Abstract
Objective: To investigate the prevalence, characteristics, and preventive status of skin injuries caused by personal protective equipment (PPE) in medical staff.
Approach: A cross-sectional survey was conducted online for understanding skin injuries among medical staff fighting COVID-19 in February 8–22, 2020. Participants voluntarily answered and submitted the questionnaire with cell phone. The questionnaire items included demographic data, grade of PPE and daily wearing time, skin injury types, anatomical sites, and preventive measures. Univariable analyses and logistic regression analyses were used to explore the risk factors associated with skin injuries.
Results: A total of 4,308 respondents were collected from 161 hospitals and 4,306 respondents were valid. The overall prevalence of skin injuries was 42.8% (95% confidence interval [CI] 41.30–44.30) with three types of device-related pressure injuries, moist-associated skin damage, and skin tear. Co-skin injuries and multiple location injuries were 27.4% and 76.8%, respectively. The logistic regression analysis indicated that sweating (95% CI for odds ratio [OR] 87.52–163.11), daily wearing time (95% CI for OR 1.61–3.21), male (95% CI for OR 1.11–2.13), and grade 3 PPE (95% CI for OR 1.08–2.01) were associated with skin injuries. Only 17.7% of respondents took prevention and 45.0% of skin injuries were treated.
Innovation: This is the first cross-sectional survey to understand skin injuries in medical staff caused by PPE, which is expected to be a benchmark.
Conclusion: The skin injuries among medical staff are serious, with insufficient prevention and treatment. A comprehensive program should be taken in the future.
Keywords: COVID-19, personal protective equipment, medical staff, occupational injury, skin injury, cross-sectional survey

Qixia Jiang, MSN, RN, ET
Introduction
Since December 2019, COVID-19 broke out and rapidly spread from Wuhan, China. More than 80,000 persons infected and 3,000 over patients were killed by the disease. The National Health Commission of the People's Republic of China announced that it was the largest public health emergency1,2 and continuously revised the guidelines on COVID-19 diagnosis and treatment, aiming to control the epidemic and reduce the mortality rate.2 Early study indicated that the confirmed cases and virus carriers can be the infected source by person-to-person.3,4 Facing the big challenge, more than 40,000 medical staff volunteered to help Wuhan, and tens of thousands of other medical staff joined to fight the COVID-19 around China. They worked daily for 8–12 h wearing personal protective equipment (PPE), including protective masks, goggles, face shield, and protective gowns.5,6 Unfortunately, 80% of them reported that different skin injuries damaged their health and increased the risk of infection.
Clinical Problem Addressed
Literatures reported that device-related pressure injury (DRPI),7–10 moisture-associated skin damage (MASD)10–13 and skin tears (ST),13,14 mostly occurred in patients, but no report of skin injuries on medical staff wearing PPE has been seen. How were the prevalence and characteristics of skin injuries among medical staff? What were the problems in prevention and treatment? This should be addressed urgently. Therefore, we conducted a cross-sectional multicenter survey online to understand the kinds and prevalence, and related factors of skin injuries, to analyze the problems in the prevention and treatment of skin injuries among medical staff during the COVID-19 pandemic, and then to provide a basis for developing strategies.
Materials and Methods
Study design
A cross-sectional multicenter study was designed to understand skin injuries occurring in medical staff fighting COVID-19 in China.
Participants and sample size
The sample size was based on the results of more than 80% skin damage reported by the first batch of medical staff fighting COVID-19 in Wuhan; the allowable error was 1.5% with a 95% confidence interval (CI) and calculated in 2,732 respondents. Considering 10% of invalid questionnaires possibly, a total of 3,036 respondents would be needed. This study was approved by the Medical Ethics Committee of Jingling Hospital, Medical School of Nanjing University.
Participant inclusion criteria were as follows. (1) According to the guidelines of the government,5,6 those medical staff who cared for the suspicious COVID-19 cases in emergency departments and screening clinics were deemed with moderate-risk exposure, and should wear surgical masks with goggles or protective face masks and protective gowns (called as grade 2 PPE); those medical staff who cared for the COVID-19 patients in the infectious department, intensive care units (ICUs), and isolation wards were deemed with high-risk exposure, and should wear N95/KN95 respirators with goggles or protective face masks,15 protective gowns, latex gloves, and shoes (known as grade 3 PPE). (2) Age ≥18 years, regardless of gender. (3) Voluntary participants.
Exclusion criteria were as follows. Medical staff who did not wear PPE or who did not contact the suspicious or confirmed COVID-19 patients.
Data collection tool
We designed a survey questionnaire according to relevant guides, research literature,7–10 and reviewed and revised three times by consulting statistics experts, nursing managers, wound care experts, and feedback from some medical staff in Wuhan. It contained general data (gender, age, the current position and occupation), information on the wearing of PPE (grade of PPE and daily wearing time, sweating), data of skin injuries (types, anatomical locations, severity or symptoms, and when they happened), whether protection was taken (Yes/No), and what preventive measures were adopted (multiple choice) and measures adopted after injury (multiple choice).
Data collection method
We disseminated the questionnaire to the front-line medical staff via the WeChat social platform from February 8 to 22, 2020. The nominated responsible person from 12 hospitals disseminated the questionnaire link to WeChat groups of medical teams who were working in Wuhan and infectious departments or isolation wards or ICUs in other hospitals around the country. Then the link was constantly forwarded to more working groups by WeChat to recruit enough medical staff. Participants voluntarily used their cell phone to answer and submit the questionnaire response online within 2 weeks.
Research quality control
We provided space for comments and multichoice response to questions to answer quickly and accurately. The classification of DRPI depended on the staging system in the 2019 International Guide for Prevention and Treatment of Pressure Ulcer/Injury.16 The 2017 Centers for Medicare & Medicaid Services (CMS) definition was used to identify MASD, “It is caused by sustained exposure to moisture which can be caused, for example, by incontinence, wound exudate, and perspiration.” It is characterized by inflammation of the skin, and occurs with or without skin erosion and/or infection.11 Meanwhile, the 2017 CMS definition was adopted to identify ST: “a result of shearing, friction, or trauma to the skin that causes a separation of the skin layers. They can be partial or full thickness.”11 The classification of ST depended on the International Skin Tear Advisory Panel classification system, including no skin loss (type 1), partial flap loss (type 2), or total flap loss (type 3) (Fig. 1).17
Figure 1.
The classification of ST by the International Skin Tear Advisory Panel. ST, skin tears.
Statistical analysis
All the data were derived from “The Questionnaire Star” website, and the analysis database was established after two researchers checked. The mean (standard deviation) was used to describe participants' characteristics for continuous variables. Categorical variables were described as frequencies (percentages). Univariate analysis was first performed for identifying potential factors for the skin injuries. Pearson's chi-square tests or Fisher's exact tests were used for comparing categorical data as appropriate. Significant variables with p < 0.05 on univariate analysis were entered multivariate logistic analysis. Binary logistic regression with backward method was used for identifying independent predictors for skin injuries. All analyses were done with the statistical software package SPSS 22.0 for Windows (SPSS, Chicago, IL).
Results
General characteristics of medical personnel
In total, 4,308 responded from 161 hospitals in 28 provinces or autonomous regions in the whole country, and of the 4,306 respondents analyzed, 516 (12.0%) were male, 3,790 (88.0%) were female, 505 (11.7%) were doctors, and 3,801 (88.3%) were nurses. Mean age was 32.5 ± 7.1 years, with 2,903 (67.4%) respondents <35 years and 1,403 (32.6%) respondents ≥35 years. Of them, 1,396 respondents (32.4%) and 2,910 respondents (67.6%) wore grade 3 and grade 2 PPE, respectively. The average daily wear time was 7.7 ± 2.9 h, with 14.3% (615 respondents) and 85.7% (3,691 respondents) daily wear time ≤4 and >4 h, respectively. There were 34.1% (1,467 respondents) with heavy sweating while wearing PPE.
Prevalence and characteristics of skin injuries in medical staff
This survey found three kinds of skin injuries in medical staff wearing PPE, namely DRPI, MASD, and ST. In total, 1,844 respondents had 4,735 skin injuries with 2.6 skin injuries per person. The overall prevalence was 42.8% (95% CI 41.30–44.30), and the prevalence of DRPI, MASD, and ST was 30.0% (95% CI 28.69–31.41), 10.8% (95% CI 9.91–11.82), and 2.0% (95% CI 1.62–2.40), respectively. Of them, 386 respondents (27.4%) had 2 or more types of injuries (coinjuries), and 1,080 respondents (76.8%) had 2 or more anatomical part injuries (multiple site injuries). Furthermore, 304 respondents (78.8%) reported coexistence between DRPI and MASD, 51 respondents (13.2%) with coexistence among DRPI, MASD, and ST, 27 respondents (7.0%) with coexistence between DRPI and ST, and 4 respondents (1.0%) with coexistence between MASD and ST. Of 1,293 respondents with DRPI, 1,049 respondents (81.1%) were stage 1, 236 respondents (18.3%) were stage 2, and 8 respondents (0.6%) had deep tissue injury. All of the 86 respondents had type 1 ST. The proportion and location of DRPI, MASD, and ST are shown in Table 1.
Table 1.
The distribution of skin injury types and anatomical sites in medical staff (sites = 4,735)
| Skin Injuries | Nose Bridge |
Cheeks |
Ear |
Forehead |
Othersa |
Total |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| DRPI (n = 1,293) | 986 | 30.6 | 929 | 28.8 | 824 | 25.5 | 448 | 13.9 | 40 | 1.2 | 3,227 | 68.2 |
| MASD (n = 465) | 363 | 29.4 | 338 | 27.3 | 309 | 25.0 | 201 | 16.3 | 26 | 2.1 | 1,237 | 26.1 |
| ST (n = 86) | 74 | 27.3 | 74 | 27.3 | 67 | 24.7 | 51 | 18.8 | 5 | 1.8 | 271 | 5.7 |
| Total (n = 1,844) | 1,423 | 30.1 | 1,341 | 28.3 | 1,200 | 25.3 | 700 | 14.8 | 71 | 1.5 | 4,735 | 100.0 |
Others include armpit, groin, and extremity.
DRPI, device-related pressure injury; MASD, moisture-associated skin damage; ST, skin tears.
The prevalence of skin injuries was higher in male than in female (59.7% vs. 40.5%, p < 0.001), in doctors than in nurses (51.9% vs. 41.6%, p = 0.001), in ones wearing grade 3 PPE than in ones wearing grade 2 PPE (88.5% vs. 21.0%, p < 0.001), in ones with daily wearing time >4 h than in ones with daily wearing time ≤4 h (47.3% vs. 18.7%, p < 0.001), in ones older than 35 years than in ones younger than 35 years (46.3% vs. 41.2%, p = 0.034), and in ones with heavy sweating than in ones without heavy sweating (91.3% vs. 17.8%, p < 0.001). Characteristics and univariate analysis of skin injuries are shown in Table 2.
Table 2.
Characteristics and univariate analysis of skin injuries in medical staff (n = 4,306)
| Characteristics | n | Prevalence of Skin Injuries, n (%) | 95% CI for Prevalence | p |
|---|---|---|---|---|
| Gender (male) | <0.001 | |||
| Male | 516 | 308 (59.7) | 55.40–63.90 | |
| Female | 3,790 | 1,536 (40.5) | 39.00–42.10 | |
| Occupation | 0.001 | |||
| Doctors | 505 | 262 (51.9) | 47.50–56.30 | |
| Nurses | 3,801 | 1,582 (41.6) | 40.10–43.20 | |
| Heavy sweat | <0.001 | |||
| Yes | 1,467 | 1,340 (91.3) | 89.90–92.80 | |
| No | 2,839 | 504 (17.8) | 16.30–19.20 | |
| Grade of PPE | <0.001 | |||
| Grade 3 | 1,396 | 1,236 (88.5) | 86.90–90.20 | |
| Grade 2 | 2,900 | 608 (21.0) | 19.50–22.40 | |
| Daily wearing time (h) | <0.001 | |||
| ≤4 | 674 | 126 (18.7) | 15.70–21.60 | |
| >4 | 3,632 | 1,718 (47.3) | 45.70–48.90 | |
| Age (years old) | 0.034 | |||
| <35 | 2,903 | 1,195 (41.2) | 39.40–43.00 | |
| ≥35 | 1,403 | 649 (46.3) | 43.60–48.90 |
CI, confidence interval; PPE, personal protective equipment.
Multivariate analysis of skin injury in medical staff
Skin injuries were set as the dependent variable (0 = none, 1 = yes), and the single factors of p < 0.05 (Table 2) were set as the independent variables: male = 1, female = 0; wearing grade 3 PPE = 1, grade 2 PPE = 0; doctors = 1, nurses = 0, heavy sweat = 1, without sweat = 0. Daily wearing time >4 h = 1 and ≤4 h = 0. A multivariate logistic regression analysis was performed with the backward method. The variable of occupation and age was removed from the final multivariate logistic model, and the heavy sweat, daily wearing time, gender, and grade of PPE were retained in the model, which associated with the occurrence of skin injuries. The omnibus tests of the model coefficients were χ2 = 3,023.496 (df = 4, p < 0.001). The Nagelkerke R2 of model summary was 0.703, which meant that 70.3% of the observed variation of dependent variable could be explained by independent variables. The results are shown in Table 3.
Table 3.
Multivariate analysis of factors associated with skin injuries
| Factors | OR | 95% CI | p |
|---|---|---|---|
| Heavy sweat (1) | 119.48 | 87.52–163.11 | <0.001 |
| Gender (male) | 1.54 | 1.11–2.13 | 0.008 |
| Grade of PPE (1) | 1.47 | 1.08–2.01 | 0.014 |
| Daily wearing time (1) | 2.27 | 1.61–3.21 | <0.001 |
| Constant | 0.02 | <0.001 |
OR, odds ratio.
Preventive and treating status of skin injuries in medical staff
In total, 763 (17.7%) respondents used preventive dressings or oil agents to prevent skin injuries. Of the 1,844 respondents who suffered skin injuries, 1,014 (55.0%) respondents had no treatment and 830 (45.0%) respondents were treated by dressings, oil agents, or other methods. The details are shown in Table 4.
Table 4.
Prevention measures for skin injuries (n = 1,407)
| Skin injuries | n | Foam |
Hydrocolloid |
Oil or Cream |
Oil with Dressings |
Personal |
Untreated |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| DRPI (a) | 911 | 57 | 6.3 | 203 | 22.3 | 89 | 9.8 | 68 | 7.5 | 75 | 8.2 | 419 | 46.0 |
| MASD (b) | 106 | 5 | 4.7 | 10 | 9.4 | 38 | 35.9 | 4 | 3.8 | 10 | 9.4 | 39 | 36.8 |
| ST (c) | 4 | 0 | 0.0 | 1 | 25.0 | 2 | 50.0 | 0 | 0.0 | 0 | 0.0 | 1 | 25.0 |
| a+b | 304 | 17 | 5.6 | 60 | 19.7 | 47 | 15.5 | 49 | 16.1 | 30 | 9.9 | 101 | 33.2 |
| a+c | 27 | 0 | 0.0 | 6 | 22.2 | 6 | 22.2 | 5 | 18.5 | 2 | 7.4 | 8 | 29.6 |
| b+c | 4 | 0 | 0.0 | 0 | 0.0 | 1 | 25.0 | 1 | 25.0 | 2 | 50.0 | 0 | 0.0 |
| a+b+c | 51 | 3 | 5.9 | 12 | 23.5 | 4 | 7.8 | 22 | 43.1 | 1 | 2.0 | 9 | 17.7 |
| Total | 1,407 | 82 | 5.8 | 292 | 20.8 | 187 | 13.3 | 149 | 10.6 | 120 | 8.5 | 577 | 41.0 |
Discussion
Prevalence and characteristics of skin injuries in medical staff were different
The pandemic outbreak of COVID-19 raised a new issue of global concern since December 2019, skin injuries among medical staff wearing PPE that impaired their health and increased the probability of infection. More than 3,000 medical staff were infected in China and much more in other countries. Subsequently, the government released an urgent notice that further protected medical staff during COVID-19 control efforts.18 Therefore, this study provided a basis for further protecting medical staff, and provided a reference for protecting skin when fighting COVID-19 in other countries. A higher prevalence of skin injuries among medical staff was found, mainly coexistence of DRPI, MASD, and ST with coinjuries and multiple anatomical sites (Tables 1 and 4). That is rare in previous studies in patients. ICU, orthopedic, and geriatric patients were the susceptible population of DRPI, MASD, and ST.11–13 Different devices caused different skin injuries and prevalence,7–10,12,13,19 and many differences were found between medical staff and patients. First, the prevalence of DRPI 30.0% (95% CI 28.69–31.41) in medical staff was higher than in patients using respiratory devices, tubes, and splints (3.1–27.9%).8,10 Second, the prevalence of MASD 10.8% (95% CI 9.91–11.82) in medical staff was lower than in patients in ICU (20%),20 but higher than in patients with chronic wounds (6.06%).21 Third, the prevalence of ST 2.0% (95% CI 1.62–2.40) in medical staff was higher than 1.06% in patients in a multicenter study,14 but significantly lower than 22% elderly patients in a systematic review.22 Fourth, the susceptible parts of skin injuries in medical staff were on the nose bridge, cheeks, ears, and forehead (Table 1), and in patients, DRPI mainly located on ears and feet,10,23 MASD occurred on skin fold, periwounds, or peristoma,19–22,24,25 and ST occurred on extremities.14,22 The reasons possibly were as follows. (1) Devices and wearing time in medical staff were different. According to Chinese regulations, medical staff wearing PPE should be replaced every 4 h. However, they actually had to work 8–12 h continuously due to the serious epidemic situation and inadequate medical resources. Of their long hours wearing PPE, the N95 respirators or surgical masks15,25 and goggles would compress nose bridge and cheeks, a mask strap would compress the ears, and face shield and surgical cap would compress the forehead, which might be the main cause of skin injuries on multiple parts of the head and face. (2) Different activity possibly resulted in different skin injuries. Most of the patients were in bed, while medical staff moved rapidly to save more people's lives with long hours and high-intensity work, which was why 1,467 (34.1%) respondents reported heavy sweating and soaked skin. Moreover, the heavy and airtight PPE made it difficult to volatilize perspiration, which changed the skin microclimate and decreased skin tolerance.12,13 All these factors would influence the development of skin injuries. (3) Sweating stimulated the skin and caused redness, pain, itching, or prickling, which might be the main cause of MASD. (4) Soaked skin combined with pressure increased friction coefficient between the PPE and skin, and when masks and goggles were removed quickly, ST was ready to happen. To sum up, these might be the reasons of coinjuries and multiple anatomical site injuries in medical staff (Fig. 2).
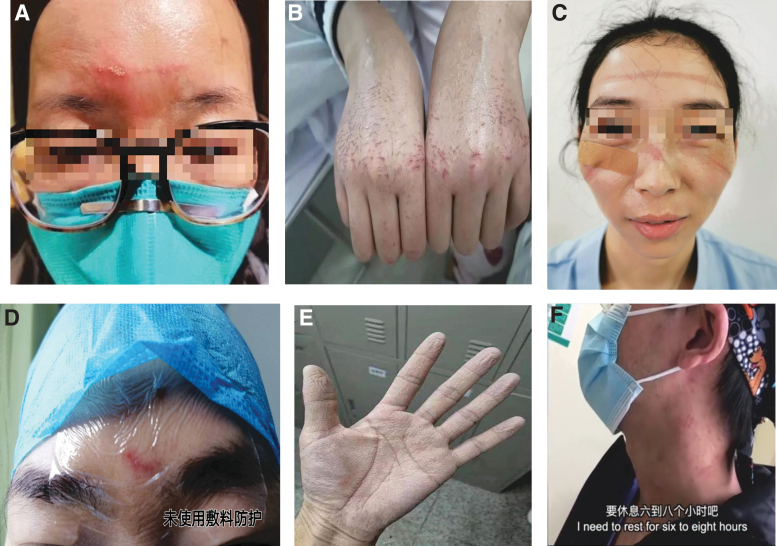
Figure 2.
(A) DRPI+MASD on forehead. (B) MASD+ST on hands. (C) DRPI+ST+MASD on face. (D) ST on forehead. (E) MASD on palm. (F) MASD+DRPI on neck. DRPI, device-related pressure injury; MASD, moisture-associated skin damage.
The related factors of skin injuries in medical staff were different
This study showed that the prevalence of skin injuries between doctors and nurses, male and female, grade 3 and grade 2 PPE, daily wearing time ≤4 and >4 h, with and without heavy sweating, age <35 and ≥35 years old was different (all p < 0.05–0.001) (Table 2). The logistic regression analysis showed that (Table 3) the grade of PPE, daily wearing time, heavy sweating, and gender (male) increased risk of skin injuries. First, heavy sweating significantly increased risk of skin injuries (odds ratio [OR] 119.48, 95% CI 87.52–163.11, p < 0.001), and it could be related to increasing perspiration when medical staff were wearing PPE. It means that controlling the sweat and moisture on the skin is very important. Second, daily wearing time (OR 2.27, 95% CI 1.61–3.21, p < 0.001) can be predicted that the longer wearing time, the greater risk of skin injuries. This is also the reason why PPE should be replaced every 4 h, as given in the national guidelines, which also proves its necessity again. Third, male (OR 1.54, 95% CI 1.11–2.13, p = 0.008) increased risk that may be related to sweating more easily than female, and most Chinese men do not pay much attention to daily skin care. It means that males need more skin protection. Fourth, grade 3 PPE (OR 1.47, 95% CI 1.08–2.01, p = 0.014) increased risk that may be related to sweating more and compression. Thus, skin injuries caused by PPE are a comprehensive effect. It means that comprehensive preventive measures are needed.
Insufficient prevention and treatment in medical staff were a big problem
The study showed that only 17.7% of respondents used prophylactic dressings and lotions to protect the skin, and of them, 40% of respondents with sweating and wearing grade 3 PPE took preventive measures. Only 45.0% of respondents with injuries adopted hydrocolloid dressing, oil, or cream to treat (Table 4). It meant that prevention and treatment were insufficient. The reasons may be related to the following factors. First, medical staff and managers ignored skin protection at early stage. Second, medical staff in the frontline received no training how to prevent and treat skin injuries, and little was known how to use dressings. Some worried that if they used dressings to protect their nose bridge and cheeks, the mask and goggles would not close enough and possibly bring higher infected risk. Finally, relevant preventive resources in response to public health emergencies were inadequate, and so, medical staff used what was available. This study suggests that it is necessary to make adequate preparations for public health emergencies. First of all, managers should pay attention to skin protection and seek a rational allocation of medical resources. Then, it is more important to train medical staff about knowledge of skin protection by WeChat, booklets, and so on. Furthermore, the protective products should be selected according to the guidelines, such as prophylactic dressings and fatty acid cream.15,25,26 The material and shape of prophylactic dressings should be improved in the future, such as to develop various prophylactic dressings suitable for the head and face to effectively keep the moisture balance and protect skin, which are beneficial to deal with skin injuries of medical staff in public health emergencies.
Limitations
Because of the emergency situation, there are some limitations to this study, such as it was difficult to observe the adverse outcome of skin injuries among medical staff and impossible to compare the results of prevention and treatment measures. These might leave us opportunities for further study.
Innovation
In response to the problems in the COVID-19 pandemic, we developed a questionnaire of the first-time surveyed skin injuries among medical staff wearing PPE. We found a higher prevalence of skin injuries characterized by coinjuries and multipart injuries, four related factors, and insufficient prevention and treatment status. This will provide a basis for protecting medical staff and improving PPE around the world.
KEY FINDINGS
This study demonstrated that the prevalence of skin injuries among medical staff caused by PPE fighting COVID-19 was higher. It was characterized by coinjuries and multiple site injuries, affecting their health and occupational safety, even becoming potential risk factors for them with COVID-19.
We found that four related factors (heavy sweating, longer daily wearing time, male, and wearing grade 3 PPE) might increase the risk of skin injuries.
The deficiency of prevention and treatment cannot be ignored.
Comprehensive preventive measures such as improving PPE, shortening wear time, and taking protective measures should be taken.
Acknowledgments and Funding Sources
The authors thank the coordinators and medical staff at the participating hospitals. They also thank the Shanghai Wang Zhengguo Trauma Medicine Development Foundation Project (WZGF20200101) and the Military Medical Service Special Project (20WQ027) for financial support.
Abbreviations and Acronyms
- CI
confidence interval
- CMS
Centers for Medicare & Medicaid Services
- COVID-19
corona virus disease 2019
- DRPI
device-related pressure injury
- ICU
intensive care unit
- MASD
moisture-associated skin damage
- OR
odds ratio
- PPE
personal protective equipment
- ST
skin tears
Author Disclosure and Ghostwriting
The authors declare that they have no conflicts of interest in this work. No ghost writer was used for the preparation of this article.
About the Authors
Qixia Jiang, MSN, RN, ET, is the head nurse in Department of Burns and Plastic Surgery, and responsible for skin and wound care in Jinling Hospital, Medical School of Nanjing University. She is responsible for designing the questionnaire, organizing survey and quality control, drafting the article, and revising it. Siping Song, BSN, assisted in checking and setting up databases, searched literature, and revised the article. Jihong Zhou, MD, is a surgeon in the Department of Burns and Plastic Surgery in Jinling Hospital. He is responsible for specialized review and quality control. Yuxiu Liu, MS, is the Director of Department of Medical Statistics in Jinling Hospital. He is responsible for checking design protocol and statistical analysis. Aihua Chen, BSN, ET, is responsible for collecting data and quality control. Yuxuan Bai, BS, is responsible for checking data and setting up databases. Jing Wang, MSN, ET; Zhixia Jiang, MSN; Yanhong Zhang, BSN, ET; Haiying Liu, BSN; Jiao Hua, BSN; Jinli Guo, MSN; Qiuying Han, MSN; and Yongli Tang, BSN, are responsible for data collection and quality control. Jiayu Xue, BSN, is responsible for monitoring and downloading data and checking.
References
- 1. National Health Commission of the People's Republic of China. Law of the People's Republic of China on Prevention and Treatment of Infectious Diseases. www.nhc.gov.cn/jkj/s7915/202001/e4e2d5e6f01147e0a8df3f6701d49f33.shtml (last accessed February15, 2020)
- 2. National Health Commission of the People's Republic of China. The Management of COVID-19 Prevention and Control (the Fifth edition). www.nhc.gov.cn/jkj/s3577/202002/a5d6f7b8c48c451c87dba14889b30147/files/3514cb996ae24e2faf65953b4ecd0df4.pdf (last accessed February21, 2020) [DOI] [PMC free article] [PubMed]
- 3. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020. Feb 28 [Epub ahead of print]; DOI: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Health Commission of the People's Republic of China. Guidelines on medical protective products during prevention and control of viral pneumonia caused by COVID-19[EB/OL]. www.nhc.gov.cn/xcs/zhengcwj/202001/e71c5de925a64eafbe1ce790debab5c6.shtml (last accessed February20, 2020)
- 6. Chinese Center for Disease Control and Prevention. Technical guidelines on the selection and use of anti-COVID-19 respirator for different populations. www.nhc.gov.cn/jkj/s7916/202002/485e5bd019924087a5614c4f1db135a2.shtml (last accessed February20, 2020)
- 7. Barakat-Johnson M, Lai M, Wand T, Li M, White K, Coyer F. The incidence and prevalence of medical device-related pressure ulcers in intensive care: a systematic review. J Wound Care 2019;28:512–521 [DOI] [PubMed] [Google Scholar]
- 8. Barakat-Johnson M, Barnett C, Wand T, White K. Medical device-related pressure injuries: an exploratory descriptive study in an acute tertiary hospital in Australia. J Tissue Viability 2017;26:246–253 [DOI] [PubMed] [Google Scholar]
- 9. Jackson D, Sarki AM, Betteridge R, Brooke J. Medical device-related pressure ulcers: a systematic review and meta-analysis. Int J Nurs Stud 2019;92:109–120 [DOI] [PubMed] [Google Scholar]
- 10. Kayser SA, VanGilder CA, Ayello EA, Lachenbruch C. Prevalence and analysis of medical device-related pressure injuries: results from the International Pressure Ulcer Prevalence Survey. Adv Skin Wound Care 2018;31:276–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ayello EA. CMS MDS 3.0 Section M skin conditions in long-term care: pressure ulcers, skin tears, and moisture-associated skin damage data update. Adv Skin Wound Care 2017;30:415–429 [DOI] [PubMed] [Google Scholar]
- 12. Woo KY, Beeckman D, Chakravarthy D. Management of moisture-associated skin damage: a scoping review. Adv Skin Wound Care 2017;30:494–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zulkowski K. Understanding moisture-associated skin damage, medical adhesive-related skin injuries, and skin tears. Adv Skin Wound Care 2017;30:372–381 [DOI] [PubMed] [Google Scholar]
- 14. Jiang Qx, Jiang ZX, Zheng MC, et al. A multicenter, and cross-sectional survey of the prevalence and epidemiologic characteristics of skin tears in hospitals. Chin Nurs Manag 2017;17:631–635 [Google Scholar]
- 15. Smith JD, MacDougall CC, Johnstone J, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ 2016;188:567–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler, ed. EPUAP/NPIAP/PPPIA, 2019 [Google Scholar]
- 17. LeBlanc K, Baranoski S, Christensen D, et al. International Skin Tear Advisory Panel: a tool kit to aid in the prevention, assessment, and treatment of skin tears using a Simplified Classification System ©. Adv Skin Wound Care 2013;26:459–478 [DOI] [PubMed] [Google Scholar]
- 18. National Health Commission of the People's Republic of China. Notice on further strengthening the protection of medical personnel during the epidemic prevention and control. www.nhc.gov.cn/yzygj/s7659/202002/75c6e88ecbeb42a9a26acb538383e2fc.shtml (last accessed February20, 2020)
- 19. Colwell JC, Ratliff CR, Goldberg M, et al. MASD part 3: peristomal moisture-associated dermatitis and periwound moisture-associated dermatitis: a consensus. J Wound Ostomy Continence Nurs 2011;38:541–553; quiz 554–555. [DOI] [PubMed] [Google Scholar]
- 20. Valls-Matarín J, Del Cotillo-Fuente M, Ribal-Prior R, Pujol-Vila M, Sandalinas-Mulero I. Incidence of moisture-associated skin damage in an intensive care unit. Enferm Intensiva 2017;28:13–20 [DOI] [PubMed] [Google Scholar]
- 21. Jiang QX, Wang JD, Dong S. Application of two skin protection methods in the treatment of chronic wound with negative pressure wound therapy. Chin J Nurs 2020;55:39–45 [Google Scholar]
- 22. Strazzieri-Pulido KC, Peres GR, Campanili TC, Santos VL. Skin tear prevalence and associated factors: a systematic review [in Portuguese]. Rev Esc Enferm USP 2015;49:674–680 [DOI] [PubMed] [Google Scholar]
- 23. Otero DP, Domínguez DV, Fernández LH, et al. Preventing facial pressure ulcers in patients under non-invasive mechanical ventilation: a randomised control trial. J Wound Care 2017;26:128–136 [DOI] [PubMed] [Google Scholar]
- 24. Whitehead F, Giampieri S, Graham T, Grocott P. Identifying, managing and preventing skin maceration: a rapid review of the clinical evidence. J Wound Care 2017;26:159–165 [DOI] [PubMed] [Google Scholar]
- 25. Loeb M, Dafoe N, Mahony J, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA 2009;302:1865–1871 [DOI] [PubMed] [Google Scholar]
- 26. Clark M, Black J, Alves P, et al. Systematic review of the use of prophylactic dressings in the prevention of pressure ulcers. Int Wound J 2014;11:460–471 [DOI] [PMC free article] [PubMed] [Google Scholar]