Abstract
Objective
To investigate the efficacy of non‐bridging external fixation in treating distal radius fractures (DRF) and its effect on wrist joint function.
Methods
The medical records of 207 patients who were treated for DRF between May 2008 and April 2017 in our hospital (age, 18.0–70.0 years; 99 males and 108 females) were retrospectively analyzed. All patients had evident wrist trauma and the diagnosis of DRF was confirmed by imaging tests. A total of 101 patients received bridging external fixation (control group), whereas another 106 received non‐bridging external fixation (study group). At 12 weeks after the procedure, the treatment effect was measured using the Dienst scoring system (rating scale: ≤3 points, excellent; 4–7 points, good; 8–11 points, fair; >12 points, poor), and the wrist joint function was evaluated by Gartland and Werley classification (rating scale: 0–2 points, excellent; 3–8 points, good; 9–20 points, fair; >21 points, poor); meanwhile, the radial length, radial inclination, and palmar tilt were examined by X‐ray. Follow‐up visits were conducted once every 2 weeks for 6 months, and the incidences of complications in the two groups within 6 months after operation were recorded, including incision infection, Kirschner wire loosening, delayed fracture healing, and arthritis.
Results
There were no differences in the sex ratio, mean age, mean injury period, Arbeitsgemeinschaft fur osteosynthesefragen classification, and cause of fracture between the two groups (all P > 0.05). In terms of the treatment effects, the study group had a higher percentage of excellent results (P < 0.001) and lower percentages of fair and poor results (P = 0.002, P = 0.001) than the control group 12 weeks after treatment, while both groups had similar percentages of good results (P = 0.109). In terms of the score of the wrist joint function, the study group had a higher proportion of excellent result than the control group 12 weeks after treatment (P = 0.029), whereas no intergroup differences in the proportion of good, fair, and poor results were observed (all P > 0.05). After follow‐up for 6 months, the incidences of incision infection, Kirschner wire loosening, delayed fracture healing, and arthritis, as well as the total complication rate were found to be similar between the two groups (all P > 0.05).
Conclusions
Using non‐bridging external fixation for treating DRF allows some level of wrist movement during the early stage of fixation, effectively maintains the radial length, radial inclination, and palmar tilt, and achieves better outcomes than bridging external fixation.
Keywords: External fixation, Radius fracture, Treatment outcome, Wrist joint
Introduction
Distal radius fractures (DRF), also called Colles’ fractures, are a common type of acute traumatic fracture. The fracture takes place in the area distal to the proximal edge of pronator quadratus muscle, in which the spongy bone of the distal radius is displaced dorsally. DRF accounts for approximately 1/6 of all fractures and usually occurs in middle‐aged and older adults over 60 years, with a higher prevalence in women. In young adults, the fracture often results from severe trauma, with injuries to the radiocarpal and distal radioulnar joints. Due to the population aging in the world, the incidence of DRF has been rising each year1, 2. Because wrist joints, especially radiocarpal joints, are complex and highly involved in daily activities, special expertise is usually required in the management of this condition, as any inappropriate treatment can affect the functional recovery of the wrist, with huge negative impacts on patients’ quality of life3, 4.
External fixation is one of the common methods for the clinical treatment of DRF. Due to the development of external fixation, it is now possible for surgeons to achieve an anatomical reduction of the articular surface, stable fixation, and good surgical results in treating fractures5. This type of fixation can be divided into bridging external fixation and non‐bridging external fixation. Bridging joints with an external fixator is a minimally invasive approach in the management of DRF. Even though this method can help to restore the length of the radius, it cannot achieve an anatomical reduction of fracture fragments or restore the normal palmar tilt. The outcome of this technique is especially poor in unstable DRF, as the healing of the bone fragment is likely to occur in a displaced or angulated site, and incomplete healing can cause post‐traumatic osteoarthritis in patients6, 7. Since 2008, non‐bridging external fixation has become a popular technique in treating DRF. In this method, several thin pins called Kirschner wires (K‐wire, 1.8–2.0 mm) are driven into distal fracture fragments at different angles for DRF reduction. This type of insertion can offer a distributed load on a wide area along the fracture line, increase the stability of fracture fragment, and allow wrist mobility and shorter recovery. Therefore, non‐bridging external fixation displays some unique advantages in these areas.
Studies have reported that in patients with an extra‐articular fracture or non‐displaced intra‐articular fracture, non‐bridging external fixation can achieve good results in fracture reduction and maintenance of reduction during bone healing8, 9. In a study by Atroshi et al., it was documented that in non‐bridging external fixation, the average operation duration decreased by 10 min and the radial length was maintained more effectively compared with those in bridging external fixation. The study reported that the radial length on the 52nd week was markedly better in the non‐bridging external fixation group, and the average difference between the changes in the ulna and the baseline was 1.4 mm (95% confidence interval 0.1–2.7, P = 0.04). Meanwhile, there were no significant intergroup differences in the palmar tilt and radial tilt10.
No consensus has been reached regarding the efficacy of bridging external fixation versus non‐bridging external fixation in treating radius fractures. Krishnan et al. reported that the efficacies of both methods were similar in treating intra‐articular fractures of the distal radius. In their study, there were no significant differences between the two techniques in grip strength, flexion, extension range of motion, and incidence of complications on the 6th, 12th, 26th, and 52nd week after treatment. In the bridging external fixation group, there were 24 complications in 18 patients, while in the non‐bridging external fixation group, there were 20 complications in 15 patients. The main complication was pin site infection, which accounted for 32% of all complications11. Hayes et al. documented that non‐bridging external fixation could increase the risk of pin site infection, which may lead to poor fracture reduction and fracture collapse after removing the K‐wires. Moreover, extensor pollicis longus tendon rupture, a rare complication, only occurred in non‐bridging external fixation. However, compared with bridging external fixation, the palmar tilt achieved in the surgery was better maintained in non‐bridging external fixation, and reduction of the wrist joint was achieved in 84% of cases. In contrast, the bridging external fixation did not perform well in maintaining reduction, and the wrist joint alignment was restored in only 63% cases. It was found that in bridging external fixation, there were more incidences of malunions, and the risks of malunion on the dorsal side and radial shortening could increase by 6 times and 2.5 times, respectively, versus non‐bridging external fixation12.
In the present study, we retrospectively analyzed the medical records of 207 patients who either received non‐bridging external fixation or bridging external fixation for management of DRF. The purpose of the study was: (i) to investigate the clinical value of non‐bridging external fixation for treating this type of fracture; (ii) to find out whether non‐bridging external fixation can achieve good outcomes in maintaining radial length, radial inclination, and palmar tilt, as well as allow some level of wrist movement during the early stage of fixation; and (iii) to analyze the safety of non‐bridging external fixation in clinical treatment.
Patients and Methods
Patients’ Characteristics
The present study retrospectively analyzed 207 patients who were treated for DRF in our hospital from May 2008 to April 2017; among these, 101 received bridging external fixation, and 106 received non‐bridging external fixation. The study was approved by the ethics committee of the hospital and was subject to its supervision. Informed consent was obtained from all patients or their family members, and the study conformed to the provisions of the Declaration of Helsinki (as revised in Brazil in 2013).
Inclusion criteria: (i) patients who had evident wrist trauma and presented with clinical features of DRF, such as swelling joints and limited mobility, and with DRF confirmed by imaging test; (ii) patients aged between 18 and 70 years who had undergone fixation for the first time; (iii) patients with stable vital signs and without any organ dysfunction, including heart, liver, or kidney dysfunction (i.e. patients who could tolerate external fixation); (iv) patients who developed indications for the surgery; (v) patients who had complete medical records13].
Exclusion criteria: (i) patients who had severe infection in the fractured part or had systemic infection; (ii) patients who had diabetes or osteoporosis; (iii) patients who were not willing to cooperate with the treatment; (iv) patients who were transferred to another hospital or whose treatment plan changed during the middle of the treatment; (v) patients who had other severe bone or joint diseases; (vi) patients who had mental illness or learning disabilities; (vii) patients who had abnormal bleeding or abnormal coagulation function; and (viii) patients who were alcoholic or took nitroglycerin in the past.
Treatment Methods
A total of 101 patients who received bridging external fixation were assigned to a control group, while another 106 patients who received non‐bridging external fixation were assigned to a study group.
During non‐bridging external fixation, patients underwent either brachial plexus anesthesia or general anesthesia, followed by thorough debridement. The K‐wire leverage was performed for the fracture reduction guided by a C‐arm X‐ray machine, and a continuous traction was applied to main the stability at the broken end. Two screws were implanted into the proximal radial side at the second metacarpal bone and the lower third of the radius, respectively, followed by installation of a carbon fiber external fixator. When an anatomical or nearly anatomical reduction was achieved, the screws of the fixator were tightened and fixed. The second layer of the carbon fiber rods was fixed in a Y‐shaped manner and one carbon rod was placed parallel to the fracture line. The rod was placed at a sharp angle extending to the styloid process of the radius and the radioulnar part of the distal fracture fragment. K‐wires (1.8 mm or 2.0 mm) were inserted into the distal fracture fragment through a small insertion. Two K‐wires were implanted into the styloid process part, one K‐wire was implanted into the dorsoulnar part, and another K‐wire was placed perpendicular to the articular surface. The K‐wires were placed in a semi‐circular shape from the dorsal horn of the radioulnar to the styloid process of the radius. The K‐wire going through the styloid process was bent before fixation. At least two K‐wires were placed in each fracture fragment, forming a stable fixation. The external fixation part bridging the radiocarpal joint was then removed, and the wrist was moved to check the stability at the fracture site.
During bridging external fixation, patients underwent either brachial plexus anesthesia or general anesthesia, followed by thorough debridement. The K‐wire leverage was performed for the fracture reduction guided by a C‐arm X‐ray machine, and continuous traction was applied to maintain the stability at the broken end. At the dorsolateral side of the second metacarpal bone, 1 cm away from the two ends of the metacarpal bone, two 1‐cm vertical incisions were made. After separating the tendon of the extensor digitorum, holes were drilled at a 30° angle to the metacarpal's frontal plane and perpendicular to the metacarpal vertical axis. Two Schanz screws were implanted into the metacarpal bone, and the rod connecting the main body and two simple adjustable clamps were installed in the two Schanz screws. In accordance with the location of the connecting rod at the proximal fracture site after a good reduction, two Schanz screws were inserted into the proximal side of the radial fracture, which was approximately 2–13 cm away from the fracture site. After the reduction was confirmed, the adjustable clamps and the rod connecting the main body were tightened and fixed.
Outcome Measures
Dienst Scoring System
Treatment effects 12 weeks after surgery were evaluated in the two groups using the Dienst scoring system. Items analyzed in this scoring system include pain level, range of motion, wrist joint function, grip strength, palmar flexion, and dorsal extension, and the score of each item was from 0 to 3 points. The rating scale of the total score was as follows: ≤3 points, excellent; 4–7 points, good; 8–11 points, fair; >12 points, poor.
Wrist Joint Function
Gartland and Werley classification was used to assess the function of the wrist joint after 12 weeks. Items analyzed in this scoring system include joint deformity, chief complaint of pain, joint range of motion, complications, arthritic change, nerve complications, and finger function14. The rating scale was as follows: 0–2 points, excellent; 3–8 points, good; 9–20 points, fair; >21 points, poor. See Table 1.
Table 1.
Gartland and Werley classification
| Items | Point |
|---|---|
| Residual deformity (0–3 points) | |
| Prominent ulnar styloid | 1 |
| Palmar tilt deformity | 2 |
| Radial deviation deformity | 2 or 3 |
| Subjective evaluation (0–6 points) | |
| Excellent: no pain, disability, or limitation of motion | 0 |
| Good: occasional pain, some limitation of motion, and weakness of wrist | 2 |
| Fair: pain, limitation of motion | 4 |
| Poor: pain, activities markedly restricted | 6 |
| Objective evaluation (0–5 points) | |
| Loss of extension (<45°) | 5 |
| Loss of ulnar deviation (<15°) | 3 |
| Loss of supination (<50°) | 2 |
| Loss of flexion (<30°) | 1 |
| Loss of radial deviation (<15°) | 1 |
| Loss of circumduction | 1 |
| Pain in distal radioulnar joint | 1 |
| Grip strength: 60% or less than on the opposite side | 1 |
| Loss of pronation | 2 |
| Complications (0–5 points) | |
| Arthritic change | |
| Minimum | 1 |
| Minimum with pain | 3 |
| Moderate | 2 |
| Moderate with pain | 4 |
| Severe | 3 |
| Severe with pain | 5 |
| Nerve complications (median nerve) | 1 or 3 |
| Poor finger function due to cast | 1 or 2 |
| Final results | |
| Excellent | 0–2 |
| Good | 3–8 |
| Fair | 9–20 |
| Poor | ≥21 |
Reduction of the Distal Radius
Twelve weeks after treatment, all patients received an X‐ray examination to assess the outcome of the fracture reduction. Based on the results of the X‐ray film, patients’ radial length, radial inclination, and palmar tilt were examined. During the measurement of the radial length, two parallel lines perpendicular to the longitudinal axis of radius were drawn on the X‐ray film; one of the lines passed through the tip of the styloid process, and another passed through the ulnar horn of the lunar bone absconsio. The radial length was measured as the distance between these two lines. Radial inclination was assessed as the angle between the line drawn perpendicular to the longitudinal axis of the radius and the line connecting the most distal points of ulnar and radial sides of the distal radius. Palmar tilt was measured as the angle between the line connecting the most distal points of volar and dorsal lips of the distal radius and another line drawn perpendicular to the longitudinal axis of the radius.
Complications
Follow‐up visits were conducted once every 2 weeks for 6 months. Incidences of complications within 6 months after operation were recorded in the two groups, including incision infection, K‐wire loosening, delayed fracture healing, and arthritis.
Statistical Analysis
Statistical software SPSS 19.0 was applied for the data analysis. The count data are expressed as number and percentage (n, %), and the comparison of rate was performed by χ2‐test; the measurement data are presented as mean ± standard deviation, and the comparison between two groups was performed by t‐test. A value of P < 0.05 was considered statistically significant.
Results
No Intergroup Differences Were Observed in Patients’ Characteristics
There were 101 patients in the control group (48 men and 53 women, 58.3 ± 5.1 years) and 106 patients in the study group (51 men and 55 women, 58.1 ± 5.2 years). No intergroup differences were found in sex ratio, mean age, mean injury period, AO classification, and cause of fracture (all P > 0.05, Table 2).
Table 2.
Patients’ characteristics
| Items | Control group (n = 101) | Study group (n = 106) | χ2/t‐value | P‐value |
|---|---|---|---|---|
| Sex (n, %) | 0.007 | 0.932 | ||
| Male | 48 (47.52) | 51 (48.11) | ||
| Female | 53 (52.48) | 55 (51.89) | ||
| Age (years, mean ± SD) | 58.3 ± 5.1 | 58.1 ± 5.2 | 0.279 | 0.780 |
| Injury period (h, mean ± SD) | 5.24 ± 3.17 | 4.58 ± 3.41 | 0.195 | 0.845 |
| AO classification (n, %) | 0.029 | 0.986 | ||
| A | 20 (19.80) | 20 (18.87) | ||
| B | 49 (48.51) | 52 (49.06) | ||
| C | 32 (31.68) | 34 (32.08) | ||
| Cause of fracture (n, %) | 0.877 | 0.831 | ||
| Traffic accident | 8 (7.92) | 10 (9.43) | ||
| Sports | 5 (4.95) | 8 (7.55) | ||
| Fall over | 82 (81.19) | 81 (76.42) | ||
| Fall from height | 6 (5.94) | 7 (6.60) |
AO, Arbeitsgemeinschaft für Osteosynthesefragen.
Better Results Were Achieved in the Study Group as Assessed by Dienst and Gartland–Werley Scoring Systems
Treatment effects in the two groups were evaluated using the Dienst scoring system. It was found that 12 weeks after treatment, the percentage of excellent results in the study group was higher than that in the control group (χ2 = 28.991, P < 0.001), whereas the percentage of fair results in the study group was lower (χ2 = 9.418, P = 0.002). No difference was found in the ratio of the fair results between the two groups (χ2 = 2.565, P = 0.109), and the study group had a lower percentage of poor results than the control group (χ2 = 11.616, P = 0.001). Wrist joint function in the two groups was also assessed after treatment using the Gartland and Werley scoring system. The results showed that 12 weeks after treatment, the percentage of patients who achieved excellent results in the study group was higher than that in the control group (χ2 = 4.739, P = 0.029). Meanwhile, no differences were observed in the percentage of good, fair, and poor results between the two groups (all P > 0.05). See Table 3.
Table 3.
Treatment effects and wrist joint function in the two groups (n, %)
| Score level | Control group (n = 101) | Study group (n = 106) | χ2‐value | P‐value |
|---|---|---|---|---|
| Dienst | ||||
| Excellent | 41 (40.59) | 82 (77.36) | 28.991 | <0.001 |
| Good | 23 (22.77) | 15 (14.15) | 2.565 | 0.109 |
| Fair | 20 (19.80) | 6 (5.66) | 9.418 | 0.002 |
| Poor | 17 (16.83) | 3 (2.83) | 11.616 | 0.001 |
| Gartland and Werley | ||||
| Excellent | 40 (39.60) | 58 (54.72) | 4.739 | 0.029 |
| Good | 44 (43.56) | 39 (36.79) | 0.987 | 0.320 |
| Fair | 10 (9.90) | 6 (5.66) | 1.304 | 0.253 |
| Poor | 7 (6.93) | 3 (2.83) | 2.018 | 0.155 |
Study Group Had Lower Magnitude of Decreases in Radial Length, Radial Inclination, and Palmar Tilt
Before treatment, there were no intergroup differences for radial length, radial inclination, and palmar tilt (all P > 0.05). However, 12 weeks after treatment, both groups experienced some level of decrease in these three indices, while the magnitude of decreases in the control group were greater (all P < 0.05). See Table 4 and Figs 1, 2, 3, 4, 5.
Table 4.
X‐ray results in the two groups (mean ± SD)
| Items | Control group (n = 101) | Study group (n = 106) | t‐value | P‐value |
|---|---|---|---|---|
| Radial length (mm) | ||||
| Before treatment | 8.37 ± 1.04 | 8.12 ± 1.01 | 1.754 | 0.081 |
| After treatment | 5.62 ± 1.33* | 6.87 ± 1.14* | 7.271 | <0.001 |
| Radial inclination (°) | ||||
| Before treatment | 18.02 ± 1.33 | 17.83 ± 1.25 | 1.060 | 0.291 |
| After treatment | 14.39 ± 2.12* | 15.73 ± 1.42* | 5.366 | <0.001 |
| Palmar tilt (°) | ||||
| Before treatment | 12.86 ± 1.13 | 13.11 ± 1.12 | 1.598 | 0.112 |
| After treatment | 8.33 ± 2.02* | 11.58 ± 1.59* | 12.895 | <0.001 |
P < 0.05 vs the same group before treatment.
Figure 1.
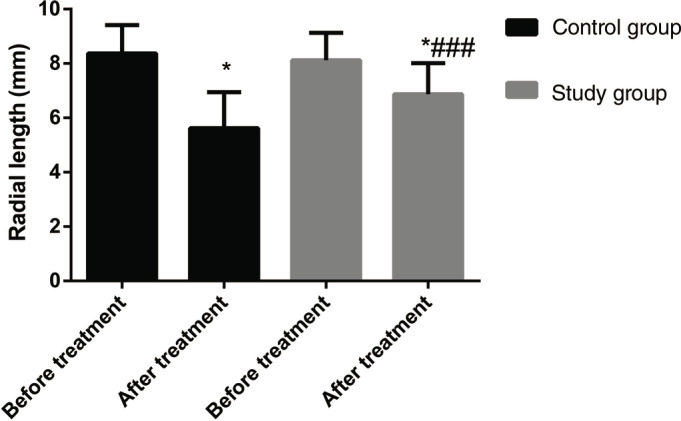
Radial length in the two groups before and after treatment. Before treatment, there were no intergroup differences; after treatment, both groups experienced some level of decrease, while the magnitude of decreases in the control group were greater. *P < 0.05 vs the same group before treatment. ### P < 0.05 vs the control group during the same period of time.
Figure 2.
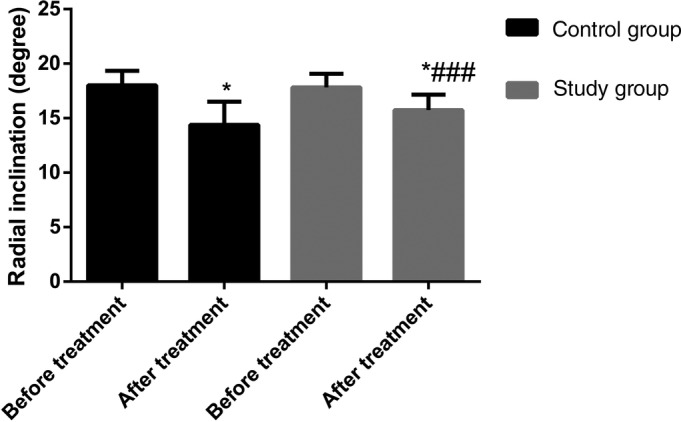
Radial inclination in the two groups before and after treatment. Before treatment, there were no intergroup differences; after treatment, both groups experienced some level of decrease, while the magnitude of decreases in the control group were greater. *P < 0.05 vs the same group before treatment. ### P < 0.05 vs the control group during the same period of time.
Figure 3.
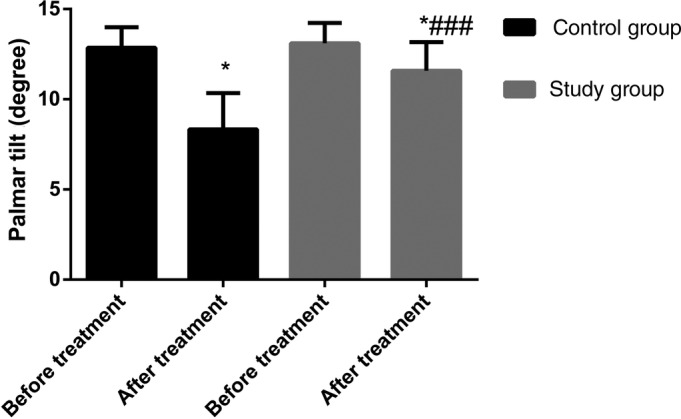
Palmar tilt in the two groups before and after treatment. Before treatment, there were no intergroup differences; after treatment, both groups experienced some level of decreases, while the magnitude of decreases in the control group were greater. *P < 0.05 vs the same group before treatment. ### P < 0.05 vs the control group during the same period of time.
Figure 4.
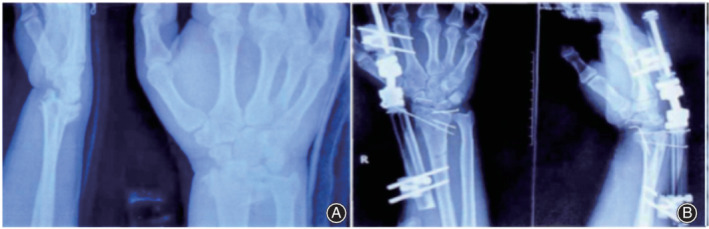
Distal radius fracture treated by non‐bridging external fixation. (A) Lateral view of the radius on X‐ray before operation. (B) Lateral view of the radius on X‐ray 1 day after operation.
Figure 5.

Distal radius fracture treated by bridging external fixation. (A) Lateral view of the radius on X‐ray before operation. (B) Lateral view of the radius on X‐ray 1 day after operation.
No Intergroup Differences Were Observed in Postoperative Complications
The results of the 6‐month follow up showed no intergroup differences in the incidences of incision infection, K‐wire loosening, delayed fracture healing, and arthritis, as well as the total complication rate (all P > 0.05, Table 5).
Table 5.
Postoperative complication (n, %)
| Complications | Control group (n = 101) | Study group (n = 106) | χ2‐value | P‐value |
|---|---|---|---|---|
| Incision infection | 7 (6.93) | 8 (7.55) | 0.029 | 0.864 |
| K‐wire loosening | 0 | 1 (0.94) | 0.948 | 0.330 |
| Delayed fracture healing | 2 (1.98) | 7 (6.6) | 2.659 | 0.103 |
| Arthritis | 2 (1.98) | 4 (3.77) | 0.591 | 0.768 |
| Total | 11 (10.89) | 20 (18.87) | 2.585 | 0.108 |
K‐wire, Kirschner wire.
Discussion
Various approaches to treating DRF have been reported in the literature, such as the combined use of plaster cast and steel pin fixation, percutaneous K‐wire fixation, and open reduction and internal fixation. However, because the local stability in DRF is poor, requirements for reduction are strict, and the distal radius is always pressed by forearm muscle, determining how to maximally restore and maintain radial length and how to minimize unevenness between dorsal angulation and the articular surface have become unresolved issues in the treatment of this disease15, 16, 17, 18. Because non‐bridging external fixation has been applied in our hospital and we have achieved good results, the efficacy of this technique was explored in this study, to obtain useful information for the clinical management of DRF.
Treatment Effects
We used the Dienst scoring system to assess the treatment effects in the two groups. The Dienst system is commonly used for evaluating the effectiveness of DRF reduction, which also includes both subjective and objective assessments of patients’ wrist joint function. The Dienst score is an outcome measure that can comprehensively evaluate the treatment effects19. The results of our study showed that non‐bridging external fixation achieved better effects than bridging external fixation in the management of DRF, and, moreover, this method obtained a higher percentage of excellent results than bridging external fixation. During the bridging external fixation on a wrist, the traction force applied should be moderate, as any excessive traction can negatively affect the ligament function. It has been documented that the negative impact exerted by non‐bridging external fixation on ligament function and connectivity is smaller than by bridging external fixation, which might help to explain why non‐bridging external fixation can achieve better efficacy20, 21. Besides, in bridging external fixation, the traction force applied is relatively big, and an extended immobilization period is required. However, a prolonged immobilization period and excessive traction can lead to persistent limitation of wrist movement22, which might be another reason why non‐bridging external fixation can achieve a better result. Zhang et al. established a visual modeling of DRF, and their finite‐element analysis included stress distribution, transmission, and displacement under the influence of contraction, extension, intorsion, and extorsion torque. The results showed that non‐bridging external fixation can offer suitable stress distribution near the fracture line, and the cradle can have a stress shielding effect on the radius23.
Wrist Joint Function and Reduction of Distal Radius
Non‐bridging external fixation has been proposed as a therapy for treating DRF that combines both closed reduction and postoperative functional exercise. It works directly on the broken end of a fractured bone, which is conducive to reduction. However, most researchers have suggested that this technique can only be applied when the width of the fracture fragment in the distal radius is long enough to hold two fixation pins and the fragment is not displaced24, 25. In the present study, patients in the study group received implantation of multiple K‐wires in the distal radius fragment using a non‐bridging hybrid external fixation technique for fracture reduction and reduction maintaining. This method is suitable for distal radius reduction and allows wrist mobility.
Regarding wrist joint function, the results evaluated by Gartland and Werley classification in our study showed that patients who received non‐bridging external fixation had better wrist joint function than those who received bridging external fixation. The Gartland and Werley classification has been proved to have good reliability and has been widely used by scholars for assessing wrist joint function in patients with fractures26, 27 . Moreover, our study showed that before treatment, there were no intergroup differences in radial length, radial inclination, and palmar tilt, whereas, at 6 weeks after treatment, the values of these three indices were higher in patients who underwent non‐bridging external fixation than in patients who received bridging external fixation. These findings have demonstrated that non‐bridging external fixation can cause less loss of radial length, radial inclination, and palmar tilt, and, thus, explain why this method can achieve better reduction in patients. Less loss of radial length, radial inclination, and palmar tilt is essential for maintaining patients’ wrist joint function because too small a radial inclination and palmar tilt can bring limitations to wrist flexion and other functions28, 29. Gradl et al. report that compared with the steel plate fixation, non‐bridging external fixation can achieve better recovery of palmar tilt30. A meta‐analysis also demonstrated that non‐bridging external fixation can bring a better range of motion in extension, pronation, and supination, as well as better maintain the radial length31.
Incidence of Complications
One systematic review and meta‐analysis has found that this technique has higher incidences of pin‐tract affection and nerve injury than bridging external fixation in treating DRF32. No intergroup differences were observed in the incidence of complications in this study, which may be due to the high quality postoperative nursing care in our hospital. More studies will be carried out in the future and we hope this study may inspire more scholars to study the application of non‐bridging external fixation in the treatment of DRF.
Conclusion
Non‐bridging external fixation, which can lead to better outcomes than bridging external fixation, is a good approach for treating DRF. The method can allow some level of wrist movement during the early stage of fixation, and can effectively maintain radial length, radial inclination, and palmar tilt.
Disclosure: The authors declare no conflict of interest.
References
- 1. Padegimas EM, Ilyas AM. Distal radius fractures: emergency department evaluation and management. Orthop Clin North Am, 2015, 46: 259–270. [DOI] [PubMed] [Google Scholar]
- 2. Mellstrand Navarro C, Ahrengart L, Tornqvist H, Ponzer S. Volar locking plate or external fixation with optional addition of K‐wires for dorsally displaced distal radius fractures: a randomized controlled study. J Orthop Trauma, 2016, 30: 217–224. [DOI] [PubMed] [Google Scholar]
- 3. Roh YH, Lee BK, Baek JR, Noh JH, Gong HS, Baek GH. A randomized comparison of volar plate and external fixation for intra‐articular distal radius fractures. J Hand Surg Am, 2015, 40: 34–41. [DOI] [PubMed] [Google Scholar]
- 4. Brogren E, Petranek M, Atroshi I. Cast‐treated distal radius fractures: a prospective cohort study of radiological outcomes and their association with impaired calcaneal bone mineral density. Arch Orthop Trauma Surg, 2015, 135: 927–933. [DOI] [PubMed] [Google Scholar]
- 5. Duncan SFM, Flowers CW. Distal radius fracture: external fixation In: Duncan SFM, Flowers CW, eds. Therapy of the Hand and Upper Extremity: Rehabilitation Protocols. Cham: Springer International Publishing, 2015; 125–126. [Google Scholar]
- 6. Lavini F, Dall'Oca C, Mezzari S, et al Temporary bridging external fixation in distal tibial fracture. Injury, 2014, 45: S58–S63. [DOI] [PubMed] [Google Scholar]
- 7. Ryu SM, Park JW, Moon JJ, Lim SW, Kwon MS, Shon OJ. Computed tomography of bicondylar tibial plateau fractures after distraction with a bridging external fixation. Int Orthop, 2018, 42: 2451–2458. [DOI] [PubMed] [Google Scholar]
- 8. Atalar AC, Erşen A. External fixation for upper extremity trauma In: Çakmak M, Şen C, Eralp L, Balci HI, Civan M, eds. Basic Techniques for Extremity Reconstruction: External Fixator Applications According to Ilizarov Principles. Cham: Springer International Publishing, 2018; 167–176. [Google Scholar]
- 9. Li‐hai Z, Ya‐nan W, Zhi M, et al Volar locking plate versus external fixation for the treatment of unstable distal radial fractures: a meta‐analysis of randomized controlled trials. J Surg Res, 2015, 193: 324–333. [DOI] [PubMed] [Google Scholar]
- 10. Atroshi I, Brogren E, Larsson GU, Kloow J, Hofer M, Berggren AM. Wrist‐bridging versus non‐bridging external fixation for displaced distal radius fractures: a randomized assessor‐blind clinical trial of 38 patients followed for 1 year. Acta Orthop, 2006, 77: 445–453. [DOI] [PubMed] [Google Scholar]
- 11. Krishnan J, Wigg AE, Walker RW, Slavotinek J. Intra‐articular fractures of the distal radius: a prospective randomised controlled trial comparing static bridging and dynamic non‐bridging external fixation. J Hand Surg Br, 2003, 28: 417–421. [DOI] [PubMed] [Google Scholar]
- 12. Hayes AJ, Duffy PJ, McQueen MM. Bridging and non‐bridging external fixation in the treatment of unstable fractures of the distal radius: a retrospective study of 588 patients. Acta Orthop, 2008, 79: 540–547. [DOI] [PubMed] [Google Scholar]
- 13. Johnson NA, Cutler L, Dias JJ, Ullah AS, Wildin CJ, Bhowal B. Complications after volar locking plate fixation of distal radius fractures. Injury, 2014, 45: 528–533. [DOI] [PubMed] [Google Scholar]
- 14. Gartland JJ Jr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am, 1951, 33: 895–907. [PubMed] [Google Scholar]
- 15. Liang JQ, Chen C, Zhao H. Revision surgery after percutaneous endoscopic transforaminal discectomy compared with primary open surgery for symptomatic lumbar degenerative disease. Orthop Surg, 2019, 11: 620–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Waljee JF, Ladd A, MacDermid JC, Rozental TD, Wolfe SW. A unified approach to outcomes assessment for distal radius fractures. J Hand Surg Am, 2016, 41: 565–573. [DOI] [PubMed] [Google Scholar]
- 17. Bartl C, Stengel D, Bruckner T, Gebhard F. The treatment of displaced intra‐articular distal radius fractures in elderly patients. Dtsch Arztebl Int, 2014, 111: 779–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Williksen JH, Husby T, Hellund JC, Kvernmo HD, Rosales C, Frihagen F. External fixation and adjuvant pins versus volar locking plate fixation in unstable distal radius fractures: a randomized, controlled study with a 5‐year follow‐up. J Hand Surg Am, 2015, 40: 1333–1340. [DOI] [PubMed] [Google Scholar]
- 19. Yin SQ, Huang YP, Li MZ, Pan JD, Ding WQ, Wang X. Relationship between radiographic parameters and clinical outcomes of elderly patients with distal radius fractures. Zhongguo Gu Shang, 2018, 31: 141–144. [DOI] [PubMed] [Google Scholar]
- 20. Kanar M, Armagan R, Oc Y, Sezer H, Eren O. Treatment unstable distal radius fractures with nonbridginig external fixation. Med Bull Sisli Hosp, 2017, 51: 96–101. [Google Scholar]
- 21. Andruszkow H, Pfeifer R, Horst K, Hildebrand F, Pape HC. External fixation in the elderly. Injury, 2015, 46: S7–S12. [DOI] [PubMed] [Google Scholar]
- 22. Lee RK, Griffith JF, Tang WK, Ng AW, Yeung DK. Effect of traction on wrist joint space and cartilage visibility with and without MR arthrography. Br J Radiol, 2017, 90: 20160932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang W, Ju CJ, Hu YL, Yang N, Han YL, Wang F. Three‐dimensional finite element stress analysison non‐bridge external fixation to distal radius fracture. Int J Clin Exp Med, 2018, 11: 10910–10916. [Google Scholar]
- 24. Abdel‐Ghany M, Tohamy TG, Shaaban WM, Atallah AHA, Abdel‐Rahman TM. Ligamentotaxis versus open reduction and internal fixation for distal radius intra‐articular fractures. Open J Orthop, 2017, 7: 21–31. [Google Scholar]
- 25. Jacob N, Amin A, Giotakis N, Narayan B, Nayagam S, Trompeter AJ. Management of high‐energy tibial pilon fractures. Trategies Trauma Limb Reconstr, 2015, 10: 137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jia XF, Cai HX, Lin GS, et al Clinical observation on the effect of joint mobilization in treating elderly patients after distal radius fractures operation. Zhongguo Gu Shang, 2017, 30: 643–646. [DOI] [PubMed] [Google Scholar]
- 27. Chen N, Wang HR, Zhou KH, Pan FG. Dorsal dual‐plate fixation for unstable distal radius fractures. Zhonghua Chuang Shang, 2014, 30: 324–327. [Google Scholar]
- 28. Jackowski SA, Baxter‐Jones AD, Gruodyte‐Raciene R, Kontulainen SA, Erlandson MC. A longitudinal study of bone area, content, density, and strength development at the radius and tibia in children 4‐12 years of age exposed to recreational gymnastics. Osteoporos Int, 2015, 26: 1677–1690. [DOI] [PubMed] [Google Scholar]
- 29. Sagerman SD, Zogby RG, Palmer AK, Werner FW, Fortino MD. Relative articular inclination of the distal radioulnar joint: a radiographic study. J Hand Surg Am, 1995, 20: 597–601. [DOI] [PubMed] [Google Scholar]
- 30. Gradl G, Gradl G, Wendt M, Mittlmeier T, Kundt G, Jupiter JB. Non‐bridging external fixation employing multiplanar K‐wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch Orthop Trauma Surg, 2013, 133: 595–602. [DOI] [PubMed] [Google Scholar]
- 31. Cui Z, Yu B, Hu Y, Lin Q, Wang B. Dynamic versus static external fixation for unstable distal radius fractures: an up‐to‐date meta‐analysis. Injury, 2012, 43: 1006–1013. [DOI] [PubMed] [Google Scholar]
- 32. Gu WL, Wang J, Li DQ, et al Bridging external fixation versus non‐bridging external fixation for unstable distal radius fractures: a systematic review and meta‐analysis. J Orthop Sci, 2016, 21: 24–31. [DOI] [PubMed] [Google Scholar]


