Abstract
Monitoring the implementation and impact of routine antenatal care (ANC), as described in the new World Health Organization (WHO) ANC model, requires indicators that go beyond the previously used global benchmark indicator of four or more ANC visits. To enable consistent monitoring of ANC content and care processes and to provide guidance to countries and health facilities, WHO developed an ANC monitoring framework. This framework builds on a conceptual framework for quality ANC and a scoping review of ANC indicators that mapped existing indicators related to recommendations in the new WHO ANC model. Based on the scoping review and following an iterative and consultative process, we developed a monitoring framework consisting of core indicators recommended for monitoring ANC recommendations in all settings, as well as a menu of additional measures. Finally, a research agenda highlights areas where ANC recommendations exist, but measures require further development. Nine core indicators can already be monitored globally and/or nationally, depending on the preferred data sources. Two core indicators (experience of care, ultrasound scan before 24 weeks) are included as placeholders requiring priority by the research agenda. Six context-specific indicators are appropriate for national and subnational monitoring in various settings based on specific guidance. Thirty-five additional indicators may be relevant and desirable for monitoring, depending on programme priorities. Monitoring implementation of the new WHO ANC model and the outcomes of routine ANC require greater attention to the measurement of ANC content and care processes as well as women’s experience of ANC.
Keywords: maternal health, obstetrics, public health
Summary box.
-
The monitoring framework for antenatal care (ANC) is composed of four key components:
A list of required ANC measures for monitoring the new World Health Organization (WHO) ANC model.
A menu of existing ANC indicators to be used in global, national and/or subnational monitoring.
A monitoring framework for interventions and strategies aimed at improving the delivery and experience of routine ANC.
A research agenda highlighting areas where ANC recommendations exist, but indicators still need to be developed.
To assist countries in monitoring implementation of the new WHO ANC model, nine core indicators are proposed that can be monitored globally and/or nationally, depending on the preferred data sources, and six context-specific indicators are appropriate for national and subnational monitoring in various settings based on specific guidance.
Most indicators are currently collected from population-based household surveys; however, as health information systems improve, we recommend collecting the majority of these indicators from routine health management information systems.
Monitoring implementation of the new WHO ANC model and the outcomes of routine ANC require greater attention to the measurement of ANC content and care processes, as well as adolescent girls’ and women’s experiences of ANC.
Introduction
In 2016, the World Health Organization (WHO) released comprehensive recommendations on antenatal care (ANC) for a positive pregnancy experience. The new model for delivering ANC is a goal-oriented approach to delivering evidence-based interventions focusing on the quality and content of care, which includes both clinical care and the adolescent girl’s or woman’s experience of care.1 In contrast to the basic or four-visit focused ANC model that the new WHO ANC model replaces, the new model recommends interventions to be delivered at a minimum of eight ANC contacts.1 By using the word ‘contact’ rather than ‘visit’, the new WHO ANC model promotes a more active connection between ANC clients and their healthcare providers. To provide guidance to countries and health facilities and to enable consistent monitoring and assessing progress towards implementation of the new model, a monitoring framework is required. Monitoring the implementation and impact of routine ANC, as described in the guideline, requires monitoring ANC content and care processes that are not captured in the global benchmark indicator of four or more ANC visits.2 Although monitoring the number of visits or contacts remains important, the new WHO ANC model’s focus is on the quality and content of the care received.
To enable the monitoring of recommendations in the new WHO ANC model, we first customised WHO’s conceptual framework for quality maternal and newborn healthcare to address three dimensions of quality ANC: (1) health systems, (2) content of care and (3) women’s experience of care. These dimensions influence antenatal outcomes and experiences at the individual and facility levels.3 Health system factors, such as service delivery models and community engagement, impact the accessibility and quality of the ANC processes. Quality of care is dependent on the provision and content of ANC, as well as women’s experiences of ANC, which rely on the availability of the health provider and physical resources.4 Content of care includes ANC interventions related to maternal and foetal assessment and management, nutrition, infectious disease testing and management, and counselling and information sharing. Women’s experience of ANC is currently limited to the assessment and management of physical symptoms, based on the recent ANC guideline. We plan to expand this limited concept of experience of care so that it more closely aligns with the WHO quality of care framework in which effective communication, respect and dignity, and emotional support are included within women’s experience of care.5
The conceptual framework for quality ANC can help assess the characteristics required to deliver quality ANC; however, monitoring implementation of the new WHO ANC model and the outcomes of routine ANC requires greater attention to the measurement of ANC content and care processes, as well as women’s experience of ANC. The purpose of this paper was to describe the process of developing the monitoring framework for the new WHO ANC model and to provide guidance on recommended indicators and data collection platforms.
The ANC monitoring framework builds on the conceptual framework for quality ANC and a scoping review focusing on indicators for routine ANC.3 A scoping exercise first mapped existing indicators for recommended interventions in the WHO ANC model. Based on the scoping review, and following an iterative and consultative process, we developed a monitoring framework consisting of core indicators for monitoring the recommended ANC interventions in all settings, as well as a menu of additional measures for context-specific recommendations. Finally, we present a research agenda highlighting areas where ANC recommendations exist, but measures require further development and validation. The monitoring framework aligns with other WHO recommendations pertinent to improving communication and support for women and families during pregnancy, as well as global monitoring efforts undertaken by initiatives such as ending preventable maternal mortality.6 7
Step 1: measures for ANC recommendations
To identify existing ANC measures and gaps where new measures are needed, we conducted a scoping review of indicators for routine measurement of implementation of the new WHO ANC model. Searches were conducted in four databases (PubMed, ISI Web of Science, ScienceDirect and Popline) and five websites (WHO, MEASURE Evaluation, The Demographic and Health Survey (DHS) Programme, UNICEF Multiple Indicator Cluster Surveys (MICS) and Countdown to 2030), following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow approach for searches and application of inclusion/exclusion criteria. The resulting measures came from a variety of sources, including household surveys, research studies and other monitoring frameworks. Data were extracted on measure information, methodology, methodological work and implementation. This scoping review focused specifically on the new WHO ANC recommendations.1 The search strategy did not include indicators for recommendations from other relevant guidelines. We acknowledge this limitation and recognise that additional guidelines include recommendations relevant to ANC for a positive pregnancy experience.1 6 8 While it may appear that indicators for certain areas of ANC are missing from the scoping review, they are present in other monitoring plans.9
The scoping review revealed 58 items describing 46 existing ANC measures that align with the new WHO ANC model and good clinical practices for ANC.3 Among the 42 WHO-recommended ANC interventions and four good clinical practices included in the scoping review, 14 recommendations and three established good clinical practices could be measured immediately using existing measures (table 1). Good clinical practices, while not specifically recommended in the 2016 guideline, are considered to be essential components of ANC.1 As such, they should be implemented as part of the new WHO ANC model. Therefore, four key good clinical practices of ANC were included in the scoping review: counselling on birth preparedness and complication readiness, counselling on family planning, monitoring of foetal heart rate and monitoring of blood pressure.
Table 1.
ANC areas for measurement by monitoring domain based on ANC recommendations
| Monitoring domain | Topic for measurement | Link to conceptual framework | WHO ANC recommendation (2016a) | Measure status | |
| Exists | Does not exist | ||||
| Inputs | Policy on task shifting for ANC (counselling and provision of selected interventions) | Health system | E.5.1 and E.5.2 | X | |
| Health worker density and distribution* | Health system | E.6 | X | ||
| Process | Health units with at least one service provider trained to care for and refer sexual and gender-based violence survivors* | Health system | B.1.3 | X | |
| Pregnant women carrying their own case notes | Health system | E.1 | X | ||
| Facilitated participatory learning and action cycles with women’s groups to improve maternal and newborn health* | Health system | E.4.1 | X | ||
| Intervention packages that include interpersonal communication and community mobilisation* | Health system | E.4.2 | X | ||
| Outputs | Availability of balanced energy and protein dietary supplementation | Content of care | A.1.3 | X | |
| On-site haemoglobin testing for anaemia* | Content of care | B.1.1 | X | ||
| On-site testing for asymptomatic bacteriuria* | Content of care | B.1.2 | X | ||
| Service-specific availability and readiness: midwife-led continuity of care* | Health system | E.2 | X | ||
| Service-specific availability and readiness: group ANC† | Health system | E.3 | X | ||
| ANC contacts (eight or more) | Health system | E.7 | X | ||
| Timing of first ANC contact | Health system | E.7 | X | ||
| Counselling on diet and exercise in pregnancy* | Content of care | A.1.1 | X | ||
| Outcomes | Iron and folic acid supplementation* | Content of care | A.2.1 and A.2.2 | X | |
| Calcium supplementation* | Content of care | A.3 | X | ||
| Vitamin A supplementation coverage* | Content of care | A.4 | X | ||
| Zinc supplementation† | Content of care | A.5 | X | ||
| Caffeine intake information | Content of care | A.10 | X | ||
| Classification of hyperglycaemia | Content of care | B.1.4 | X | ||
| Assessment for tobacco use and secondhand smoke exposure | Content of care | B.1.5 | X | ||
| Assessment for use of alcohol and other substances | Content of care | B.1.6 | X | ||
| Pregnant women counselled and tested for HIV and know their results | Content of care | B.1.7 | X | ||
| Screening for syphilis | Content of care | B.1.7 | X | ||
| Testing for tuberculosis* | Content of care | B.1.8 | X | ||
| Daily foetal movement counting† | Content of care | B.2.1 | X | ||
| Symphysis–fundal height measurement* | Content of care | B.2.2 | X | ||
| Ultrasound scan before 24 weeks | Content of care | B.2.4 | X | ||
| Treatment for asymptomatic bacteriuria | Content of care | C.1 | X | ||
| Prophylaxis for recurrent urinary tract infections† | Content of care | C.2 | X | ||
| Prophylaxis with anti-D immunoglobulin in non-sensitised Rhesus-negative pregnant women† | Content of care | C.3 | X | ||
| Treatment for helminths* | Content of care | C.4 | X | ||
| Intermittent preventive treatment for malaria * | Content of care | C.6 | X | ||
| Antiretroviral pre-exposure prophylaxis to prevent HIV infection* | Content of care | C.7 | X | ||
| Information and treatment for common physiological symptoms (eg, leg cramps, constipation and nausea) | Experience of care | D.1–D.6 | X | ||
| Counselling on birth preparedness and complication readiness | Content of care | Good clinical practice | X | ||
| Counselling on postpartum family planning | Content of care | Good clinical practice | X | ||
| Monitoring of foetal heart rate | Content of care | Good clinical practice | X | ||
| Monitoring of blood pressure | Content of care | Good clinical practice | X | ||
| Impact | Newborns protected at birth from tetanus | Content of care | C.5 | X | |
The monitoring domains for indicators that do not yet exist could change, depending on the types of indicators developed for specific recommendations.
*Measure is context-specific.
†Measure is for recommendations in the context of research.
ANC, antenatal care.
Given thematic overlap between measures in the final scoping review inventory, some recommendations and established good clinical practices within ANC have multiple existing measures: iron and folic acid supplements (n=7), HIV and syphilis screening and treatment (n=7), tetanus toxoid vaccination (n=6), monitoring of blood pressure (n=5), intermittent preventive treatment of malaria in pregnancy (n=4), intimate partner violence (n=2), tobacco (n=2), counselling on birth preparedness and complication readiness (n=2) and counselling on family planning (n=2). Thus, existing measures in table 1 (denoted by an ‘X’ under the column ‘Measure status: exists’) may include multiple unique measures for a particular ANC topic for measurement. Twenty-eight of the guideline’s recommendations and one established good clinical practice lack existing measures. Table 1 lists these existing and non-existent measurement areas by monitoring domain.
Existing measures could permit immediate measurement of 14 ANC recommendations in the 2016 WHO guideline using currently available data sources. Three of the 14 recommendations (B.1.7, C.6 and E.7) are perfectly aligned with existing measures.1 The 11 remaining recommendations have subtle gaps or discrepancies with the existing measures and would require minimal modification or disaggregation to be relevant. Furthermore, some of the existing measures are used solely in research settings and may not be applicable or feasible for routine monitoring and use. These measures require modification based on the new recommendations. Among the recommendations lacking existing measures, these non-existent measures relate to interventions involving health systems (n=8), nutrition (n=7), maternal and foetal assessment (n=7), common physiological symptoms (n=6), preventative measures (n=4) and counselling and information sharing (n=1).
Patient and public involvement
While the scoping review did not involve patients, the need for this scoping review was initiated by the WHO ANC guideline. Women’s views, specifically the desire for a positive pregnancy experience during ANC, informed the development of this guideline and are central to evidence-based practices included in the guideline. As part of the guideline’s development, a systematic review synthesised qualitative evidence on women’s needs and perspectives during ANC to inform the scope of the guideline, and the guideline development panel included a patient representative and members representing women.
Step 2: identifying core indicators and additional indicators
To monitor implementation of the new WHO ANC model, WHO facilitated an iterative and consultative process to reach consensus on indicators and an ANC monitoring framework. Following the scoping review, this process involved (1) soliciting written feedback from stakeholders within WHO; (2) facilitating working groups at the Mother and Newborn Information for Tracking Outcomes and Results technical advisory group meetings in May and November 2018 to reach consensus on the core and context-specific indicators, as well as indicator metadata; and (3) facilitating consultations in writing on the monitoring framework from experts and stakeholders participating in the July 2018 WHO Regional Office for Africa meeting on the dissemination of reproductive, maternal, newborn, and child health guidelines; the July 2018 WHO Regional Office for Southeast Asia Regional Meeting on Accelerating Reduction of Maternal, Newborn Mortality and Stillbirths: Towards Achieving the Sustainable Development Goals; and a September 2018 Expert Advisory Group on Maternal Immunisation. Selection of the core indicators was influenced by these consultations, as well as the criteria in WHO’s Global Reference List of 100 Core Health Indicators:
The indicator is prominent in the monitoring of major international declarations to which all member states have agreed or has been identified through international mechanisms such as reference or interagency groups as a priority indicator in specific programme areas.
The indicator is scientifically robust, useful, accessible, understandable as well as specific, measurable, achievable, relevant and time bound.
There is a strong track record of extensive measurement experience with the indicator (preferably supported by an international database).
The indicator is being used by countries in the monitoring of national plans and programmes.10
Core and context-specific indicators
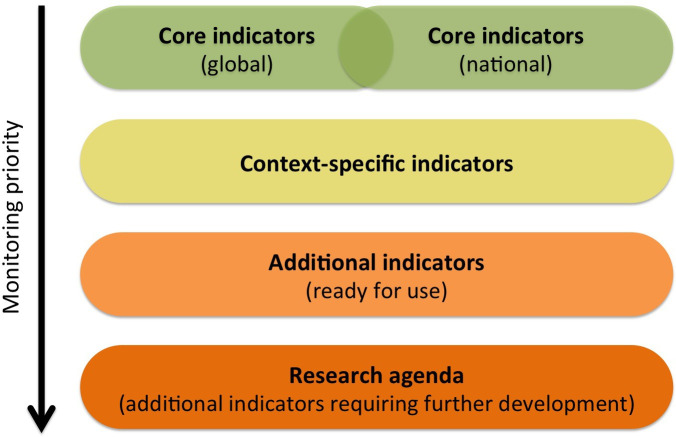
Based on the criteria listed previously and feedback from the various consultative processes, WHO recommends a list of universally relevant core indicators to be measured and monitored by all countries, as well as a menu of additional indicators from which countries can select indicators based on programme priorities (figure 1). Monitoring priority, indicated by the arrow in figure 1, starts with core indicators. The core indicators, indicated in green, can be collected immediately for global and national monitoring. Context-specific indicators, in yellow, will be appropriate for national and subnational monitoring in various settings (eg, undernourished populations, high-prevalence settings and malaria-endemic areas) based on the ANC recommendations. Additional indicators, in orange, may be relevant and desirable for monitoring, depending on local priorities. Some additional indicators can be used immediately in their current form, depending on the implementation context and available data sources. Other additional indicators exhibit serious measurement issues, warranting caution and additional research before they can be implemented. The research agenda reflects the challenges with these additional indicators.
Figure 1.
Menu of indicators.
Table 2 outlines the nine core indicators for monitoring the new WHO ANC model. These nine core indicators will track seven recommendations and three established good clinical practices. However, additional indicators should be developed to monitor adolescent girls’ and women’s experiences of ANC. Two core indicators (ultrasound scan before 24 weeks and experience of care) are included as placeholders requiring priority by the research agenda; these recommended indicators will be updated in the future once additional research is conducted and the indicators have been validated. Table 2 also includes the data sources for each indicator, including the preferred data source and other potential data sources. At this time, the majority of indicators are collected from population-based household surveys; however, in the future, as health information systems improve, it would be better to collect the majority of these indicators from routine health management information systems (HMIS) and other administrative data sources. Core indicator metadata are detailed in table 3.
Table 2.
Core and context-specific indicators for monitoring routine ANC
| Core indicators | ||||
| Monitoring domain | Indicator | Current preferred data source | Other data sources | WHO ANC model |
| Outputs | Percentage of pregnant women with first ANC contact in the first trimester (before 12 weeks of gestation) | Population-based surveys | HMIS | Recommendation E.7* |
| Outcomes | Percentage of pregnant women who received iron and folic acid supplements for 90+ days | Population-based surveys | HMIS | Recommendations A.2.1 and A2.2* |
| Percentage of pregnant women screened for syphilis during ANC | HMIS | Recommendations B.1.7* and 4.1† | ||
ANC contacts:
|
Population-based surveys | Recommendation E.7* | ||
| Percentage of pregnant women who were told about pregnancy danger signs during ANC | Population-based surveys | Recommendation 1‡ | ||
Blood pressure measurement:
|
Population-based surveys (indicator A) HMIS (indicator B) |
HMIS (indicator A) | Good clinical practice | |
| Percentage of pregnant women whose baby’s heartbeat was listened to at least once during ANC | Population-based surveys | HMIS | Good clinical practice | |
| Percentage of pregnant women with an ultrasound scan before 24 weeks§ | HMIS | Recommendation B.2.4* | ||
| Experience of care (eg, waiting time and support received during ANC contacts)§ | Population-based surveys | Research and health facility surveys | Good clinical practice | |
| Context-specific indicators | |||||
| Monitoring domain | Indicator | Monitoring context | Current preferred data source | Other data sources | WHO ANC model |
| Inputs | Health worker density and distribution | Rural and remote areas | Civil registration and vital statistics | HMIS, health facility surveys and annual administrative reports | Recommendation E.6* |
| Process | Percentage of health units with at least one service provider trained to care for and refer survivors of gender-based violence | Settings where there is the capacity to provide a supportive response (including referral where appropriate) and that meet the WHO minimum requirements for responding to intimate partner violence and sexual violence against women | Health facility assessments | Recommendation B.1.3* | |
| Outcomes | Percentage of pregnant women counselled and tested for HIV | High-prevalence settings | Population-based surveys | HMIS | Recommendation B.1.7* |
| Percentage of pregnant women reporting having received any drug for intestinal worms | Helminth-endemic areas | Population-based surveys | Recommendation C.4* | ||
| Percentage of women who received three or more doses of IPTp | Malaria-endemic areas in Africa | Population-based surveys | HMIS | Recommendation C.6* | |
| Percentage of PrEP | Pregnant women at substantial risk of HIV infection | Population-based surveys | HMIS | Recommendation C.7* | |
*Recommended by WHO.1
†Recommended by WHO.8
‡Recommended by WHO.6
§Placeholder for recommended indicator that may be updated in the future once additional research is conducted.
ANC, antenatal care; HMIS, health management information systems; IPTp, intermittent preventive treatment in pregnancy; PrEP, pregnant women who received oral pre-exposure prophylaxis.
Table 3.
Catalogue of core indicators and metadata
| WHO ANC model | Indicator name | Numerator | Denominator | Preferred data source | Other data sources |
| Outputs | |||||
| Recommendation E.7* | Percentage of pregnant women with first ANC contact in the first trimester (before 12 weeks of gestation) | Number of pregnant women aged 15–49 years who had their first antenatal contact in the first trimester | Total number of women aged 15–49 years with at least one ANC contact | Population-based surveys | |
| Number of antenatal clients with first contact before 12 weeks | Total number of antenatal clients with a first contact | HMIS | |||
| Outcomes | |||||
| Recommendations A.2.1 and A.2.2* | Percentage of pregnant women who received iron and folic acid supplements for 90+ days | Number of pregnant women who received the recommended number of iron/folic acid tablets during last pregnancy | Total number of women with a live birth | Population-based surveys | |
| Indicator not yet developed | Indicator not yet developed | HMIS | |||
| Recommendation B.1.7* | Percentage of pregnant women screened for syphilis during ANC | Number of antenatal clients screened for syphilis | Total number of antenatal clients with a first contact | HMIS | |
| Recommendation E.7* | ANC contacts
|
Number of women aged 15–49 years with a live birth who received ANC from any provider:
|
Total number of women aged 15–49 years with a live birth | Population-based surveys | |
| Recommendation 1† | Percentage of pregnant women who were told about pregnancy danger signs during ANC | Number of women aged 15–49 years with a live birth told about pregnancy danger signs during ANC | Total number of women aged 15–49 years with at least one ANC contact | Population-based surveys | |
| Good clinical practice | Blood pressure measurement: percentage of pregnant women with at least one blood pressure measure during ANC |
Number of women aged 15–49 years with a live birth who had their blood pressure measured during the last pregnancy that led to a live birth | Total number of women age 15–49 years with a live birth | Population-based surveys | |
| Number of antenatal clients with blood pressure measurement | Total number of antenatal clients with first contact | HMIS | |||
| Blood pressure measurement: percentage of pregnant women with at least one blood pressure measure in the third trimester during ANC |
Number of antenatal clients with blood pressure measurement in third trimester | Total number of antenatal clients with first contact | HMIS | ||
| Good clinical practice | Percentage of pregnant women whose baby’s heartbeat was listened to at least once during ANC | Number of women 15–49 years with a live birth whose baby’s heart was listened to at least once during ANC | Number of women 15–49 years with a live birth who received ANC | Population-based surveys | |
| Number of antenatal clients whose baby’s heartbeat was listened to | Total number of antenatal clients with a first contact | HMIS | |||
| Recommendation B.2.4* | Percentage of pregnant women with an ultrasound scan before 24 weeks‡ | Number of antenatal clients who had an ultrasound scan before 24 weeks | Total number of antenatal clients with a first contact | HMIS | |
| Good clinical practice | Experience of care (eg, waiting time and support received during ANC)‡ | Indicator not yet developed | Indicator not yet developed | Population-based surveys | Research and health facility surveys |
There are gaps in the core indicators for some recommendations due to a lack of existing and validated measures. We envision moving towards a monitoring framework that better measures content and experience of care, filling gaps in these crucial domains. This shift requires additional research and greater data collection from client exit interviews or observations, as this information cannot generally be captured from population-based surveys. It would also require strengthening HMIS to facilitate better measurement of ANC content, such as improved measures of alcohol and tobacco use during pregnancy, as well as moving to individual records as opposed to aggregated information that does not allow for tracking individual women over time.
Multiple ANC recommendations are unique to specific contexts and may be monitored nationally and subnationally.1 Existing indicators to monitor six context-specific recommendations are listed in table 2. Depending on the setting and the health system’s capacity, countries may track one or more context-specific indicators, in addition to the set of core indicators. Context-specific indicator metadata are detailed in table 4.
Table 4.
Catalogue of context-specific indicators and metadata
| WHO ANC model | Indicator name | Numerator | Denominator | Preferred data source | Other data sources |
| Inputs | |||||
| Recommendation E.6 | Health worker density and distribution | Number of health workers | Total population | Civil registration and vital statistics | HMIS, health facility surveys, annual administrative reports |
| Process | |||||
| Recommendation B.1.3 | Percentage of health units with at least one service provider trained to care for and refer survivors of gender-based violence | Number of health facilities reporting that they have both documented and adopted a protocol for the clinical management of sexual and gender-based violence survivors | Total number of health facilities surveyed | Health facility assessments | |
| Outcomes | |||||
| Recommendation B.1.7 | Percentage of pregnant women counselled and tested for HIV | Number of women counselled and offered voluntary HIV testing at ANC before their most recent birth and received their test results | Total number of women with a live birth | Population-based surveys | HMIS |
| Recommendation C.4 | Percentage of pregnant women reporting having received any drug for intestinal worms | Number of pregnant women reporting having received any drug for intestinal worms | Total number of women with a live birth | Population-based surveys | |
| Recommendation C.6 | Percentage of women who received three or more doses of IPTp | Number of pregnant women receiving three or more doses of recommended treatment | Total number of women with a live birth | Population-based surveys | |
| Number of pregnant women given at least three doses of recommended treatment (sulfadoxine/pyrimethamine) | Number of antenatal clients with first contact | HMIS | |||
All recommendations come from the 2016 ANC guideline.1
ANC, antenatal care; HMIS, health management information systems; IPTp, intermittent preventive therapy for malaria during antenatal care contacts during their last pregnancy.
Additional indicators
Many of the measures found by the scoping review were limited to research studies and may not yet be feasible for routine monitoring. Thirty-five existing indicators (online supplementary annex 1) do not meet the criteria of core or context-specific indicators but may be relevant and desirable for monitoring, depending on priorities.3 Some of these indicators (n=22) can be used immediately in their current form, depending on the implementation context and available data. Other indicators exhibit serious measurement issues (n=13), such as variation in their definitions or limited testing, and require additional research before they are implemented. Countries are advised to proceed with caution in selecting additional indicators that require further research. With continued development and input from stakeholders, additional indicators could provide valuable insight into the delivery of routine ANC. Given that multiple indicators may align with the same recommendation (eg, A.2.1 and B.1.7), individuals monitoring ANC could choose the most appropriate indicator based on available data sources and country preferences.
bmjgh-2020-002605supp001.pdf (216KB, pdf)
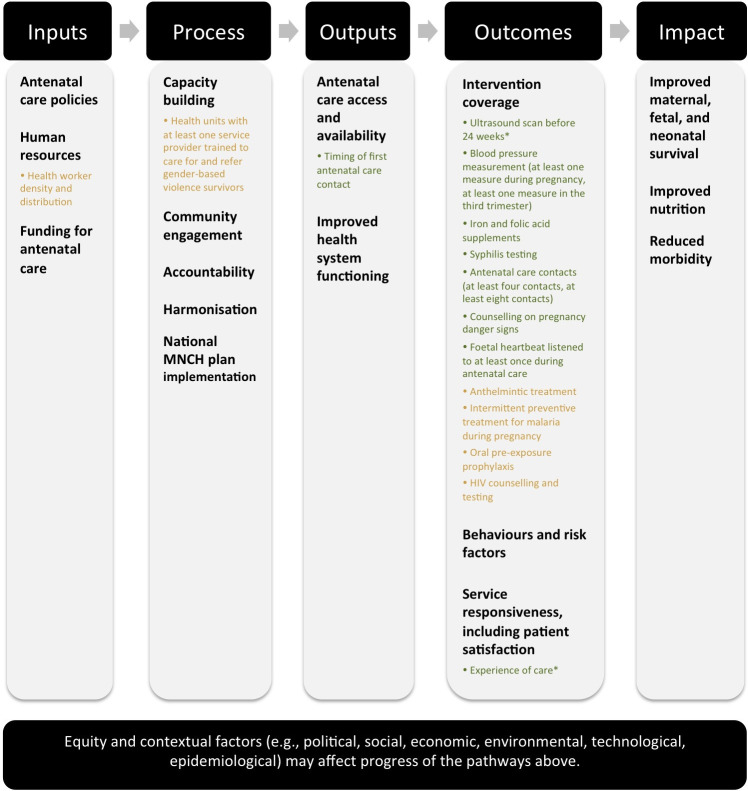
Step 3: monitoring framework for routine ANC
The monitoring framework depicting core and context-specific indicators for the new WHO ANC model (figure 2) was adapted from the evaluation framework for the scale-up for maternal and child survival and from the WHO’s 100 core health indicators by results chain.10 11 It depicts the pathways by which routine components of ANC are implemented. At the top of this framework, we include the domains under which indicators may be monitored. At the bottom of this framework, we recognise that equity and contextual factors (eg, social, technological and epidemiological) may affect the progress of the pathways depicted previously. Headings in black (eg, ANC policies, capacity building and improved nutrition) capture routine components of ANC from WHO recommendations, including recommendations for good clinical practices and health promotion.1 5 6 8 Male involvement, for example, would fit within community engagement. The bulleted points in figure 2 illustrate where core indicators (in green) and context-specific indicators (in yellow) from the new WHO ANC model (eg, iron and folic acid supplements, ultrasound scan before 24 weeks and anthelmintic treatment) and other recent recommendations (eg, syphilis testing and counselling on pregnancy danger signs) fit into the framework. Indicators are currently available to measure recommendations primarily under the ‘outcomes’ domain.
Figure 2.
Monitoring framework depicting core and context-specific indicators for the new WHO ANC model core indicators are in green. Context-specific indicators are in yellow. *Placeholder indicator. ANC, antenatal care; MNCH, maternal, newborn, and child health.
The new WHO ANC model aims to achieve maternal outcomes (eg, infections, side effects and symptomatic relief), foetal/neonatal outcomes (eg, preterm birth, congenital abnormalities and low birth weight), test accuracy outcomes (eg, sensitivity and specificity) and health systems outcomes (eg, ANC coverage and facility-based delivery).1 These outcomes of interest guided the development of the new WHO ANC model and provide clarity on what the monitoring framework’s ‘impact’ domain means for ANC. This illustrative monitoring framework is not static. As indicators are developed and as guidance changes, this monitoring framework will be updated, along with the accompanying menu of indicators.
Step 4: research agenda for monitoring ANC
Among the ANC interventions recommended by WHO, 28 recommendations and one good clinical practice lack existing indicators (table 1).1 3 Monitoring and assessing the quality of routine ANC requires urgent attention to the development of new standardised measures. Specifically, monitoring routine ANC requires developing new measures for the content of ANC (n=19), the health system (n=7), and adolescent girls’ and women’s experiences of care (n=6). Researchers must also address challenges, such as a need for additional validation studies, in order for selected existing indicators to be reliably implemented with confidence.
Adolescent girls’ and women’s experiences of ANC are located at the core of the quality of care framework for routine ANC.3 Women consider experience of care to be a crucial component of quality of care and respectful care.4 12 Yet, unlike intrapartum care,13 we have no valid measures to capture adolescent girls’ and women’s experiences of ANC. Measuring the quality and delivery of ANC requires greater attention to adolescent girls’ and women’s voices, if healthcare services are to effectively implement a woman-centred approach.14 Furthermore, research on ANC indicators must also fill gaps in needed indicators to measure quality of care, including respectful care. In addition, limited measures exist for counselling services during ANC, as well as tobacco and alcohol exposure. These critical areas require additional research to develop measures, as well as greater collaboration with allied fields in the development and monitoring of ANC.
Conclusion
Based on the scoping review and iterative consultative process, WHO recommends nine core indicators for measuring and monitoring the new WHO ANC model in all settings and six context-specific indicators that are unique to specific national and subnational contexts. To monitor all 42 recommended interventions in the new WHO ANC model, improved data sources are required. Women’s individual ANC records (case notes) and health policy guidelines/directives could provide data for eight recommendations lacking existing indicators; however, data from existing clinical records are often not linked for each ANC contact and could be challenging to procure. Population-based surveys (eg, DHS and MICS) fall short in capturing the data required for these recommendations. Properly monitoring quality ANC requires additional reliable, high-quality data sources, as well as stronger HMIS and routine data systems at the patient level.
To facilitate comparability across settings and time, new and existing measures to monitor ANC must be standardised in definition, measurement, and level of data collection and usage. Standardising and strengthening the development of ANC measures would benefit efforts beyond monitoring the new WHO ANC model. New and refined measures would assist researchers and programme implementers in their efforts to analyse the content and quality of ANC, locate ANC implementation bottlenecks, evaluate equity of ANC programme coverage and use, and evaluate the effectiveness of new innovations for delivering maternal health services.15–18
We envision a future in which monitoring routine ANC moves from only coverage measures to more comprehensive and meaningful measures of quality-adjusted ANC that include content and appropriate actions taken. It is simply not enough to measure whether a health provider measured a woman’s blood pressure once during pregnancy. Did the woman receive the recommended package of quality ANC services at each contact? If the woman’s blood pressure was high, did the provider act on the high measure? We encourage researchers to take the aforementioned points into consideration when designing and testing these much-needed indicators for monitoring routine ANC.
Acknowledgments
We thank participants at the May and November 2018 Mother and Newborn Information for Tracking Outcomes and Results advisory group meetings in Geneva, Switzerland; participants at the July 2018 Regional Office for Africa meeting in Kigali, Rwanda; participants at the July 2018 Regional Office for Southeast Asia meeting in New Delhi, India; and members of the Expert Advisory Group on Maternal Immunization who met in September 2018 in Geneva, Switzerland for their input on this monitoring framework. We also acknowledge inputs from Dr Maurice Bucagu, Dr Doris Chou, Dr Juan-Pablo Pena-Rosas and Dr Lisa Rodgers.
Footnotes
Handling editor: Seye Abimbola
Contributors: SRL wrote the first draft of the manuscript, and all authors contributed to subsequent revisions. SRL and ACM contributed equally to this paper.
Funding: This work was supported by the United Nations Development Programme-United Nations Population Fund-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction, a cosponsored programme executed by the WHO.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
The data extraction workbook for the scoping review is available on request from ÖT (tuncalpo@who.int) at the WHO.
Ethics statements
Patient consent for publication
Not required.
References
- 1. WHO . WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO, 2016. [PubMed] [Google Scholar]
- 2. Hodgins S, D'Agostino A. The quality-coverage gap in antenatal care: toward better measurement of effective coverage. Glob Health Sci Pract 2014;2:173–81. 10.9745/GHSP-D-13-00176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lattof SR, Tunçalp Ö, Moran AC, et al. Developing measures for WHO recommendations on antenatal care for a positive pregnancy experience: a conceptual framework and scoping review. BMJ Open 2019;9:e024130. 10.1136/bmjopen-2018-024130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Downe S, Finlayson K, Tunçalp Ö, et al. Provision and uptake of routine antenatal services: a qualitative evidence synthesis. Cochrane Database Syst Rev 2019;6:CD012392. 10.1002/14651858.CD012392.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. WHO . Standards for improving quality of maternal and newborn care in health facilities. Geneva: WHO, 2016. [Google Scholar]
- 6. WHO . Who recommendations on health promotion interventions for maternal and newborn health. Geneva: World Health Organization, 2015. [PubMed] [Google Scholar]
- 7. Moran AC, Jolivet RR, Chou D, et al. A common monitoring framework for ending preventable maternal mortality, 2015-2030: phase I of a multi-step process. BMC Pregnancy Childbirth 2016;16:250. 10.1186/s12884-016-1035-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. WHO . Syphilis screening and treatment for pregnant women. Geneva: World Health Organization, 2017. [PubMed] [Google Scholar]
- 9. WHO . Working with individuals, families and communities to improve maternal and newborn health: a toolkit for implementation. Geneva: World Health Organization, 2017. [Google Scholar]
- 10. WHO . Global reference list of 100 core health indicators (plus health-related SDGs. Geneva: World Health Organization, 2018. [Google Scholar]
- 11. Bryce J, Victora CG, Boerma T, et al. Evaluating the scale-up for maternal and child survival: a common framework. Int Health 2011;3:139–46. 10.1016/j.inhe.2011.04.003 [DOI] [PubMed] [Google Scholar]
- 12. Bohren MA, Titiloye MA, Kyaddondo D, et al. Defining quality of care during childbirth from the perspectives of Nigerian and Ugandan women: a qualitative study. Int J Gynaecol Obstet 2017;139 Suppl 1:4–16. 10.1002/ijgo.12378 [DOI] [PubMed] [Google Scholar]
- 13. Bohren MA, Mehrtash H, Fawole B, et al. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. The Lancet 2019;394:1750–63. 10.1016/S0140-6736(19)31992-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Downe S, Finlayson K, Tunçalp Ӧ, et al. What matters to women: a systematic scoping review to identify the processes and outcomes of antenatal care provision that are important to healthy pregnant women. BJOG 2016;123:529–39. 10.1111/1471-0528.13819 [DOI] [PubMed] [Google Scholar]
- 15. Benova L, Tunçalp Ö, Moran AC, et al. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Health 2018;3:e000779. 10.1136/bmjgh-2018-000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Baker U, Okuga M, Waiswa P, et al. Bottlenecks in the implementation of essential screening tests in antenatal care: syphilis, HIV, and anemia testing in rural Tanzania and Uganda. Int J Gynaecol Obstet 2015;130 Suppl 1:S43–50. 10.1016/j.ijgo.2015.04.017 [DOI] [PubMed] [Google Scholar]
- 17. Balakrishnan R, Gopichandran V, Chaturvedi S, et al. Continuum of care services for maternal and child health using mobile technology – a health system strengthening strategy in low and middle income countries. BMC Med Inform Decis Mak 2016;16:1–8. 10.1186/s12911-016-0326-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baqui AH, Rosecrans AM, Williams EK, et al. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan 2008;23:234–43. 10.1093/heapol/czn012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-002605supp001.pdf (216KB, pdf)
Data Availability Statement
The data extraction workbook for the scoping review is available on request from ÖT (tuncalpo@who.int) at the WHO.