internal fixation in femoral neck fractures. Orthopedics, 2014, 37: e1117–e1123. [DOI] [PubMed] [Google Scholar]
- 10. Lu‐Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta‐analysis of one hundred and six published reports. J Bone Joint Surg Am, 2005, 3: 29–33. [DOI] [PubMed] [Google Scholar]
- 11. Catto M. A histological study of avascular necrosis of the femoral head after transcervical fracture. J Bone Joint Surg, 1965, 47: 749–776. [PubMed] [Google Scholar]
- 12. Faje A. Body composition and skeletal health: too heavy? Too thin? Curr Osteoporos Rep, 2012, 10: 208–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim H, Lee S, Kim B, et al Association between obesity and femoral neck strength according to age, sex, and fat distribution. Osteoporos Int, 2017, 28: 2137–2146. [DOI] [PubMed] [Google Scholar]
- 14. Bhandari M, Devereaux P, Tornetta P III, et al Operative management of displaced femoral neck fractures in elderly patients: an international survey. J Bone Joint Surg Am, 2005, 87: 2122–2130. [DOI] [PubMed] [Google Scholar]
- 15. Pawar AY, O'leary PF. Combined type II odontoid fracture with Jefferson's fracture treated with temporary internal fixation. Asian Spine J, 2015, 9: 966–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Banaszkiewicz PA. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end‐result study using a new method of result evaluation In: Classic Papers in Orthopaedics. New York, NY: Springer, 2014; 13–17. [PubMed] [Google Scholar]
- 17. Söderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement?. Clin Orthop Relat Res, 2001, 384: 189–197. [DOI] [PubMed] [Google Scholar]
- 18. Nikolopoulos K, Papadakis S, Kateros K, et al Long‐term outcome of patients with avascular necrosis, after internal fixation of femoral neck fractures. Injury, 2003, 34: 525–528. [DOI] [PubMed] [Google Scholar]
- 19. Liu YJ, Xu B, Li ZY, Zhang Q, Zhang YZ. Quantitative score system for the surgical decision on adult femoral neck fractures. Orthopedics, 2012, 35: e137–e143. [DOI] [PubMed] [Google Scholar]
- 20. Xiao YP, Shu DP, Bei MJ, Ji T, Kan WS, Li SG. The clinical application of a novel method of internal fixation for femoral neck fractures—dynamic locking compression system. J Orthop Surg Res, 2018, 13: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bachiller FG, Caballer AP, Portal LF. Avascular necrosis of the femoral head after femoral neck fracture. Clin Orthop Relat Res, 2002, 399: 87–109. [DOI] [PubMed] [Google Scholar]
- 22. Schep NWL, Heintjes RJ, Martens EP, van Dortmont LMC, van Vugt AB. Retrospective analysis of factors influencing the operative result after percutaneous osteosynthesis of intracapsular femoral neck fractures. Injury, 2004, 35: 1003–1009. [DOI] [PubMed] [Google Scholar]
- 23. Barnes R, Brown JT, Garden RS, et al Subcapital fractures of the femur. A prospective review. J Bone Joint Surg Br, 1976, 58: 2–24. [DOI] [PubMed] [Google Scholar]
- 24. Zhang L, Gao J, Zhang Z, Wang XW, Zhang JZ, Sun TS. Comparison of clinical effects of total artificial hip replacement and cannulated screw fixation for the treatment of displaced femoral neck fractures in elderly patients. China J Orthop Traumatol, 2018, 31: 103–110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 The influencing factor for the femoral head necrosis rate by univariate regression analysis.
Table S2 The risk factor for femoral head necrosis rate by multivariate logistic regression analysis.
Table S3 The factors influencing Hip joint Harris scores (Rate of excellence) by univariate regression analysis.
Table S4 The risk factors for Hip joint Harris scores (Rate of excellence) by multivariate logistic regression analysis.


