Abstract
Background: Electronic cigarettes (e-cigarettes) are increasing in popularity in the United States. Prior prevalence estimates of e-cigarette use in pregnancy range from 1% to 15%.
Materials and Methods: We assessed prevalence of e-cigarette and conventional cigarette use during preconception or pregnancy in a large sample of racially/ethnically diverse, low-income pregnant women via telephone survey (2015–2018) and compared sociodemographic characteristics and mental health conditions.
Results: Of 1365 pregnant women surveyed, 54 (4.0%) reported e-cigarette use (regardless of other tobacco use), 372 (27.3%) reported conventional cigarette use without e-cigarette use (conventional cigarette use), and 939 (68.8%) reported no tobacco or nicotine replacement therapy (NRT) product use during the preconception period and/or pregnancy. Seventy-four percent of women using e-cigarettes reported also using conventional cigarettes. Women who used e-cigarettes were more likely to report high school education or greater, income <$30,000, White race, and non-Hispanic ethnicity than women who used conventional cigarettes. Women who used e-cigarettes were more likely than women who used conventional cigarettes or no tobacco/NRT to report symptoms of depression. Women who used e-cigarettes and women who used conventional cigarettes were more likely than women who used no tobacco/NRT to report a history of severe mental health conditions, alcohol use during pregnancy, and marijuana or other drug use during preconception.
Conclusions: In this sample, 4% of women used e-cigarettes during preconception and/or pregnancy and most also used conventional cigarettes. Increased efforts by providers to screen for tobacco (including use of e-cigarette) and polysubstance use and to provide cessation services could improve outcomes of mothers and children.
Keywords: smoking, nicotine, substance abuse, mental health, obstetrics
Introduction
Electronic cigarettes (e-cigarettes) are devices that heat a liquid (usually containing nicotine1) to generate aerosol that is inhaled. E-cigarettes were patented in 20032 and began to appear in the United States in 2007.2 E-cigarette use is rapidly increasing in the United States among adolescents and young adults,3–5 and many individuals who use e-cigarettes, including pregnant women, are motivated by a perception that e-cigarettes are safer than conventional cigarettes and an effective aid in cigarette smoking cessation.6,7 The long-term health effects of e-cigarette use are largely unknown, but e-cigarette aerosols can contain harmful substances such as heavy metals, volatile organic compounds, and cancer-causing agents.2,8 Most e-cigarettes contain nicotine, which is a known reproductive and developmental toxicant.2,9
The American College of Obstetricians and Gynecologists (ACOG) recommends that obstetric providers screen all patients for use of any tobacco or nicotine products, including e-cigarettes.10 However, England et al. found that 40% of obstetric providers reported that they did not ever screen pregnant women for noncombustible tobacco product use.11 Given the increasing popularity of e-cigarettes and the potential risks of e-cigarette use during pregnancy, identifying the prevalence of e-cigarette use among women near the time of conception and during pregnancy and characteristics associated with e-cigarettes use may inform clinical and preventive interventions. For example, this information could help direct tobacco screening recommendations by identifying high-risk groups, such as those with co-occurring mental health issues. A small number of prior studies have assessed the prevalence of e-cigarette use in small samples of pregnant women. Within the United States, the rates range from 0.06% (n = 326) in a university sample to 15.1% (n = 286) in a national online sample of pregnant women.12–14 One nationally representative sample of pregnant women in the United States in 2013–2014 (n = 388 pregnant women) found that 4.9% reported use of e-cigarettes, a prevalence estimate among tobacco products that was second only to that of conventional cigarette use.15 The largest study to date (n = 3277) sampled from two states in the Southwestern United States in 2016 and reported a prevalence of 1.4% in the last 3 months of pregnancy, but a prevalence of 7% during the period from 3 months before pregnancy through time of survey (2–6 months postpartum).16 Finally, in a nationally representative sample based on data from the National Health Interview Survey (2014–2017), 3.6% of pregnant women (total n = 1071) used e-cigarettes, which was similar to the rate of use in nonpregnant women of reproductive age (total n = 26,849).14
The current study extends prior studies by using a more recent sample of pregnant women assessed between 2015 and 2018. Specifically, we measured e-cigarette use in a sample of 1365 racially/ethnically diverse, low-income pregnant women. The data were collected from telephone screening surveys that were part of several larger studies of tobacco use during the preconception period and/or pregnancy. Data were analyzed to address the following aims: (1) What is the prevalence of e-cigarette use in the preconception period and/or during pregnancy? (2) What are the sociodemographic characteristics of individuals who used e-cigarettes in the preconception period and/or during pregnancy and how do they compare to women who used conventional cigarettes without e-cigarettes and to women who do not use any tobacco products? (3) Are there differences in the prevalence of mental health conditions and in the use of other substances in women who used e-cigarettes versus women who used conventional cigarettes without e-cigarettes or no tobacco products in preconception and/or pregnancy?
Materials and Methods
Participants
Participants included in this study completed a telephone survey as a part of two larger studies that focused on effects of maternal cigarette smoking on fetal and infant neurodevelopment. Participants included in this study were assessed with the telephone survey in January 2015 through April 2018 (n = 1365). The survey included questions about tobacco product use (conventional cigarettes, e-cigarettes, hookah, herbal cigarettes, cigars, cigarillos, chewing tobacco, pipes, snuff, snus, and other forms) and nicotine replacement therapy (NRT) product use (nicotine patches, gum, or lozenges) during the preconception period and/or pregnancy. Participants who reported using e-cigarettes were included in the e-cigarette use category regardless of whether they also used conventional cigarettes, other tobacco products, or NRT. Participants who reported using conventional cigarettes and not e-cigarettes were included in the conventional cigarette use category, regardless of whether they also used other tobacco products or NRT. Participants using no tobacco or NRT products were considered unexposed and were classified in the no tobacco/NRT group. Participants who did not use conventional cigarettes or e-cigarettes, but reported using other tobacco or NRT products were excluded from analysis. In total, the survey was administered to 1476 women. Of those, 111 (7.5%) reported using other tobacco or nicotine products but not conventional cigarettes or e-cigarettes and were excluded from further analysis. All participants were pregnant and 16–45 years old at the time of the survey.
Procedures
Telephone survey
Participants were recruited for the telephone survey through active recruitment at a single, low-income, urban clinic and through flyers and advertisements at local obstetric offices and community centers. Participants provided verbal consent to a telephone survey to determine eligibility for two larger studies that focused on effects of maternal cigarette smoking on fetal and infant neurodevelopment. The telephone survey was completed before participation in the larger studies to determine eligibility for the larger studies. Participants completed a series of survey questions over the telephone including items pertaining to tobacco or nicotine use, substance and alcohol use, mental health, medications, and demographic information. The study was approved by the local Institutional Review Board (Women and Infants Hospital, FWA No. 00000056).
Measures
Demographic and obstetric factors
Demographic variables included maternal age at the time of survey (in years), number of people in their household, number of children, income, education, and race/ethnicity. Obstetrical factors included estimated gestational age (EGA) at the time of survey. Annual household income was reported as a categorical variable that was consolidated into the following categories: <$30,000; $30,000–49,999; $50,000–74,999; $75,000–99,999; and ≥$100,000. Highest level of education was reported as a categorical variable that was consolidated into the following categories: less than high school; high school diploma/GED; some college or Associate's degree; college degree or greater. In the telephone survey, respondents were asked to select the race and ethnicity identities with which they most closely identify and were encouraged to select as many categories as applied. Participants were also given the option to select “other” and to name the other category if no listed categories were appropriate. Write-in responses were recoded if appropriate (e.g., if two race groups were written in, a category of “multiracial” was assigned). For the purpose of analyses, responses were consolidated into the following categories: non-Hispanic Asian American, non-Hispanic Black or African American, non-Hispanic Native American or Alaska Native, non-Hispanic White, multiracial, or another race (here “other” was combined with Native Hawaiian, or Pacific Islander because of small numbers); Hispanic/Latinx. Participants were coded as multiracial if they selected more than one racial category or selected the “multiracial” category. Household income, race/ethnicity, and education were all also analyzed as dichotomous variables (less than or greater than $30,000 per year; non-Hispanic White or other race/ethnicity; and less than high school or high school and above, respectively). EGA was calculated based on participant report of last menstrual period or ultrasound.
Tobacco product use
To assess for e-cigarette use before and during pregnancy, respondents were asked, Are you currently using any of the following tobacco or nicotine products? If respondents reported tobacco or nicotine use, they were prompted to select the type of product from a list. Respondents were considered to have used e-cigarettes if they selected the e-cigarette category (e-cigarettes, vaping, e-hookah or hookah pens, e-juice, vape pipes or pens, ENDS). (ENDS are electronic nicotine delivery systems.) Participants were then asked, Did you use any of those products I listed during this pregnancy or 3 months prior to pregnancy? followed by a presentation of the same options as the previous item. As previously described, participants were included in the “e-cigarette use” category if they reported any e-cigarette use in the 3 months before pregnancy (referred to as “preconception”) and/or during pregnancy, regardless of whether they also used conventional cigarettes, other tobacco products, or NRT. To assess conventional cigarette use before and/or during pregnancy, respondents were first asked, Do you smoke cigarettes? Those who responded “yes” were asked, Approximately how many cigarettes have you smoked per day during your pregnancy? Did you use any of those products I listed during this pregnancy or 3 months prior to pregnancy? Respondents who were not current smokers were asked, Did you smoke at all during this pregnancy or in the 3 months prior to pregnancy? Those who responded “yes” were asked how many cigarettes they smoked per day during that period. Respondents were included in the “conventional cigarette use” category if they reported conventional cigarette use in preconception and/or pregnancy but did not use e-cigarettes, regardless of whether they also used other tobacco products or NRT. Participants were only included in the “no tobacco/NRT use” category if they did not use any tobacco or NRT products of any kind in preconception and/or pregnancy.
Mental health
Women were categorized as having symptoms of depression during pregnancy if they responded yes to both questions, During your pregnancy, did you ever feel depressed or down or sad or irritable or lost pleasure in things you usually enjoy? and Did you feel like this most of the day, nearly every day, for 2 weeks or more? Women were not asked about symptoms of depression before pregnancy. Women were also asked whether they had ever been diagnosed with bipolar disorder, schizophrenia, schizoaffective disorder, or psychosis; those responding “yes” were categorized as having a severe mental health condition.
Alcohol, marijuana, and other substance use
A series of questions were administered to determine alcohol use during pregnancy and to assess marijuana use and other substance use in the 3 months before pregnancy. Respondents were considered to have used alcohol during their pregnancy if they responded “yes” to the question, Have you drunk any alcohol during this pregnancy, including the weeks before you found out? Those who responded “yes” were asked, How many drinks per week on average? Because of the potential for stigma, we assessed the use of marijuana and other illicit drugs only during the preconception period. Respondents were considered to have used marijuana if they responded “yes” to the question, In the 3 months prior to this pregnancy, did you use marijuana? Following a section on alcohol, tobacco, and marijuana, respondents were also asked, In the 3 months prior to this pregnancy, did you use other drugs? Those who responded “yes” were considered to have used other drugs in the preconception period.
Statistical analyses
Analyses were performed using Stata Version 15. Sample characteristics included demographic factors, gestational age, tobacco or nicotine product use, mental health and alcohol, marijuana, and other substance use, as previously described. Means and frequencies for study variables were generated across tobacco product use categories, and global tests of differences were conducted. For continuous variables, analysis of variance was used to produce an F-statistic and associated p-value. For binary, ordinal, and categorical variables, a chi square statistic was generated with associated p-value. p-Values of ≤0.05 were considered statistically significant.
If global tests indicated differences across tobacco product use categories for a specific variable, differences were independently assessed in two separate regression models where tobacco product use category was the independent variable. In one model, “conventional cigarette use” was set as the referent value, and in the other, “no tobacco use” was set as the referent value. Count variables were modeled using negative binomial regression for variables that were highly dispersed (number of drinks per week and number of cigarettes per day), or Poisson regression (number of children and number of people in household), which both generate incidence rate ratios. Incidence rate ratios can be interpreted as the magnitude of the increase or decrease in the count variable associated with moving from the referent category (no tobacco use or conventional cigarette use) to the comparison category (e-cigarette use or conventional cigarette use). The association between tobacco product use category and binary variables (income less than or greater than $30,000 per year; non-Hispanic White or other race/ethnicity; and less than high school or high school and above) was analyzed using logistic regression to generate odds ratios (ORs). Because the number of women who used e-cigarettes was small, all regression analyses were unadjusted.
Results
Prevalence of e-cigarette use in pregnancy
As shown in Table 1, in our sample of 1365 pregnant women, 4.0% (n = 54) reported e-cigarette use, 27.3% (n = 372) reported conventional cigarette use, and 68.8% (n = 939) reported no tobacco product use during preconception and/or pregnancy. Of women who reported e-cigarette use, 74.1% (n = 40) also reported conventional cigarette use, while 25.9% reported only e-cigarette use. More women reported e-cigarette use during preconception and/or pregnancy in 2015–2016 (4.7%) than 2017–2018 (2.4%) (p = 0.046).
Table 1.
Sample Characteristics by Tobacco Product Use in Preconception and/or Pregnancy, 2015–2018 (N = 1365)
| |
E-cigarette use,a(4%/n = 54) |
Conventional cigarette use,a(27%/n = 372) |
No nicotine use (69%/n = 939) |
Total (N = 1365) |
|---|---|---|---|---|
| N (%) | ||||
| Race/ethnicity | ||||
| Black/African American, non-Hispanic | 4 (7.4) | 63 (16.9) | 159 (16.9) | 226 (16.5) |
| White, non-Hispanic | 35 (64.8) | 160 (43.0) | 294 (31.3) | 489 (35.8) |
| Hispanic/Latinx | 1 (1.9) | 61 (16.4) | 277 (29.5) | 339 (24.8) |
| Asian American, non-Hispanic | 0 (0.0) | 2 (0.1) | 29 (3.1) | 31 (2.3) |
| Native American/Alaska Native, non-Hispanic | 1 (1.9) | 13 (3.5) | 18 (1.9) | 32 (2.3) |
| Multiracial, non-Hispanic | 11 (20.4) | 54 (14.5) | 132 (14.1) | 197 (14.4) |
| Another race, non-Hispanicb | 0 (0.0) | 0 (0.0) | 6 (0.6) | 6 (0.4) |
| Missing | 2 (3.7) | 19 (5.1) | 24 (2.6) | 45 (3.3) |
| Education | ||||
| Less than HS | 14 (25.9) | 150 (40.3) | 266 (28.3) | 430 (31.5) |
| HS/GED | 22 (40.7) | 122 (32.8) | 294 (31.3) | 438 (32.1) |
| Some college/associate's degree | 13 (24.1) | 67 (18.0) | 175 (18.6) | 255 (18.7) |
| College or greater | 4 (7.4) | 25 (6.7) | 178 (18.9) | 207 (15.2) |
| Missing | 1 (1.9) | 9 (2.4) | 26 (2.8) | 35 (2.6) |
| Income >$30,000/year | 20 (43.5) | 68 (21.3) | 336 (39.9) | 424 (35.2) |
| Depression symptoms during pregnancy | 13 (32.5) | 61 (18.9) | 83 (10.11) | 157 (13.3) |
| Serious mental health conditions | 8 (20.0) | 51 (15.5) | 37 (4.5) | 96 (8.0) |
| Marijuana (preconception)c | 21 (38.9) | 157 (43.0) | 151 (16.1) | 329 (24.2) |
| Other drugs (preconception)c,d | 2 (4.9) | 13 (4.0) | 1 (0.1) | 16 (1.3) |
| Alcohol during pregnancy | 20 (48.8) | 120 (37.7) | 166 (20.2) | 306 (25.9) |
| Mean (SD) | ||||
|---|---|---|---|---|
| Maternal age (years) |
26.8 (5.6) |
27.4 (5.1) |
27.0 (5.2) |
27.1 (5.2) |
| Cigarettes per daye |
8.9 (6.4) |
6.2 (4.9) |
0.0 (0.0) |
1.1 (3.2) |
| No. of children |
1.1 (1.2) |
1.3 (1.5) |
1.1 (1.2) |
1.14 (1.3) |
| No. of people in household |
3.6 (1.7) |
3.4 (1.7) |
3.3 (1.4) |
3.32 (1.5) |
| Drinks per weeke | 4.30 (6.5) | 4.2 (7.4) | 1.7 (2.1) | 2.86 (5.3) |
E-cigarette use defined as e-cigarette use regardless of conventional cigarette, other tobacco product, or NRT product use. Conventional cigarette use defined as conventional cigarette use and not e-cigarette use, regardless of other tobacco products or NRT product use. No nicotine use defined as no e-cigarette, conventional cigarette, other tobacco, or NRT product use.
Another race consisted of race category selection “other” combined with Native Hawaiian or Pacific Islander.
Preconception is defined as the 3 months before pregnancy.
Other drugs refers to any substances other than tobacco and nicotine products, alcohol, and marijuana.
Cigarettes per day and drinks per week analyses included only participants who reported any cigarette before or during pregnancy and any alcohol use during pregnancy, respectively.
e-cigarette, electronic cigarettes; HS, high school; NRT, nicotine replacement therapy; SD, standard deviation.
Sociodemographic characteristics
Characteristics of the sample by tobacco product use category are shown in Table 1. Mean maternal age was 27.1 (standard deviation [SD] = 5.2), and the average gestational age at the time of the survey was 13.7 weeks (SD = 9.2). The majority of participants (64.8%) reported an income below or equal to $30,000 per year, and 65.3% reported they had attained a high school education or less. Our sample was reflective of the racial and ethnic demographics of Southern New England, with 25.7% identifying as Hispanic/Latinx, 37.1% non-Hispanic White, 17.1% non-Hispanic Black or African American, 2.4% non-Hispanic Asian American, 2.4% non-Hispanic Native American or Alaska Native, and 14.9% non-Hispanic multiracial. A small percentage (3.3%) of women did not identify with one of the above listed racial identities or chose not to respond.
Likelihood of sociodemographic characteristics by tobacco product use category are shown in Table 2. Women who reported e-cigarette use in preconception and/or pregnancy were more likely to identify racially and ethnically as non-Hispanic White compared to women who reported conventional cigarette use (OR = 2.48; 95% confidence interval [CI] = 1.34–4.60) and compared to women who reported no tobacco use (OR = 4.25; 95% CI = 2.40–7.89). Women who reported e-cigarette use were significantly more likely to have completed education beyond high school (OR = 1.95; 95% CI = 1.02–3.72) compared to women who reported conventional cigarette use. Additionally, women who reported e-cigarette use were more likely to have an annual household income >$30,000 than women who reported conventional cigarette use (OR = 2.84; 95% CI = 1.49–5.39).
Table 2.
Likelihood of Selected Study Variables Associated with Tobacco Use in Preconception and/or Pregnancy
| E-cigarette use compared to no tobacco/NRT usea |
E-cigarette use compared to conventional cigarette usea |
Conventional cigarettes use compared to no tobacco/NRT usea |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Logistic regression | |||||||||
| OR | p | 95% CI | OR | p | 95% CI | OR | p | 95% CI | |
| White, non-Hispanic | 4.25 | <0.001 | 2.40 to 7.89 | 2.48 | 0.004 | 1.34 to 4.60 | 1.75 | <0.001 | 1.36 to 2.25 |
| Income >$30,000 | 1.16 | 0.635 | 0.64 to 2.10 | 2.84 | 0.001 | 1.49 to 5.39 | 0.41 | <0.001 | 0.30 to 0.55 |
| Less than HS degree | 1.15 | 0.672 | 0.61 to 2.14 | 1.95 | 0.042 | 1.02 to 3.72 | 0.59 | <0.001 | 0.46 to 0.76 |
| Depression symptoms during pregnancy | 4.28 | <0.001 | 2.13 to 8.62 | 2.06 | 0.048 | 1.00 to 4.22 | 2.07 | <0.001 | 1.45 to 2.98 |
| Serious mental health conditions | 5.34 | <0.001 | 2.30 to 12.40 | 1.36 | 0.470 | 0.59 to 3.11 | 3.94 | <0.001 | 2.52 to 6.14 |
| Marijuana (preconception)b | 3.32 | <0.001 | 1.87 to 5.89 | 0.84 | 0.567 | 0.47 to 1.51 | 3.93 | <0.001 | 3.00 to 5.16 |
| Alcohol during pregnancy | 3.76 | <0.001 | 1.99 to 7.11 | 1.57 | 0.175 | 0.82 to 3.02 | 2.40 | <0.001 | 1.80 to 3.18 |
| Other drugs (preconception)b,c | 42.41 | 0.002 | 3.76 to 477.82 | 1.24 | 0.783 | 0.27 to 5.69 | 34.24 | 0.001 | 4.46 to 262.82 |
| Linear regression |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef. | p | 95% CI | Coef. | p | 95% CI | Coef. | p | 95% CI | |
| Maternal age (years) | −0.27 | 0.712 | −1.70 to 1.16 | −0.61 | 0.420 | −2.10 to 0.88 | 0.34 | 0.285 | −0.29 to 0.97 |
| Poisson regression |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| IRR | p | 95% CI | IRR | p | 95% CI | IRR | p | 95% CI | |
| No. of children |
1.00 |
0.993 |
0.74 to 1.36 |
0.80 |
0.16 |
0.59 to 1.09 |
1.25 |
<0.001 |
1.11 to 1.40 |
| No. of people in household | 1.10 | 0.275 | 0.93 to 1.29 | 1.08 | 0.405 | 0.91 to 1.28 | 1.02 | 0.592 | 0.95 to 1.09 |
| Negative binomial regression |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| IRR | p | 95% CI | IRR | p | 95% CI | IRR | p | 95% CI | |
| Cigarettes per dayd |
— |
— |
— |
1.43 |
0.051 |
1.00 to 2.05 |
— |
— |
— |
| Drinks per weekd | 2.49 | 0.002 | 1.40 to 4.42 | 1.03 | 0.915 | 0.58 to 1.84 | 2.41 | <0.001 | 1.78 to 3.27 |
E-cigarette use defined as e-cigarette use regardless of conventional cigarette, other tobacco product, or NRT product use. Conventional cigarette use defined as conventional cigarette use and not e-cigarette use, regardless of other tobacco products or NRT product use. No tobacco/NRT use defined as no e-cigarette, conventional cigarette, other tobacco, or NRT product use.
Preconception is defined as the 3 months before pregnancy.
Other drugs refers to any substances other than tobacco and nicotine products, alcohol, and marijuana.
Cigarettes per day and drinks per week analyses included only participants who reported any cigarette before or during pregnancy and any alcohol use during pregnancy, respectively.
Bold values indicate a statistically significant association.
CI, confidence interval; OR, odds ratio.
Concurrent mental health conditions
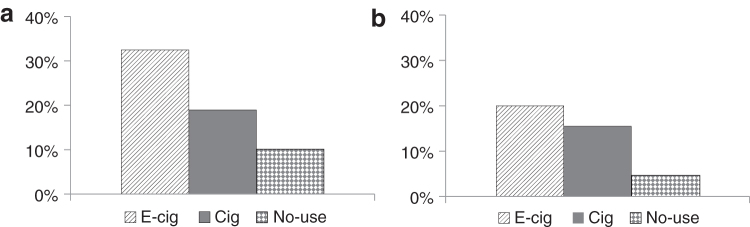
Likelihood of concurrent mental health conditions by category of tobacco product use is shown in Table 2. Women who reported e-cigarette use were more likely than women who reported conventional cigarette use (OR = 2.06, 95% CI = 1.00–4.22) and women who reported no tobacco use (OR = 4.28, CI = 2.13–8.62) to report symptoms of depression in pregnancy (Fig. 1a). Women who reported conventional cigarette use were more likely than women who reported no tobacco use to report symptoms of depression in pregnancy (OR = 2.07; 95% CI = 1.45–2.98). Compared to women who reported no tobacco use, both women who reported conventional cigarette use (OR = 3.94, 95% CI = 2.52–6.14) and women who reported e-cigarette use (OR = 5.34; 95% CI = 2.30–12.40) were more likely to have a history of a severe mental health condition (bipolar disorder, psychosis, schizoaffective disorder, or schizophrenia) (Fig. 1b).
FIG. 1.
Prevalence of mental health conditions and symptoms by tobacco product use in preconception and/or pregnancy. (a) Depression symptoms in pregnancy. (b) Severe mental health conditions. Cig, conventional cigarette users; E-Cig, electronic-cigarette users; No-use, no tobacco/NRT product use; NRT, nicotine replacement therapy.
Among women who reported e-cigarette use, the majority also reported using conventional cigarettes (74%). Among all women who used conventional cigarettes, women who used e-cigarettes smoked around 43% more conventional cigarettes per day than women who did not use e-cigarettes (i.e., 8.86 vs. 6.18 cigarettes per day), and this finding was statistically significant (incidence rate ratio [IRR]: 1.43, 95% CI = 1.00–2.05). Women who reported e-cigarette use were significantly more likely to have used alcohol during pregnancy compared to women who reported no tobacco use (OR = 3.76; 95% CI = 1.99–7.11). Women who reported e-cigarette use and who drank alcohol during pregnancy consumed 2.49 times the number of drinks per week compared to women who reported no tobacco use and who drank alcohol (i.e., 4.30 vs. 1.73 drinks per week; IRR = 2.49; 95% CI = 1.40–4.42). Women who reported e-cigarette use (OR = 3.32; 95% CI = 1.87–5.89) and women who reported conventional cigarette use (OR = 3.93, 95% CI = 3.00–5.16) were more likely to report having used marijuana in the preconception period compared to women who reported no tobacco use. Both women who reported e-cigarette use (OR = 42.41; 95% CI = 3.76–477.82) and women who reported conventional cigarette use (OR = 34.24; 95% CI = 4.46–262.82) were more likely than women who reported no tobacco use to have used one or more other drugs in the 3 months before pregnancy.
Discussion
Our study surveyed e-cigarette use in a large convenience sample of pregnant women in Southern New England. Of the 1365 pregnant women surveyed between 2015 and 2018, the prevalence of e-cigarette use during preconception and/or pregnancy was 4.0%, which is consistent with the most recent estimate from a nationally representative sample, 3.6%.14 Prior studies based on smaller convenience samples have reported prenatal e-cigarette use prevalence ranging from 0.06% to 15.1%.12,13,16 More than 70% of women in our sample who reported using e-cigarettes also reported using conventional cigarettes during preconception and/or pregnancy, and at least some of these women may have been using e-cigarettes and conventional cigarettes simultaneously. Earlier research has suggested that dual use of these two types of tobacco may be associated with higher odds of cardiovascular disease and with higher levels of biomarkers related tobacco exposure, such as 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol (NNAL) and N-nitrosonornicotin (NNN), than with exclusive use of conventional cigarettes.17,18 This finding is also consistent with previous studies among pregnant women and in the general population in which a high proportion of women using e-cigarettes also used conventional cigarettes.6,12,15 Women in this study who reported using e-cigarettes and conventional cigarettes also reported that they smoked more cigarettes on average in preconception and/or pregnancy than women who reported smoking only conventional cigarettes. To our knowledge, this is the first study on e-cigarette use in preconception and/or pregnancy to quantify conventional cigarette use according to the amount of use, rather than just the presence or absence of use.
In our sample of racially and ethnically diverse and low-income pregnant women, women who reported conventional cigarette use were significantly more likely to identify as non-Hispanic White than women who reported no tobacco use, which is similar to findings in other studies.12,15 In our study, women who reported using e-cigarettes were even more likely than women who reported conventional cigarette use to identify as non-Hispanic White. Other studies have also found that pregnant women who use e-cigarettes are more likely to identify as non-Hispanic White,6,12 but pregnant women who use e-cigarettes were not previously compared to pregnant women who used conventional cigarettes. Additionally, women who reported e-cigarette use were more likely than those who reported conventional cigarette use to have at least some higher education and an income of above $30,000. Previous studies have reported inconsistent findings regarding income and education characteristics of women who use e-cigarettes.12,13
To our knowledge, this study is the first to report rates of depression symptoms and severe mental health conditions in women who use e-cigarettes in preconception or pregnancy. One prior study reported higher rates of externalizing psychiatric symptoms in pregnant e-cigarette users than nonusers.15 Nearly one-third of women who reported e-cigarette use in this study had symptoms of depression in pregnancy, which was four times that of women who reported no tobacco use and twice that of women who reported conventional cigarette use. Prior studies have noted similar prevalence of depression (37.5%) in women who use conventional cigarettes in pregnancy19 and have demonstrated strong associations between nicotine addiction in pregnancy and current depressive symptoms.20,21 There are several possible explanations for associations between depression and e-cigarette use. Women may use nicotine in pregnancy to self-medicate, or cope with the symptoms of depression.11 Alternatively, depressive symptoms may make cessation more difficult.20,22 More research is needed to explore the link between depression in pregnancy and e-cigarette use.
Women who reported e-cigarette use and women who reported conventional cigarette use were more likely than women who reported no tobacco use to have a history of severe mental health conditions, such as schizophrenia, bipolar disorder, and other forms of psychosis. According to national surveys, prevalence of cigarette use among individuals diagnosed with a psychotic episode or disorder is much higher than prevalence in individuals with no psychiatric diagnosis (49.8% vs. 15.5%).23,24 Our study is the first to examine the prevalence of severe mental health conditions in women who used e-cigarettes during preconception and/or pregnancy. Tobacco cessation interventions may need to be tailored for this vulnerable population.
In addition to a higher prevalence of depressive symptoms and serious mental health conditions, we also found an increased likelihood of alcohol use in pregnancy and marijuana and other substance use before pregnancy in both categories of women who used tobacco (e-cigarette use and conventional cigarette use) compared with women who reported no tobacco use. Cigarette smoking and other substance use frequently co-occur: in the United States, more than half of all adults who meet diagnostic criteria for substance use disorder report current cigarette smoking, with lifetime smoking rates in this population reaching 75%.24 Similar patterns have been observed in the general population, among those who meet diagnostic criteria for alcohol use disorder 39% of this population reports current cigarette smoking, 65% reporting lifetime smoking.23 Among pregnant women, prevalence of alcohol use is substantially higher among women who smoke than those who do not smoke.25 Any alcohol consumption during pregnancy is considered by the USDA and others to be excessive.26
Many women believe that e-cigarettes are safer in pregnancy than conventional cigarettes.7,27,28 Prior research suggests that the general population regards the use of e-cigarettes in pregnancy as safer than cigarettes. Thus, there may be less social stigma and greater public acceptance of e-cigarettes compared to cigarettes, which may motivate some women to use e-cigarettes as an alternative to cigarettes.29–31 Women who use e-cigarettes during pregnancy cite cessation, safety, and reduced stigma as primary motivating factors for their use.9,29 A qualitative review of online forums found that while some women felt it was not safe to use e-cigarettes in pregnancy, many pregnant women viewed switching to e-cigarette use as safer than quitting “cold turkey” (without nicotine replacement) and safer than conventional cigarette smoking.28
Most e-cigarettes contain nicotine, which is a known developmental toxicant.9,32 Animal studies have demonstrated that prenatal nicotine exposure interferes with the formation of synapses and axons along with other neuromolecular functions resulting in problems with neurodevelopment and cognitive functioning.28–36 In addition to specific neurobehavioral effects, animal research has demonstrated systemic effects of prenatal nicotine exposure on physical health resulting in increased systemic inflammation and impaired pulmonary functioning.37,38 In addition to nicotine, prenatal e-cigarette use exposes the mother and fetus to flavoring chemicals and humectants, typically propylene glycol and vegetable glycerin. There are thousands of chemical compounds for flavoring available for e-cigarettes,39 some of which have been linked to harmful pulmonary effects in mice after prenatal exposure40,41 and cytotoxicity in human cells.42 Additional research is needed to better understand the specific health effects of e-cigarette use in pregnancy, alone and in combination with combusted cigarettes, and the potential effects of components other than nicotine, such as flavorings and other additives.
Our study was limited by several factors. These data were collected from a convenience sample in a small region in Northeastern United States and results cannot be extrapolated to other regions of the United States. However, the sample is highly diverse, and the race/ethnicity distribution is similar to that of the underlying source population. The study is also limited by the framing of survey questions, which asked whether participants used e-cigarettes and conventional cigarettes 3 months before pregnancy or during pregnancy, and did not specify at what specific time point in pregnancy or how frequently participants used e-cigarettes. Participants who reported e-cigarette use could have used them on a single occasion only, or up to multiple times daily and could have changed their use after becoming pregnant. Furthermore, all measures of tobacco, alcohol, and substance use were based on self-report, and were not verified with biochemical measures, which could result in underestimation of prevalence. Additionally, to assess depression symptoms in pregnancy, we asked two questions regarding symptoms and duration, as specified in the DSM-V, and did not use a standardized depression measure. In future studies the use of standardized measures of depression would improve the validity and generalizability of findings. Finally, these data describe a discrete 3-year period (2015–2018), but e-cigarette products and the characteristics of those using e-cigarettes are continually evolving. Therefore, it is important for research to continue to assess trends of e-cigarette use in pregnancy to provide the most accurate information for clinical care and policy.
Our study also has several strengths. This was the first to specifically assess for depressive symptoms and serious mental health conditions in pregnant women who used e-cigarettes during preconception and/or pregnancy. We found the prevalence of depression was significantly higher in women who used e-cigarettes than in women who used conventional cigarettes, and the prevalence of serious mental illness was higher for women using e-cigarettes or conventional cigarettes than those using no tobacco. Further, our data were collected from a racially and ethnically diverse population of pregnant women with relatively low education and low income, which contributes important information about the use of e-cigarettes in a high-psychosocial-risk population. More research is needed to identify health outcomes associated with the amount and type of e-cigarette exposure in pregnancy.
Conclusions
In a large, diverse sample of pregnant women, we found the prevalence of e-cigarette use before or during pregnancy and/or preconception was 4.0%. In addition, the majority of women using e-cigarettes also used conventional cigarettes. Women who used e-cigarettes and women who used conventional cigarettes had a high prevalence of other substance use, symptoms of depression, and of serious mental health conditions. Increased efforts by providers to screen for tobacco use (including e-cigarette use) and polysubstance use, and to provide or refer to evidence-based cessation interventions could improve outcomes of mothers and children.
Acknowledgments
We gratefully acknowledge the women who contributed to this study. We are also grateful to the Maternal-Infant Studies Laboratory staff for their assistance with data collection.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This work was supported by 2T32MH078788 to L.G.R., T32 AA007459 to N.A.S., and NIDA grants 5R01DA036999 and 5R01DA045492 to L.R.S.
References
- 1. Marynak KL, Gammon DG, Rogers T, Coats EM, Singh T, King BA. Sales of nicotine-containing electronic cigarette products: United States, 2015. Am J Public Health 2017;107:702–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. U.S. Department of Health and Human Services. E-cigarette use among youth and young adults. A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2016 [Google Scholar]
- 3. Ayers JW, Ribisl KM, Brownstein JS. Tracking the rise in popularity of electronic nicotine delivery systems (electronic cigarettes) using search query surveillance. Am J Prev Med 2011;40:448–453 [DOI] [PubMed] [Google Scholar]
- 4. McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, Klein JD. Trends in electronic cigarette use among U.S. adults: Use is increasing in both smokers and nonsmokers. Nicotine Tob Res 2015;17:1195–1202 [DOI] [PubMed] [Google Scholar]
- 5. Gentzke AS, Creamer M, Cullen KA, et al. Vital signs: Tobacco product use among middle and high school students—United States, 2011–2018. MMWR Morb Mortal Wkly Rep 2019;68:157–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patel D, Davis KC, Cox S, et al. Reasons for current E-cigarette use among U.S. adults. Prev Med 2016;93:14–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McCubbin A, Fallin-Bennett A, Barnett J, Ashford K. Perceptions and use of electronic cigarettes in pregnancy. Health Educ Res 2017;32:22–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. Washington, DC: The National Academies Press, 2018 [PubMed] [Google Scholar]
- 9. State of California Environmental Protection Agency. Proposition 65 list of chemicals. Office of Environmental Health Hazard Assessment, Safe Drinking Water And Toxic Enforcement Act of 1986 Chemicals Known to the State to Cause Cancer or Reproductive Toxicity. 2016. Available at: http://oehha.ca.gov/media/downloads/proposition-65//p65single080516.pdf Accessed November1, 2019.
- 10. American College of Obstetricians and Gynecologists. Tobacco use and women's health. Obstet Gynecol 2011;118:746–75021860316 [Google Scholar]
- 11. England LJ, Anderson BL, Tong VTK, et al. Screening practices and attitudes of obstetricians-gynecologists toward new and emerging tobacco products. Am J Obstet Gynecol 2014;211:695..e1–695.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mark KS, Farquhar B, Chisolm MS, Coleman-Cowger VH, Terplan M. Knowledge, attitudes, and practice of electronic cigarette use among pregnant women. J Addict Med 2015;9:266–272 [DOI] [PubMed] [Google Scholar]
- 13. Wagner NJ, Camerota M, Propper C. Prevalence and perceptions of electronic cigarette use during pregnancy. Matern Child Health J 2017;21:1655–1661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu B, Xu G, Rong S, et al. National estimates of e-cigarette use among pregnant and nonpregnant women of reproductive age in the United States, 2014–2017. JAMA Pediatr 2019;173:600–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kurti AN, Redner R, Lopez AA, et al. Tobacco and nicotine delivery product use in a national sample of pregnant women. Prev Med 2017;104:50–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kapaya M, D'Angelo DV, Tong VT, et al. Use of electronic vapor products before, during, and after pregnancy among women with a recent live birth—Oklahoma and Texas, 2015. MMWR Morb Mortal Wkly Rep 2019;68:189–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rostron BL, Corey CG, Chang JT, et al. Associations of cigarettes smoked per day with biomarkers of exposure among US adult cigarette smokers in the Population Assessment of Tobacco and Health (PATH) Study Wave 1 (2013–2014). Cancer Epidemiol Biomarkers Prev 2019;28:1443–1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Osei AD, Mirbolouk M, Orimoloye OA, et al. Association between e-cigarette use and cardiovascular disease among never and current combustible-cigarette smokers. Am J Med 2019;132:949–954.e2. [DOI] [PubMed] [Google Scholar]
- 19. Zhu S-H, Valbø A. Depression and smoking during pregnancy. Addict Behav 2002;27:649–658 [DOI] [PubMed] [Google Scholar]
- 20. Orr ST, Blazer DG, Orr CA. Maternal prenatal depressive symptoms, nicotine addiction, and smoking-related knowledge, attitudes, beliefs, and behaviors. Matern Child Health J 2012;16:973–978 [DOI] [PubMed] [Google Scholar]
- 21. Lewis SJ, Araya R, Davey Smith G, et al. Smoking is associated with, but does not cause, depressed mood in pregnancy—A Mendelian Randomization Study. PLoS One 2011;6:e21689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berlin I, Covey LS. Pre-cessation depressive mood predicts failure to quit smoking: The role of coping and personality traits. Addiction 2006;101:1814–1821 [DOI] [PubMed] [Google Scholar]
- 23. de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res 2005;76:135–157 [DOI] [PubMed] [Google Scholar]
- 24. Smith PH, Mazure CM, McKee SA. Smoking and mental illness in the U.S. population. Tob Control 2014;23:e147–e153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Oh S, Reingle Gonzalez JM, Salas-Wright CP, Vaughn MG, DiNitto DM. Prevalence and correlates of alcohol and tobacco use among pregnant women in the United States: Evidence from the NSDUH 2005–2014. Prev Med 2017;97:93–99 [DOI] [PubMed] [Google Scholar]
- 26. U.S. Department of Health and Human Services, U.S. Department of Agriculture. 2015. –2020 Dietary guidelines for Americans, 8th ed. December 2015. Available at http://health.gov/dietaryguidelines/2015/guidelines Accessed November1, 2019.
- 27. Stroud LR, Papandonatos GD, Borba K, Kehoe T, Scott-Sheldon LAJ. Flavored electronic cigarette use, preferences, and perceptions in pregnant mothers: A correspondence analysis approach. Addict Behav 2018;91:21–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wigginton B, Gartner C, Rowlands IJ. Is it safe to vape? Analyzing online forums discussing e-cigarette use during pregnancy. Womens Heal Issues 2017;27:93–99 [DOI] [PubMed] [Google Scholar]
- 29. England LJ, Tong VT, Koblitz A, Kish-Doto J, Lynch MM, Southwell BG. Perceptions of emerging tobacco products and nicotine replacement therapy among pregnant women and women planning a pregnancy. Prev Med Rep 2016;4:481–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Baeza-Loya S, Viswanath H, Carter A, et al. Perceptions about e-cigarette safety may lead to e-smoking during pregnancy. Bull Menninger Clin 2014;78:243–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Suter MA, Mastrobattista J, Sachs M, Aagaard K. Is there evidence for potential harm of electronic cigarette use in pregnancy? Birth Defects Res Part A Clin Mol Teratol 2015;103:186–195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: A neglected element in the electronic cigarette debate. Am J Prev Med 2015;49:286–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bryden DW, Burton AC, Barnett BR, et al. Prenatal nicotine exposure impairs executive control signals in medial prefrontal cortex. Neuropsychopharmacology 2016;41:716–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ma XD, Li BP, Han Y, Tian YP, Wu L, Wang H. Influence of exposure to nicotine during pregnancy on the learning and memory for adult offspring. Exp Ther Med 2018;15:2404–2410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Aoyama Y, Toriumi K, Mouri A, et al. Prenatal nicotine exposure impairs the proliferation of neuronal progenitors, leading to fewer glutamatergic neurons in the medial prefrontal cortex. Neuropsychopharmacology 2016;41:578–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. England LJ, Aagaard K, Bloch M, et al. Developmental toxicity of nicotine: A transdisciplinary synthesis and implications for emerging tobacco products. Neurosci Biobehav Rev 2017;72:176–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mohsenzadeh Y, Rahmani A, Cheraghi J, Pyrani M, Asadollahi K. Prenatal exposure to nicotine in pregnant rat increased inflammatory marker in newborn rat. Mediators Inflamm 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Spindel ER, McEvoy CT. The role of nicotine in the effects of maternal smoking during pregnancy on lung development and childhood respiratory disease: Implications for dangers of e-cigarettes. Am J Respir Crit Care Med 2016;193:486–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhu S-H, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: Implications for product regulation. Tob Control 2014;23(Suppl 3):iii3–iii9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Clapp PW, Pawlak EA, Lackey JT, et al. Flavored e-cigarette liquids and cinnamaldehyde impair respiratory innate immune cell function. Am J Physiol Lung Cell Mol Physiol 2017;313:278–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One 2015;10:e0116732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Behar RZ, Davis B, Wang Y, Bahl V, Lin S, Talbot P. Identification of toxicants in cinnamon-flavored electronic cigarette refill fluids. Toxicol In Vitro 2014;28:198–208 [DOI] [PubMed] [Google Scholar]