Abstract
Background:
Surgical specialties face unique challenges caused by SARS-COV-2 (COVID-19). These disruptions will call on clinicians to have greater consideration for non-operative treatment options to help manage patient symptoms and provide therapeutic care in lieu of the traditional surgical management course of action. This study aimed to summarize the current guidance on elective surgery during the COVID-19 pandemic, assess how this guidance may impact orthopaedic care, and review any recommendations for non-operative management in light of elective surgery disruptions.
Methods:
A systematic search was conducted, and included guidance were categorized as either “Selective Postponement” or “Complete Postponement” of elective surgery. Selective postponement was considered as guidance that suggested elective cases should be evaluated on a case-by-case basis, whereas complete postponement suggested that all elective procedures be postponed until after the pandemic, with no case-by-case consideration. In addition, any statements regarding conservative/non-operative management were summarized when provided by included reports.
Results:
A total of 11 reports from nine different health organizations were included in this review. There were seven (63.6%) guidance reports that suggested a complete postponement of non-elective surgical procedures, whereas four (36.4%) reports suggested the use of selective postponement of these procedures. The guidance trends shifted from selective to complete elective surgery postponement occurred throughout the month of March. The general guidance provided by these reports was to have an increased consideration for non-operative treatment options whenever possible and safe. As elective surgery begins to re-open, non-operative management will play a key role in managing the surgical backlog caused by the elective surgery shutdown.
Conclusion:
Global guidance from major medical associations are in agreement that elective surgical procedures require postponement in order to minimize the risk of COVID-19 spread, as well as increase available hospital resources for managing the influx of COVID-19 patients. It is imperative that clinicians and patients consider non-operative, conservative treatment options in order to manage conditions and symptoms until surgical management options become available again, and to manage the increased surgical waitlists caused by the elective surgery shutdowns.
Keywords: COVID-19, nonoperative treatment, pandemic, surgery
Background
The COVID-19 pandemic has had a major impact on healthcare systems globally. The COVID-19 spread has resulted up to now in over nearly 3 million cases and over 200,000 deaths, which has tested the capacity and resources of global healthcare systems, as this influx of cases occurred in a rapid and unexpected timeframe.1 To combat this, many forms of guidance have been provided to assist in risk mitigation of viral spread, potential therapy options to treat COVID-19 patients, and reorganization strategies for hospital departments to help manage the increased patient load.2,3 Surgical specialties face unique challenges caused by COVID-19.4 For many urgent surgical procedures, additional steps are required to protect both patients and healthcare workers from the virus.5–7
Non-urgent and elective surgical procedures have seen a disruption due to the COVID-19 pandemic as well.8,9 Personal experiences of surgical departments have summarized how they have managed elective surgery procedures during the COVID-19 pandemic, and guidance in the published literature has highlighted the importance of minimizing resource utilization for elective surgeries in order to provide greater support for COVID-19 patient management.8,10–13 Due to increases in resource needs within urgent and critical care patients, the certainty around scheduled elective procedures may be limited for both surgeons and patients.9
Disruptions to non-essential surgery may have left patients waiting for a rescheduled procedure, with no clarity on when elective surgical practices will return to normal.14 Within orthopaedics, previous research has demonstrated that postponing major elective surgery, such as total joint arthroplasty or surgical non-union management, causes a considerable decrease in a patients’ quality of life.15–18 A significant deterioration of patient quality of life may occur over the course of their pre-operative waiting period.16,17 Globally, a vast number of patients are at risk of suffering major quality of life deterioration as a result of their elective surgery being postponed or cancelled.
These disruptions will call on clinicians to have greater consideration for conservative non-surgical treatment options to help manage patient symptoms and provide therapeutic care in lieu of the original surgical management course of action. This study aimed to summarize the current guidance on elective surgery during the COVID-19 pandemic, assess how this guidance may impact orthopaedic care, and review any recommendations for non-operative management in light of elective surgery disruptions.
Methods
Systematic search
This review followed PRISMA guidance on systematic review reporting.19 A systematic search was conducted in order to identify current elective surgery guidance globally as a result of the COVID-19 pandemic within MEDLINE, EMBASE, Global Health and Emcare from the databases from inception until 6 April 2020 (Appendix A).20 The search was repeated on 19 April 2020, but no additional articles were eligible. A hand search using Google and reference lists of relevant publications was conducted to identify any additional publications or grey literature that may be relevant for inclusion. In addition, all articles with a surgical focus were screened from a recently conducted scoping review on COVID-19 literature.21 Reports were included if they provided health association recommendations or position statements regarding non-urgent/elective surgery in the COVID-19 pandemic. Reports were excluded if they were personal opinion, secondary guidance in reference to a primary guidance document, or reviews of guidance given by health associations. One of the included reports also provided a comprehensive overview of guidance for the eventual phased re-introduction of elective surgery, which is summarized in this review as well.20
Data extraction and analysis
Pertinent data regarding the date of publication, country, elective surgery recommendations, and information about conservative management guidance were extracted from each of the included reports. Recommendations were summarized and plotted over time to identify the cumulative number of reports providing elective surgery guidance. These reports were categorized as either “Selective Postponement” or “Complete Postponement” of elective surgery. Selective postponement was considered for guidance that suggested elective cases should be evaluated and possibly postponed if needed. Complete postponement was considered when guidance suggested that all elective procedures be postponed until after the pandemic. In addition, any statements regarding conservative/non-operative management were summarized when provided by included reports.
Results
Report selection
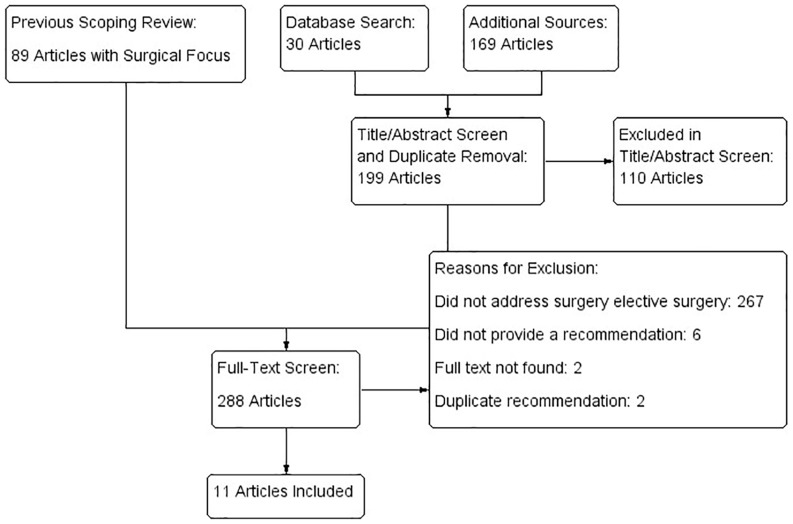
A total of 240 reports were identified for potential inclusion. The systematic literature search identified 30 articles, whereas an additional 169 articles were identified through additional searches of association websites and reference lists. The previously conducted scoping review identified 90 articles with a surgical focus. After article screening, a total of 11 reports from nine different medical associations were included in this review.14,22–31 A summary of the screening process is included in Figure 1.
Figure 1.
Article screening process.
Summary of included reports
The included reports were published between 29 February 2020 and 26 March 2020. Their guidance was provided from organizations in the United States (US; four reports), United Kingdom (UK; four reports), China (one report), and Australia (one report). One report [World Health Organization (WHO)] was considered an international guidance document (Table 1). Two reports were published in peer-reviewed journals, whereas nine were reported directly on association websites.
Table 1.
Elective surgery guidance from health organizations.
| Organization | Country | Date published | Details regarding elective surgery | Details regarding nonoperative management |
|---|---|---|---|---|
| CDC25 | US | 29 February 2020 | Reschedule elective surgeries as necessary. Shift elective urgent inpatient diagnostic and surgical procedures to outpatient settings, when feasible. | None |
| Tao et al.14 (Overview of National Health Commission of the People’s Republic of China) | China | 1 March 2020 | For patients undergoing elective surgery, it is recommended not to perform surgical treatment for the time being, and they can be elective after the epidemic is under control. | None |
| Royal Australasian College of Surgeons28 | Australia | 1 March 2020 | Series of statements from sub-specialty associations: Non-urgent and elective surgeries to be suspended immediately. | Non operative treatment treatments will confer advantage over operative treatments if similar outcomes, or even slightly downgraded outcomes are expected. |
| American College of Surgeons22 | US | 13 March 2020 24 March 2020 |
Reschedule elective surgeries as necessary. Shift elective
urgent inpatient diagnostic and surgical procedures to
outpatient settings, when feasible. List by subspecialty declaring which surgeries should be schedule or reschedule depending the phase of COVID-19 pandemic. Phase II (curtail elective practice), phase III (eliminate elective practice). Full list by subspecialty in document. |
None Consider nonoperative management whenever it is clinically appropriate for the patient. |
| Centers for Medicare and Medicaid Services26 | US | 15 March 2020 | CMS urges healthcare facilities and clinicians to consider using a tiered approach to curtailing non-emergent, elective medical services and treatment. | None |
| NHS31 | UK | 16 March 2020 | The elective component of trauma and orthopaedic work may be curtailed. Elective resources should be repurposed to support influx of COVID cases. | A number of injuries can be managed either operatively or non-operatively. Clinical decisions during a serious incident must take into account the available facility for the current patient and also the impact this may have on the whole community. |
| 18 March 2020 | NHS hospitals in England have been told to suspend all non-urgent elective surgery for at least 3 months from 15 April 2020 | None | ||
| British Orthopaedic Association24 | UK | 24 March 2020 | Patients should have consultant-delivered, definitive decision-making at first attendance and, in particular, should not be scheduled for surgery without senior input. | Aim for non-operative management for the majority of injuries where this is possible and safe. |
| WHO30 | International | 25 March 2020 | Many routine and elective services may be postponed or suspended. Establishing effective patient flow (including screening, triage, and targeted referral of COVID-19 and non-COVID-19 cases) is essential at all levels. | None |
| Royal College of Surgeons29 | UK | 26 March 2020 | Acute/emergency patients are priority. Only emergency endoscopic procedures should be performed. | Where non-operative management is possible and reasonable (such as for early appendicitis and acute cholecystitis) this should be implemented. |
CDC, Centers for Disease Control and Prevention; NHS, National Health Service; UK, United Kingdom; US, United States; WHO, World Health Organization.
Elective surgery guidance
There were seven (63.6%) guidance reports that suggested a complete postponement of non-elective surgical procedures, whereas four (36.4%) reports suggested the use of selective postponement of these procedures. Throughout the month of March, elective surgery guidance became increasingly strong in its suggestions for completely postponing all elective surgery. Figure 2 provides an overview of the cumulative number of guidance documents within these categories over time. The guidance for postponement of elective surgeries typically suggested that procedures should be rescheduled to a time after the COVID-19 pandemic is over; however, it is unclear as to when this will be. Guidance from the British National Health Service (NHS) has suggested elective surgery will postponed until at least mid-July, as guidance suggested a 3 month postponement starting 15 April.27,31
Figure 2.
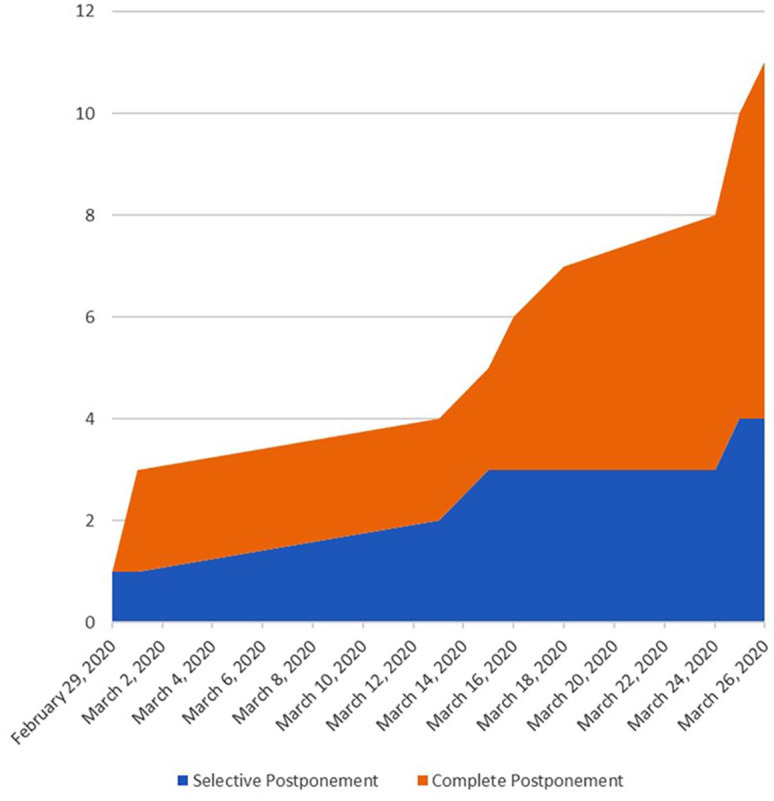
Guidance documents for elective surgery postponement.
Data presented as cumulative number of reports.
The trend of stronger recommendations against elective surgery throughout the month of March is highlighted by two guidance reports provided by the American College of Surgeons on 13 and 24 March 2020. Guidance on 13 March 2020 suggested to “reschedule elective surgeries as necessary” in order to facilitate care for the increased hospital load of COVID-19 patients. Less than 2 weeks later, guidance from the same organization strengthened their guidance to provide a three-phase plan, which ends in “phase III: to eliminate all elective practice”. This trend was seen across guidance groups, indicating that the widespread elimination of elective surgical procedures is apparent. Table 1 provides a brief summary of each report’s guidance on elective surgery in light of the COVID-19 pandemic.
Non-operative management guidance
There were five reports (45.5%) that specifically provided suggestions on the non-operative management of patients who have had their surgery postponed. The general guidance provided by these reports was to consider non-operative treatment options whenever it is possible and safe, in order to limit or delay the need for surgery. When discussing potential outcomes of non-operative treatment, guidance stated “Non-operative treatments will confer advantage over operative treatments if similar outcomes, or even slightly downgraded outcomes are expected”. A summary of the guidance provided by each report is provided in Table 1.
Summary of phased re-introduction of elective surgery
Recently, guidance provided an overview of strategies to eventually phase elective surgery back into clinical practice.20 This guidance suggests that phased introduction of elective surgery will continue to postpone non-urgent elective surgery, with semi-urgent and more urgent elective surgery cases being slowly scheduled when feasible. This feasibility would depend on patient characteristics, potential benefits and harms of surgery, pandemic severity, and hospital resources – including available personal protective equipment (PPE).20 Testing policies are also required to ensure health professional safety, which may be difficult in areas that have limited COVID-19 testing resources. In addition, a prioritization of access to outpatient rehabilitation services will be beneficial in limiting the impact on hospital resource demand for elective surgery phased re-introduction. This includes the use of tele-health and tele-rehabilitation efforts for post-operative follow-ups, which will minimize hospital resources required after surgery.20
Discussion
Summary of current guidance
Based on the guidance documents included in this review, it is apparent that elective surgical practices are being postponed globally. Transitions from selective rescheduling to complete rescheduling of all elective patients has been occurring throughout the month of March. Major guidance groups such as the Centers for Disease Control and Prevention (CDC), NHS, and WHO, have provided guidance on elective surgery, which has been disseminated by smaller organizations and local governments.9 A recently published review of US State guidance on elective surgery provided a similar summary of local government guidance as we have seen within the health association recommendations. This review highlighted that 30 states have called for the complete postponement of elective surgery, and 16 states have suggested selective postponement of elective surgery.9 These recommendations come as a follow up to the reports we have summarized in this review, as health organizations have helped guide local governments in their decision to postpone elective surgery.
Available guidance has agreed that elective surgery must be postponed to help make healthcare needs for the influx of COVID-19 patients more readily accessible and available. What is not apparent is how long this postponement of elective surgery will be required for, as the uncertainty of the COVID-19 patient projections remains. With elective surgery postponed, patients are finding themselves within a treatment gap. They are still living with their condition, but cannot be surgically treated. This period of time has been shown to be a vital time for maintaining patient health and quality of life, as increased surgical wait times can have serious negative health implications.16,17 It is imperative that these patients receive some form of treatment for the time being, until after the pandemic and their surgery can be rescheduled. Currently, it is unclear when this may be, which means it is unknown for how long these patients will be without treatment if they are not offered some sort of conservative intervention. The Royal Australasian College of Medicine suggested that “Non operative treatments will confer advantage over operative treatments if similar outcomes, or even slightly downgraded outcomes are expected”, as even slightly worse outcomes than what would be expected with surgery may still be a better option than providing no treatment at all.28 Decisions for symptom management or conservative therapies that may resolve the condition should be considered during these times due to the removal of surgical intervention as an option. The use of non-operative treatment options is going to play a vital role in the coming years, as the backlog of surgical patients created by the postponement of elective surgery will have a drastic impact on surgical waitlists. In order to judiciously manage and curtail excessive waitlist times for the foreseeable future, clinicians will need to have increased consideration towards non-operative care whenever appropriate. Clinicians should also give greater consideration to options that allow patients to remain at home in order to reduce the burden on healthcare systems. This includes telehealth and virtual follow ups, virtual fracture clinics, as well as treatment options like physical therapy and exercises, that can be administered virtually.
Implications for orthopaedic practice
There are a number of common orthopaedic conditions that would typically be managed operatively, but would not be deemed as urgent procedures within the COVID-19 crisis. Following the COVID-19 pandemic, there will be an increased role of non-operative management to help minimize the impact that the elective surgery shutdowns have had on surgical waitlists. Four major orthopaedic areas affected by this include trauma, sports medicine, spine and joint arthroplasty. Other than acute trauma cases, many procedures for non-urgent fractures or non-unions will be postponed during this pandemic. Within fracture care, this will call on an increased use of non-operative modalities, as well as non-union risk mitigation efforts. Options for non-operative fracture/non-union care may include such modalities as splinting/bracing/casting, bone stimulation using low intensity pulsed ultrasound (LIPUS), physical therapy, or osteoporosis medications (teriparatide). Whereas use of osteoporosis medications have limited evidence for fracture healing specifically,32 LIPUS treatment has demonstrated positive healing properties, particularly within non-unions.33–36 Additional considerations for mitigating the risk of non-union would be to limit the use of non-steroidal anti-inflammatory drugs (NSAIDs), opioids, alcohol, and smoking.37
Sports medicine specialists dealing with soft tissue injury may need to consider the use of physical therapy, bracing, NSAIDs, or local injectables to help manage patient symptoms.38,39 Within arthroplasty practices, physiotherapy, NSAIDs, and injectables may all be potential options for managing patient symptoms in the scenario that their surgical procedure has been postponed.40,41 Evidence has demonstrated patient improvements in pain for 3–6 months after injection with high molecular weight hyaluronic acid for their knee osteoarthritis.42,43 Other options, such as corticosteroid injections may also provide pain relief, but demonstrate a more short-term benefit.44 WHO guidance against the use of corticosteroids in COVID-19 patients has led to some professional groups suggesting that corticosteroids should not be used for pain management during this pandemic.45,46 Clinicians should be cautious in deciding to use corticosteroids due to this guidance. In addition, recent evidence has demonstrated patients who underwent physical therapy had less pain and functional disability than patients who received corticosteroid injection after 1 year.41 Due to social distancing efforts to combat COVID-19, physical therapy interventions may need to be provided through video or tele-health options opposed to in-person sessions. Recent guidelines that specifically address the non-operative management of osteoarthritis have been published by professional groups such as OARSI, which should also be given increased consideration when managing these patients.47 Programs such as the GLA: D program in Canada or the Escape Pain program in the UK have been introduced to help provide remote physical therapy and exercise programs to individuals suffering from arthritis. This allows for patients to remain socially isolated, while still gaining the benefits of physical therapy. The use of virtual and telehealth interventions to help manage patient symptoms will not only provide therapeutic relief to patients, but also reduce the burden on healthcare centers during the COVID-19 pandemic.
Spine surgeons also face unique challenges due to the postponement of non-urgent surgery. For conditions such as lumbar disc herniation, there is some evidence that non-operative options could provide some symptom relief. Whereas surgical intervention may provide superior outcomes, the absence of surgery as a treatment option may lead to an increased consideration for non-operative care.48 Given the progress that has been made on limiting exposure to opioids and decreasing opioid utilization, decisions surrounding treatment pathways should maintain strict protocols around pain management options. Table 2 provides a summary of non-operative management options that one may consider for patients who have had their operative treatment postponed.
Table 2.
Potential orthopaedic non-operative management options.
| Indication | Non-operative treatment options |
|---|---|
| Fractures/non-unions | Bracing/splinting/casting Physical therapy Bone stimulation (LIPUS) Osteoporosis Medications |
| Osteoarthritis | Bracing Physical therapy Weight Loss NSAIDs Injectables: Hyaluronic acid injection Corticosteroid injection Platelet-rich plasma |
| Soft tissue injury | Bracing/splinting/casting Physical therapy NSAIDs Injectables: Corticosteroid injection* Platelet-rich plasma Local anaesthetics |
| Spine | Physical therapy Pain medication Bed rest |
LIPUS, low intensity pulsed ultrasound; NSAIDS, non-steroidal anti-inflammatory drugs.
May be contraindicated for COVID-19 patients.
Strengths and limitations
This review is strengthened by its systematic approach to identifying relevant literature. Despite this approach, it remains a challenge to identify all relevant documents, as many organizations are opting to publish guidance directly on their websites, opposed to through traditional peer-reviewed journals. While this allows for a more rapid dissemination of information, it poses as a challenge when synthesizing all available reports. Forgoing the peer-review process also risks that information is not being thoroughly vetted before being publicly released. In addition, there are changing recommendations within individual organizations and societies that are occurring in real-time. There is a current struggle between having new information rapidly available and having information thoroughly reviewed for accuracy. Despite the possibility that some non-peer reviewed guidance from medical association websites or internal correspondence was not captured in this review, the available documents provide a representative sample of the current global recommendation trends regarding the postponement of elective surgery.
Conclusion
Global guidance from major medical associations are in agreement that elective surgical procedures require postponement in order to minimize the risk of COVID-19 spread, as well as increase available hospital resources for managing the influx of COVID-19 patients. For patients that have their elective surgery postponed, there is no clarity as to how long it will be before their elective surgeries will be rescheduled. It is imperative that clinicians and patients consider non-operative, conservative treatment options in order to manage conditions and symptoms until surgical management options become available again, and to manage the increased surgical waitlists caused by the elective surgery shutdowns.
Supplemental Material
Supplemental material, COVID_Appendix_A for Impact of COVID-19 on orthopaedic care: a call for nonoperative management by Mark R. Phillips, Yaping Chang, Robert D. Zura, Samir Mehta, Peter V. Giannoudis, Peter A. Nolte and Mohit Bhandari in Therapeutic Advances in Musculoskeletal Disease
Footnotes
Conflict of interest statement: Mark Phillips: Employer received grant support from Bioventus
Yaping Chang: Nothing to disclose
Robert D. Zura: Consultant for Osteocentric and Bioventus
Samir Mehta: Paid presenter/speaker for DePuy Synthes, GE Healthcare, NuVasive, and Smith and Nephew. Paid consultant for Smith & Nephew, and DePuy Synthes. Receives publishing royalties from Wolters Kluwer Health-Lippincott Williams & Wilkins. Board member for the Pennsylvania Orthopaedic Society and Current Opinion in Orthopedics.
Peter V. Giannoudis: Nothing to disclose
Peter A. Nolte: Nothing to disclose
Mohit Bhandari: Personal fees from AgNovos Healthcare, Sanofi Aventis, Stryker, Pendopharm, Bioventus, grants from DJ Orthopaedics, Acumed
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a grant from Bioventus.
ORCID iDs: Mark R. Phillips  https://orcid.org/0000-0003-0923-261X
https://orcid.org/0000-0003-0923-261X
Yaping Chang  https://orcid.org/0000-0002-0549-5087
https://orcid.org/0000-0002-0549-5087
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Mark R. Phillips, Department of Health Research Methods, Evidence, and Impact, McMaster University, 1280 Main St West, Hamilton, ON L8S 4L8, Canada.
Yaping Chang, OrthoEvidence Inc., Burlington, ON, Canada.
Robert D. Zura, Department of Orthopaedic Surgery, Louisiana State University Health Sciences Center, New Orleans, LA, USA
Samir Mehta, Department of Orthopaedic Surgery, University of Pennsylvania, Philadelphia, PA, USA.
Peter V. Giannoudis, Department of Trauma and Orthopaedic Surgery, Leeds University, Leeds, UK
Peter A. Nolte, Department of Orthopaedic Surgery, Spaarne Gasthuis, Hoofddorp, the Netherlands
Mohit Bhandari, Division of Orthopaedic Surgery, McMaster University, Hamilton, ON, Canada.
References
- 1. World Health Organization. Novel coronavirus (2019-nCoV) situation reports, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (2020, accessed April 15, 2020).
- 2. Greenland JR, Michelow MD, Wang L, et al. COVID-19 infection: implications for perioperative and critical care physicians. Anesthesiol J Am Soc Anesthesiol. Epub ahead of print 18 March 2020. DOI: 10.1097/ALN.0000000000003303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Halawi MJ, Wang DD, Hunt TR. What’s important: weathering the COVID-19 crisis: time for leadership, vigilance, and unity. J Bone Joint Surg Am. Epub ahead of print 8 April 2020. DOI: 10.2106/JBJS.20.00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Swiontkowski M. COVID-19 pandemic and JBJS. J Bone Joint Surg Am. Epub ahead of print 2 April 2020. DOI: 10.2106/JBJS.20.00471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vannabouathong C, Devji T, Ekhtiari S, et al. Novel coronavirus COVID-19: current evidence and evolving strategies. J Bone Joint Surg Am. Epub ahead of print 1 April 2020. DOI: 10.2106/JBJS.20.00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brindle M, Gawande A. Managing COVID-19 in surgical systems. Ann Surg. Epub ahead of print 23 March 2020. DOI: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wong J, Goh QY, Tan Z, et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anesth Can Anesth. Epub ahead of print 11 March 2020. DOI: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chang Liang Z, Wang W, Murphy D, et al. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. Epub ahead of print 20 March 2020. DOI: 10.2106/JBJS.20.00236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sarac NJ, Sarac BA, Schoenbrunner AR, et al. A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. J Bone Joint Surg Am. Epub ahead of print 13 April 2020. DOI: 10.2106/JBJS.20.00510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chan JYK, Wong EWY, Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic: an experience in Hong Kong. JAMA Otolaryngol Neck Surg. Epub ahead of print 20 March 2020. DOI: 10.1001/jamaoto.2020.0488. [DOI] [PubMed] [Google Scholar]
- 11. Chan MC, Yeo SEK, Chong YL, et al. Stepping forward: urologists’ efforts during the COVID-19 outbreak in Singapore. Eur Urol. Epub ahead of print 17 March 2020. DOI: 10.1016/j.eururo.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chandy PE, Nasir MU, Srinivasan S, et al. Interventional radiology and COVID-19: evidence-based measures to limit transmission. Diagn Interv Radiol Ank Turk. Epub ahead of print 31 March 2020. DOI: 10.5152/dir.2020.20166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guo X, Wang J, Hu D, et al. Survey of COVID-19 disease among orthopaedic surgeons in Wuhan, people’s Republic of China. J Bone Joint Surg Am. Epub ahead of print 8 April 2020. DOI: 10.2106/JBJS.20.00417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tao KX, Zhang BX, Zhang P, et al. Recommendations for general surgery clinical practice in 2019 coronavirus disease situation. Zhonghua Wai Ke Za Zhi 2020; 58: 170–177. [DOI] [PubMed] [Google Scholar]
- 15. Brinker MR, Trivedi A, O’Connor DP. Debilitating effects of femoral nonunion on health-related quality of life. J Orthop Trauma 2017; 31: e37–e42. [DOI] [PubMed] [Google Scholar]
- 16. Ostendorf M, Buskens E, van Stel H, et al. Waiting for total hip arthroplasty: avoidable loss in quality time and preventable deterioration. J Arthroplasty 2004; 19: 302–309. [DOI] [PubMed] [Google Scholar]
- 17. Scott CEH, MacDonald DJ, Howie CR. “Worse than death” and waiting for a joint arthroplasty. Bone Joint J 2019; 101–B: 941–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brinker MR, Hanus BD, Sen M, et al. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am 2013; 95: 2170–2176. [DOI] [PubMed] [Google Scholar]
- 19. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Prada C, Chang Y, Poolman R, et al. Best practices for surgeons: COVID-19 evidence-based scoping review. Version 2. OrthoEvidence, http://myoe.blob.core.windows.net/docs/OE-Best-Practices-for-Surgeons-COVID-19-Evidence-Based-Scoping-Review.pdf?utm_source=activecampaign&utm_medium=email&utm_campaign=covid19_surgical_protocols&utm_content=Version2 (2020, accessed 14 April 2020).
- 21. Gazendam A, Ekhtiari S, Wong E, et al. The “Infodemic” of journal publication associated with the novel coronavirus disease. J Bone Joint Surg Am. Epub ahead of print 12 May 2020. DOI: 10.2106/JBJS.20.00610. [DOI] [PubMed] [Google Scholar]
- 22. American College of Surgeons. COVID-19: recommendations for management of elective surgical procedures, https://www.facs.org/covid-19/clinical-guidance/elective-surgery (2020, accessed 14 April 2020).
- 23. American College of Surgeons. COVID-19: elective case triage guidelines for surgical care, https://www.facs.org/covid-19/clinical-guidance/elective-case (2020, accessed 14 April 2020).
- 24. British Orthopaedic Association. BOAST - Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic, https://www.boa.ac.uk/resources/covid-19-boasts-combined.html (2020, accessed 24 March 2020).
- 25. Centers for Disease Control and Prevention. COVID-19: interim guidance for elective surgery and outpatient clinics - Diseases, https://www.health.nsw.gov.au/Infectious/diseases/Pages/coronavirus-elective-outpatient-guidance.aspx (2020, accessed 14 April 2020).
- 26. Centers for Medicare and Medicaid Services. CMS releases recommendations on adult elective surgeries, non-essential medical, surgical, and dental procedures during COVID-19 response, https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental (2020, accessed 14 April 2020).
- 27. Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ 2020; 368: m1106. [DOI] [PubMed] [Google Scholar]
- 28. Royal Australasian College of Surgeons. COVID-19 information hub: RACS, https://www.surgeons.org/media-centre/covid-19-information-hub#Elective%20surgery%20recommendations%20from%20specialty%20societies (2020, accessed 14 April 2020).
- 29. Royal College of Surgeons. Updated intercollegiate general surgery guidance on COVID-19, https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/ (2020, accessed 14 April 2020).
- 30. World Health Organization. COVID-19: operational guidance for maintaining essential health services during an outbreak, https://www.who.int/publications-detail/covid-19-operational-guidance-for-maintaining-essential-health-services-during-an-outbreak (2020, accessed 14 April 2020).
- 31. National Health Service. Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic, https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-orthopaedic-trauma-and-coronavirus-v1-16-march-2020.pdf (2020, accessed 14 April 2020).
- 32. Shin YH, Shin WC, Kim JW. Effect of osteoporosis medication on fracture healing: an evidence based review. J Bone Metab 2020; 27: 15–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zura R, Mehta S, Della Rocca GJ, et al. A cohort study of 4,190 patients treated with low-intensity pulsed ultrasound (LIPUS): findings in the elderly versus all patients. BMC Musculoskelet Disord 2015; 16: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zura R, Della Rocca GJ, Mehta S, et al. Treatment of chronic (>1 year) fracture nonunion: heal rate in a cohort of 767 patients treated with low-intensity pulsed ultrasound (LIPUS). Injury 2015; 46: 2036–2041. [DOI] [PubMed] [Google Scholar]
- 35. Leighton R, Watson JT, Giannoudis P, et al. Healing of fracture nonunions treated with low-intensity pulsed ultrasound (LIPUS): a systematic review and meta-analysis. Injury 2017; 48: 1339–1347. [DOI] [PubMed] [Google Scholar]
- 36. Rutten S, van den Bekerom MPJ, Sierevelt IN, et al. Enhancement of bone-healing by low-intensity pulsed ultrasound: a systematic review. JBJS Rev 2016; 4: 01874474-201603000-00006. [DOI] [PubMed] [Google Scholar]
- 37. Zura R, Braid-Forbes MJ, Jeray K, et al. Bone fracture nonunion rate decreases with increasing age: a prospective inception cohort study. Bone 2017; 95: 26–32. [DOI] [PubMed] [Google Scholar]
- 38. Hotfiel T, Seil R, Bily W, et al. Nonoperative treatment of muscle injuries - recommendations from the GOTS expert meeting. J Exp Orthop. 2018; 5: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hertel J. The role of nonsteroidal anti-inflammatory drugs in the treatment of acute soft tissue injuries. J Athl Train 1997; 32: 350–358. [PMC free article] [PubMed] [Google Scholar]
- 40. Bannuru RR, Schmid CH, Kent DM, et al. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med 2015; 162: 46–54. [DOI] [PubMed] [Google Scholar]
- 41. Deyle GD, Allen CS, Allison SC, et al. Physical therapy versus glucocorticoid injection for osteoarthritis of the knee. N Engl J Med 2020; 382: 1420–1429. [DOI] [PubMed] [Google Scholar]
- 42. Bannuru RR, Natov NS, Dasi UR, et al. Therapeutic trajectory following intra-articular hyaluronic acid injection in knee osteoarthritis-meta-analysis. Osteoarthritis Cartilage 2011; 19: 611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Phillips M, Vannabouathong C, Devji T, et al. Differentiating factors of intra-articular injectables have a meaningful impact on knee osteoarthritis outcomes: a network meta-analysis. Knee Surg Sports Traumatol Arthrosc. Epub ahead of print 3 January 2020. DOI: 10.1007/s00167-019-05763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bannuru RR, Natov NS, Obadan IE, et al. Therapeutic trajectory of hyaluronic acid versus corticosteroids in the treatment of knee osteoarthritis: a systematic review and meta-analysis. Arthritis Rheum 2009; 61: 1704–1711. [DOI] [PubMed] [Google Scholar]
- 45. World Health Organization. Clinical management of severe acute respiratory infection when COVID-19 is suspected, https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected (accessed 27 April 2020).
- 46. Faculty of Pain Medicine of the Royal College of Anaesthetists. FPM response to concern related to the safety of steroids injected as part of pain procedures during the current COVID-19 virus pandemic, https://fpm.ac.uk/sites/fpm/files/documents/2020-03/FPM-COVID-19-Steroid-Statement-2020.pdf (2020, accessed 14 April 2020).
- 47. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 2019; 27: 1578–1589. [DOI] [PubMed] [Google Scholar]
- 48. Chen BL, Guo JB, Zhang HW, et al. Surgical versus non-operative treatment for lumbar disc herniation: a systematic review and meta-analysis. Clin Rehabil 2018; 32: 146–160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, COVID_Appendix_A for Impact of COVID-19 on orthopaedic care: a call for nonoperative management by Mark R. Phillips, Yaping Chang, Robert D. Zura, Samir Mehta, Peter V. Giannoudis, Peter A. Nolte and Mohit Bhandari in Therapeutic Advances in Musculoskeletal Disease