Abstract
Pyogenic granuloma (PG) is a benign lesion, with a female predilection, commonly associated with local irritation or trauma. We report an unusual, destructive case of PG, displaying excessive loss of blood and destruction of alveolar bone leading to the loss of maxillary anterior teeth in an 18-year-old female, compromising function and esthetics. The incisional and excisional biopsy specimen of this recurrent lesion obtained during a 5-year span was studied, which revealed an increase in vascularity and extensive proliferation of endothelial cells admixed with varying degree of inflammatory cell infiltrate. The clinical, radiographic, and histopathological diagnostic tools enabled to precisely diagnose the lesion as an aggressive variant of PG, distinguishing it from other vascular neoplasms. No recurrence has been noted during a 5-year follow-up. The clinicians should be aware of the aggressive and destructive clinical behavior of PG to avoid the inadvertent treatment of this reactive lesion.
Keywords: Aggressive, pyogenic granuloma, recurrent, vascular neoplasm
INTRODUCTION
Pyogenic granuloma (PG) is the most common nonneoplastic tumor-like growth of gingiva occurring more commonly during the second decade of life with a female predilection.[1] It is a type of a reactive hyperplastic lesion owing to various local and systemic factors. Although benign and reactive in nature, its aggressive behavior may simulate a vascular neoplasm, thus becoming a diagnostic dilemma.[1] Here, we report a case of PG with multiple recurrences, with the second recurrence displaying features that mimicked a vascular neoplasm. We also add a note on the differential diagnosis. Our purpose is to introduce the clinicians to the deceptive behavior of PG which is otherwise considered to be a mere benign, reactive, hyperplastic lesion. It is of paramount importance to recognize the local and systemic etiological factors and to be aware of such a deceiving presentation, so as to avoid aggressive and inadvertent treatment of the lesion.
CASE REPORT
In 2009, a 13-year-old female patient presented with a swelling in the upper front tooth region of 5-month duration with a history of bleeding from the gums on brushing. The patient gave a history of trauma 5 years back in the concerned region, owing to a fall while playing. On examination, the lesion was pedunculated, measuring 1 cm × 1.5 cm, with well-defined margins located in the maxillary labial gingiva with respect to 11 and 21. The lesion was clinically and histopathologically diagnosed as PG [Figures 1-3]. Within 12 days, the patient reported with a well-defined, pedunculated growth of 2 cm × 3 cm, in the palatal region of 11 and 21 which bled profusely during excision. The lesion was again clinically and histopathologically confirmed to be a PG. The patient reported after 5 years in May 2014 with a swelling and mobility of maxillary anterior teeth. The lesion appeared ulcerated and fiery red, extending on the labial and palatal gingiva of 12–23 with diffuse margins appearing more aggressive and destructive. The lesion was soft and nontender [Figure 1a and b]. 11 and 21 were Grade II and Grade III mobile, respectively.
Figure 1.
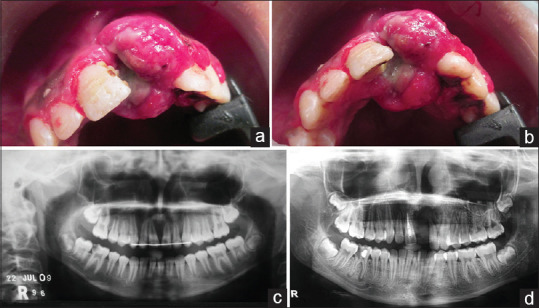
(a and b) Show a diffuse bright red lesion with a lobulated surface is noted in the labial and palatal aspect extending from 11 to 23 with ill-defined margins; (c) In the initial presentation, the orthopantomography shows a well-defined radiolucency in the interdental region of 11, 21; (d) In the second recurrence, the orthopantomography shows ill-defined radiolucency in the interradicular area extending into the alveolus and palatal region from 11 to 22
Figure 3.
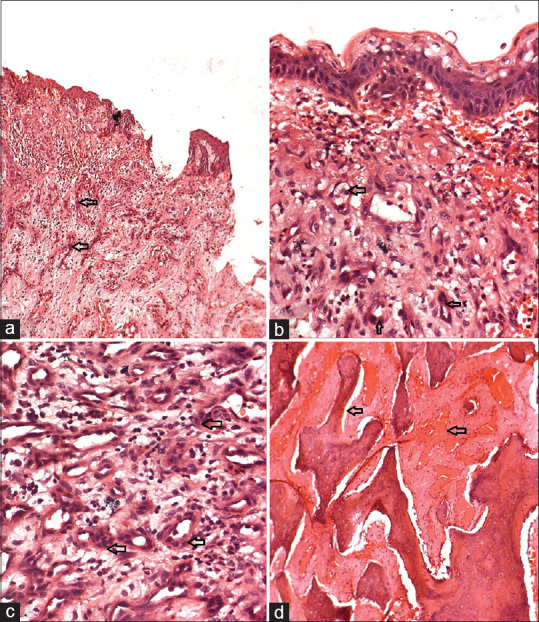
Second recurrence- (a-c) show the discontinuous oral epithelium with the adjacent stroma showing numerous capillaries lined with plump endothelial cell proliferation and lymphocytic infiltration; (a: H and E stains, low-magnification view ×10; b and c: H and E, high-magnification views ×40); (d) The decalcified section of the bony trabeculae with dilated blood vessels. (H and E, high-magnification views ×40)
The orthopantomography revealed bone loss in the anterior maxillary labial and palatal region [Figure 1c and d]. Excessive and uncontrolled bleeding was noted on extracting 21 and the patient was transfused with five units of blood. A thorough hematological examination revealed a transient and abnormal bleeding profile with a significant increase in the bleeding time, clotting time and prothrombin time and was managed with Vitamin K administration. No other significant medical history was noted. The lesion was excised and curetted under general anesthesia, and subsequently 11, 22 and 23 were extracted. The histopathological examination revealed an overlying ulcerated epithelium, with the underlying cellular stroma, displaying numerous capillaries of varying sizes lined by the proliferating endothelial cells and diffuse infiltration of chronic inflammatory cells. The decalcified sections of the alveolar bone also displayed numerous dilated blood vessels indicating the extent of the lesion. On comparing the histopathology of the three episodes, an increase in vascularity was noted. In the first recurrence, the vascular channels extended until the stalk of the lesion. The second recurrence showed similar features, but the cellularity and the vascularity of the lesion had increased enormously in comparison to the first two episodes.
The histopathological examination showed no features of pleomorphism or atypical mitotic figures, thus aiding in confirming the lesion to be a PG [Figures 2 and 3]. The patient was administered with intralesional corticosteroids. The follow-up revealed a significant loss of soft tissue and alveolar bone [Figure 4]. The extracted teeth have been replaced with a fixed prosthesis. The patient is currently under a close follow-up for 5 years and no recurrence has been noted.
Figure 2.
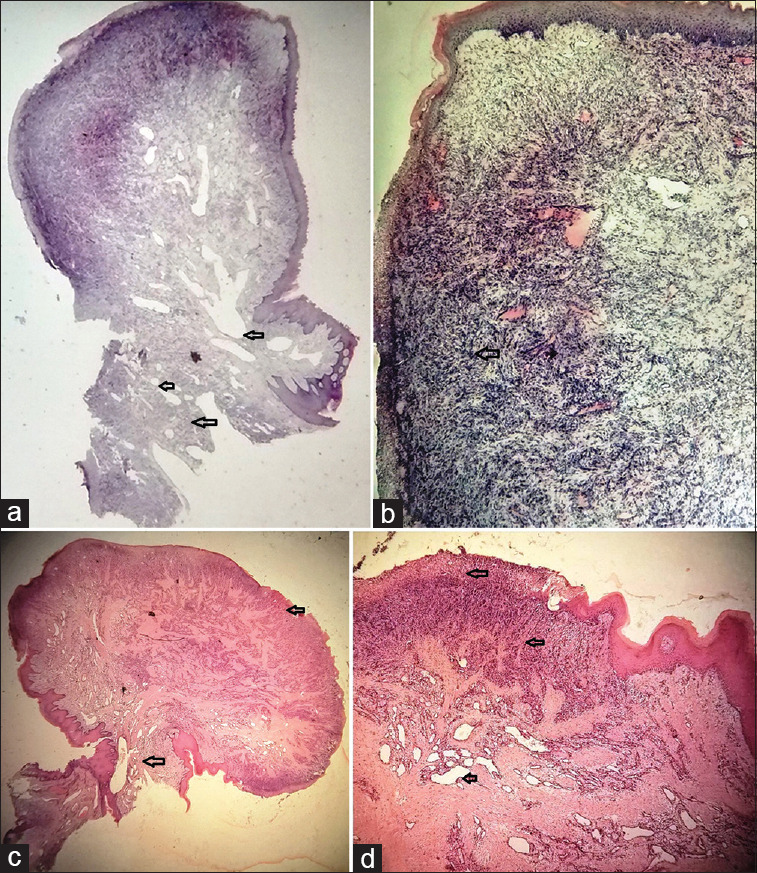
(a and b) Initial presentation showing a pedunculated mass with an ulcerated epithelium and stroma is chronically inflamed, cellular, vascular with endothelial cell proliferation. (H and E, low-magnification views ×1.25 and ×10); (c and d) first recurrence showing a pedunculated growth with surface ulceration and the vascularity extending till the stalk of the lesion. Note the increase in the size and the vascularity of the lesion. (H and E, low-magnification views ×1.25 and ×10)
Figure 4.
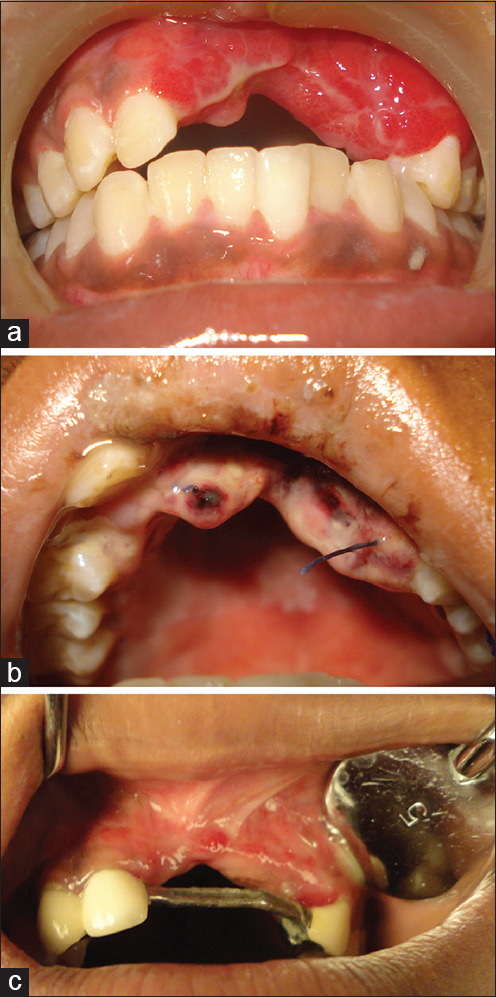
(a) Followups showing wellhealed lesions displaying loss of alveolar bone and soft tissue; (b) and erythematous lesion in the second followup. (c) The missing teeth are replaced with a fixed prosthesis
DISCUSSION
PG is an inflammatory reactive lesion developing in response to chronic, recurring tissue injury that stimulates an exhilarated tissue repair response.[1,2]
The lesion presents as a painless, pedunculated/sessile polypoidal mass or as an ulcerative growth with predilection for the maxillary labial gingiva, less commonly occurring on lips, tongue, and buccal mucosa.[1,2] In the present case, the labial and palatal aspects of the anterior maxillary gingiva were involved, displaying rapid growth, excessive bleeding, and significant bone loss.
Females are more commonly affected during the second decade of life due to vascular effects of hormones.[2] In the present case, the patient was in the pubertal age when she first reported with the lesion and the first recurrence. A surge in the estrogens and progesterone is noted during puberty, and gingiva, being the target tissue, shows an increase in the gingival receptors to these hormones. In addition to the hormonal changes, a drastic change in the subgingival microbiota has been noted. All these factors synergistically exaggerate the preexisting gingival inflammation.
In about 3% of the cases, PG grows to enormous sizes and has a high tendency to recur with extensive and fatal blood loss, alveolar bone resorption leading to mobility of the associated teeth. This aggressive clinical behavior in conjunction with the histopathological features displaying excessive proliferation of the vasculature deceptively appears like a malignant vascular tumor. These findings are similar to the case reports that we reviewed.[3,4,5,6,7]
On comparing the histopathology of all the three episodes in the present case, a gradual increase in vascularity and its extent was noted. The vascularity had enhanced enormously with the increase in the number of capillaries and proliferation of plump endothelial cells which were seen extending up to the stalk of the lesion and the alveolar bone with varying degree of chronic inflammatory cell infiltration. The size of the lesion had increased by two-folds on the subsequent recurrences. All the above-stated histological features, recurrence of the lesion, and the aggressive clinical behavior on the second recurrence, characterized by the rapidly enlarging growth, excessive and spontaneous bleeding from the lesion and the loss of bone, and the consequent mobility of tooth, persuaded us to consider a malignant vascular neoplasm in the differential diagnosis. Despite the absence of features such as pleomorphism and mitosis, which are more suggestive of a malignancy, and the literary evidence of reactive lesions occasionally displaying aggressive features, it has aided us in ruling out a malignant vascular neoplasm, thus concluding the case as PG.
The local and systemic factors trigger the release of various endogenous substances such as angiogenic factors from tumor cells which lead to a disturbance in the vascular system of the affected area. In the present case, the possible etiopathogenesis has been hypothesized as per Figure 5.
Figure 5.
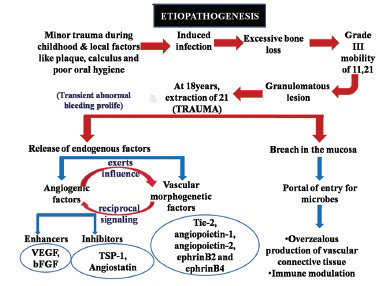
The possible etiopathogenesis of the present case wherein, trauma, local and systemic factors, and microorganisms play a vital role. (VEGF – Vascular endothelial growth factor; bFGF – Basic fibroblast growth factor; TSP-1 – Thrombospondin 1; Tie-2 – Tyrosine kinase with immunoglobulin-like and EGF-like domains-2)
Various angiogenic enhancers, inhibitors and vascular morphogenic factors have been shown to be upregulated in PG compared to healthy gingival.[1] The expression of inducible nitric oxide synthase and a low apoptotic rate expression of the Bax/Bcl-2 proteins have also been noted. Immunohistochemical markers for endothelial cells (CD31 and 34) do not aid in distinguishing PG from vascular neoplasms. PG could have such a deceptive presentation both clinically and histopathologically, and the closest differential diagnosis is given in Table 1.[8,9]
Table 1.
Describes the differential diagnosis of the present case
| Lesion | Clinical features | Histo-pathological features | Differentiating features |
|---|---|---|---|
| Angiosarcoma | Mimics aggressive pyogenic granuloma | Made of disorganized proliferation of endothelial cells Interconnecting vascular channels |
Occurs in older age group Endothelial cells are atypical and polyhedral Vascular channels invade the deeper connective tissue |
| Capillary hemangioma | Multinodular bluish red in color | Proliferation of capillaries | More common in children Endothelial cells are more plump No acute inflammatory cells |
| Epitheloid hemangioendothelioma | Exophytic, ulcerated, painless red mass | Proliferation of epitheloid like endothelial cells | Rare in the oral cavity More common in submandibular region Intracytoplasmic vacuoles in epitheloid cells |
| Kaposi Sarcoma | Raised nodule with bright red appearance | Atypical vascular channels, extravasated RBCs, inflammatory cells | HIV associated lesion Occurs in the palate Vascular clefts, intracellular hyaline globules |
| Bacillary Angiomatosis | Raised, nodular lesion appearing bright red. Occasional alveolar bone loss |
Proliferating capillaries arranged around ectatic vessels | HIV associated lesion Epitheloid endothelial cells noted Eosinophilic aggregates containing fibrin and bacilli |
PG is treated with complete excision of the lesion down to the periosteum or periodontal ligament and removal of local irritants. Lasers, cryosurgery and intralesional cortecosteroids are the other modalities of treatment.[6] A recurrence rate of 16% has been reported and attributed to incomplete excision and failure to remove the etiology, re injury to the area; and it most commonly recurs on the gingiva, after conservative excision and during pregnancy.[1,2,10]
CONCLUSION
PG, being a reactive inflammatory benign vascular neoplasm, may sometimes have serious consequences owing to its structural characteristics and bleeding tendencies. A complete excision with curettage is necessary to avoid recurrences. A close follow-up and maintenance of oral hygiene is required. It is paramount to recognize this lesion to avoid inadvertent and aggressive treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mastammanavar D, Hunasgi S, Koneru A, Vanishree M, Surekha R, Vardendra M. Aggressive pyogenic granuloma: A case report. Int J Oral Maxillofac Pathol. 2014;5:29–32. [Google Scholar]
- 2.Mohan M, Karikal A, Bhat S, Padmaja A, Thilak G. Aggressive pyogenic granuloma causing bone erosion. A case report. Healtalk. 2012;4:12–4. [Google Scholar]
- 3.Martins-Filho PR, Piva MR, Da Silva LC, Reinheimer DM, Santos TS. Aggressive pregnancy tumor (pyogenic granuloma) with extensive alveolar bone loss mimicking a malignant tumor: Case report and review of literature. Int J Morphol. 2011;29:164–167. [Google Scholar]
- 4.Singh RK, Kaushal A, Kumar R, Pandey RK. Profusely bleeding oral pyogenic granuloma in a teenage girl. BMJ Case Rep. 2013;2013:bcr2013008583. doi: 10.1136/bcr-2013-008583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panseriya BJ, Hungund S. Pyogenic granuloma associated with periodontal abscess and bone loss – A rare case report. Contemp Clin Dent. 2011;2:240–4. doi: 10.4103/0976-237X.86478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saikhedkar R, Shrivastava S, Melkundi M, Vishwanathan V. Pyogenic Granuloma- A case report. Int J Dent Clin. 2011;3:87–8. [Google Scholar]
- 7.Verma PK, Srivastava R, Baranwal HC, Chaturvedi TP, Gautam A, Singh A. “Pyogenic granuloma – Hyperplastic lesion of the gingiva: Case reports”. Open Dent J. 2012;6:153–6. doi: 10.2174/1874210601206010153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shenoy SS, Dinkar AD. Pyogenic granuloma Associated with bone loss in an eight year old child: A case report. J Indian Soc Pedod Prev Dent. 2006;24:201–3. doi: 10.4103/0970-4388.28078. [DOI] [PubMed] [Google Scholar]
- 9.Tripathi AK, Kumar V, Saimbi CS, Sinha J. Pyogenic granuloma with alveolar bone loss. J Int Clin Dent Res Org. 2015;7:75–8. [Google Scholar]
- 10.Vaidya S, Kapoor C, Ohri N, Singh HP. Pyogenic granuloma/lobular hemangioma: A diagnostic dilemma. Int J Med Dent Sci. 2013;2:88–93. [Google Scholar]


