Abstract
Background:
Oral pyogenic granuloma is a soft-tissue lesion of the oral mucosa. This lesion has a tendency to reoccur after surgical excision.
Materials and Methods:
A total of 28 patients underwent surgical excision of pyogenic granuloma in the period from September 2014 to May 2016. Two surgical techniques were used to remove pyogenic granuloma: simple excision with root planing and modified excision with deep curettage.
Results:
Females (54%) were slightly more predominant than males (46%). The upper and lower jaws were almost equally affected by the lesion with more predilection toward the posterior region. The size of the lesion ranged from 0.5 to 3 cm in diameter with slow-growing rate. Rural residents were more affected (57%) than urban people. The lesion appears clinically as a small red mass with sessile base, and these clinical features were similar in pregnant and nonpregnant women. The recurrence rate was 14.8% and seen only in patients treated by simple excision. Histopathological feature was consistent with inflammatory hyperplastic lesion, and there was no radiographic evidence of bone resorption associated with the lesion.
Conclusion:
Modified excision with deep curettage prevents the recurrence of the lesion after 1-year follow-up.
Keywords: Clinical features, etiology, pyogenic granuloma, recurrence, surgery
INTRODUCTION
Pyogenic granuloma, which is a nonneoplastic soft-tissue lesion, occurs as a result of inflammatory reaction.[1] It is mostly affecting the gingiva and very rarely other sites of the oral cavity such as lip, tongue, and buccal mucosa.[2] Pyogenic granuloma is not considered as an appropriate term, as it does not occur as a consequence of granulomatous inflammation and does not contain pus material.[3] Previous studies suggested that soft-tissue injury due to infection was the main cause of this lesion.[4] Others, however, stated that the invasive stimuli of lowgrade intensity behind the development of pyogenic granuloma.[5,6] These include chronic irritation from dental calculus or retained roots and trauma. In addition, hormonal changes during pregnancy or puberty, and certain drugs such as cyclosporine could be the etiological factors of pyogenic granuloma.[7] Besides, certain cases of pyogenic granuloma have been reported in patients who underwent guided tissue regeneration[4] and dental implant.[8]
Pyogenic granuloma is usually seen in young adult females and most commonly occurring at the anterior gingiva of the upper jaw.[9,10] Clinically, this lesion presented as exophytic mass with smooth or ulcerative surface. Though, sometimes the lesion appears as a small erythematous papule on a pedunculated or sessile base.[11] The growing of pyogenic granuloma is slow and takes weeks to months to reach optimal size.[12] Therefore, the size of the lesion during presentation ranges from few millimeters to 4 cm in diameter.[13] Although there are many treatment modalities of pyogenic granuloma, surgical excision is still the treatment of choice to eradicate this lesion.[7] Many researches showed that there was no recurrence following such a treatment modality.[12,14] However, the recurrence of the lesion was reported and rated between 5.8% and 16% after surgery.[15,16]
The aim of this work is to study the clinicopathological aspect of pyogenic granuloma and to detect the recurrence rate after 1-year follow-up of two surgical techniques used to manage this lesion.
MATERIALS AND METHODS
Successive patients who underwent surgical excision of pyogenic granuloma in the Department of Oral Surgery, College of Dentistry, University of Babylon, during the period from September 2014 to May 2016 were studied. A consent form was taken from each patient before surgical procedure. Patients' information (age, sex, and resident) and features of the lesion (site – anterior or posterior/upper or lower jaw, size and duration of the lesion, clinical feature, and recurrence) were reported and analyzed. The etiology of the lesion whether local factors such as bad oral hygiene and occlusal trauma or systemic factors like hormonal changes as in case of puberty and pregnancy were recorded as well. A periapical view was taken for all patients to detect bone resorption.
The lesion was excised under local anesthesia for all patients. To detect the effect of surgical technique on recurrence rate of the lesion, patients were divided equally into two groups: in the first group, the excision was confined to the original lesion followed by root planing of the adjacent tooth and removal of the local causative factors, and in the second group, 2 mm of the normal adjacent tissue was excised with deep curettage until healthy bone and removal of the causative agents. For brevity, the first technique was described as simple excision with root planing and the second technique was modified excision with deep curettage. The excised specimens were kept in formaldehyde solution and sent for histopathological investigation. Patients were instructed to improve oral hygiene using toothbrushing and flossing. Topical antimicrobial agents such as metronidazole gel and chlorhexidine mouthwash were prescribed for 1 week. The treated cases were followed up for 1 year to detect any possibility of recurrence. This study was approved by the Ethical Committee of College of Dentistry.
RESULTS
A total of 28 patients with pyogenic granuloma were studied, in which 13 (46%) were male, and 15 (54%) were female. The ratio of male to female was 1:1.15. Six cases out of 15 were pregnant women. The mean age of the affected patients was 35.7(±12.5), with an age range of 11–65 years. The most frequent cases of pyogenic granuloma were seen in the age group of 30–39 years, as shown in Figure 1. Rural residents were more affected than urban people (57% and 43%). The upper and lower jaws were almost equally affected by the lesion, and the premolar–molar area of the upper and lower jaws was more predominant (36% and 64%) than the anterior part, as depicted in Table 1. Most of the cases presented clinically as a sessile lesion (72%). The size of the lesion ranged from 0.5 to 3 cm in diameter with duration ranging between 5 days and 9 months. The majority of the cases were developed as a result of bad oral hygiene (78%) and the rest due to hormonal changes during pregnancy, as shown in Table 2. After 1-year follow-up, four cases were reported with recurrence in the group treated by simple excision and root planing, whereas no cases of recurrence had been reported in patients treated by modified excision with deep curettage [Tables 1, 2 and Figures 1, 2a, b and 3a-d].
Figure 1.
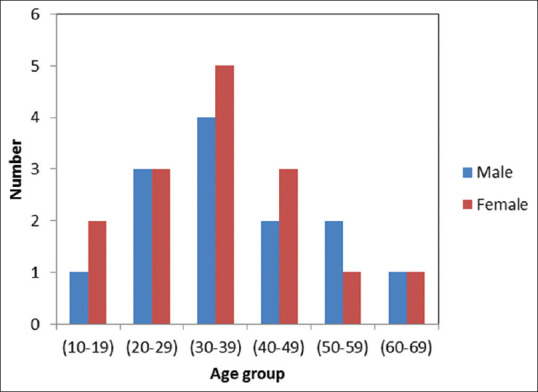
Distribution of pyogenic granuloma according to age groups
Table 1.
Distribution of the site of the lesion according to age groups
| Age group | Jaw | Region | ||
|---|---|---|---|---|
| Upper jaw | Lower jaw | Anterior | Posterior | |
| 10-19 | 2 | 1 | 1 | 2 |
| 20-29 | 2 | 4 | 2 | 4 |
| 30-39 | 5 | 4 | 4 | 5 |
| 40-49 | 3 | 2 | 3 | 2 |
| 50-59 | 1 | 2 | 0 | 3 |
| 60-69 | 1 | 1 | 0 | 2 |
| Total | 14 | 14 | 10 | 18 |
Table 2.
Distribution of clinical features, etiology, and residents according to age groups
| Age group | Clinical feature | Etiology | Residents | |||
|---|---|---|---|---|---|---|
| Sessile | Pedunculated | Local | Systemic | Rural | Urban | |
| 10-19 | 3 | 0 | 3 | 0 | 2 | 1 |
| 20-29 | 4 | 2 | 5 | 1 | 4 | 2 |
| 30-39 | 6 | 3 | 5 | 4 | 6 | 3 |
| 40-49 | 3 | 2 | 4 | 1 | 2 | 3 |
| 50-59 | 2 | 1 | 3 | 0 | 1 | 2 |
| 60-69 | 2 | 0 | 2 | 0 | 1 | 1 |
| Total | 20 | 8 | 22 | 6 | 16 | 12 |
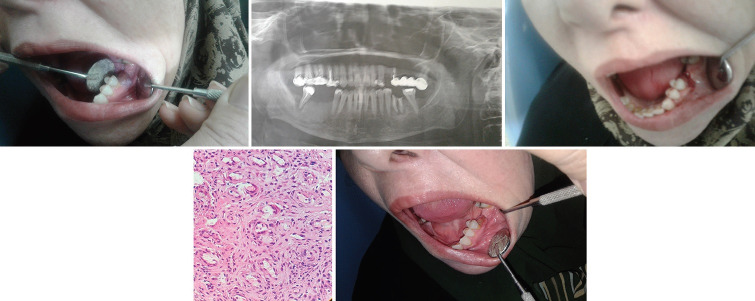
Figure 2.

(a) Preoperative view of the lesion; (b) Postoperative view
Figure 3.
(a) Preoperative view of lesion removed by simple excision; (b) Orthopantographic view of the region; (c) Postoperative view; (d) Histopathological view of the lesion; (e) Follow-up of the patient after 7 days
DISCUSSION
Oral pyogenic granuloma can be seen in all age groups from children to elderly people. The present study showed that the mean age of the affected patients with pyogenic granuloma was 35.7 years and the most affected age group was people in the fourth decade of life. These findings disagree with the results of Epivatianos et al.,[17] where the mean age was 52 years and the lesion more frequently occurred in the sixth decade of life. Other studies stated that the peak incidence of pyogenic granuloma was seen in the second, third, and fourth decades of life.[3,5,18,19]
Adult females were slightly more affected by pyogenic granuloma than males, and the ratio of male to female was 1:1.15. The outcome of this work is similar to that of other studies, and this could be associated with female sex hormone and contraceptive medications.[12,20,21] The high-level estrogen and progesterone during puberty and pregnancy deteriorate the already established gingival inflammation by increasing dilatation and proliferation of blood vessels and releasing vasoactive mediators from the damaged mast cells.[6,9,22] It is thought that the expression of angiogenic factors such as basic fibroblast growth factor and vascular endothelial growth factor can be enhanced by trauma and female sex hormones which cause the development of pyogenic granuloma.[23] In the present work, six cases were pregnant women, and the surgical excision was carried out in the second trimester. This is to avoid the side effect of surgery on pregnancy.
Both the jaws were almost equally affected by pyogenic granuloma, and the premolar–molar region was more predominant than the anterior one, particularly the labiobuccal aspect of the marginal gingiva. This is because the posterior portion is more subjected to occlusal trauma and difficult to clean during toothbrushing. These findings are in agreement with previous study[12] but disagree with that found by Al-Khateeb and Ababneh[15] where the upper jaw was more affected than the lower one with high incidence of the anterior region of the jaw.
Clinically, most cases of pyogenic granuloma presented as painless red mass tends to bleed easily upon probation and a smooth surface attached at a sessile base. A similar feature was seen by Jafarzadeh et al.[4] but disagrees with that observed by Al-Khateeb and Ababneh[15] where the lesion was ulcerated and a part of the lesion had pedunculated base. Pyogenic granuloma of short duration tends to bleed easily because of high vascularity and less collagen fibers, while mature lesion contains more collagen and less vasculature.[4] It is worth mentioning that the clinical feature of pyogenic granuloma in pregnant women was similar to that of nonpregnant women.
The role of oral hygiene and socioeconomic status (according to patient's income) of the patients in the evolution of pyogenic granuloma was obvious in the present study, as more rural residents suffered from this lesion compared to that of urban people. However, the sample size in the present work may be not enough to judge about the distribution of the lesion between rural and urban population.
The size of the lesion in this research ranged between 0.5 and 3 cm in diameter and small lesion developed within 5–20 days, whereas larger one took longer time (6–9 months). This indicates that the development of pyogenic granuloma is slow, and this phenomenon was reported by other studies.[24,25] However, other reports stated that this lesion could grow rapidly.[22,26]
There are two techniques were used to manage pyogenic granuloma in this study. In the first group, simple excision (confined to the base of the lesion) was used followed by root planing of the adjacent tooth and removal of the causative agents such as dental calculus, overhanging filling, or retained roots. In the second group, surgical excision of the lesion with 2 mm of the adjacent normal tissue with deep curettage up to healthy bone and removal of the irritants was performed. This is to detect the effect of surgical technique on recurrence rate of the lesion.
Follow-up of the treated patients indicated that there was no evidence of recurrence in patients treated by modified excision with deep curettage. In contrast, the recurrence of the lesion was seen in 4 (14.3%) who treated by simple excision with root planing. The recurrence appeared with different intervals ranging between 10 months and 1 year. Although there were no huge differences between the two groups, this indicates that removal of 2 mm from the normal tissue and deep curettage may have an influence in the prevention of recurrence of the lesion. It has been postulated that recurrence is ascribed to incomplete removal of the lesion and persistent of the causative agents.[14] Therefore, 2 mm of the adjacent normal tissue was excised to ensure complete removal of the lesion. The exposed bone was covered with iodoform gauze impregnated with white head varnish sutured to the adjacent tissue, as this technique implies healing by secondary intention.[27,28] The suture and iodoform gauze were removed after 7 days of the surgical operation. Follow-up of the patients denoted that complete healing occurred after 1–2 months of the second surgical technique. The finding of this study indicated that the modified surgical technique is not advisable in the anterior region, as the healing process took longer time in comparison to the simple excision technique.
Notably, recurrence was not observed in women who were pregnant during surgical removal of the lesion. This is despite the fact that some of them were treated by simple excision with no prophylactic removal of the normal tissues. This might be associated with the size of the lesion, as most of the cases seen in the pregnant women were small in size and ranged between 0.5 and 1.5 cm. The finding of the present work was close to that of Bugshan et al.[29] who found that the recurrence rate was 15.8%. However, the sample size should be considered when comparing this work with previous study. It is worth to mention that the recurrent cases seen in this study were associated with bad oral hygiene and not due to systemic factors.
Histopathologic examination of the excised lesion revealed pieces of rich vascular granulation tissue infiltrated with macrophages and other inflammatory cells consistent with that of pyogenic granuloma. In accordance with the study of Kamal et al.,[30] this study reveals that there was no radiographical evidence of bone resorption associated with the lesion.
CONCLUSION
Females in the fourth decade of life and rural residents were more prone to develop pyogenic granuloma. The posterior region of the upper and lower jaws, particularly labiobuccal aspect, was more affected by such a lesion. There is no difference in the clinical feature of pyogenic granuloma between pregnant and nonpregnant women. The majority of the cases occurred as a result of local factors such as deep pocket or retained roots. The size of the lesion was not exceeding 3 cm with slow-growing rate. Modified excision with deep curettage was successful to eradicate pyogenic granuloma with no recurrence after 1-year follow-up. Histopathologic investigation of the excised lesion was consistent with hyperplastic inflammatory lesion. Radiographically, there was no evidence of bone resorption associated with the lesion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Khaitan T, Sinha R, Sarkar S, Kabiraj A, Ramani D, Sharma M. Conservative approach in the management of oral pyogenic granuloma by sclerotherapy. J Indian Acad Oral Med Radiol. 2018;30:46–51. [Google Scholar]
- 2.Pandy R, Gupta R, Rawat S. Pyogenic granuloma of buccal mucosa mimicking as traumatic fibroma in pregnancy. Indian J Dent Adv. 2016;8:172. [Google Scholar]
- 3.Gonçales ES, Damante JH, Fischer Rubira CM, Taveira LA. Pyogenic granuloma on the upper lip: An unusual location. J Appl Oral Sci. 2010;18:538–41. doi: 10.1590/S1678-77572010000500019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci. 2006;48:167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 5.Amadei SU, Pereira AC, Silveira VA, Carmo ED, Scherma AP, Rosa LE. Prevalence of non-neoplastic proliferative processes in the oral cavity: A forty-year retrospective study. Dentistry clinic and research-UNITAU. 2009;1:38–42. [Google Scholar]
- 6.China AL, Souza NM, Amanajás TA, Pedreira EN. Pyogenic granuloma: Reporting of atypical case on lower lip. Rev Para Med. 2010;24:(3/4). [Google Scholar]
- 7.Rossa C, Cartagena A, Torre A. Oral pyogenic granuloma diagnosis and treatment: A series of cases. Rev Odontol Mex. 2017;21:244–52. [Google Scholar]
- 8.Kaya A, Ugurlu F, Basel B, Sener CB. Oral pyogenic granuloma associated with a dental implant treated with an Er: YAG laser: A case report. J Oral Implantol. 2015;41:720–3. doi: 10.1563/AAID-JOI-D-13-00251. [DOI] [PubMed] [Google Scholar]
- 9.Leal RM, Rodrigues AM, Mendonça AA, Chrcanovic BR. Oral pyogenic granuloma: Epidemiology of 171 cases. Rev Min Estomatol. 2004;1:13–9. [Google Scholar]
- 10.Gordón-Núñez MA, de Vasconcelos Carvalho M, Benevenuto TG, Lopes MF, Silva LM, Galvão HC. Oral pyogenic granuloma: A retrospective analysis of 293 cases in a Brazilian population. J Oral Maxillofac Surg. 2010;68:2185–8. doi: 10.1016/j.joms.2009.07.070. [DOI] [PubMed] [Google Scholar]
- 11.Parajuli R, Maharjan S. Unusual presentation of oral pyogenic granulomas: A review of two cases. Clin Case Rep. 2018;6:690–3. doi: 10.1002/ccr3.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaya A, Kaya B. Oral pyogenic granuloma Review of 10 cases. Indian J Med Res Pharm Sci. 2015:2. [Google Scholar]
- 13.Newman MG, Takei H, Carranza FA. Textbook of Carranza's Clinical Periodontology. 10th ed. The Netherlands: Elsevier publication; 2006. pp. 176–7. [Google Scholar]
- 14.Tiwari S, Neelakanti A, Sathyanarayana S. An innovative and less invasive management of recurrent pyogenic granuloma in the esthetic zone: A case report with 18-month follow-up. J Indian Soc Periodontol. 2017;21:241–4. doi: 10.4103/jisp.jisp_61_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: A retrospective analysis of 108 cases. J Oral Maxillofac Surg. 2003;61:1285–8. doi: 10.1016/s0278-2391(03)00729-8. [DOI] [PubMed] [Google Scholar]
- 16.Hasanoglu Erbasar GN, Senguven B, Gultekin SE, Cetiner S. Management of a recurrent pyogenic granuloma of the hard palate with diode laser: A case report. J Lasers Med Sci. 2016;7:56–61. doi: 10.15171/jlms.2016.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epivatianos A, Antoniades D, Zaraboukas T, Zairi E, Poulopoulos A, Kiziridou A, et al. Pyogenic granuloma of the oral cavity: Comparative study of its clinicopathological and immunohistochemical features. Pathol Int. 2005;55:391–7. doi: 10.1111/j.1440-1827.2005.01843.x. [DOI] [PubMed] [Google Scholar]
- 18.Abdulai A, Nuamah I, Baddoo H, Gyasi R. Oral pyogenic granuloma in Ghanaians: A review of cases. Int Med Biomed Res. 2013;2:173–8. [Google Scholar]
- 19.Saravana GH. Oral pyogenic granuloma: A review of 137 cases. Br J Oral Maxillofac Surg. 2009;47:318–99. doi: 10.1016/j.bjoms.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Lin RL, Janniger CK. Pyogenic granuloma. Cutis. 2004;74:229–33. [PubMed] [Google Scholar]
- 21.Shenoy SS, Dinkar AD. Pyogenic granuloma associated with bone loss in an eight year old child: A case report. J Indian Soc Pedod Prev Dent. 2006;24:201–3. doi: 10.4103/0970-4388.28078. [DOI] [PubMed] [Google Scholar]
- 22.Reyes A, Pedron IG, Utumi ER, Aburad A, Soares MS. Pyogenic granuloma: Focus on periodontal disease as an etiological factor. Clí Pesq Odontol Curitiba. 2008;4:29–33. [Google Scholar]
- 23.Pauly G, Kashyap R, Kini R, Rao K, Bhandarka G, Surashmi P. The age old misnomer: Oral pyogenic granuloma-a case report. Mod App Dent Oral Health care. 2018:3. [Google Scholar]
- 24.Regezi JA, Sciubba JJ, Jordan RC. Clinical Pathologic Correlations: Text Book of Oral Pathology. 4th ed. Philadelphia: WB Saunders; 2003. pp. 115–6. [Google Scholar]
- 25.Vasconcelos MG, Vasconcelos RG, Mafra RP, Guedes Queiroz LM. Pyogenic granuloma on the lower lip: An unusual location. Stomatos. 2012;18:34–8. [Google Scholar]
- 26.Gomes RA, Duarte DA. Pyogenic granuloma in a pediatric patient: literature review and clinical case report. Odontol Clí Científ Recife. 2008;7:75–80. [Google Scholar]
- 27.Caballero L, Aguilar M. Oral pyogenic granuloma: Treatment. Cient Dent. 2012;9:33–40. [Google Scholar]
- 28.Gomes SR, Shakir QJ, Thaker PV, Tavadia JK. Pyogenic granuloma of the gingiva: A misnomer? A case report and review of literature. J Indian Soc Periodontol. 2013;17:514–9. doi: 10.4103/0972-124X.118327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bugshan A, Patel H, Garber K, Meiller TF. Alternative therapeutic approach in the treatment of oral pyogenic granuloma. Case Rep Oncol. 2015;8:493–7. doi: 10.1159/000441839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol. 2012;16:79–82. doi: 10.4103/0973-029X.92978. [DOI] [PMC free article] [PubMed] [Google Scholar]