Abstract
Background:
Breast cancer survivors with elevated inflammation have a greater risk for cancer recurrence, premature mortality, and comorbid disease development. The psychological stress survivors experience when confronted with a breast cancer diagnosis and cancer treatment can heighten inflammation. Identifying factors that reduce stress and inflammation could lead to improvements in survivors’ long-term health. Accordingly, this study examined the health-enhancing effects of romantic relationships—a key health determinant—on breast cancer survivors’ stress and inflammation.
Methods:
Breast cancer survivors (n = 139, stages 0-IIIC) completed a baseline visit before treatment and two follow-up visits 6 and 18 months after treatment ended. Women completed self-report questionnaires assessing their romantic relationship satisfaction and perceived stress, and they provided a blood sample for serum markers of inflammation at each visit. The longitudinal design allowed for examination within and between survivors. We conducted multilevel mediation analyses to assess how changes in survivors’ relationship satisfaction were related to changes in stress and inflammation from visit to visit (i.e., within-person effects), as well as how the average effects of relationship satisfaction were associated with average stress and inflammation levels throughout the study (i.e., between-person effects).
Results:
At the within-person level, at visits in which survivors were more satisfied with their relationships, they also perceived less stress, which in turn was related to lower than their own average levels of serum C-reactive protein and proinflammatory cytokines (tumor necrosis factor-α, interleukin-6, and interleukin-1β). At the between-person level, survivors who had greater relationship satisfaction throughout the study had lower perceived stress, which was linked to lower levels of inflammation.
Conclusion:
Breast cancer survivors in satisfying romantic relationships felt less stressed and in turn had lower inflammation throughout cancer treatment. This study illustrates the utility of a within-person approach to not only consider the average effects of relationship satisfaction, but also how changes in their own relationship satisfaction impact stress and inflammation over time. Our findings demonstrate important psychological and immunological pathways through which satisfying relationships may promote breast cancer survivors’ long-term health.
Keywords: cancer survivors, inflammation, stress, romantic relationships, health
1. Introduction
Inflammation carries significant health risks to breast cancer survivors. Elevated inflammation increases the chance of cancer recurrence and comorbid disease development (Pierce et al., 2009; Smyth et al., 2004), and contributes to accelerated aging and premature mortality (Aggarwal et al., 2006; Alfano et al., 2017). Survivors’ psychological stress also increases while confronting a breast cancer diagnosis and undergoing cancer treatment (Weber and Solomon, 2008). These elevated stress levels can in turn heigthen inflammation (Powell et al., 2013). Indeed, breast survivors who were more stressed during treatment had higher inflammation than their less stressed counterparts (Mundy-Bosse et al., 2011).
Epidemiological research has highlighted the importance of intimate relationships as a key health determinant, particularly in stressful times (Holt-Lunstad et al., 2010; Pietromonaco and Collins, 2017). Partners in highly satisfying relationships live longer and have fewer health problems than their unsatisfied and single counterparts (Kiecolt-Glaser and Newton, 2001; Robles et al., 2014). Moreover, the impact of people’s relationships on their long-term health is comparable or greater than that of well-known factors such as body mass index (Holt-Lunstad et al., 2010). The stress- and health-buffering effects of satisfying relationships are also evident in breast cancer survivors, helping them deal with the emotional and physical health consequences of receiving a potentially life-threatening diagnosis and undergoing treatment. For instance, a close and supportive partner helps to reduce survivors’ stress levels during treatment (Kayser and Scott, 2008), while an avoidant and unsupportive partner can boost survivors’ stress and impair their physical functioning (Manne et al., 2005). After expressing concerns about their cancer, survivors whose partners also disclosed personal feelings and cancer-related concerns were less distressed than survivor whose partners were less disclosing (Manne et al., 2004b). In addition, a partner’s disclosure, along with feeling accepted, understood, and cared for by a partner, was associated with greater intimacy among survivors (Manne et al., 2004a). These findings demonstrate that survivors’ relationships can facilitate adaptation to their diagnosis and throughout cancer treatment, including reducing their stress and improving their health.
Relationships also have important implications for immune functioning; for example, people in more satisfying relationships had better immune responses to a vaccine than their less satisfied counterparts (Phillips et al., 2006). In addition, following supportive and conflictual marital interactions, less negative and hostile partners (e.g., less sarcasm and withdrawal/disengagement) had lower inflammation compared to more hostile partners (Kiecolt-Glaser et al., 2005). The more partners were engaged in the marital discussions, the lower their inflammation the next day (Graham et al., 2009). Longitudinal research over a two-year period showed that partners in less distressing and more satisfying relationships had better cellular immune function, while their more distressed and unsatisfied counterparts had greater cellular immune dysregulation over time (Jaremka et al., 2013b). Though the salutary effects of relationships on immune function are shown in healthy partners, their benefits have not been examined among cancer survivors—a group that is particularly at risk for inflammation-related health problems (Alfano et al., 2017; Pierce et al., 2009).
Stress is an important path connecting relationship perceptions to health (Robles et al., 2014; Slatcher and Selcuk, 2016). Indeed, stress in relationships promotes inflammation both cross-sectionally and longitudinally (Kiecolt-Glaser et al., 2005, 2003). Partners in less secure relationships have elevated cortisol and poorer cellular immune function (Jaremka et al., 2013a). Though a satisfying relationship can prevent or reduce stress perceptions and protect health (Schoebi and Randall, 2015; Uchino, 2004), much of the literature demonstrates the stress-promoting and immune-compromising effects of low-quality and hostile relationships (Kiecolt-Glaser et al., 2018, 2005, 2003). The emphasis on negative aspects of relationships has created a gap in the literature on how high-quality and satisfying relationships may contribute to lower inflammation (Robles and Kiecolt-Glaser, 2003).
Given the role of relationships in health outcomes—particularly among those with chronic illness (Kiecolt-Glaser and Wilson, 2017; Robles et al., 2014; Shrout, 2019)—it is important to understand how breast cancer survivors’ relationships relate to their stress and inflammation. A breast cancer diagnosis and cancer treatment can negatively impact many facets of survivors’ relationships, including time with their partners, open and honest communication, and planning for the future (Manne et al., 2014, 2006). After survivors complete cancer treatment, resuming their pre-treatment or “normal” lives with their partners can be difficult (Kim et al., 2010). These changes in breast cancer survivors’ relationship satisfaction throughout treatment may offer a new pathway to survivors’ stress and inflammation levels, ultimately affecting their long-term health.
This longitudinal study assessed the effects of satisfying relationships on breast cancer survivors’ stress and inflammation. We measured breast cancer survivors’ relationship satisfaction, perceived stress, and inflammation before treatment began, and then 6 and 18 months after primary treatment completion. In addition to examining the average effects of relationship satisfaction on stress and inflammation throughout the study (i.e., between-person effects), the longitudinal design allowed for examination of how changes in their own relationship satisfaction relate to changes in their stress and inflammation over time (i.e., within-person effects). These within-person (i.e., intra-individual) processes are important in understanding how a survivor’s own relationship satisfaction changes before and after treatment, as well as how these changes impact how her own stress and inflammation change from visit to visit, rather than how her stress and inflammation compare to other survivors. Thus, parsing out effects between and within survivors offers novel insights not only into how relationships impact average levels of stress and inflammation across survivors, but also into how changes in relationship satisfaction are associated with changes in stress and inflammation within a given survivor. Within survivors, we expected that at visits in which survivors were more satisfied with their relationships, they would also perceive less stress, which would be associated with lower than their own average levels of inflammation. Between survivors, we hypothesized that survivors who were satisfied with their romantic relationship throughout the study would also perceive less stress, which in turn would relate to lower average inflammation levels.
2. Methods and materials
2.1. Participants and procedure
Participants were women who were married/domestic partners with a breast cancer diagnosis (n = 139, stages 0-IIIC) identified at cancer clinics for a larger longitudinal study on fatigue and immune function. This study was thus a secondary analysis from the larger study and was not pre-registered. Nevertheless, this study was informed by a priori, conceptually driven hypotheses, and data are available upon request from the first author. The larger study included 209 women; however, 70 women were excluded from these analyses because they were not married/domestic partners (i.e., they were single, divorced, windowed). The excluded women did not differ on the current study’s outcome variables (ps > .10). Women were recruited within 1–3 months after their diagnosis to complete a baseline visit prior to beginning cancer treatment and two follow-up visits 6 and 18 months after treatment ended (surgery, radiation, or chemotherapy, whichever came last). At each visit, women completed self-report questionnaires and provided a blood sample. Exclusion criteria included a history of cancer except basal or squamous cell skin carcinomas and significant visual, auditory, or cognitive impairments that would interfere with study completion. Women were on average 55 years old (SD = 9.65, range 32–78) and primarily White (86%). Table 1 provides additional sample characteristics. The Ohio State University Institutional Review Board approved the project, and all women gave written informed consent prior to participation.
Table 1.
Baseline characteristics of breast cancer survivors.
| Number (%) | |
|---|---|
| Race | |
| White | 120 (86%) |
| Black | 10 (7%) |
| Other | 9 (7%) |
| Education | |
| < College | 62 (44%) |
| ≥ College | 77 (56%) |
| Cancer stage | |
| 0 | 29 (21%) |
| I | 53 (38%) |
| II | 40 (29%) |
| IIIA-C | 16 (12%) |
| Cancer treatment | |
| Surgery only | 40 (29%) |
| Radiation and surgery | 36 (26%) |
| Chemotherapy and surgery | 24 (17%) |
| Radiation, chemotherapy, and surgery | 38 (28%) |
Note: The reported data reflect information obtained at the first visit.
2.2. Self-report measures
The 4-item Couples Satisfaction Index (CSI-4) assessed relationship satisfaction (Funk and Rogge, 2007). Developed using item response theory, the short version of the CSI distinguishes between satisfied and dissatisfied partners with greater precision than most commonly used relationship satisfaction scales (Funk and Rogge, 2007). Cronbach’s α for the CSI-4 ranged from .92 to .95 across the three visits. The 4-item Perceived Stress Scale (PSS-4) measured perceived stress over the past week (Cohen et al., 1983). The 4-item version provides researchers the opportunity to assess perceived stress more easily where short questionnaires are required, such as in longitudinal research (Cohen et al., 1983). Cronbach’s α for the PSS-4 ranged from .79 to .85 across the three visits.
2.3. Inflammation assays
Fasting blood samples were collected between 7:00 and 9:00 AM to control for diurnal variation. Serum C-reactive protein (CRP) was measured using a chemilluminescence methodology via the Immulite 1000 (Siemens Healthcare Diagnostics, Inc., Deerfield, IL). Sensitivity for the assay was .3 mg/L. The intra-assay coefficient of variation (CV) was 3.1%, and the inter-assay CV was 7.3%. Serum levels of proinflammatory cytokines tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and interleukin-1β (IL-1β) were measured using an electrochemiluminescence method with Meso Scale Discovery kits, and read using the Meso Scale Discovery Sector Imager 2400 (Meso Scale Discovery, Rockville, MD). Sensitivity was .3 pg/mL, .4 pg/mL, and .2 pg/mL for TNF-α, IL-6, and IL-1β, respectively. The intra-assay and inter-assay CVs for TNF-α were 4.32% and 5.30%, respectively; corresponding values were 1.43% and 4.42% for IL-6 and 4.15% and 4.03% for IL-1β. Each participant’s frozen samples were assayed for all inflammatory markers at one time, thus using the same controls for all time points for each person. Inflammatory measurements were natural-log transformed prior to analyses to better approximate normality of residuals. In addition to CRP, a z-score composite of the serum cytokines (TNFα-, IL-6, and IL-1β) was calculated to obtain a summary inflammatory cytokine measure (Alfano et al., 2017). The composite had the advantage of reducing the number of statistical tests, particularly given the correlations among cytokine values across the study (rs = .41 to .56).
2.4. Analytic plan
First, preliminary analyses examined correlations between and among the main study variables across the visits, as well as changes in study variables over time. Next, multilevel mediation analyses were conducted to test the study hypotheses that relationship satisfaction would be linked to inflammation through perceived stress. This multilevel modeling approach accounted for the non-independence in participants’ data (i.e., an individual’s scores on the same variable over time) and maximized the use of existing data by including all participants in the analyses, regardless of missing data points (Brauer and Curtin, 2018). Relationship satisfaction, stress, and inflammation were assessed at each visit, allowing for within-person (i.e., level 1–1-1) and between-person (i.e., level 2–2-2) mediation hypothesis testing. We used the MLmed macro for SPSS (Rockwood and Hayes, 2017) with robust standard errors (REM estimation) to simultaneously account for within-person and between-person variability (Bauer et al., 2006). Thus, variables at the within-person level were person-centered so that participants’ scores at each visit reflected how much higher or lower their satisfaction, stress, and inflammation deviated from their own average across the study. At the between-person level, variables were grand mean-centered to represent the average associations between satisfaction, stress, and inflammation throughout the study. Indirect effects were tested with Monte Carlo simulations generating 95% confidence intervals (CIs) using 10,000 resamples and were significant if the CIs did not include zero (Rockwood and Hayes, 2017). The effect of chemotherapy treatment, comorbidities, body mass index (BMI), education level, age, and time were controlled for in all analyses.
3. Results
3.1. Descriptives
Table 2 reports summary statistics for key study variables. Correlations across the study showed that higher relationship satisfaction was correlated with lower stress (rs = −.22 to −.43, ps < .04) but not CRP levels (rs = −.12 to .15, ps > .19) or the cytokine composite (rs = −.02 to .01, ps > .89). Stress was not associated with CRP (rs = .03 to .13, ps > .24) or the cytokine composite (rs = .02 to .09, ps > .28). Higher CRP was related to greater cytokine composite scores at the first visit (r = .21, p = .01) but not at the second or third visits (rs = .16 to .18, ps > .10). In addition, relationship satisfaction scores were positively correlated across the visits (rs = .52 to .82, ps < .001), as were stress (rs = .43 to .70, ps < .001), CRP (rs = .71 to .74, ps < .001), and cytokines composite levels (rs = .62 to .82, ps < .001).
Table 2.
Estimated marginal means and standard errors of primary study variables.
| Visit 1 | Visit 2 | Visit 3 | |
|---|---|---|---|
| Relationship satisfaction | 16.07a (.46) | 14.70b (.43) | 15.15b (.43) |
| Stress | 5.86a (.30) | 4.18b (.29) | 4.34b (.30) |
| CRP (log10) | .05 (.05) | .04 (.05) | .13 (.06) |
| Cytokine composite (log10) | −.03 (.07) | −.04 (.07) | −.08 (.08) |
Note. CRP = C-reactive protein. Cytokine composite reflects a composite of TNF-α, IL-6, and IL-1β (standardized and averaged). CRP and cytokine composite data are log transformed, consistent with the analyses. Means that do not share the same superscript differ at p < .05.
We then conducted linear mixed models to examine changes in relationship satisfaction, perceived stress, CRP, and cytokine composite scores over time (see Table 2 for estimated marginal means and standard deviations). This approach allowed for explicit modeling of the within-person correlation across visits. Relationship satisfaction was higher at the first visit (before treatment) compared to the second visit (6 months after treatment; b = 1.38, β = 1.38, SE = .40, p = .001, 95% CI [.601, 2.161]) and third visit (18 months after treatment; b = .92, β = .92, SE = .40, p = .02, 95% CI [.136, 1.709); there were no differences between relationship satisfaction at the second and third visits (b = −.46, β = −.46, SE = .36, p = .21, 95% CI [−1.177, .259). Perceived stress was higher at the first visit than at the second (b = 1.67, β = 1.67, SE = .28, p < .001, 95% CI [1.119, 2.226]) and third visits (b = 1.52, β = .1.52, SE = .31, p < .001, 95% CI [.914, 2.122]; stress was not different at the two post-treatment visits (b = −.15, β = −.15, SE = .29, p = .60, 95% CI [−.735, .426]). CRP levels did not change over time (ps < .06), nor did cytokine composite levels (ps < .43).
3.2. Multilevel mediation analyses predicting CRP
We first conducted multilevel mediation analyses to test the indirect effect of relationship satisfaction on CRP through stress while simultaneously accounting for within-person and between-person variability (see Figure 1 for coefficients). At both the within- and between-person levels, higher relationship satisfaction was associated with lower perceived stress (pwithin = .04, 95% CI [−.274, −.008]; pbetween < .001, 95% CI [−.357, −.124]). Higher stress was also linked to higher CRP levels (pwithin < .001, 95% CI [.132, .174]; pbetween = .001, 95% CI [.033, .096]). Relationship satisfaction was not directly associated with CRP with and without perceived stress in the model (ps > .06), however, it was indirectly related to CRP through perceived stress at both within- and between-person levels (pwithin = .04, 95% CI [−.042 −.001]; pbetween = .004, 95% CI [−.027, −.006]). That is, at the within-person level, visits at which survivors had higher relationship satisfaction than usual, the less stressed they felt, which in turn was associated with lower than their own average levels of CRP. At the between-person level, compared to their less satisfied peers, survivors who had greater relationship satisfaction throughout the study had lower stress, which was related to lower levels of CRP. Thus, the beneficial effects of satisfying relationships on inflammation were transmitted through lower perceived stress levels.
Figure 1.
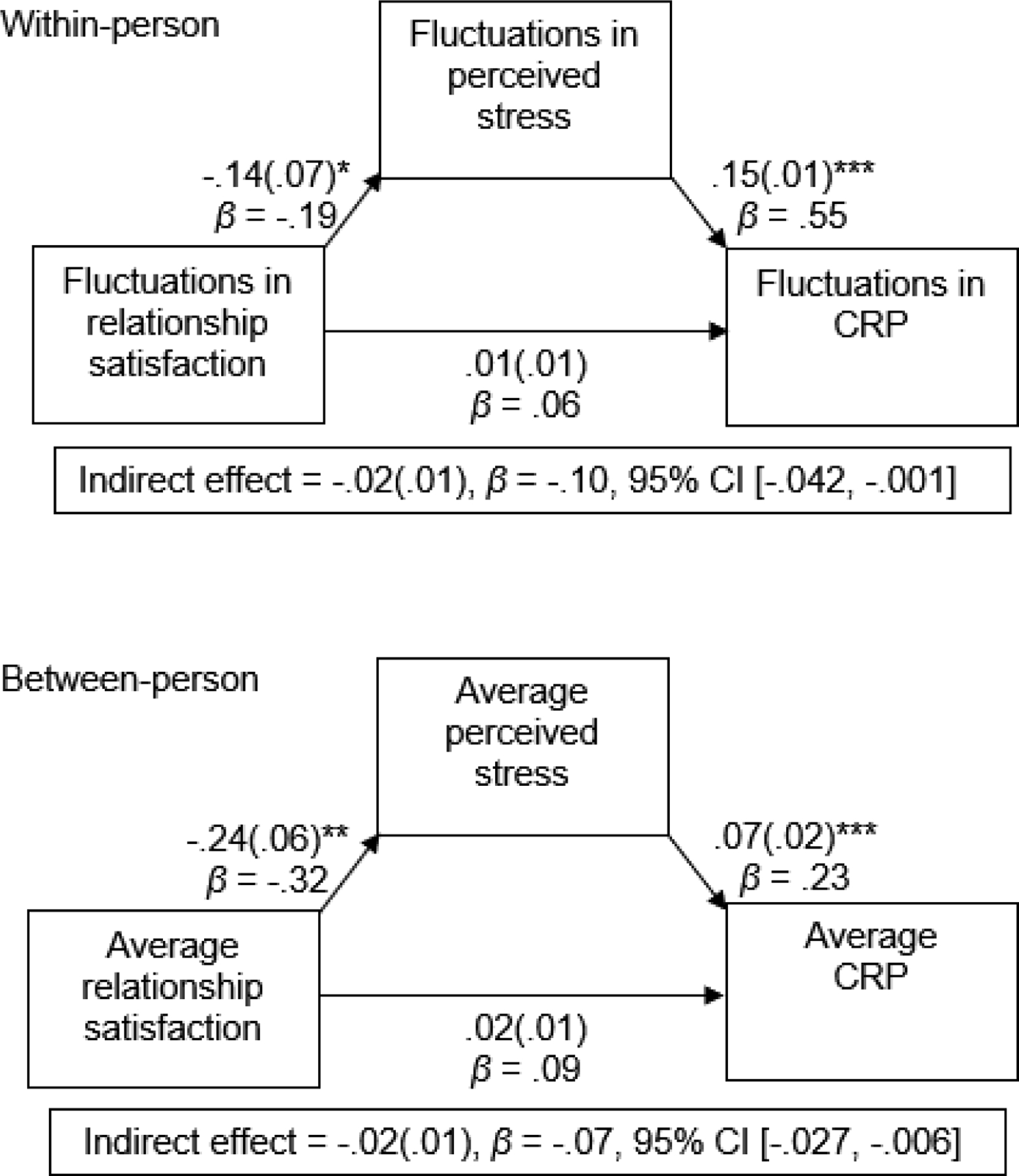
CRP = C-reactive protein. Coefficients for the multilevel mediation models on CRP, separately for the within- and between-person level of analysis; unstandardized path coefficients (and standard errors) are shown first, followed by standardized path coefficients. Within-person analyses demonstrate associations among fluctuations in relationship satisfaction, stress, and inflammation from visit to visit. Between-person analyses demonstrate associations among average relationship satisfaction, stress, and inflammation across the study.
*p < .05; **p < .01; ***p < .001
In addition to these main study variables, there were several significant covariates. Perceived stress levels decreased over time (b = −.08, β = −.21, SE = .02, p < .001, 95% CI [−.101, −.043]) and with age (b = −.06, β = −.16, SE = .02, p = .02, 95% CI [−.104, −.011]). A higher number of comorbidities was also linked to greater stress (b = .52, β = .16, SE = .25, p = .04, 95% CI [.035, 1.013]). BMI, education level, and chemotherapy treatment were not related to perceived stress (ps > .35). For CRP, levels increased over time (b = .01, β = .14, SE = .00, p = .002, 95% CI [.007, .022]), with age (b = .01, β = .07, SE = .00, p = .04, 95% CI [.000, .017]), and among those with a higher BMI (b = .04, β = .26, SE = .01, p < .001, 95% CI [.026, .051]); chemotherapy treatment, education level, and number of comorbidities were not predictive of CRP (ps > .08).
3.3. Multilevel mediation analyses predicting inflammatory cytokines
Next, we assessed the indirect effect of relationship satisfaction on the cytokine composite through perceived stress (see Figure 2 for coefficients). Consistent with the model predicting CRP, higher relationship satisfaction was linked to lower stress perceptions at the within- and between-person levels (pwithin = .04, 95% CI [−.275, −.007]; pbetween < .001, 95% CI [−.351, −.119]). Likewise, as perceived stress increased, so did cytokine composite levels (pwithin < .001, 95% CI [.178, .232]; pbetween = .007, 95% CI [.036, .150]). There was no direct link between relationship satisfaction and the cytokine composite with and without perceived stress in the model (ps > .27); however, as with the model with CRP as the outcome, the indirect effect of relationship satisfaction on cytokine composite levels through stress was significant (pwithin = .04, 95% CI [−.057, −.001]; pbetween = .01, 95% CI [−.041, −.007]). At the within-person level, when survivors’ relationship satisfaction was higher at a given visit compared to their own average satisfaction across the study, the less stressed they felt, which was associated with lower than their own average cytokine levels. At the between-person level, higher relationship satisfaction throughout the study was associated with lower perceived stress and in turn lower cytokine levels.
Figure 2.
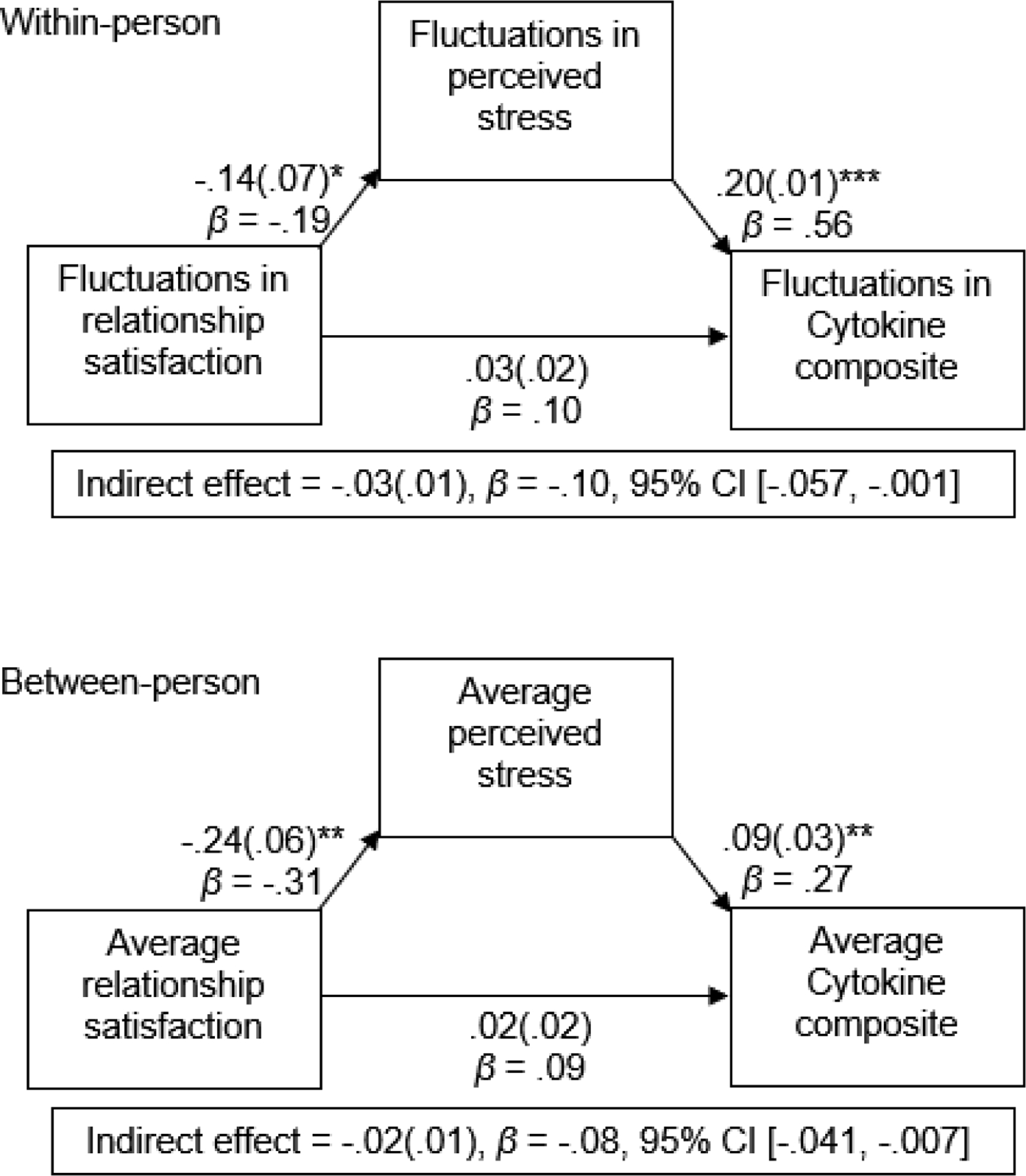
Cytokine composite reflects a composite of TNFα-, IL-6, and IL-1β (standardized and averaged). Coefficients for the multilevel mediation models on pro-inflammatory cytokine levels, separately for the within- and between-person level of analysis; unstandardized path coefficients (and standard errors) are shown first, followed by standardized path coefficients. Within-person analyses demonstrate associations among fluctuations in relationship satisfaction, stress, and inflammation from visit to visit. Between-person analyses demonstrate associations among average relationship satisfaction, stress, and inflammation across the study.
*p < .05; **p < .01; ***p < .001
Significant covariates indicated that stress decreased over time (b = −.08, β = −.21, SE = .02, p < .001, 95% CI [−.108, −.043]) and with age (b = −.06, β = −.17, SE = .02, p = .01, 95% CI [−.106, −.013]). As the number of comorbidities increased, so did stress levels (b = .55, β = .17, SE = .25, p = .03, 95% CI [.071, 1.045]). BMI, education level, and chemotherapy treatment were not related to stress (ps > .39). Lastly, increases in survivors’ age were associated with higher cytokine composite levels (b = .02, β = .16, SE = .01, p = .03, 95% CI [.003, .033]); time, BMI, education level, chemotherapy treatment, and comorbidities were not related to cytokine composite levels (ps > .10).
3.4. Alternative models
Although the purpose of this study was to assess the indirect effects of relationship satisfaction on inflammation through stress, it is possible that stress was indirectly related to inflammation through relationship satisfaction. Therefore, we tested alternative models with stress predicting changes in relationship satisfaction and in turn inflammation. For the model predicting CRP, fit indices indicated that the hypothesized model with relationship satisfaction as the predictor had better fit (AIC = 1825.72) than the alternative model with stress as the predictor (AIC = 1954.36). Similarly, model fit for the hypothesized model predicting the cytokine composite had better fit (AIC = 2064.40) than the alternative model (AIC = 2192.36). These results suggest that the hypothesized model with relationship satisfaction as the predictor should be retained. In addition, it is plausible that relationship satisfaction and stress combine to impact inflammation. We therefore tested models with interactions between relationship satisfaction and stress, rather than indirect effects. These interactions did not significantly predict CRP or cytokine composite levels at the within- or between-person levels (ps< .28), providing additional confidence in our proposed models.
4. Discussion
Consistent with our hypotheses, breast cancer survivors in highly satisfying romantic relationships felt less stressed and in turn had lower levels of inflammation throughout the study. The connection between satisfying relationships and lower stress and inflammation were shown when examining their associations both within and between survivors; at visits in which survivors were more satisfied with their relationships, they also reported less perceived stress than usual, which ultimately was related to lower than their own average CRP and cytokine levels. Likewise, greater relationship satisfaction throughout the study was associated with lower perceived stress, which in turn was linked with lower levels of the inflammatory markers. These findings illustrate the utility of a within-person approach to not only consider the average effects of relationship satisfaction, but also how changes in a survivor’s own relationship satisfaction impact stress and inflammation over time.
Importantly, the beneficial effects of survivors’ satisfying relationships on inflammation were indirect through lower stress; that is, relationship satisfaction was not directly associated with inflammation. Identifying perceived stress as a psychological pathway through which relationships influence immune function helps to explain why prior work showed that marital satisfaction was not directly associated with inflammation (Uchino et al., 2018); thus, perceived stress may be a key link when considering connections between relationship satisfaction and immune function. Indeed, prior work has demonstrated the intervening role of psychological mechanisms on the link between relationships and biological health (Robles et al., 2014; Robles and Kiecolt-Glaser, 2003; Slatcher and Selcuk, 2016). This study paves the way for future research to assess additional psychological and affective pathways that may connect relationship perceptions to inflammation, particularly among those who have a high risk for inflammation-related health problems, such as breast cancer survivors.
Previous research has repeatedly shown ties between relationship quality and immune function in healthy populations. For example, people in satisfying and less distressing relationships had better immune regulation and less inflammation after vaccination (Phillips et al., 2006), during supportive and conflictual marital interactions (Kiecolt-Glaser et al., 2005, 2003), and over a two-year period (Jaremka et al., 2013b). The present study extends these findings to breast cancer survivors and provides evidence for relationship satisfaction as a robust predictor of survivors’ inflammation. Breast cancer survivors with elevated inflammation have a high risk for cancer recurrence, premature mortality, and developing serious comorbid health conditions such as cardiovascular disease, osteoporosis, and diabetes (Aggarwal et al., 2006; Alfano et al., 2017; Pierce et al., 2009; Smyth et al., 2000). Fostering survivors’ relationships and encouraging survivors to draw on and connect with their partners may help reduce their inflammation and promote their long-term health. As clinicians caring for cancer survivors work to implement screening for distress in accordance with national guidance from the American College of Surgeons’ Commission on Cancer (2020) and the American Society of Clinical Oncology (Andersen et al., 2014), these results underscore the need for screening for relationship satisfaction and referral for couples’ counseling when appropriate.
These findings also fit within previous research demonstrating how satisfying relationships promote breast cancer survivors’ health. For instance, survivors had better adjustment to their diagnosis and treatment when their partners were supportive (Manne et al., 2005), open to discussing personal feelings and cancer-related concerns (Manne et al., 2004b), and made survivors feel accepted, understood, and cared for (Manne et al., 2004a). The current study contributes to the literature by revealing the importance of survivors’ relationships in how their stress and inflammation changed before and after treatment. Thus, not only can satisfying relationships enhance how survivors deal with their cancer-related emotional and physical health consequences, fluctuations in survivors’ relationship satisfaction can also help to lower their stress and inflammation throughout treatment. These findings also provide insight into how changes in relationship satisfaction may contribute to stress and inflammation in other illness contexts. For instance, when managing an illness with a slow onset, people may not experience as many changes, or as intense changes, in their relationships. However, the uncertainty about a disease’s progression or the unpredictability in symptom flare-ups over many years may wear on relationships, reducing their typical salutary effects. Thus, future research can draw on the current study to understand how relationships connect to inflammation across several illnesses.
The current study also has important implications for understanding how to leverage breast cancer survivors’ relationships to promote health. Much of the research connecting romantic relationships to health demonstrates a harsher effect of stress on women’s health than that of men (Kiecolt-Glaser and Newton, 2001; Umberson et al., 2006). In addition, research has focused on how the negative aspects of relationships harm health, neglecting the positive aspects of relationships that may bolster health in times of stress (Robles and Kiecolt-Glaser, 2003). The present study addresses these gaps by emphasizing the positive aspects of relationships and by focusing on women’s health. By exploring these important avenues, the findings demonstrated that satisfying relationships indeed were linked to lower stress and in turn lower inflammation during early breast cancer survivorship, providing evidence for a novel health-promoting effect of women’s satisfying relationships.
Key study strengths include assessment of survivors from breast cancer diagnosis to 18 months after cancer treatment. In particular, the pre-treatment assessment helped to push the boundaries of our current knowledge of how romantic relationships contribute to survivors’ inflammation before receiving treatment and during early survivorship. Moreover, the longitudinal examination allowed for comparison both between and among survivors, providing novel insight into how changes in a survivor’s relationship satisfaction from visit to visit predicted changes in stress and inflammation across the study. This work also identified perceived stress as mechanistic pathway through which satisfying relationships are linked with breast cancer survivors’ inflammation. Additionally, examination of low-grade inflammation and proinflammatory cytokines demonstrated ties between relationship satisfaction, stress, and inflammation across several important inflammatory markers.
One limitation of this study was the diversity of the sample. Though the current study showed that relationship satisfaction was linked to inflammation through lower stress while accounting for important confounds, such as BMI, age, education level, comorbidities, and cancer treatment, participants’ demographic characteristics were fairly homogenous. Although the current study controlled for the effects of cancer treatment, the group sizes for treatment type and cancer stage were too small to assess indirect effects of relationship satisfaction on inflammation within these specific sub-groups. Researchers should examine how relationship perceptions impact survivors’ inflammation, directly and indirectly, based on how intensive their treatment is and the stage of their diagnosis. In addition, we cannot draw conclusions about the role of physiological stress. Among cancer survivors, greater physiological stress promotes inflammation-related symptoms such as fatigue (Fagundes et al., 2011), and physiological and psychological stress often work in tandem to influence health (Kiecolt-Glaser, 2018). Future work assessing breast cancer survivors’ psychological and physiological stress is needed to tease apart their effects.
In this longitudinal study on breast cancer survivors, we demonstrated that high relationship satisfaction was associated with lower stress and in turn inflammation levels within and between survivors. At visits in which survivors were more satisfied with their relationships, they also perceived less stress, which was associated with lower than their own average levels of inflammation. Likewise, survivors who were satisfied with their romantic relationship throughout the study also perceived less stress and consequently had lower average inflammation levels. This research paves the way for future studies to explore the effects of relationships on inflammation in cancer survivors, as well as provides psychological and immunological pathways through which strong, satisfying relationships promote health.
Highlights.
Breast cancer survivors completed visits before and 6 and 18 months after treatment
When survivors were more satisfied with their relationship, they were less stressed
In turn, feeling less stressed was related to lower inflammation levels
Longitudinal examination demonstrated associations between and within survivors
We show utility of within-person approaches to assess survivors’ changes over time
Funding:
Work on this project was supported by NIH grants CA131029, UL1TR000090, CA016058, and K05 CA172296.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflict of interest to report.
References
- Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G, 2006. Inflammation and cancer: How hot is the link? Biochem. Pharmacol 72, 1605–1621. 10.1016/j.bcp.2006.06.029 [DOI] [PubMed] [Google Scholar]
- Alfano CM, Peng J, Andridge RR, Lindgren ME, Povoski SP, Lipari AM, Agnese DM, Farrar WB, Yee LD, Carson WE, Kiecolt-Glaser JK, 2017. Inflammatory cytokines and comorbidity development in breast cancer survivors versus noncancer controls: Evidence for accelerated aging? J. Clin. Oncol 35, 149–156. 10.1200/JCO.2016.67.1883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, DeRubeis RJ, Berman BS, Gruman J, Champion VL, Massie MJ, Holland JC, Partridge AH, Bak K, Somerfield MR, Rowland JH, 2014. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology guideline adaptation. J. Clin. Oncol 32, 1605–1619. 10.1200/JCO.2013.52.4611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM, 2006. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychol. Methods 11, 142–163. 10.1037/1082-989X.11.2.142 [DOI] [PubMed] [Google Scholar]
- Brauer M, Curtin JJ, 2018. Linear mixed-effects models and the analysis of nonindependent data: A unified framework to analyze categorical and continuous independent variables that vary within-subjects and/or within-items. Psychol. Methods 23, 389–411. 10.1037/met0000159 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R, 1983. A global measure of perceived stress. J. Health Soc. Behav 24, 385–396. [PubMed] [Google Scholar]
- Commission on Cancer, 2020. Optimal resources for cancer care: 2020 Standards. 1–106.
- Fagundes CP, Murray DM, Hwang BS, Gouin JP, Thayer JF, Sollers JJ, Shapiro CL, Malarkey WB, Kiecolt-Glaser JK, 2011. Sympathetic and parasympathetic activity in cancer-related fatigue: More evidence for a physiological substrate in cancer survivors. Psychoneuroendocrinology 36, 1137–1147. 10.1016/j.psyneuen.2011.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk JL, Rogge RD, 2007. Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the couples satisfaction index. J. Fam. Psychol 21, 572–583. 10.1037/0893-3200.21.4.572 [DOI] [PubMed] [Google Scholar]
- Graham JE, Glaser R, Loving TJ, Malarkey WB, Stowell JR, Kiecolt-Glaser JK, 2009. Cognitive word use during marital conflict and increases in proinflammatory cytokines. Heal. Psychol 28, 621–630. 10.1037/a0015208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB, 2010. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 7 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Glaser R, Loving TJ, Malarkey WB, Stowell JR, Kiecolt-Glaser JK, 2013a. Attachment anxiety is linked to alterations in cortisol production and cellular immunity. Psychol. Sci 24, 272–279. 10.1177/0956797612452571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Glaser R, Malarkey WB, Kiecolt-Glaser JK, 2013b. Marital distress prospectively predicts poorer cellular immune function. Psychoneuroendocrinology 38, 2713–2719. 10.1016/j.psyneuen.2013.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayser K, Scott JL, 2008. Helping couples cope with women’s cancers: An evidence-based approach for practitioners. New York: Springer Science+Business Media. [Google Scholar]
- Kiecolt-Glaser JK, 2018. Marriage, divorce, and the immune system. Am. Psychol 73, 1098–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, Glaser R, 2005. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Arch. Gen. Psychiatry 62, 1377–1384. 10.1001/archpsyc.62.12.1377 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL, 2001. Marriage and health: His and hers. Psychol. Bull 127, 472–503. 10.1037/0033-2909.127.4.472 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R, 2003. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc. Natl. Acad. Sci. U. S. A 100, 9090–9095. 10.1073/pnas.1531903100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Wilson SJ, 2017. Lovesick: How Couples’ Relationships Influence Health. Annu. Rev. Clin. Psychol 13, 421–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Wilson SJ, Bailey ML, Andridge R, Peng J, Jaremka LM, Fagundes CP, Malarkey WB, Laskowski B, Belury MA, 2018. Marital distress, depression, and a leaky gut: Translocation of bacterial endotoxin as a pathway to inflammation. Psychoneuroendocrinology 98, 52–60. 10.1016/j.psyneuen.2018.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Kashy DA, Spillers RL, Evans TV, 2010. Needs assessment of family caregivers of cancer survivors: Three cohorts comparison. Psychooncology. 19, 573–582. 10.1002/pon.1597 [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Rini C, Fox K, Goldstein L, Grana G, 2004a. The interpersonal process model of intimacy: the role of self-disclosure, partner disclosure, and partner responsiveness in interactions between breast cancer patients and their partners. J. Fam. Psychol 18, 589–599. 10.1037/0893-3200.18.4.589 [DOI] [PubMed] [Google Scholar]
- Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, Fox K, 2004b. Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. J. Consult. Clin. Psychol 10.1037/0022-006X.72.4.660 [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff JS, Norton TR, Fox K, Goldstein L, Grana G, 2006. Cancer-related relationship communication in couples coping with early stage breast cancer. Psychooncology. 15, 234–247. 10.1002/pon.941 [DOI] [PubMed] [Google Scholar]
- Manne SL, Siegel S, Kashy D, Heckman CJ, 2014. Cancer-specific relationship awareness, relationship communication, and intimacy among couples coping with early stage breast cancer. J. Soc. Pers. Relat 31, 314–334. 10.1177/0265407513494950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Winkel G, Ostroff J, Grana G, Fox K, 2005. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: Patient and partner perspectives. Heal. Psychol 24, 635–641. 10.1037/0278-6133.24.6.635 [DOI] [PubMed] [Google Scholar]
- Mundy-Bosse BL, Thornton LM, Yang HC, Andersen BL, Carson WE, 2011. Psychological stress is associated with altered levels of myeloid-derived suppressor cells in breast cancer patients. Cell. Immunol 270, 80–87. 10.1016/j.cellimm.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips AC, Carroll D, Burns VE, Ring C, Macleod J, Drayson M, 2006. Bereavement and marriage are associated with antibody response to influenza vaccination in the elderly. Brain. Behav. Immun 20, 279–289. 10.1016/j.bbi.2005.08.003 [DOI] [PubMed] [Google Scholar]
- Pierce BL, Ballard-Barbash R, Bernstein L, Baumgartner RN, Neuhouser ML, Wener MH, Baumgartner KB, Gilliland FD, Sorensen BE, McTiernan A, Ulrich CM, 2009. Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J. Clin. Oncol 27, 3437–3444. 10.1200/JCO.2008.18.9068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietromonaco PR, Collins NL, 2017. Interpersonal mechanisms linking close relationships to health. Am. Psychol 72, 531–542. 10.1037/amp0000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell ND, Tarr AJ, Sheridan JF, 2013. Psychosocial stress and inflammation in cancer. Brain. Behav. Immun 30, S41–S47. 10.1016/j.bbi.2012.06.015 [DOI] [PubMed] [Google Scholar]
- Robles TF, Kiecolt-Glaser JK, 2003. The physiology of marriage: Pathways to health. Physiol. Behav 79, 409–416. 10.1016/S0031-9384(03)00160-4 [DOI] [PubMed] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM, 2014. Marital quality and health: A meta-analytic review. Psychol. Bull 140, 140–187. 10.1037/a0031859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwood NJ, Hayes AF, 2017. MLmed: An SPSS macro for multilevel mediation and conditional process analysis Poster Present. Annu. Meet. Assoc. Psychol. Sci. (APS), Boston, MA. [Google Scholar]
- Schoebi D, Randall AK, 2015. Emotional dynamics in intimate relationships. Emot. Rev 7, 342–348. 10.1177/1754073915590620 [DOI] [Google Scholar]
- Shrout MR, 2019. Couples and nonvisible chronic illness: An integrated model of dyadic Coping. Dissertation 23, 2019. [Google Scholar]
- Slatcher RB, Selcuk E, 2016. A social psychological perspective on the links between close relationships and health. Curr. Dir. Psychol. Sci 26, 16–21. 10.1177/0963721416667444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth MJ, Cretney E, Kershaw MH, Hayakawa Y, 2004. Cytokines in cancer immunity and immunotherapy. Immunol. Rev 202, 275–293. 10.1111/j.0105-2896.2004.00199.x [DOI] [PubMed] [Google Scholar]
- Smyth MJ, Taniguchi M, Street SEA, 2000. The anti-tumor activity of IL-12: Mechanisms of innate immunity that are model and dose dependent. J. Immunol 165, 2665–2670. 10.4049/jimmunol.165.5.2665 [DOI] [PubMed] [Google Scholar]
- Uchino BN, 2004. Social support and physical health: Understanding the health consequences of relationships., Social support and physical health: Understanding the health consequences of relationships., Current perspectives in psychology. Yale University Press, US. [Google Scholar]
- Uchino BN, de Grey RGK, Cronan S, Smith TW, Diener E, Joel S, Bosch J, 2018. Life satisfaction and inflammation in couples: An actor–partner analysis. J. Behav. Med 41, 22–30. 10.1007/s10865-017-9880-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers DA, Liu H, Needham B, 2006. You make me sick: Marital quality and health over the life course. J. Health Soc. Behav 47, 1–16. 10.2307/30040295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber KM, Solomon DH, 2008. Locating relationship and communication issues among stressors associated with breast cancer. Health Commun. 23, 548–559. 10.1080/10410230802465233 [DOI] [PubMed] [Google Scholar]


