Short abstract
Objectives
Our objective was to assess the health care system impacts associated with the December 2013 east coast flooding in Boston, Lincolnshire, in order to gain an insight into the capacity of the health care sector to respond to high-impact weather.
Methods
Semistructured interviews were held with regional strategic decision makers and local service managers within 1 km of the recorded flood outline to ascertain their experiences, views and reflections concerning the event and its associated health impacts and disruption to health care services. A snowballing sampling technique was used to ensure the study had participants across a broad range of expertise. Interviews were recorded and transcribed verbatim, and data analysis was preformed using NVivo (v10) to apply a thematic coding and develop a framework of ideas.
Results
The results of this case study provide a vital insight into the health care disruption caused by flooding. All sectors of the health care system suffered disruption, which placed a strain on the whole system and reduced the capacity of the sector to respond to the health consequences of flooding and delivering routine health care. The formal recovery phase in Lincolnshire was stood-down on 4th February 2014. The results of this work indicate limitations in preparedness of the health care system for the reasonable worse-case scenario for an east coast surge event.
Conclusions
The health care sector appears to have limited capacity to respond to weather-related impacts and is therefore unprepared for the risks associated with a future changing climate. Further work is required to ensure that the health care system continues to review and learn from such events to increase climate resilience.
Keywords: climate change, climate resilience, east coast surge, extreme weather events, high-impact weather, public health
Introduction
The resilience of health care systems is an emerging topic of international importance, reflecting concerns about the wide-ranging consequences for human health from climate change.1,2 Health care systems themselves need to be resilient to climatic events to ensure that there is sufficient capacity to address the impacts of climate change on human health.2–6 The World Health Organization’s working definition of a climate resilient health system is one ‘that is capable to anticipate, respond to, cope with, recover from and adapt to climate related shocks and stress, so as to bring sustained improvements in population health, despite an unstable climate.’7
Storms and floods are known to reduce the ability of health care systems to respond to health crises, affecting the quality of health care provision.8–10 Despite recognition of the vulnerability, there is a lack of research into how climate change will impact on health care systems and what mitigation measures are available.2,5 More specifically, few studies have explored in detail the impacts of flooding on health care systems,10 despite previous flood events having detrimental effects on health care system infrastructure across Europe.7,11
Coastal flooding is considered a significant risk to the United Kingdom’s (UK) national security according to the National Risk Register of Civil Emergencies and has been shown to damage critical national infrastructure, including health care assets.2,12–15 Given the country’s investment in health care, the financial risks are considerable. According to the UK Health Accounts, published by the Office for National Statistics, health care expenditure in the UK accounted for 9.8% of gross domestic product in 2016. Ascertaining the current level of risk is challenging due to the dynamic nature of flood risk. Approximately 14% of ambulance stations (n = 111), 12% of fire stations (n = 160), 11% of police stations (n = 47) and 6% to 8% of hospitals (n = 111), care homes (n = 1044) and surgeries (n = 800) in the UK are located in areas that are susceptible to fluvial and coastal flooding.16 Assuming a continuation of climate change, future climate projections for the UK suggest that flood risk to health care assets is likely to increase. The proportion of care homes, emergency services, hospitals and doctors’ surgeries at risk of flooding in England is set to increase by 13%, 11%, 4% and 12%, respectively, by the 2050s under a 2-degree warming scenario.2,6,17
The 2008 Pitt Review, conducted after the 2007 floods in England, highlighted the vulnerability of the UK’s health care systems to flooding and concluded that there were significant failings in the management and response to flood risks.18 More recently, the National Adaptation Programme made specific reference to the need for climate resilience within the health care system.19 However, research on the impact of climate change is lacking. We believe this paper is the first in the UK to seek to address this knowledge gap by investigating the impact of the 2013–2014 flood events in Boston, England.
Winter 2013–2014
The winter of 2013–2014 was exceptionally stormy across the UK and was identified as England’s wettest winter in 250 years.20 On Thursday, 5th December 2013, a deepening pressure system coincided with spring tides and strong to gale force north-westerly winds to generate a coastal surge along the east coast of England. Coastal water levels exceeded some of those recorded during the ‘great storm’ of 1953 which resulted in 307 fatalities and evacuation of 32,000 people21 and which is the basis for the reasonable worse-case scenario used in emergency planning assumptions (Table 1).
Table 1.
Planning assumption for reasonable worse-case scenario (multiple breaches of defences).22
| Vulnerable profile | Local infrastructure |
|---|---|
| 80,500 properties at risk | 6 fire/police/ambulance stations |
| 3 hospitals | 176 km of road |
| 29 schools | 30 bridges |
| 32 care homes | 11.8 km of rail |
| 1 prison | 6 major hazard sites |
| 20 fatalities | 32 electricity sub-stations |
| 300 casualties | 63 water pumping |
| 50,000 evacuees | 15 sewage works |
The December 2013 surge overtopped 18 to 20 km of flood defences and breached flood defences in four locations, causing an estimated £8.1m worth of damage to flood defences and infrastructure. Across Lincolnshire, several hundred homes were flooded (the majority in Boston, Trusthorpe and Susworth), 121 businesses were flooded, 44 persons and two pets were rescued from flood waters and 203 people received assistance to evacuate.22
Methods
This study aimed to assess the health care system impacts associated with the December 2013 east coast storm surge and subsequent flooding in Boston, a port town in Lincolnshire. Semistructured interviews were undertaken with personnel involved in preparing for, responding to and recovering from the December 2013 flooding: regional strategic decision makers (those within the County Emergency Centre or with responsibility for more than one health asset, for example, Public Health Consultants) and local service managers (those with responsibility for one health asset, for example, family doctor practice managers). A document analysis of the published Local Resilience Forum (LRF) postincident review provided additional information and confidence in the robustness of the findings.
Semistructured interviews gave space for the interviewee to influence the focus of the interview and encouraged a conversational two-way dialogue between the interviewer and the interviewee.23 Interviews were designed to enable responders to express their experiences, views and reflections of the event whilst also providing an insight into the level of damage and disruption to sites, infrastructure, equipment and services before, during and after 5th December 2013.
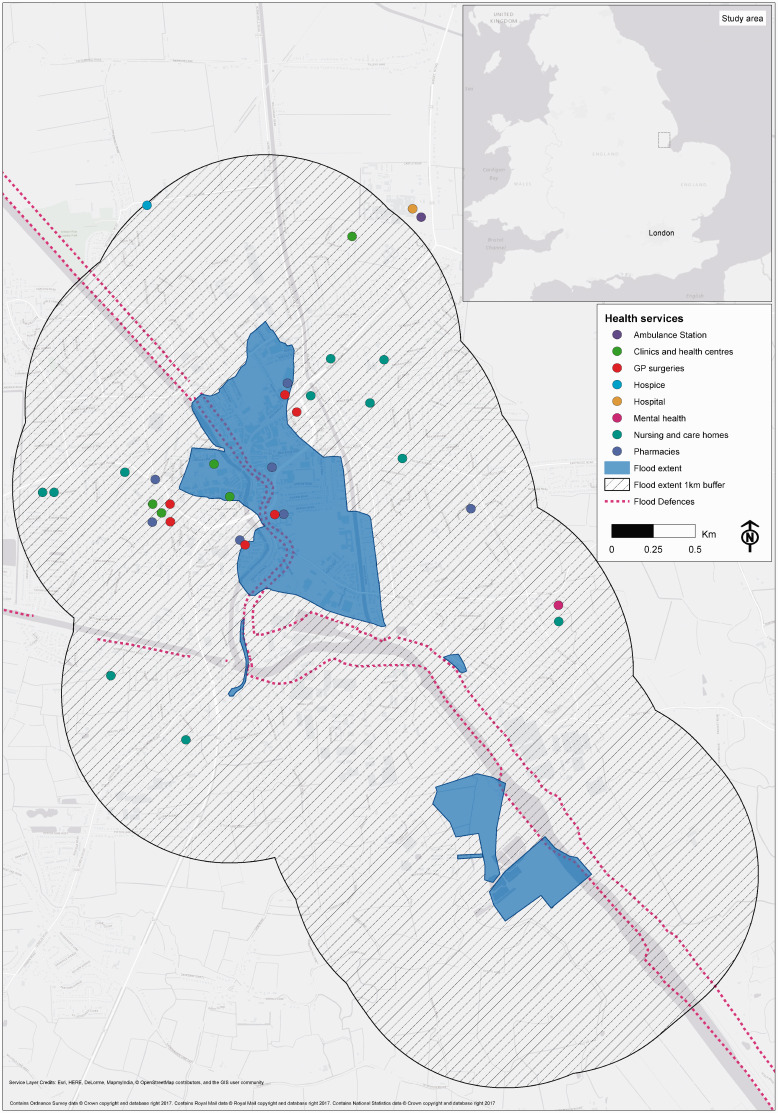
The December 2013 flood outline was ascertained using the Environment Agency historical flood extent database. Health care sites and contact details were obtained from Public Health England (PHE) databases. Geospatial extraction was performed using ArcMap v10.2. The 32 local service managers within 1 km of the flood extent were invited via post to participate in a 30-minute telephone interview (Figure 1). The 1-km radius enabled the inclusion of health care facilities and services directly flooded and those disrupted or otherwise indirectly affected by the flooding.
Figure 1.
Flood extent of December 2013 east coast surge and location of health care sites.
GP: general practitioner.
Regional strategic decision makers were identified in collaboration with the East Midlands PHE Centre and the Public Health Department of Lincolnshire County Council. A total of 15 participants were invited via email to participate in a 1-hour telephone or face-to-face interview, depending upon their availability and preference. Using telephone interviews also overcame the constraints of time, resources and geographical location for researchers and participants.
Interviews were conducted during June and July 2016, using snowball sampling to ensure the study had participants across a broad range of expertise. A strategy to determine the appropriateness of the sample size broadly in line with the concept of saturation was applied,24 with suggested individuals/services being invited and interviewed until no new themes or issues emerged. All participants provided written consent prior to participation, and interviews were recorded and transcribed verbatim for data analysis. To maintain confidentiality, participants were ascribed a random participant number. The data were analysed using NVivo (v10) to apply thematic coding,25 permitting a framework of ideas to be established from the data. NVivo facilitates management and organization of data into codes that take the form of analytic themes arising from the data. Once coded, the resulting data files were read and reread and treated to several iterations of sense making. This process was primarily data led, with a focus on emergent concerns, but it was also informed by the existing literature and key concerns relevant to policy. The coding framework was created iteratively, with an initial coding exercise carried out by the research team using a selection of transcripts to agree initial themes and ensure consistency.
Results
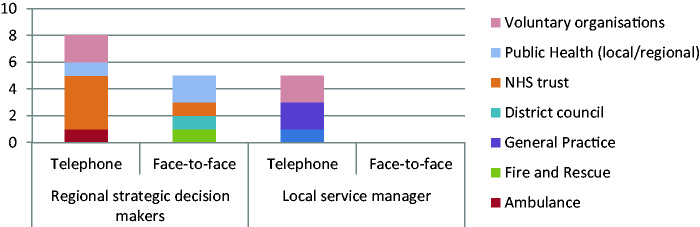
A total of 18 semistructured interviews were conducted, 7 face-to-face and 11 via telephone; 5 local service managers across 4 localities and 13 regional strategic decision makers participated in the study. The response rate amongst regional strategic decision makers was 86.6%; for local service managers, it was 15.6%. Participants were drawn from a wide range of frontline health care services and strategic organizations, including National Health Service (NHS) trusts, emergency services and local government. Two voluntary sector organizations were included in the study, one offering palliative and end-of-life care and another providing people, equipment, space and resources to support those affected by an emergency (Figure 2).
Figure 2.
Breakdown of interviews by interview and organization type.
NHS: National Health Service.
The analysis revealed the following five major themes: warning and preparedness, at-risk populations, evacuation, health care infrastructure and services, and opportunities for resilience. These themes are discussed in the following sections.
Warning and preparedness
Levels of preparedness, recognition of the flood risk and awareness of the potential impacts of the surge were found to be inconsistent across the health care system, with a particular divergence between strategic and frontline organizations. Respondents described limited preparatory action among local frontline services, despite the inclusion of the health care system within the multiagency coastal flooding Exercise Lazarus held in November 2013.
A high level of preparedness was reported amongst regional strategic decision makers: ‘In fact, they [Flood Forecasting Centre] are so good now at forecasting the impacts … we do take them very seriously’ (strategic decision maker 008). However, this view was not echoed by frontline staff who stated ‘[flooding] was worse than we expected … the actual aftermath of patients wanting to be seen etc., was a lot more chaotic’ (local service manager 030). Some frontline providers also reported that their organizations were not registered to receive direct flood alerts.
The flood risk threatened the 391-bed Pilgrim District General Hospital and led to precautionary action being taken at a cost of over £5,000: ‘ … the infrastructure of the hospital is under ground level so we’d actually lose electric, gas, oxygen, everything, if we got a couple of inches of water’ (strategic decision maker 044). Where local frontline preparedness was discussed, activity included sandbagging and the moving of medical records upstairs: ‘ … it was 2 o’clock in the morning … I actually was in work at that time … we were able to prepare and try and sandbag off … we did actually move some of the medical records’ (local service manager 030).
At-risk populations
Determining vulnerability to the health impacts of flooding is complex. Difficulties in defining the term ‘vulnerability’ and different institutional practices for formatting data hindered information sharing and the compilation of a comprehensive list of vulnerable individuals. ‘Hidden’ populations (such as (unregistered) migrant workers) and those with English as a second language challenged effective communication of flood risks.
Institutional challenges in identifying at-risk individuals emerged: ‘ … someone who is registered blind with significantly reduced mobility but actually lives in supported housing … and her daughter does her shopping … she is a significant vulnerable person but she’s not sitting on anybody’s list’ (strategic decision maker 043). Furthermore, vulnerability is not a static characteristic: ‘[people] … suddenly find themselves vulnerable, a mother who’s just been released out of hospital after having a baby’ (strategic decision maker 008).
Challenges defining flood vulnerability led to miscommunication between frontline responders and the Strategic Coordination Group (SCG) responsible for coordinating the joint response to the flooding: ‘the NHS … asked us for a list of vulnerable patients … so we were asking, what do you mean and they didn’t have a set criteria … another practice would have done what they thought’ (local service manager 030). Postflooding, several general practices developed a set of vulnerability criteria to aid future flood management. Different data formats hindered the compilation of a comprehensive list of vulnerable people; some vulnerable individuals were identified after the flooding through door-to-door knocking and referred to the voluntary sector: ‘ … the lists of lists didn’t work … So we produced a questionnaire on an A4 sheet of paper … to go and door knock and … find out what the vulnerabilities are’ (strategic decision maker 008).
A significant population of migrant workers presented a challenge to effective communication of the flood risks: ‘ … there was a significant percentage or proportion of people that … didn’t have English as their first language’ (strategic decision maker 003). One strategic decision maker reflected: ‘ … there are 70 different languages spoken … and so we contacted [local translation company] and they … went round with the Police doing the door knocking … we’d send them [our public communications] … and we’d have that back in five or six different languages’. The effectiveness of public flood alerts was also raised: ‘ … after [the flood] … people [public] then say “I received a flood warning, I didn’t know what to do with it”’ (strategic decision maker 008).
Evacuation
Evacuation of the Boston area was complex due to densely occupied housing, refusal to evacuate and cases of complex health care being delivered at home. In addition, routine health care was disrupted by evacuation. Commenting on the refusal to evacuate, one participant reflected:
People would literally refuse to move and potentially put themselves in danger unless their pet could go with them … refused to answer the door to the police so you have to get a district nurse or a health worker to go with the police and try to persuade the patient. (local service manager 005)
Logistical challenges were introduced by a very high number of evacuees having a body mass index of 40+. Patients receiving complex health care at home were encountered during the evacuation process:
If patients were complex or especially bariatric, that some logistics were going to be needed to move them, we would advise the police … some patients made the decision that they wouldn't move, … so for them it’s a case of keeping them safe where they are … .it’s about how you get that support into them and that they’re understanding the implications of the choices that they’ve made ….an individual that is very vulnerable and just refuses to move can take an enormous amount of effort to sort out. (local service manager 005)
Challenges regarding mental capacity (a person’s ability to make their own decisions) and the right for palliative patients to refuse evacuation were also raised: ‘There was one gentleman who had a palliative diagnosis … he was living in the upstairs of his house because the lower floor was flooded … but the gentleman had [mental] capacity, he didn’t want to move out of his house … ’ (local service manager 006).
Evacuees arrived at rest centres without their prescription medication and reported stress-related conditions. Sourcing medication proved difficult despite the presence of prescribing nurses at the evacuation centres:
Mostly it [work in the rest centres] was related to people who’d been evacuated, who hadn’t got medication, people who, due to the stress of being evacuated also then developed chest pain or breathing difficulties … trying to identify pharmacists was quite difficult. (local service manager 006)
Evacuation and temporary relocation was found to compromise patient tracking. However, deducing an evacuee’s regular medication was aided by summary care records (an electronic patient record providing a summary of NHS patient data held on a central database covering England) ‘ … in terms of finding out what medication someone is on, summary care records are available and they are important technologies to exploit’ (local service manager 005). Record management issues also caused difficulties in tracking vulnerable children: ‘ … the evacuation centres’ use of paper records … caused us problems in terms of being able to access our records and look at where those vulnerable children might have gone, making sure we could keep track of those children (local service manager 005).
Health care infrastructure and services
All participants reported health care sector disruption; one health care site was reportedly flooded with two feet of water. At a time of seasonal pressure on services (the increase in demand for health and social care services seen in winter), mutual aid was required across health care providers, and services were relocated to other sites around Boston because of flooding or power loss.
Nursing staff and assets were relocated to support other services and the emergency response (for example, evacuation centres). Staff from the voluntary sector provided support. Disruptions caused by staff shortages were widely reported, alongside difficulty accessing sites for both patients and staff: ‘The Police were stopping people travelling down certain roads … it took a while before the Police on the ground were allowing NHS staff through … so there were people working a couple of hours’ longer waiting for their relief to come in’ (strategic decision maker 044).
Staff-owned four-wheel drive vehicles were used to transport doctors to home visits and to assist health care staff in getting to work. The Lincolnshire 4 × 4 Response charity provided support to the health care sector: ‘ … the 4 by 4 people were out in their big 4 by 4 Range Rovers getting places, getting staff moved ’ (strategic decision maker 044). Staff being personally affected by flooding further reduced workforce levels: ‘I had both staff that couldn't get into work because of their own personal concerns at home’ (strategic decision maker 042).
Routine health care was disrupted across multiple services. In light of the flooding, dialysis treatment was delayed and appointments rescheduled for the next day; disruptions were also reported for dentistry and sexual health services. Family doctor appointments were rescheduled, home visits were extended into the evening, and telephone consultations were offered as an alternative to face-to-face consultations. Mental health services followed instructions to evacuate one unit in Boston, leading to the withdrawal of face-to-face services for one day.
Pilgrim District General Hospital prepared for vertical evacuation (moving patients to a higher floor away from the area of danger) with clinicians undertaking evacuation triage of inpatients. Elective surgery and outpatient clinics were cancelled for 6th December 2013, and discharges were halted the evening of the surge:
We can’t discharge 90 year olds to homes that were about to be flooded, … we halted all discharges … Luckily for us, we had spare beds that night … we run generally around 97-99%, we’re always pretty full … it increases the pressure on transport to get people out. (strategic decision maker 004)
Ambulance diversions to alternative hospitals were also activated: ‘ … if somebody was inbound on an ambulance and … they were on the cusp of going to one hospital or another … we said it’s still open but it could be flooded so you might as well send them to another hospital’ (strategic decision maker 044). Furthermore, ‘ … ambulances couldn’t get through the water … we had to pull a couple of them out [ambulances assigned to the rescue operation] to go and deal with a chest pain that was in an area where the ambulances couldn’t get to’ (strategic decision maker 010).
Admission criteria were relaxed for evacuees receiving complex health care at home in order to place them in community hospitals overnight. With limited places and the need to maintain services, the movement of patients and mutual aid required between organizations placed a strain on services felt across the health care sector:
If the nursing homes were going to be evacuated, where were we going to put those people because at that time, it was a time of winter pressures as well … how would we maintain the acute trust services because if we put some of those into our community hospitals, then the community hospitals wouldn’t be able to discharge, so it raised a lot of questions in terms of the whole system working. (local service manager 006)
Disruption to the day-to-day work of the health care system led to the prioritization of patients and the cancellation of services outside the flooded area:
People that were expecting the district nurses and were not going to get it … and what’s the implication of that and is that critical, that visit, or not critical … and that could be for patients that are nowhere near the flooding at all … . (local service manager 005)
The impact on health care service demand was described as a surge:
It might be water contamination or illness … you do tend to get a bit of a surge of patients turning up … general practice often feel the brunt of that, of course, A&E department to an extent as well but particularly general practice. (local service manager 005)
Furthermore, an increased demand for psychological services was reported in the area postflooding: ‘ … there was an increase in the number of people seeing their GP, with anxiety and depression … there was some evidence of a slight increase in psychological demand’ (strategic decision maker 002).
Opportunities for resilience
All participants reported that their organizations had reviewed policy and practice following the flooding: ‘It focused the mind and it did make us make changes and make a difference’ (local service manager). An increase in frontline preparedness and subscription to flood alert services was reported postflooding:
Now, if we get a flood warning saying this is going to happen, move stuff off the floor and have the sandbags prepared … .so I think if we get a serious warning in the future, it will be taken a lot more seriously. (local service manager 030)
Following the event, predefined search criteria for vulnerable patients have been agreed between some GP practices and a new vulnerable persons protocol has been created by the LRF: ‘we have now said to organisations “you hold your own list, we will contact you and tell you what the risk is and what you need to do and then you contact your own people”’ (strategic decision maker 043). During future floods, this approach will be supported by a temporary telephone helpline number for those who find themselves vulnerable: ‘So we’re capturing those that suddenly find themselves vulnerable … to then contact the relevant organisations within health to provide that support’ (strategic decision maker 008).
The evacuation plan for Pilgrim District General Hospital was revised:
Pilgrim Hospital have had a robust review of their hospital evacuation plan … some of the learning and the benefits … is that the [evacuation] plan, whereas previously has been written very much in silo by the hospital, has now absolutely had consultation with wider partners. (strategic decision maker 043)
An action card for the medical director has been created: ‘We’ve got an action card now for our medical director, so the medical lead has now been incorporated into our major incident plan’ (strategic decision maker 044). Business continuity arrangements have also been reviewed with one participant reflecting: ‘ … our evacuation plans had been [to relocate] to health centres close by and in fact, those health centres would have also been flooded … it did make us look at a wider range of business continuity’ (local service manager 005).
Barriers to property-level protection included cost, confusion over the level of flood risk and tenancy agreements: ‘We’ve looked at flood gates … I think they said it was going to cost about £20k, so we’ll take the risk’ (local service manager 030). Difficulties obtaining sandbags were reported, and accounts of sandbags being stolen were shared by participants. One GP practice now stores sand and empty sandbags on-site for future events.
Participants reflecting on the event identified some positive themes. Despite a reported low uptake (∼50%) of household insurance,22 engagement with the Association of British Insurers within the recovery phase was considered successful, as: ‘ … very distressed and emotional members of the public, were able to have a single point … that could address all their concerns … and that worked extremely well’ (strategic decision maker 003). Within the SCG, the amalgamation of the originally separate health and social care cells provided a more holistic health sector perspective. Participants reflected that the impact upon the health care sector would have been significantly worse, had it not been for the staff themselves: ‘The NHS does stand up and goes beyond the call of duty … that’s good in a way, but bad for long-term planning … you can’t rely on that goodwill forever’ (strategic decision maker 044).
Discussion
The responses from participants demonstrate the challenges associated with delivering frontline health care services at times of heightened flood risk. Following an event, it is often only the immediate, traumatic health impacts associated with flooding that are recorded. This study contributes to the limited evidence surrounding health care system disruption by revealing the wider system impacts and capacity issues. Appropriate methodologies for measurement, surveillance and evaluation are required to produce further insights that can be applied to flood risk management and other environmental hazards.
The magnitude of the December 2013 surge is comparable to the 1953 event; however, advances in flood defences and forecasting served to minimize impacts. Nonetheless, breaching and overtopping of flood defences led to disruption of the health service. It is clear that despite the impacts being significantly lower than the reasonable worst-case scenario (Table 1), the 2013 event tested the resilience and capacity of the health care sector, indicating inadequate preparedness to respond to a future North Sea event whilst minimizing disruption to day-to-day services.
Based upon the findings of this research, the lack of preparedness is due to insufficient appreciation of flood risks and poor understanding of the impact of flood damage and disruption, particularly at the frontline of health care services. Extreme weather events often present an opportunity to reflect upon readiness and increase resilience through experience and learning. Implementation of the lessons learnt through Exercise Lazarus, carried out one month before the December event, appears to have been limited due to the short time between the exercise and flood event. The tendency to work in silos hindered the development of working partnerships and business continuity planning, undermining cross-system resilience. Furthermore, governance, oversight and the development of coherent strategies were challenged by fragmentation of health services. Greater multiagency linking of planning assumptions to preparedness and resilience measures is required to ensure long-term behavioural change is established and ensure the goodwill described by NHS staff is not relied upon in future. Ongoing research is required to monitor the preparedness and resilience of health care systems.
Ascertaining vulnerability to the health consequences of flooding is a complex26 process and is determined by factors beyond event magnitude (for example, social circumstances). This study has highlighted the difficulties associated with classifying vulnerability in the context of flooding risk and the challenges of communicating the risk to marginalized groups.27 With a growing, ageing population and a projected increase in complex health care being delivered at home, the identification of hidden, vulnerable populations is an urgent priority.
The creation of flood vulnerability criteria may aid future flood management, but the result is likely to identify hundreds if not thousands of individuals. Further work is required to develop a more sensitive search that considers unmet health and social care needs. With responsibility for contacting vulnerable individuals in Lincolnshire moving to individual health care services, individuals are likely to be contacted several times; this has been known to cause frustration in previous flood incidents.
Vulnerability to flooding is increasing due to population growth, land use, demographic change and increasing levels of poor health which impact on the ability of individuals, communities and services to respond to an emergency. Emerging vulnerable populations have also been identified. With an increasing prevalence of obesity in the UK, the evacuation challenges presented here should be considered for future flood planning and practice. Furthermore, bed capacity across the whole health care system was tested, particularly in community hospital settings, when people with complex health care were evacuated from their home and placed in a health care bed. Cases of refusal to evacuate take considerable time and resourcing to address during the emergency response phase. In these cases, this study highlights the need for clinical advice in accordance with the Mental Capacity Act (2005) that ensures individuals have an understanding of the potential implications whilst balancing the rights of the patient and risk to frontline responders.
This study supports the findings of other studies on medication disruption during evacuation28 but has also identified difficulties tracking preexisting patients and sourcing medication. The provision of psychological and pharmaceutical support at evacuation centres requires clarification. Mutual aid arrangements between health care providers need to reconsider the potential geographical scale of an event. In the event of another 1953-type surge, several LRFs are likely to be affected, therefore increasing the demand on external assistance and equipment.
This work illustrates the important role of the voluntary sector in supporting the health care sector during times of high-impact weather. Voluntary sector organizations should therefore be included in pre-event incident planning and exercising. The development of a questionnaire for door-to-door knocking is an example of a health needs assessment that could inform public health interventions during an emergency response and aid understanding of flood-related health impacts and effective interventions. Difficulties with insurance and insurance claims are a recognized secondary stressor that influences the psychological morbidity associated with flooding.29,30 The early engagement of the insurance sector in flood response should therefore be encouraged.
This research provides insight and learning on the impacts and disruption associated with flooding that may be applicable to other high-impact weather events (for example, heatwaves) and to other regions along the east coast of England and those international health systems around the North Sea Basin that share common functions and goals. The results of this research are unlikely to be unique to Lincolnshire, and further work is required to ascertain the scalability and its applicability to other regions.
Limitations
Several limitations for this study must be recognized. Interviews were conducted more than two years after the event, thereby introducing recall, recruitment and interviewer bias. The relatively low response rate from frontline health care providers introduces a sampling bias that potentially inhibits the scalability of the study.
Conclusion
This study has demonstrated the difficulties experienced by health care services in Boston in responding to the 2013 coastal flood. Flooding and coastal change risk are considered one of the top six interrelated climate change risks for the UK, and analysis suggests that 0.5 to 1 m of sea level rise could make some 200 km of coastal flood defences in England highly vulnerable to failure in storm conditions,2,6 indicating the scale of greater preparedness required to protect health in light of a changing climate. Health care service commissioners and regional strategic decision makers should assure themselves that local service managers are registered to directly receive high-impact weather alerts and have completed the learning resources on high-impact weather available. Despite increasing fragmentation of health services in England, greater vertical and horizontal communication is required across stakeholders including non-health partners.
The considerable scale of health care disruption in December 2013 occurred despite only a small number of health care assets being directly flooded and the timing of the surge outside normal working hours. Improved recording of flood impacts and disruption is required,14 and the emergency planning community should ensure that multiagency exercises contain a realistic portrayal of capacity within the health sector. The creation of a new exercise that accurately reflects the health care disruption documented in this study should be considered.
The December 2013 east coast surge was the first significant flood event since the introduction of new roles and responsibilities associated with the Health and Social Care Act (2012). Nonetheless, measures and efforts to increase preparedness in the health care system need to be proportionate to the exposure of the system to weather-related hazards. More work is required to increase the climate resilience of the health care sector, particularly when climate change is set to increase the risk of weather-related impacts.
Acknowledgements
The authors wish to thank the stakeholders that participated in the research.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
The study was submitted to the Lincolnshire Local Health Resilience Partnership for comments. Ethical approval was granted by the PHE Research Ethics and Governance Group (R&D 257), the Observational/Interventions Research Ethics Committee, London School of Hygiene and Tropical Medicine (Reference 10610) and the NHS Research and Innovation Department, Lincolnshire Community Health Services (LCHS Permission).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research was part-funded by the National Institute for Health Research (NIHR) Health Protection Research Unit in Environmental Change and Health at the London School of Hygiene and Tropical Medicine in partnership with PHE and in collaboration with the University of Exeter. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care or PHE.
References
- 1.Desai B, Maskrey A, Peduzzi P, et al. Making development sustainable: the future of disaster risk management, global assessment report on disaster risk reduction. Switzerland: United Nations Office for Disaster Risk Reduction, 2015. [Google Scholar]
- 2.Kovats RS, Osborn D. UK climate change risk assessment evidence report: chapter 5, people and the built environment. London: Adaptation Sub-Committee of the Committee on Climate Change, 2016. [Google Scholar]
- 3.Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet 2009; 373: 1693–1733. [DOI] [PubMed] [Google Scholar]
- 4.Mayhew S, Belle SV, Hammer M. Are we ready to build health systems that consider the climate? J Health Serv Res Policy 2014; 19: 124–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Woodward A, Smith KR, Campbell-Lendrum D, et al. Climate change and health: on the latest IPCC report. Lancet 2014; 383: 1185–1189. [DOI] [PubMed] [Google Scholar]
- 6.Sayers PB, Horritt MS, Penning-Rowsell E, et al. Climate change risk assessment 2017: projections of future flood risk in the UK. Sayers and partners LLP report for the committee on climate change. London, UK: Committee on Climate Change UK, 2015. [Google Scholar]
- 7.World Health Organization. Operational framework for building resilience health systems. Geneva, Switzerland: World Health Organization, 2015. [Google Scholar]
- 8.World Health Organization. Floods: climate change and adaptation strategies for human health. Report on a WHO meeting. London, UK: World Health Organization, Regional Office for Europe, 2002. [Google Scholar]
- 9.Roccaforte JD, Cushman JG. Disaster preparedness, triage, and surge capacity for hospital definitive care areas: optimizing outcomes when demands exceed resources. Anesthesiol Clin 2007; 25: 161–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edwards JR, Peterson KD, Andrus ML, et al. National Healthcare Safety Network (NHSN) report, data summary for 2006. Am J Infect Control 2007; 35: 290–301. [DOI] [PubMed] [Google Scholar]
- 11.Meusel D, Kirch W. Lessons to be learned from the 2002 floods in Dresden, Germany In: Wilhelm K, Menne B, Bertollini R. (eds) Extreme weather events and public health responses. Berlin Heidelberg: Springer, 2005, pp. 175–183. [Google Scholar]
- 12.HM Government. National flood resilience review. Report. UK: HM Government, 2016. [Google Scholar]
- 13.Binder L. Climate change and watershed planning in Washington State. J Am Water Resour Assoc 2006; 42: 915–926. [Google Scholar]
- 14.Landeg O, Lawson J. Effective flood resilience in health providers: flooding at a major NHS Blood and Transplant facility. Chem Hazards Poisons Rep 2014; 24: 88–91. [Google Scholar]
- 15.Klinger C, Landeg O, Murray V. Power outages, extreme events and health: a systematic review of the literature from 2011-2012. PLOS Curr Dis 2014; 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adaptation Sub-Committee Progress Report. Managing climate risks to well-being and the economy. London: Committee on Climate Change, 2014. [Google Scholar]
- 17.UK Climate Impacts Programme. UKCP18, http://ukclimateprojections.metoffice.gov.uk/ (2018, accessed 26 November 2018).
- 18.Pitt M. The Pitt review: learning lessons from the 2007 floods. Report, Cabinet Office, London, 2008, June 2008.
- 19.HM Government. The National Adaptation Programme: making the country resilient to a changing climate. Report, HM Government, London, 2013, Published 19 July 2018. [Google Scholar]
- 20.Environment, Food and Rural Affairs Committee. Winter floods 2013-14. London: House of Commons First Report of Session 2014-15, 2014. [Google Scholar]
- 21.Met Office. 1953 east coast flood – 60 years on, http://www.metoffice.gov.uk/news/in-depth/1953-east-coast-flood (2016, accessed 18 April 2016).
- 22.Lincolnshire Resilience Forum. The east coast Tidal Surge, 5th December 2013 Lincolnshire Resilience Forum’s Response & Recovery ‘After Action’ Report, Lincolnshire County Council, Lincolnshire, 20 March 2014.
- 23.Bennett K. Interviews and focus groups In: Shurmer-Smith P. (ed) Doing cultural geography. London: Sage, 2002, pp. 151–164. [Google Scholar]
- 24.Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine Publishing Company, 1967. [Google Scholar]
- 25.Gibbs GR. Thematic coding and categorizing, analyzing qualitative data. London: Sage Publications Ltd, 2007. [Google Scholar]
- 26.Lowe D, Ebi KL, Forsberg B. Factors increasing vulnerability to health effects before, during and after floods. IJERPH 2013; 10: 7015–7067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menne B, Murray V. Floods in the WHO European region: health effects and their prevention. Copenhagen: World Health Organization, 2013. [Google Scholar]
- 28.Ochi S, Hodgson S, Landeg O, et al. Medication supply for people evacuated during disasters. J Evid Based Med 2015; 8: 39–41. [DOI] [PubMed] [Google Scholar]
- 29.Lock S, Rubin GJ, Murray V, et al. Secondary stressors and extreme events and disasters: a systematic review of primary research from 2010-2011. PLOS Curr Dis 2012; 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waite TD, Chaintarli K, Beck CR, et al. The English national cohort study of flooding and health: cross-sectional analysis of mental health outcomes at year one. BMC Public Health 2017; 17: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]